Abstract
Malaria is endemic in large parts of India and can cause multiorgan failure and death. Acute pancreatitis as a complication is rare and is potentially fatal. This case series describes five adult patients between 2005 and 2010 who presented with a short duration febrile illness and diagnosed to have malaria with acute pancreatitis. The mean age of the five patients with acute pancreatitis was 40.4 years and four of them were males. None of them were alcohol consumers and did not have any other risk factor for acute pancreatitis. Plasmodium falciparum was responsible for all the cases. Pancreatic enzymes were significantly elevated in all the patients with a mean serum lipase level of 1795 U/L (normal value: <190 U/L) and a mean serum amylase level of 584 U/L (normal value: <100 U/L). Ultrasonography evidence of acute pancreatitis (bulky pancreas) was seen in two patients, and a further two patients had minimal left-sided pleural effusion. Thrombocytopenia (platelet count <100,000/cumm), renal dysfunction (serum creatinine >1.4 mg/dl), and hyperbilirubinemia were seen in all the patients. One patient died due to multiorgan failure. Acute pancreatitis is a very rare complication of malaria, and a high index of suspicion is required in patients presenting with severe malaria and abdominal pain.
Keywords: Complication, malaria, pancreatitis
Introduction
Malaria is a common protozoan disease in tropical countries caused by the genus Plasmodium transmitted by the bite of infected anopheles mosquitoes. Severe complicated malaria is most frequently caused by Plasmodium falciparum and much less commonly by Plasmodium vivax or other Plasmodium species. Abdominal pain as a presenting complaint has been reported in 21.4–33.5% of patients with malaria and is usually mild and transient.[1] It occasionally can be severe and persistent, especially with complications such as splenic infarction, splenic rupture, splenic torsion, acalculous cholecystitis, and hepatitis. However, acute pancreatitis causing abdominal pain and complicating malaria is very rare and there are only 12 cases reported from literature till now. We describe five patients who were diagnosed to have malaria complicated by acute pancreatitis.
Case Report
Five patients admitted in the Christian Medical College, Vellore between 2005 and 2010 with a diagnosis of malaria and acute pancreatitis are described. Malaria was confirmed by demonstration of the characteristic ring forms of either P. falciparum or P. vivax on a thin blood smear. Acute pancreatitis was diagnosed in the presence of at least two of the following criteria: Acute, persistent, and severe abdominal pain not subsiding with proton pump inhibitors, elevation in serum lipase or amylase to three times greater than the upper limit of normal, and characteristic findings of acute pancreatitis on radiographic imaging. Other causes of pancreatitis such as alcohol, gall stones, and hypercalcemia were ruled out.
In addition, a Medline search was performed to identify the cases of malaria with acute pancreatitis reported in the literature using the search terms “malaria,” “P. falciparum,” “P. vivax”, and “pancreatitis.” Cases were accepted where information regarding the demographics, laboratory tests, and the outcome was provided.
This study was approved by the Institutional Review Board of Christian Medical College, Vellore (IRB Min No. 8327), and patient confidentiality was maintained using unique identifiers.
Results
The mean age of the patients was 40.4 years, and 4 out of 5 were males. All the patients were healthy before the current illness, and none had prior history of chronic alcohol consumption or cholelithiasis. None of the patients had any prior history of abdominal procedures including endoscopic retrograde cholangiopancreatography. The mean duration of fever before presentation was 7.8 days. All the patients had a history of abdominal pain, which was central and did not improve with proton-pump inhibitors. The pain started 2–9 days after the onset of fever. None of the patients had pain radiating to the back. All of these patients had P. falciparum infection with a variable parasitic index, ranging from 0.14 to 32, as demonstrated on a thin film.
Pancreatic enzymes were significantly elevated in all, with a mean serum lipase level of 1795 U/L (normal value: <190 U/L) and a mean serum amylase level of 584 U/L (normal value: <100 U/L). Ultrasonography evidence of acute pancreatitis (bulky pancreas) was seen in two patients, and a further two patients had minimal left-sided pleural effusion. Thrombocytopenia (platelet count <100,000/cumm), renal dysfunction (serum creatinine >1.4 mg/dl) and hyperbilirubinemia were seen in all the patients.
All the patients were treated with an artemisinin-based combination therapy along with doxycycline. Acute pancreatitis was managed conservatively with nil oral intake and opioid pain killers. Gradual feeds were started once the pain reduced. One of the patients (Case 5) required a nasojejunal tube placement for pancreatitis. Clinical characteristics and medications including antibiotics are mentioned in Table 1. Four of the patients required hemodialysis for renal dysfunction. One patient (Case 3) who presented with a parasitic index of 0.5% severe malaria with hepatic, renal, neurological and hematological dysfunction and required invasive ventilator support and multiple sessions of hemodialysis. Despite these aggressive measures, he succumbed to the illness on the 7th day of admission. The patient profile, laboratory investigations, and outcome of these five patients are shown in Table 2.
