Abstract
The eradication of Helicobacter pylori is essential for prevention and treatment of various conditions associated with this infection. However, its effectiveness is limited and influenced by factors linked to the bacteria and the host. In particular, influence of the biotype, smoking, diabetes mellitus, and previous treatment failure in eradication is understudied. Our center proposed to evaluate these aspects in a real life cohort by applying a questionnaire with demographic and lifestyle variables in patients who consecutively underwent urease breath test after the eradication therapy.
Keywords: Helicobacter pylori, eradication, questionnaire
1. Introduction
Classically, the resistance of Helicobacter pylori (H. pylori) to eradication therapies is considered the most important factor negatively affecting the effectiveness of those therapies. However, treatment effectiveness also depends on a series of host factors alongside with the antibiotic resistance. In the last two decades, several studies have shown strong evidence of some of these factors related to the host that negatively influence the eradication rates, especially polymorphisms in the genes CYP2C19, MDR1, and IL-1,[1-3] low compliance,[4] and hypersecretion of hydrochloric acid.[5] However, the evidence is scarce for other factors, particularly the impact biotype,[6] smoking,[7] diabetes mellitus (DM),[8] and previous treatment failure. In particular, it is unknown whether the body mass index (BMI) influences in a clinically significant way the pharmacokinetics and/or pharmacodynamics of the drugs involved in eradication (in particular, the proton pump inhibitors and antibiotics). Furthermore, to date, studies are in most cases controlled in relation to the therapeutic regimen used, imposing doubts about its application in real life cohorts.
Materials and Methods
For six months (from June to December 2015), all patients undergoing breath test for eradication of H. pylori infection were enrolled, regardless of indication for treatment. The initial diagnosis was confirmed by gastric histology after upper endoscopy. Breath test was performed at least one month after the end of antibiotic therapy, with suspension of proton pump inhibitors (PPI) at least two weeks earlier. The result was considered positive or negative according to the manufacturer’s reference. Patients with prior failure of eradication treatment undergoing a new breath test were also included.
All patients completed a questionnaire indicating the symptoms, including dyspepsia and gastroesophageal reflux, and personal or family history of H. pylori infection, peptic ulcer disease, gastric adenocarcinoma or gastric lymphoma. In all the cases, habitual medication, smoking and alcoholic habits (considered relevant if >80 g/d in men and >40 g/d in women) were recorded. Patients were also questioned about comorbidities such as depression, anxiety, and diabetes mellitus.
Weight and height were recorded in all patients, with a subsequent calculation of BMI. According to the value, patients were grouped into low weight (<18 kg/m2), normal weight (18-24.9 kg/m2), overweight (25-29.9 kg/m2) and obesity (>30 kg/m2).
According to the information provided by the patient and the medical records, the prescribed eradication schemes were collected, distinguishing between the various PPIs and their duration (7, 10 or 14 days). Triple, concomitant and sequential therapies were taken into account. Finally, patients were questioned about adherence to therapy and presence of adverse symptoms.
Statistical analysis
Data were collated in an SPSS® database (20.0, SPSS, Chicago, IL). All data were expressed as median (range). Different groups were defined for analysis according to BMI, obese and non-obese, smoker and non-smoker, diabetes and non-diabetes, previous treatment failure, PPI used, eradication scheme used, and duration of treatment. Differences between groups were evaluated using the Mann–Whitney test. Fisher’s exact was used to compare the H. pylori eradication rates yielded by the groups. Multiple logistic regression was used to assess the relationship between the eradication rate and age, gender, smoking habits, pattern of gastritis, and BMI. A P value < 0.05 was considered statistically significant.
Results
A total of 121 patients were evaluated, 70% of whom were females, with a mean age 50 ± 13 years. Eighty patients (66.1%) were referred by the Surgery consultation; in majority of cases, in the context of preparation for bariatric surgery.
Most patients reported symptoms, namely dyspepsia (46%) and/or regurgitation/heartburn (20%). Previous failed one or more eradication schemes was observed in 27% of the patients. The majority had an abnormal endoscopy with chronic gastritis in 69%, and intestinal metaplasia in 13%. In 28%, endoscopy was considered as normal.
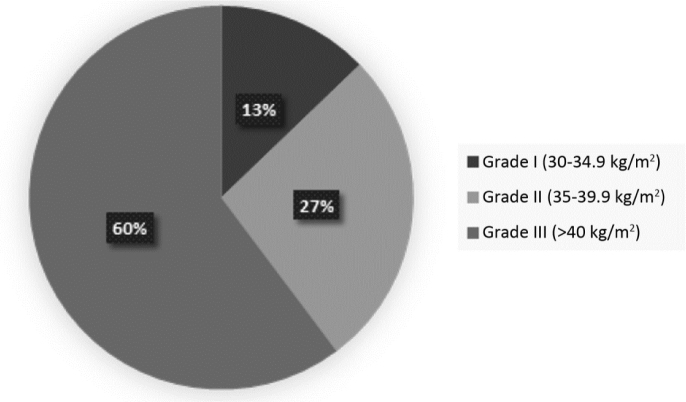
Seventy-nine patients (65.3%) met obesity criteria (BMI>30kg/m2), and that in 60% of cases was considered morbidly (BMI>40 kg/m2) (Figure 1).
