Abstract
Objective
Healthy lifestyle interventions addressing obesity in people with serious mental illness (SMI) lead to modest weight losses that tend not to be sustained over time. By augmenting lifestyle interventions with family and peer support targeting health behavior change, greater weight loss might be obtained and sustained in this population. The purpose of this study was to assess the feasibility of increasing support from family and friends to enhance a healthy lifestyle intervention (In SHAPE) adapted for individuals with SMI.
Method
A sample of 7 dyads (14 total participants) participated in this small-scale open-feasibility trial of social support strategies to enhance health promotion. Weekly 1-hour health coaching sessions were augmented by sessions designed to increase support for healthy eating and exercise through active learning and didactic instruction. Feasibility was assessed by program participation and by examining participants’ satisfaction and exploring suggestions for improving the model post-intervention.
Results
The majority of participants (57%) nominated a friend, followed by adult child-parent pairs (28%) and sibling pairs (14%) to participate as support partners in the study. All participant-partner dyads (100%) completed 12 sessions within 16 weeks. Participants reported high satisfaction and perceived benefits from the program. Recommend modifications by the dyads included more interactive sessions, a combination of group and dyadic sessions, and hands-on cooking classes.
Conclusions
This formative research showed that the study design is feasible and that the intervention can facilitate social support for health behavior change in people with SMI. Further research is needed to evaluate the effectiveness of this intervention.
Keywords: mental disorders, social support, weight loss, sedentary lifestyles, exercise
The life expectancy of people with serious mental illness (SMI), including schizophrenia, schizoaffective disorder, major depression, and bipolar disorder, is 10 to 25 years less than that of the general population (Colton & Manderscheid, 2006; Walker, McGee, & Druss, 2015). The primary cause of this early mortality is cardiovascular disease associated with obesity and smoking (Druss, Zhao, Von Esenwein, Morrato, & Marcus, 2011). People with SMI experience rates of obesity nearly double the observed rates within the general population (Scott & Happell, 2011). Although antipsychotic medications contribute to weight gain (Manu et al., 2015), lifestyle behaviors such as diet and exercise are a major cause of obesity in this population and can be modified to improve health (Laursen, Nordentoft, & Mortensen, 2014). Effective interventions are needed to help adults with SMI make health behavior changes needed to achieve and maintain weight loss.
Studies of lifestyle interventions have emerged over the past decade that specifically target weight loss in people with SMI. For instance, the In SHAPE healthy lifestyle intervention is tailored for individuals with SMI and has been studied in two separate randomized controlled trials (RCTs; Bartels et al., 2013; Bartels et al., 2015). In both studies, In SHAPE achieved reduced cardiovascular risk in approximately half of participants with SMI, defined as either ≥5% weight loss or clinically significant increase in walking distance. Other researchers have reported similarly successful results from studies of group-based models of behavioral weight management for individuals with SMI (Daumit et al., 2013; Green et al., 2015). Despite the promise of these lifestyle interventions, many are resource intensive and time limited, with only limited evidence supporting the long-term maintenance of health benefits. Helping individuals with SMI make lasting lifestyle changes to address obesity might require professional facilitation of social support in home and social environments where health behaviors take place.
One potentially important but neglected resource for enhancing lifestyle interventions in the SMI population is the person’s natural support system. The influence of social networks on health behaviors and health outcomes has been well established in general populations (Christakis & Fowler, 2013; Leahey, Gokee La-Rose, Fava, & Wing, 2011). However, lifestyle interventions targeting people with SMI have focused almost exclusively on the individual, with little attention paid to the larger social context in which eating and exercise behaviors occur. Behavioral weight loss interventions for the general population have targeted participants’ family members and friends as facilitators of weight loss. This approach encourages partners to make the same dietary and physical activity changes as the primary participant to promote initial and long-term weight loss. RCTs in general populations have demonstrated that enhancing behavioral weight loss treatment by enrolling family and friends results in greater weight losses for participants, with the added benefit of weight loss by the support partners (Gorin et al., 2013; Sorkin et al., 2014; Wing & Jeffery, 1999).
Family psychoeducation interventions that provide families with information and skills training for coping with a relative’s mental illness have consistently been shown to reduce symptom levels in individuals with SMI (Dixon et al., 2001; Mueser, Deavers, Penn, & Cassisi, 2013). Despite strong evidence supporting the effectiveness of family psychoeducation programs as an adjunct to medication management for individuals with SMI (Lyman et al., 2014), research involving family members and friends in health promotion for this population remains scarce. Family members and friends could conceivably help individuals with SMI apply what they learn about dietary change and exercise from lifestyle interventions to making lasting health behavior changes in their home and social environments.
Individuals with SMI often have small social networks characterized by limited contact with social ties, such as family members and friends (Lee, Wong, & Rothbard, 2014; Thorup et al., 2006). Therefore, an important first step in exploring the feasibility of a partner support intervention for health behavior change among individuals with SMI is to assess the views of participants and providers on the potential of engaging family and significant others in an intervention to support health goals. Previously, we conducted research with participants and health coaches in the In SHAPE healthy lifestyle intervention for individuals with SMI to explore their perspectives on the potential advantages and challenges of involving family members and friends in a healthy lifestyle intervention. Participants viewed emotional support (e.g., encouragement, praise, recognition) and practical help (e.g., transportation) for health behavior change as potential benefits of involving family members and friends in a lifestyle intervention along with the potential to enhance the quality of these relationships (Aschbrenner et al., 2012). In contrast to the common perception that persons with SMI have minimal contact with friends and family, the majority (80%) of participants enrolled in In SHAPE reported regular contact with a close family member or friend who influenced their health goals (Aschbrenner, Mueser, Pratt, & Bartels, 2013). Despite the availability of potential support partners and the perceived benefits of their involvement, health coaches rarely interacted with participants’ family members or significant others (Aschbrenner et al., 2015).