Table 1.
Clinical characteristics and medications
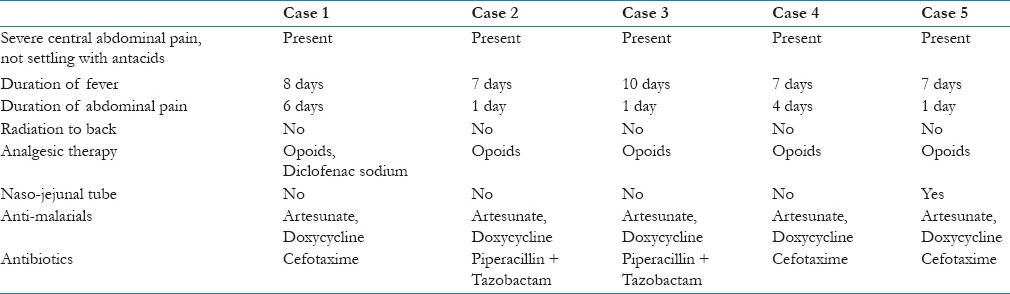
Table 2.
Profile of five cases of malaria with acute pancreatitis

Discussion
India's expansive geography and tropical environment are ideal for sustaining malaria vectors, and it accounts for 76% of cases from Southeast Asia. Although the overall deaths have reduced since the launch of National Malaria Control Program, it is argued that reports of approximately 1000 deaths per year are grossly underestimated.[2] Multiorgan involvement or dysfunction is reported in both P. falciparum and P. vivax infections. P. falciparum contributes to 52% of the total malaria cases in India and is responsible for the majority of deaths.[2] Acute pancreatitis as a complication of malarial infection, though rare, has been usually reported with P. falciparum. It has been associated with at least four deaths, in the reported 15 cases reported in literature based on our Medline search. Primary care physicians deal mostly with vivax malaria in most parts of India as it is usually the predominant species. In our case series, two patients had pancreatitis due to P. vivax malaria. Recent studies have shown that vivax malaria can be as severe as falciparum malaria, a fact consistent with our finding of a severe complications such as pancreatitis due to P. vivax.[3]
In our case series, one patient died as a result of multiorgan involvement including acute pancreatitis, the causative organism being P. falciparum. Only two patients (Case 1 and Case 4) had a high parasitic index. Seshadri et al., Mandal et al. and Mohapatra and Gupta have reported pancreatitis with very high parasitic indices.[4,5,6] Hyperparasitemia though a predictor for severe malaria is not the only marker for severity. In patients not previously exposed to malaria poor immunity may result in severe disease even with parasitic index as low as 2%. The pathogenesis of pancreatitis is probably not different from that of other organ involvement in malaria and includes cytoadherence of infected red blood cells (RBCs) to the vascular endothelium, sequestration of RBCs, and rosetting. This is especially true in falciparum malaria. However, sequestration occurring in other organs including pancreas is not known as of now.
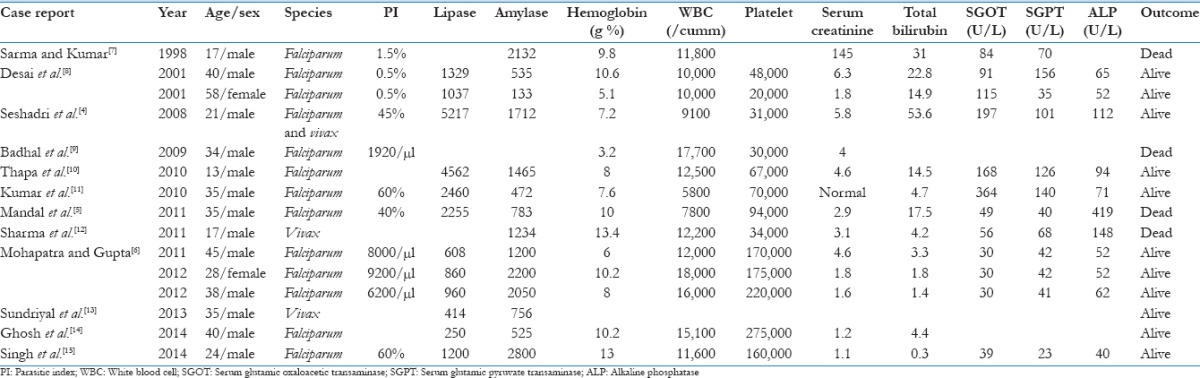
In our literature search, we found only 15 cases of malaria complicated by pancreatitis and their profile is summarized in Table 3.[4,5,6,7,8,9,10,11,12,13,14,15]
Table 3.