Figure 1.
Distribution according to severity of obesity
Five patients had previous history of peptic ulcer disease (4.1%), and one patient had a history of gastric MALT lymphoma. No patient had a history of gastric adenocarcinoma, although 18.2% (22 patients) reported history of adenocarcinoma in first or second degree relatives. Twenty-five patients had a history of depression (20.7%), and eighteen patients reported anxiety disorder (14.9%). Twenty-one percent of patients presented with type II DM (in 88% of cases non-insulin dependent) and the same percentage were active smokers. The main concomitant medications included antihypertensive drugs (42.1%), oral antidiabetics (18.2%), and aspirin / non-steroidal anti-inflammatory drugs (9.1%).
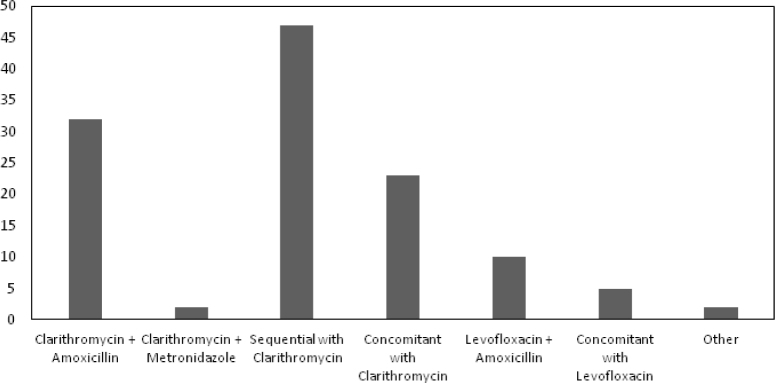
The overall eradication rate was 72.7%. The most widely used proton pump inhibitors included esomeprazole (37.2%), omeprazole (28.1%) and pantoprazole (27.3%). The most commonly used schemes were: sequential therapy with clarithromycin (39% of patients – eradication rate of 81%), triple therapy with clarithromycin (26% of patients – eradication rate of 75%) and concomitant with clarithromycin (19% of patients – eradication rate of 61%) (Figure 2). Levofloxacin-based therapies were used in 12.4%.
Figure 2.
Antibiotic schemes used for eradication
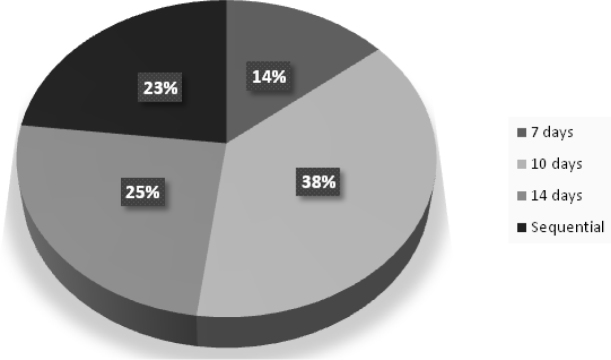
The duration of therapy was at least 10 days in 86% of cases (Figure 3).
Figure 3.
Duration of treatment
None of the analyzed variables, including the presence of obesity (71% vs. 76%, P = 0.553), body mass index, smoking (68% vs. 74%, P = 0.551), and diabetes (76% vs. 72%, P = 0.680), significantly influenced the rate of eradication, irrespective of the scheme used.
Discussion
As a tertiary care center, a significant percentage of respiratory test requests are made by the bariatric Surgery consultation, so the pool of patients with obesity and metabolic syndrome is considerable. This fact has given us the possibility to evaluate in a particular way if, in real life, the biotype of the patients influences the eradication capacity of H. pylori.
The impact of BMI on H. pylori. eradication is debatable. The role of the dose of PPIs has already been evaluated in reflux disease, without an increase in dose being justified because of the greater volume of distribution. Abdullahi et al.[6] compared 40 overweight/obese patients with 41 normal weight patients in a non-diabetic cohort and suggested that overweight/obese nondiabetic patients showed a significantly lower rate of eradication rate of H. pylori. infection than controls, and that BMI and corpus-predominant gastritis appear to be independent risk factors for eradication failure, concluding that alternative treatment regimens with higher dose and/or longer duration may be necessary in obese/overweight patients to achieve a higher eradication rate. However, in our cohort, it was not possible to find differences in eradication rates among the various subgroups according to the BMI, neither dividing patients as obese and non-obese (71 vs. 42 patients), regardless of the duration of treatment. Possibly the previously found effect is biased by the limited number of patients.