The purpose of the present study was to conduct initial feasibility testing of an intervention designed to engage and facilitate social support from a partner (i.e., family member or friend) for dietary changes and exercise among individuals with SMI currently enrolled in a lifestyle intervention. Participants enrolled in the In SHAPE healthy lifestyle program were invited to participate with a self-selected support partner in a 12-week added component—Fit Together—designed to facilitate social support for the participant’s In SHAPE fitness and weight loss goals. Feasibility of the Fit Together model was assessed by examining participant–partner recruitment and attendance rates, as well as participant–partner satisfaction and suggestions for improving the model. This preliminary feasibility study will be used to inform a larger pilot study to test the potential effectiveness of the Fit Together intervention on changes in health behaviors and weight loss.
Method
Participants
Participants were recruited for the Fit Together study from two New Hampshire community mental health centers (CMHCs) from August 2013 to January 2014. In addition to being an active participant in the In SHAPE program, eligibility criteria included being 18 years old or older; having a serious mental illness, defined as an Axis I diagnosis of major depression, bipolar disorder, schizoaffective disorder, or schizophrenia; having a body mass index (BMI) of 25 or greater; and having a family member, friend, or significant other (e.g., boyfriend or girlfriend) willing to participate in the Fit Together study as a support partner. In SHAPE participants were excluded from participation in the Fit Together study if they reported being unable to walk a city block without stopping; were either currently pregnant or planned to become pregnant within 6 months; had a significant cognitive impairment, defined as a score less than 24 on the Mini-Mental State Examination; or had a terminal illness with mortality expected within 1 year. Support partners had to be 18 years old or older and have at least weekly in-person contact with the In SHAPE participant; no BMI criteria were established for the support partners.
Procedures
Our target enrollment was eight dyads (i.e., In SHAPE “primary” participants and support partners), for a total of 16 participants. Recruitment began with referrals from the In SHAPE health coaches. The health coaches were asked to identify participants who had been in the In SHAPE program for at least 3 months and who might benefit from receiving additional support from family and friends for their health goals. The coaches provided the research team with the names of interested, potentially eligible participants. Research staff met with potential participants to provide details about the study and assess their eligibility. Interested and eligible participants were invited to nominate a family member, friend, or significant other as their support partner. The research staff then contacted the persons nominated as support partners to ascertain their interest in participating in the study. Eligible pairs were invited to attend an orientation session, during which the study was described in detail and informed consent was obtained from both members of the dyad. This research was approved by the Institutional Review Board of a university in the Northeastern United States.
A total of 16 In SHAPE participants were referred to the pilot study from the health coaches. Two participants were unable to be reached after initial contact and one participant had medical complications preventing participation. Among the remaining participants, one participant separated from her partner before the intervention started, two people had partners who could not participate because of scheduling conflicts, one person had a partner who did not meet the age criterion for participation, and two participants had partners who were not interested in participating. Of the 12 In SHAPE participants who were eligible for the Fit Together study, seven (58%) had partners who were willing and able to participate in the study.
Seven dyads (i.e., primary participant and support partner) were enrolled in an open-trial feasibility study of the Fit Together program. Primary participants received $20 for completing a 2-hour baseline assessment, and their support partners received $10 for completing a 45-minute baseline assessment. Primary participants received $30 and support partners received $20 for completing a post-intervention assessment, and both dyad members received $20 for completing an in-depth qualitative interview following the intervention. The primary purpose of conducting pre/post quantitative interviews was to test the feasibility of a full-length assessment battery proposed for a larger pilot trial of the intervention. The present study assessed feasibility through the participant satisfaction data collected at the post-assessment and the qualitative data collected during in-depth interviews following the intervention. Follow-up assessments were conducted by trained research interviewers who were not involved in delivering the intervention to the participants they interviewed.
Intervention
Fit Together was designed to augment the In SHAPE healthy lifestyle intervention for individuals with SMI by increasing support from participants’ family members and significant others for the participants’ fitness and weight-loss goals set in the In SHAPE program. In SHAPE is a fitness intervention embedded within community mental health centers that consists of weekly 1-hour sessions with a certified personal fitness trainer (i.e., health coach) and instruction on healthy eating and nutrition (Bartels et al., 2015). The In SHAPE model is based on principles of social inclusion and recovery, with participants actively involved in setting their health goals and building an active life in their own communities, which in turn, is expected to lead to better health. The In SHAPE health coach works with each participant to develop personalized lifestyle and fitness evaluations, and meets weekly with participants for 1-hour sessions at a local gym (e.g., YMCA). During the gym sessions, the health coach provides supported fitness coaching and individualized attention to the participant’s nutrition goals and objectives. The coaches also provide participants with support for managing mental health symptoms that interfere with exercise and healthy eating.
The In SHAPE program does not have a protocol for engaging family members, friends, or significant others from the participant’s natural environments to support health behavior changes. Helping participants translate lessons learned during individual coaching sessions at a fitness facility to their home and social environments might be critical for long-term weight loss success. Fit Together was designed to augment the In SHAPE one-on-one health coach model with a complementary component designed to facilitate support from friends and family for participants’ goals for dietary changes and exercise goals to promote greater initial weight loss and long-term maintenance of weight loss.
The development of the Fit Together intervention was informed by the social ecological model and social support theories of health promotion. The social ecological model is a comprehensive public health approach that recognizes multiple levels of influence on individual health behaviors, including societal, community, and interpersonal levels (Breslow, 1996; Stokols, 2000). According to the model, a person’s closest social circle—peers, family members, and significant others—has the most immediate influence on eating behaviors and physical activity. Social support theories suggest the quality and function of these relationships can have a significant effect on perceived social support (Berkman, 1995). Thus, mobilizing support from existing social networks might require training social network members with the social, behavioral, and communication skills needed to provide effective support for health behavior change (Heaney & Israel, 2008).
The 12-session Fit Together intervention used didactic instruction and experiential learning activities with the dyads to increase social support for healthy eating and exercise (see Table 1). The Fit Together intervention ran concurrently with the In SHAPE intervention, and consisted of weekly 1-hour sessions with a Fit Together partner support coach who reinforced and facilitated partner support for the fitness and weight loss goals that participants set in the In SHAPE intervention. The In SHAPE coach referred clients to the Fit Together program and was informed of their progress through informal discussions with the Fit Together coach throughout the program.