Literature review of patients with malaria and acute pancreatitis
In our country, malaria continues to be a major public health problem in India, accounting for sizeable morbidity and mortality. The burden of falciparum malaria is very high in places such as Orissa and the Northeastern states where the mortality rate due to malaria is even higher. Fever and abdominal pains are very common presentations to the emergency department and pancreatitis accounts for about 11% of those cases.[16] Primary care physicians’ deal with these common problems in their daily practice and their etiology quite often remains a diagnostic dilemma. Greater awareness of the rare complications of a common infection such as malaria is essential to recognize it early and to initiate early management or early referral to a higher center.
Conclusion
Physicians may be familiar with the various complications of falciparum malaria but less so with acute pancreatitis. The ability to properly diagnose and to manage acute pancreatitis due to malaria is particularly important in malaria-endemic areas such as India. Maintaining a high index of suspicion for acute pancreatitis in patients with malaria presenting with abdominal pain can be important in the early diagnosis and prevention of pancreatic complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zaki SA. Abdominal pain as a presenting feature in malaria. Sri Lanka J Child Health. 2010;39:158–9. [Google Scholar]
- 2.Kumar A, Valecha N, Jain T, Dash AP. Burden of malaria in India: Retrospective and prospective view. Am J Trop Med Hyg. 2007;77(6 Suppl):69–78. [PubMed] [Google Scholar]
- 3.Mitra S, Abhilash K, Arora S, Miraclin A. A prospective study from South India to compare the severity of malaria caused by Plasmodium vivax, P. falciparum and dual infection. J Vector Borne Dis. 2015;52:281–6. [PubMed] [Google Scholar]
- 4.Seshadri P, Dev AV, Viggeswarpu S, Sathyendra S, Peter JV. Acute pancreatitis and subdural haematoma in a patient with severe falciparum malaria: Case report and review of literature. Malar J. 2008;7:97. doi: 10.1186/1475-2875-7-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mandal B, Das BK, Chatterjee SK, Guh P, Shai S, Sharma A, et al. Acute pancreatitis in a case of falciparum malaria – A rare presentation. J Assoc Physicians India. 2011;59:731–3. [PubMed] [Google Scholar]
- 6.Mohapatra MK, Gupta MP. Falciparum malaria complicated with acute pancreatitis: A report of case series. J Vector Borne Dis. 2011;48:177–9. [PubMed] [Google Scholar]
- 7.Sarma PS, Kumar RS. Abdominal pain in a patient with falciparum malaria. Postgrad Med J. 1998;74:425–7. doi: 10.1136/pgmj.74.873.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Desai DC, Gupta T, Sirsat RA, Shete M. Malarial pancreatitis: Report of two cases and review of the literature. Am J Gastroenterol. 2001;96:930–2. doi: 10.1111/j.1572-0241.2001.03658.x. [DOI] [PubMed] [Google Scholar]
- 9.Badhal SS, Irshad M, Badhal S, Yadav K. Acute on chronic pancreatitis masking falciparum malaria: A case report. Glob J Health Sci. 2009;1:123–5. [Google Scholar]
- 10.Thapa R, Mallick D, Biswas B. Childhood Plasmodium falciparum malaria complicated by acute pancreatitis. Trop Doct. 2010;40:184–5. doi: 10.1258/td.2010.090420. [DOI] [PubMed] [Google Scholar]
- 11.Kumar S, Jain AP, Vikas Falciparum malaria presenting as acute pancreatitis. J Vector Borne Dis. 2010;47:121–2. [PubMed] [Google Scholar]
- 12.Sharma V, Sharma A, Aggarwal A, Bhardwaj G, Aggarwal S. Acute pancreatitis in a patient with vivax malaria. JOP. 2012;13:215–6. [PubMed] [Google Scholar]
- 13.Sundriyal D, Kumar N, Chandrasekharan A, Sharma B, Patnaik I, Kamble U. Fatal complications of Plasmodium vivax malaria: A series of three case reports. Ann Trop Med Public Health. 2013;6:578–80. [Google Scholar]
- 14.Ghosh S, Das SK, Sharma A. Unusual presentation of acute pancreatitis in falciparum malaria. Trop Parasitol. 2014;4:56–7. doi: 10.4103/2229-5070.129188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh J, Dinkar A, Atam V, Atam I, Jitendra S. An uncommon presentation of severe falciparum malaria: Acute pancreatitis. Int Res J Med Sci. 2014;2:26–8. [Google Scholar]
- 16.Chanana L, Jegaraj MA, Kalyaniwala K, Yadav B, Abilash K. Clinical profile of non-traumatic acute abdominal pain presenting to an adult emergency department. J Family Med Prim Care. 2015;4:422–5. doi: 10.4103/2249-4863.161344. [DOI] [PMC free article] [PubMed] [Google Scholar]