In 2006, Suzuki et al.[7] published a meta-analysis that provided information on eradication failure according to smoking status, and the pooled odds-ratio for eradication failure among smokers relative to nonsmokers was 1.95, which corresponded to a difference in eradication rate between smokers and nonsmokers of 8.4%. In our cohort, one in four patients was a smoker. However, there were no differences in eradication rates. This may be due to the limited number of smokers (25 out of 121 patients), but the high number of obese and overweight patients may have influenced these results.
Although a number of studies have been performed on the association of H. pylori and diabetes mellitus, the results have been controversial. In a large study performed by Xia et al.,[9] the seroprevalence of H. pylori infection was not statistically different in patients with diabetes mellitus and nondiabetic controls. However, Sargýn et al.,[8] comparing 40 diabetic patients and 40 non-diabetic dyspeptic patients treated on triple therapy for 10 days found an eradication rate 50% lesser in the diabetic group versus 85% in the non-diabetic control. They postulated that Immunosuppression in diabetes, as well as absorption problems (partly related to dysmotility), may influence eradication capacity in this population. This was not reinforced by our findings. In fact, the eradication rate was slightly better in the population with diabetes (76% vs. 72%), so it does not appear that this condition could influence the efficacy of the treatment. This cannot be explained by the duration of treatment, since in more than 80% of patients the treatment was also 10 days or more. It is also surprising that an eradication rate as low as 50% has been reported in this study.
In this cohort, eradication was lower than expected, which meets the latest evidence on the antimicrobial resistance. Patient’s biotype, smoking, diabetes and previous failure did not affect the results. These data support that previously published data on these factors in the eradication of H. pylori may not be as evident in a real life context, where the schemes used and duration of treatment vary significantly. This suggests that no benefit without altering the therapeutic approach in these populations, compared to what is actually recommended for the general population by the various societies of gastroenterology.
Footnotes
Conflict of Interest None declared.
References
- 1.Padol S, Yuan Y, Thabane M, Padol IT, Hunt RH.. The effect of CYP2C19 polymorphisms on H. pylori eradication rate in dual and triple first-line PPI therapies: a meta-analysis. Am J Gastroenterol. 2006;101:1467–75. doi: 10.1111/j.1572-0241.2006.00717.x. [DOI] [PubMed] [Google Scholar]
- 2.Furuta T, Sugimoto M, Shirai N, Matsushita F, Nakajima H, Kumagai J. et al. Effect of MDR1 C3435T polymorphism on cure rates of Helicobacter pylori infection by triple therapy with lansoprazole, amoxicillin and clarithromycin in relation to CYP 2C19 genotypes and 23S rRNA genotypes of H. pylori Aliment Pharmacol Ther. 2007;26:693–703. doi: 10.1111/j.1365-2036.2007.03408.x. [DOI] [PubMed] [Google Scholar]
- 3.Hwang IR, Kodama T, Kikuchi S, Sakai K, Peterson LE, Graham DY. et al. Effect of interleukin 1 polymorphisms on gastric mucosal interleukin-1beta production in Helicobacter pylori infection. Gastroenterology. 2002;123:1793–803. doi: 10.1053/gast.2002.37043. [DOI] [PubMed] [Google Scholar]
- 4.O’Connor JP, Taneike I, O’Morain C.. Improving compliance with Helicobacter pylori eradication therapy: when and how? Therap Adv Gastroenterol. 2009;2:273–9. doi: 10.1177/1756283X09337342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Labenz J, Stolte M, Blum AL, Jorias I, Leverkus F, Sollböhmer M. et al. Intragastric acidity as a predictor of the success of Helicobacter pylori eradication: a study in peptic ulcer patients with omeprazole and amoxicillin. Gut. 1995;37:39–43. doi: 10.1136/gut.37.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdullahi M, Annibale B, Capoccia D, Tari R, Lahner E, Osborn J. et al. The eradication of Helicobacter pylori is affected by body mass index (BMI) Obes Surg. 2008;18:1450–4. doi: 10.1007/s11695-008-9477-z. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki T, Matsuo K, Ito H, Sawaki A, Hirose K, Wakai K. et al. Smoking increases the treatment failure for Helicobacter pylori eradication. Am J Med. 2006;119:217–24. doi: 10.1016/j.amjmed.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Sargýn M, Uygur-Bayramicli O, Sargýn H, Orbay E, Yavuzer D, Yayla A.. Type 2 diabetes mellitus affects eradication rate of Helicobacter pylori World. J Gastroenterol. 2003;9:1126–8. doi: 10.3748/wjg.v9.i5.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia HH, Talley NJ, Kam EP, Young LJ, Hammer J, Horowitz M.. Helicobacter pylori infection is not associated with diabetes mellitus, nor with upper gastrointestinal symptoms in diabetes mellitus. Am J Gastroenterol. 2001;96:1039–46. doi: 10.1111/j.1572-0241.2001.03604.x. [DOI] [PubMed] [Google Scholar]