Table 1.
Overview of the Fit Together Intervention Curriculum for Dyad Participants
| Session | Session content |
|---|---|
| 1 | Striving for a healthy lifestyle
|
| 2 | Basics of physical activity and exercise
|
| 3 | Health goals: Setting yourself up for success
|
| 4 | Fit Together social support plan
|
| 5 | Getting Fit Together
|
| 6 | Exercising together
|
| 7 | Basics of healthy eating
|
| 8 | Healthy eating goals and partner support
|
| 9 | Understanding food labels and portion sizes
|
| 10 | Making healthy choices when eating out
|
| 11 | Problem solving for healthy eating and exercising
|
| 12 | Progress review and next steps
|
The Fit Together intervention was delivered by two master’s-level trained social workers with prior research experience in health promotion for individuals with SMI. Coaches for the Fit Together program participated in a 2-day In SHAPE training, during which they received instruction on healthy eating and nutrition and were trained in motivational interviewing and tailoring wellness plans to the needs of persons with SMI. In addition, Fit Together coaches received a half-day training on the principles of family behavioral therapy, including dyadic communication skills training. Throughout the study, Fit Together coaches participated in required weekly supervision consisting of a 60-minute call with a study co-investigator who was a clinical psychologist with expertise in behavioral family therapy and behavior change. All cases were reviewed during these supervision calls.
Figure 1 depicts the overarching logic model for the Fit Together intervention. In this model, three core components—health promotion education, tailored social support planning, and dyadic communication skills training—are expected to affect proximal outcomes of social support, self-efficacy, and weight-loss behavior stage of change, which in turn, will have an effect on physical activity and dietary behaviors, and thus ultimately influence weight loss and fitness outcomes.
Figure 1.
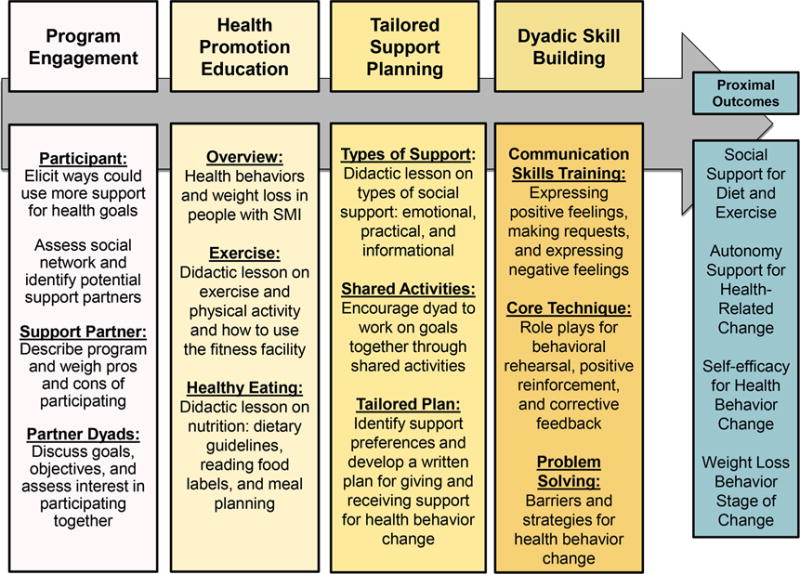
Logic model of Fit Together intervention
To encourage collaboration between the primary participants and their respective support partners, the Fit Together coach provided the dyads with instruction in communication skills with the aim of increasing positive support and effective problem-solving strategies for health behavior change. Participants and their support partners also received gym memberships and wearable physical activity tracking devices (Fitbits) to promote self-monitoring and shared physical activity. The Fitbit Zip is an accelerometer, comparable in size to a pedometer, worn by clipping the device to clothing or carrying it in a pocket. The Fitbit Zip tracks steps, distance, and calories burned.
Health Promotion Education
During the initial sessions, the Fit Together coach addressed common myths and assumptions about health behavior change in individuals with SMI by presenting evidence-based strategies for weight management specifically tailored to the SMI population. The Fit Together coach described the overall goals and activities of the In SHAPE program and encouraged the primary participants to share the specific nutrition and exercise goals they had set as part of the In SHAPE program. In addition, the coach elicited participants’ stories of success they experienced in the In SHAPE program as well as areas in which they continued to struggle but wanted to make a change. The coach then invited the support partners to share health goals they wanted to address in the Fit Together program. Last, the coach provided the dyads with basic health promotion education to increase the participants’ knowledge and awareness of the benefits of healthy eating and physical activity. These initial sessions established the foundation for subsequent sessions designed to identify strategies for increasing social support and targeting health behavior change.
Tailored Social Support Strategies
The Fit Together coach guided the dyads to identify support strategies targeting health behavior change (e.g., reminders and cues, praise and recognition, transportation to gym or grocery store) based on their own needs, values, and preferences. The coach and each dyad worked as a team to develop a behaviorally specific personalized plan for supporting the participant’s health goals. This process included identifying the type of support the participant desired and then determining when and how often the partner would provide support. The Fit Together coach encouraged the dyad to collaborate in selecting mutual health goals to work on together. Participants and support partners were encouraged to check in with each other throughout the week and plan ways they could engage in healthy activities together, such as preparing healthy meals or going to the gym together. The support plans were reviewed at the beginning of each session and adjustments or new plans were made on a weekly basis.
Communication Skills Training
The Fit Together intervention incorporated communication-skills training based on the principles and techniques of social-skills training with families and couples coping with mental illness (Mueser & Glynn, 1999; Mueser, Glynn, & Liberman, 1994). Key behavioral techniques, including role modeling, behavioral rehearsal, positive reinforcement, and home assignments were used to teach both members of the dyad to communicate their emotions and needs more effectively to one another in order to receive and provide support for health goals. Participants were taught more effective ways to express positive feelings (e.g., recognizing success, expressing gratitude), make requests (e.g., going to the gym together, helping with transportation), and express negative feelings (e.g., feeling disappointed) related to health behavior changes. Communication-skills training was integrated throughout the program and was reinforced through home assignments that encouraged participant dyads to practice skills when and where these skills could be most helpful in their daily environments.
Study Design
We used an interventional mixed-methods study design that incorporated quantitative assessments and in-depth interviews to assess program feasibility (Fetters, Curry, & Creswell, 2013). Using multiple methods allows for a more complete and thorough understanding of feasibility issues in the target population (Eyles et al., 2014; Smith et al., 2014). Our assessment of the feasibility of implementing the intervention included participation and perceived benefit and satisfaction with the program from the perspective of primary participants and their selected support partners.
Study Measures
Quantitative measures of feasibility included program attendance and participant and partner satisfaction. Fit Together coaches tracked attendance at each of the 12 sessions for both participants and their partners and submitted weekly attendance reports to the study coordinator. Participant and partner satisfaction with the program was assessed using a participant satisfaction questionnaire adapted from a prior feasibility study of a psychosocial intervention for individuals with SMI (Meyer, Johnson, Parks, Iwanski, & Penn, 2012), which was designed to measure satisfaction, usefulness, ease of use, and ease of learning. Participants responded to eight questions that asked for ratings of their level of satisfaction with various components of the program. Example items included, “How useful was the written plan for social support?” and “How helpful did you find the role-play practice?” All responses used the same 3-point Likert rating scale ranging from not at all satisfied (coded 1) to very satisfied (coded 3).
Qualitative Interviews
We conducted in-depth qualitative interviews with participants and their support partners using a semistructured interview guide with questions targeting the dyad’s satisfaction with the program; perceived benefits of specific intervention components (i.e., tailored social support planning, fitness facility membership, and wearable physical activity tracking devices); overall program experiences; dyadic relational experiences; and recommended program modifications. The dyad members participated in separate 1-hour qualitative interviews conducted in person by research interviewers who were trained and supervised by the study’s principal investigator, who is an experienced qualitative researcher. The researchers who conducted the qualitative interviews were not involved in delivering the interventions to the participants they interviewed. All interviews were audiotaped and transcribed verbatim.
Data Analysis
We used descriptive statistics, including means and frequencies, to summarize participant satisfaction ratings and performed statistical analyses using SPSS software, version 20.0. The methodology for the qualitative assessment involved a rapid assessment process described by Beebe (2001) as targeted qualitative inquiry using iterative data analysis. Each transcript was reviewed independently by two members of the research team using a template that identified key domains from the qualitative interview guide. The researchers summarized key findings within each domain by each type of respondent and across respondents. We then created a matrix of key findings by respondent and domain that enabled us to synthesize important findings by noting similarities, differences, and trends across respondents. This technique is particularly useful when there is a pragmatic need for qualitative data, as is often the case with formative research used to develop and refine an intervention (Solomon, 2007).
Results
The background characteristics of participants and their support partners are presented in Tables 2a and 2b. The average age of the primary participants was 43.3 years (SD = 13.7), the majority were females (71%), and all were White. At the time of the study, none of the primary participants were married, with the majority reporting they had never been married (57%) and the others were either separated or divorced. The majority of primary participants were living with family (71%). The primary participants had a mean BMI of 41.4kg/m2 (SD = 11.4), which is considered Class III obesity with an extremely high disease risk relative to normal weight and waist circumference.
Table 2a.
Characteristics of Primary Participants (n = 7)
| Age (M ± SD) | 43.3 ± 13.7 |
|
| |
| Weight (M ± SD) | 259.3 ± 61.1 |
|
| |
| Body mass index (M ± SD) | 41.4 ± 11.4 |
|
| |
|
% (n)
|
|
| Gender (female) | 71 (5) |
|
| |
| Race (White) | 100 (7) |
|
| |
| Psychiatric diagnosis | |
|
| |
| Schizophrenia | 14.3 (1) |
|
| |
| Schizoaffective disorder | 28.6 (2) |
|
| |
| Major depression | 28.6 (2) |
|
| |
| Bipolar disorder | 14.3 (1) |
|
| |
| Psychosis NOS | 14.3 (1) |
|
| |
| Educational level | |
|
| |
| High school graduate/GED | 42.9 (3) |
|
| |
| Some college | 42.9 (3) |
|
| |
| College graduate | 14.3 (1) |
|
| |
| Marital status | |
|
| |
| Never married | 57.1 (4) |
|
| |
| Married | 0 (0) |
|
| |
| Divorced/separated | 42.9 (3) |
|
| |
| Current living status | |
|
| |
| Living independently | 28.6 (2) |
|
| |
| Living with family | 71.4 (5) |
Note. NOS = not otherwise specified. GED = General Educational Development certificate.
Table 2b.
Characteristics of Support Partners (n = 7)
| Age (M ± SD) | 52.9 ± 13.9 |
|
| |
| White | 100 (7) |
|
| |
| Gender (female) | 86 (6)
|
| % (n) | |
|
| |
| Relationship to participant | |
|
| |
| Parent | 14.3 (1) |
|
| |
| Child | 14.3 (1) |
|
| |
| Sibling | 14.3 (1) |
|
| |
| Friend | 57.1 (4) |
|
| |
| Length of relationship with dyad partner | |
|
| |
| 2–4 years | 14.2 (1) |
|
| |
| 10 or more years | 42.9 (3) |
|
| |
| Lifetime | 42.9 (3) |
|
| |
| Currently lives with dyad partner | 42.9 (3) |
|
| |
| Amount of contact with dyad partner | |
|
| |
| Nearly every day | 42.9 (3) |
|
| |
| 2–3 times per week | 42.9 (3) |
|
| |
| 2–3 times per month | 14.2 (1) |
More than half of the sample of support partners was composed of friends (58%), followed by parents (paired with their adult child; 28%), and siblings (14%). In 83% of cases, the first potential support partner identified by the participant agreed to participate in the study. Support partners were older than primary participants, with an average age of 52.9 years (SD = 13.9). The majority of the support partners were female (86%). Most of the support partners (85.8%) reported knowing the primary participants for 10 or more years, and most support partners had in-person contact with participants at least two or three times per week (85.8%). Fewer than half of the dyads lived together at the time of the study (42.9%). Each of the dyads (100%) completed all 12 Fit Together sessions within a 16-week period.
Participant-Dyad Satisfaction
Overall, both the primary participants and their support partners appraised Fit Together positively and both reported that the program was useful, convenient, and helped them reach their goals (see Table 3). In addition, all of the support partners reported that the program helped them with their own health goals. The majority of primary participants reported that the role-play practices were very helpful (83.3%) whereas 42.9% of support partners reported that the role-plays were very helpful. All of the participants and support partners indicated that they were very likely to recommend the program to someone else.
Table 3.
Participant and Partner Satisfaction With the Fit Together Program (N = 14)
| Item | Not at All | Somewhat | Very | |||
|---|---|---|---|---|---|---|
| PPT | Partner | PPT | Partner | PPT | Partner | |
| % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | |
| Did the program help you with your goals? | 0 (0) | 0 (0) | 14.3 (1) | 42.9 (3) | 85.7 (6) | 57.1 (4) |
| How easy was it for you to understand the materials? | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 100 (7) | 100 (7) |
| How useful was the written plan for social support? | 0 (0) | 0 (0) | 0 (0) | 42.9 (3) | 100 (7) | 57.1 (4) |
| How helpful did you find the role-play practice? | 0 (0) | 0 (0) | 16.7 (1) | 57.1 (4) | 83.3 (5) | 42.9 (3) |
| How helpful was the Fitbit for tracking your physical activity? | 14.3 (1) | 14.3 (1) | 0 (0) | 0 (0) | 85.7 (6) | 85.7 (6) |
| How convenient was it for you to participate in the program? | 0 (0) | 0 (0) | 14.3 (1) | 14.3 (1) | 85.7 (6) | 85.7 (6) |
| Overall, how satisfied are you with the program? | 0 (0) | 0 (0) | 14.3 (1) | 14.3 (1) | 85.7 (6) | 85.7 (6) |
| How likely is it that you will recommend this program to others? | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 100 (7) | 100 (7) |
Note. PPT = primary participant
Intervention Content
Overall program
Primary participants reported that Fit Together increased the support and encouragement they received from their partner for the goals they had set in the In SHAPE program; in general, support partners felt they had learned more effective ways to support participants. One participant said, “I thought it was great, I really liked it. I got a lot of encouragement from my mom, she helped to keep me on the right track with my goals every week.” One support partner commented, “I was surprised when my sister asked me about doing it. We had fun. We kind of grew closer together and I think she enjoyed me going with her to the gym instead of just doing it by herself.”
Fit Together support plan
Both primary participants and their support partners noted the benefits of the Fit Together written plan for providing support for the dietary changes and exercise goals the participant had set in the In SHAPE program. Participants reported that developing a written support plan assured them that their partner was committed to supporting their health goals. As one participant noted, “I liked it [written plan], because it gave you an idea of how long it would take to achieve the goal and how I would do it and how I could get help from my partner.” Support partners reported feeling the written plan made it more acceptable to give suggestions and advice to their partner: “With the program I felt I had the right to motivate and push her. In the past I have tried to give her advice and she has never accepted it.”
Support received and provided
Participants and support partners reported helping each other to make positive dietary changes while in the program. One support partner said, “She helped me eat healthier, like on Thursdays, I go with my case manager to Dunkin Donuts and I would probably get unhealthy stuff, so she reminds me to get healthier stuff to eat.”
Making healthy changes together was a common theme among participant-partner dyads. Several support partners commented that they became motivated to work on their own health goals in the Fit Together program. One support partner explained, “I exercised a lot more. We were trying to exercise together three times a week compared to once a week.” Some partners focused on helping the participant make positive dietary changes while they continued to struggle with their own health behaviors: “I learned new ways to support her but I don’t know if it helped me. A lot of things I know I am doing wrong. I eat out too much. That is my downfall.”
Fitness memberships
Participants and their support partners reported that access to the fitness facility was one of the most appealing aspects of the Fit Together program. As one participant explained, “I joined the program because there was a possibility that my sister could come to the gym with me.” Another participant commented, “It kind of helped because it got me more motivated and helped me get in the flow of working out more and more.” One support partner described how she relied on the participant’s help to go to the gym: “To get me into a gym is hard, but we went. If I call her, she picks me up at 7:00 in the morning and we go to the gym.” Two participants reported challenges with the “availability” and “ability” of support partners to exercise with them, which they described as “disappointing.” Both participants wondered if they had made the right choice in a support partner for the program.
Fitbit activity tracker
The wearable physical activity trackers (Fitbits) were a motivator for participants and their partners to increase their physical activity, even among those who were not able to work out together. Overall, participants reported high satisfaction with using the activity tracking devices, stating the devices were easy to use, motivational, and helpful for setting and monitoring goals. In many cases, participants reported a friendly competition with their partner for increasing daily steps. One participant commented, “We were competing against each other because we had the Fitbit. It was fun. I would do it again.”
Quality of relationships
Participants and their support partners reported benefits in the quality of their relationships as a result of the program. Participants attributed the improved relationship to spending more time together and learning more about their partner’s experiences and perspectives on health behavior change. One participant commented, “We are both starting to eat healthier and take better care of ourselves. We got closer, it seems like we have the same goals, to lose weight and eat healthier.” Support partners also reported improvements in the quality of their relationship with participants. One support partner commented, “I think it brought us together—when you are with somebody and you are exercising, you can talk more and get whatever is off our chest, so I think it worked.” Participants and their support partners reported communicating more effectively with their partner as a result of the program, which might have contributed to more positive relationships: “We communicated better; more for portion sizes of food, more vegetables. As far as exercise or losing a bit more weight, she gave me a lot of positive appraisals.”
Recommendations
Interactive learning activities
The Fit Together intervention primarily involved didactic health promotion education and instruction. Both participants and support partners expressed a desire for more interactive activities to help them acquire new skills for behavior change (i.e., not just education). Several participants and their partners explained that although they had prior knowledge of basic nutrition and principles of exercise, what they most needed was help with taking action to change their behaviors. As one participant commented, “The reading material was the only part I didn’t like but at the same time [the materials] were good because they helped encourage me to eat the right stuff and keep going to the gym and trying to eat more vegetables and fruits.” His partner shared this sentiment: “It is probably because I am an old lady and I have diabetes and have been to so many nutrition classes because of other stuff, and my son has too, so some of the things were too easy.”
Individual and group sessions
Many participants and their partners expressed a desire for a combination of individual and group-based Fit Together sessions. Specifically, they wanted an opportunity to meet and potentially give and receive support to other participant-partner dyads in the program. As support partner explained, “If we met together as a group once a week and discussed what we liked and what was easier, maybe that would bring us together with the other people in the program to share helpful cooking or exercise tips.”
Cooking classes
Participants and their partners recommended group-based cooking classes as a fun and interactive way to teach cooking skills and increase self-efficacy in preparing healthy meals. Several participants and their partners explained that they had never learned to prepare and cook healthy meals. As one support partner commented, “Me and my sister do not know how to cook and my mom didn’t cook that much when she was younger, so maybe more cooking experiences and recipes. We know how to cook the basics but not the healthier way.”
Discussion
We evaluated the initial feasibility of a social support component (Fit Together) designed to augment the In SHAPE healthy lifestyle intervention for individuals with SMI with increased support from family and friends targeting health behavior change. Our results indicate that the Fit Together intervention was feasible to implement. All dyads (100%) completed the 12-session program within 16 weeks. Participants reported high satisfaction and perceived benefits from the program. Recommended modifications include more interactive sessions, a combination of group and dyadic sessions, and hands-on cooking classes. These recommendations for improving the model will help refine the intervention prior to a larger pilot study evaluating its potential effectiveness.
For this small-scale study, our target for enrollment was eight dyads, with each composed of an In SHAPE participant and a support partner (16 people total). Of the 12 participants who were eligible for the Fit Together intervention, 58% (n = 7) had a support partner who was willing and able to participate in the study. In a majority of cases, the first invited support partner agreed to participate in the Fit Together intervention. Almost all of the participants had contact with their support partners at least two or three times per week and most had known their partners at least 10 years. Most dyads were composed of friends (58%), with smaller numbers of adult child–parent pairs (28%) and sibling pairs (14%). These findings support the initial feasibility of recruiting and retaining participants and their natural supports for a multisession program to increase support for health behavior change among overweight and obese individuals with SMI.
The focus of the Fit Together intervention was on teaching partners to support the primary participant’s fitness and weight loss goals; however, the program also offered support for the partner’s health goals, and many dyads chose to work on similar health goals. Unlike recent studies of increasing social support for weight loss in general populations (Gorin et al., 2013; Sorkin et al., 2014), we did not require support partners to meet an overweight or obese BMI classification or have an interest in losing weight or improving fitness themselves. Because individuals with SMI often have small social networks (Davis & Brekke, 2013), we did not want to limit the potential pool of support partners by requiring them to share the participant’s health and wellness goals. However, several participant dyads in this study described how they supported each other’s health goals (e.g., healthy cooking together, reminder calls for appointments, and transportation to the gym) and reported that working on health goals together improved the quality of their relationship. Focusing on dyadic collaboration in health behavior change has the potential to foster significant changes in lifestyle behaviors and could be an effective strategy to promote long-term change.
Participants and support partners recommended adding more interactive and collaborative material to increase engagement in health promotion sessions. The Fit Together coaching sessions primarily involved didactic education and instruction, similar to the structure of numerous evidence-based behavioral weight management programs (Kramer et al., 2009; Wing et al., 2014) and family psychoeducation programs for individuals with SMI (Dixon et al., 2001). We incorporated active learning activities to help participants “learn by doing” and reflect on their experiences; however, participant dyad feedback indicated there was not enough interaction during sessions. Health promotion education alone does not generally lead to the adoption of recommended health behaviors. A variety of other factors play an important role in eating and exercise behavior change, including personal attitudes and beliefs, self-regulation skills and abilities, and social facilitation (Ryan, 2009). Didactic education might not be an optimal approach to addressing factors other than knowledge that influence decisions regarding healthful behaviors. Future research should strive for a balance between didactic instruction to teach essential health information and active, collaborative learning strategies to promote social interaction skills and to apply the content to real life situations. Collaborative learning concepts from the field of education (Cortright, Collins, & DiCarlo, 2005; Fagen, Crouch, & Mazur, 2002) have the potential to guide novel approaches to developing health promotion curriculum that engages dyads through participatory experiences. Coaching sessions that involve a high degree of active participation to teach core concepts could enable members to clarify their own understanding, build upon each other’s contributions, search out meanings, and ask and answer questions, while strengthening social connections and relying less on expert instruction. Future research should incorporate these concepts to help participant-dyads strengthen positive social support relationships targeting health behavior change.
Several dyads recommended restructuring the program to include a combination of dyadic and group sessions to provide an opportunity to meet other participants in the program. Individuals with SMI and their families often benefit from group-based interventions where they can learn from similar others and share coping strategies (Dixon et al., 2001; McFarlane, 1994). Individuals with SMI and their natural supports might also benefit from opportunities to interact with other participants and their partners facing similar challenges with respect to health behavior change. A large body of research exists on family-based group nutrition interventions for addressing obesity in youth (Epstein, Kilanowski, Paluch, Raynor, & Daniel, 2015; Wilfley et al., 2007), and group weight loss nutrition interventions have been evaluated in a variety of adult patient populations (Subak et al., 2009; Wing et al., 2014). A group-based nutrition component could provide an opportunity for participants to develop supportive connections and broaden their social networks while learning practical skills for preparing and cooking nutritious meals together.
Limitations
The current study has several limitations. First, the sample was small, involving only volunteers who were self-selected, and the study was implemented with an uncontrolled study design consistent with the intent of a pilot feasibility study (Leon, Davis, & Kraemer, 2011). The primary purpose of this study was to understand the user’s experience with the intervention to identify areas for future refinement. Future studies with a larger sample size are needed to evaluate the potential effectiveness of social support interventions in improving health outcomes for persons with SMI.
Second, just over half of those eligible for the intervention (58%) consented with their partner to participate, perhaps limiting the generalizability of findings. It is noteworthy that none of the participants were married; therefore we cannot comment on spousal support in health behavior change for this population. In addition, the majority of the dyads did not live together. The effect of social supports might even be greater when partners share a living environment.
Third, the study measures were based on self-report. We used a participant satisfaction questionnaire and in-depth qualitative interviews to assess the feasibility of the intervention. Participants might have been inclined to respond more favorably because of social desirability or demand effects. Future studies should consider semistructured interviews to measure perceived changes in social support as well as objective measures of dyadic communication skills.
Fourth, a structured protocol was not used to assess the fidelity of delivering the intervention. Instead, Fit Together coaches participated in a required 60-minute supervision call each week with the study co-investigator (a clinical psychologist with expertise in behavioral family therapy and behavior change). All cases were reviewed during these supervision calls. Future studies of the intervention should involve formal fidelity assessments with observations and objective ratings of fidelity.
Finally, the participants were representative of the regional population in New Hampshire, and thus our sample was limited by a lack of racial/ethnic diversity. Feasibility results do not necessarily generalize beyond the inclusion and exclusion criteria of the pilot design and should be interpreted with caution. Despite these limitations, a unique strength of this study was the exploration of feasibility from the perspective of key stakeholders: service recipients and their natural supports (i.e., family members and friends). Using a mixed-methods framework allowed us to study in depth how participants and their partners experienced the intervention and explore their recommendations for refinements to the model.
Implications for Future Research
Recommended modifications to the Fit Together intervention included adding more interactive sessions, using a combination of dyadic and group sessions, and incorporating cooking classes. As Fit Together evolves, these recommendations will help improve and refine the model to better meet the needs of participants and their support partners. Future intervention research should examine whether (a) participatory and collaborative learning techniques increase the acceptability of social support interventions targeting health behavior change; (b) a hybrid treatment model involving both dyadic and group-based sessions increases social support for participants and their support partners; and (c) incorporating hands-on cooking courses empower participants and their support partners to be self-sufficient in the kitchen and able to prepare healthy meals. In addition, different social circumstances and relationships exist that might warrant variations on social support models for health promotion to be tested in future research, including co-residing partners and kinship versus friendship dyads. Future research should explore demographic and relationship moderators of intervention effects. Social cognitive theory might be a useful framework for studying the influence of social relationships on increasing self-efficacy for health behavior change (Bandura, 2004). For example, social modeling and social persuasion could be key constructs for helping individuals with SMI believe that they are capable of successfully making dietary changes and increasing physical activity to lose weight.
The Fit Together intervention was delivered by trained social workers who were equipped by virtue of their professional backgrounds to help individuals with SMI identify social factors that contributed to their health problems and to engage family members and significant others as potential sources of support for health behavior change. The Fit Together intervention ran concurrently with the In SHAPE program; however, the Fit Together coaches communicated only periodically with the In SHAPE health coaches. For a variety of reasons, including scope, time, and cost, the Fit Together intervention was not fully integrated into the In SHAPE program in this initial pilot study. In a prior qualitative study, the In SHAPE health coaches commented that they did not feel qualified to work directly with participants’ support partners; however, the coaches were interested and willing to collaborate with other providers who could facilitate social support for participants’ health goals. Social workers could play a critical role on health promotion teams addressing health risk behaviors in adults with SMI by using their knowledge and skills to engage and train natural supports to promote health behavior change. Future research should explore in more depth opportunities to integrate social support components into lifestyle interventions using collaborative approaches involving social workers as key members of multidisciplinary health promotion teams.
Conclusions
Increasing natural support for health behavior change is a promising strategy for increasing the effectiveness of healthy lifestyle interventions for individuals with SMI. The existing literature has theoretically supported the potential promise of social support interventions to promote lifestyle change in people with SMI. The current study builds on the limited knowledge base of the feasibility of such intervention strategies in this population. This formative research showed that the study design and intervention are feasible and that the intervention can facilitate social support for health behavior change in people with SMI. Qualitative reports noted high satisfaction and perceived benefits from the program. Further research is needed to evaluate the potential effectiveness of social support interventions in improving health outcomes for persons with SMI.
Acknowledgments
Support for this research was provided by the Dartmouth Health Promotion and Disease Prevention Research Center, supported by Cooperative Agreement Number U48DP005018 from the Centers for Disease Control and Prevention, and by a Career Development Award from the Agency for Healthcare Research and Quality (K12 HS021695-01). The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the funding sources.
Biographies
Kelly A. Aschbrenner is an assistant professor of psychiatry at the Geisel School of Medicine at Dartmouth College, an assistant professor in the Dartmouth Institute for Health Policy and Clinical Practice, and an investigator at The Health Promotion Research Center at Dartmouth.
Kim T. Mueser is a clinical psychologist and executive director of the Center for Psychiatric Rehabilitation at Boston University.
John A. Naslund is a doctoral candidate in The Dartmouth Institute for Health Policy and Clinical Practice.
Amy A. Gorin is an associate professor in The Department of Psychology, University of Connecticut.
Allison Kinney is a project manager at The Dartmouth Institute for Health Policy and Clinical Practice.
Lucas Daniels is a research assistant at The Dartmouth Institute for Health Policy and Clinical Practice.
Stephen J. Bartels is a professor of psychiatry, community and family medicine, and The Dartmouth Institute for Health Policy and Clinical Practice at the Geisel School of Medicine at Dartmouth. He is also the director of the Dartmouth Centers for Health and Aging and the Health Promotion Research Center at Dartmouth.
Contributor Information
Kelly A. Aschbrenner, Health Promotion Research Center at Dartmouth
Kim T. Mueser, Boston University Center for Psychiatric Rehabilitation
John A. Naslund, The Dartmouth Institute for Health Policy and Clinical Practice
Amy A. Gorin, University of Connecticut
Allison Kinney, The Dartmouth Institute for Health Policy and Clinical Practice.
Lucas Daniels, The Dartmouth Institute for Health Policy and Clinical Practice.
Stephen J. Bartels, The Dartmouth Centers for Health and Aging
References
- Aschbrenner K, Bartels S, Mueser K, Carpenter-Song E, Kinney A. Consumer perspectives on involving family and significant others in a healthy lifestyle intervention. Health & Social Work. 2012;37:207–215. doi: 10.1093/hsw/hls032. http://dx.doi.org/10.1093/hsw/hls032. [DOI] [PubMed] [Google Scholar]
- Aschbrenner K, Mueser K, Bartels S, Carpenter-Song E, Pratt S, Barre L, Naslund J, Kinney A. The other 23 hours: A qualitative study of fitness provider perspectives on social support for health promotion for adults with mental illness. Health & Social Work. 2015;40:91–99. doi: 10.1093/hsw/hlv006. http://dx.doi.org/10.1093/hsw/hlv006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner KA, Mueser KT, Bartels SJ, Pratt SI. Perceived social support for diet and exercise among persons with serious mental illness enrolled in a healthy lifestyle intervention. Psychiatric Rehabilitation Journal. 2013;36:65–71. doi: 10.1037/h0094973. http://dx.doi.org/10.1037/h0094973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, Mueser KT. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric Services. 2013;64:729–736. doi: 10.1176/appi.ps.003622012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe R, Bird BL. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. American Journal of Psychiatry. 2015;172:344–352. doi: 10.1176/appi.ajp.2014.14030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe J. Rapid assessment process: An introduction. Walnut Creek, CA: Altamira Press; 2001. [Google Scholar]
- Berkman LF. The role of social relations in health promotion. Psychosomatic Medicine. 1995;57:245–254. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- Breslow L. Social ecological strategies for promoting healthy lifestyles. American Journal of Health Promotion. 1996;10:253–257. doi: 10.4278/0890-1171-10.4.253. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Statistics in Medicine. 2013;32:10. doi: 10.1002/sim.5408. 10.02/sim.5408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- Cortright RN, Collins HL, DiCarlo SE. Peer instruction enhanced meaningful learning: ability to solve novel problems. Advances in Physiology Education. 2005;29(2):107–111. doi: 10.1152/advan.00060.2004. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, Appel LJ. A behavioral weight-loss intervention in persons with serious mental illness. New England Journal of Medicine. 2013;368:1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis L, Brekke JS. Social networks and arrest among persons with severe mental illness: An exploratory analysis. Psychiatric Services. 2013;64:1274–1277. doi: 10.1176/appi.ps.201200443. [DOI] [PubMed] [Google Scholar]
- Dixon L, McFarlane WR, Lefley H, Lucksted A, Cohen M, Falloon I, Sondheimer D. Evidence-based practices for services to families of people with psychiatric disabilities. Psychiatric Services. 2001;52:903–910. doi: 10.1176/appi.ps.52.7.903. [DOI] [PubMed] [Google Scholar]
- Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Medical Care. 2011;49:599–604. doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Kilanowski C, Paluch RA, Raynor H, Daniel TO. Reducing variety enhances effectiveness of family-based treatment for pediatric obesity. Eating Behavoirs. 2015;17:140–143. doi: 10.1016/j.eatbeh.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyles C, Leydon G, Hoffman C, Copson E, Prescott P, Lewith G. Mindfulness for the fatigue, anxiety and depression in women with metastatic breast cancer: a mixed method feasibility study. Journal of Alternative and Complementary Medicine. 2014;20(5):A60. doi: 10.1089/acm.2014.5157.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagen AP, Crouch CH, Mazur E. Peer instruction: Results from a range of classrooms. The Physics Teacher. 2002;40:206–209. [Google Scholar]
- Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs—Principles and practices. Health Services Research. 2013;48:2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Raynor HA, Fava J, Maguire K, Robichaud E, Trautvetter J, Wing RR. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health Psychology. 2013;32:128–137. doi: 10.1037/a0026959. http://dx.doi.org/10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Yarborough BJ, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, Stevens VJ. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. American Journal of Psychiatry. 2015;172:71–81. doi: 10.1176/appi.ajp.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney CA, Israel BA. Social networks and social support. Health behavior and health education: Theory, research, and practice. 2008;4:189–210. [Google Scholar]
- Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, Orchard TJ. Translating the diabetes prevention program: A comprehensive model for prevention training and program delivery. American Journal of Preventive Medicine. 2009;37:505–511. doi: 10.1016/j.amepre.2009.07.020. http://dx.doi.org/10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology. 2014;10:425–448. doi: 10.1146/annurev-clinpsy-032813-153657. [DOI] [PubMed] [Google Scholar]
- Leahey TM, Gokee LaRose J, Fava JL, Wing RR. Social influences are associated with BMI and weight loss intentions in young adults. Obesity. 2011;19:1157–1162. doi: 10.1038/oby.2010.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Wong YL, Rothbard A. Effects of social networks on physical health among people with serious mental illness. Psychiatric Quarterly. 2014;85:453–465. doi: 10.1007/s11126-014-9306-6. [DOI] [PubMed] [Google Scholar]
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. Journal of psychiatric research. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyman DR, Braude L, George P, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME. Consumer and family psychoeducation: assessing the evidence. Psychiatric Services. 2014;65:416–428. doi: 10.1176/appi.ps.201300266. [DOI] [PubMed] [Google Scholar]
- Manu P, Dima L, Shulman M, Vancampfort D, De Hert M, Correll CU. Weight gain and obesity in schizophrenia: epidemiology, pathobiology, and management. Acta Psychiatrica Scandinavica. 2015 doi: 10.1111/acps.12445. [DOI] [PubMed] [Google Scholar]
- McFarlane WR. Multiple-family groups and psychoeducation in the treatment of schizophrenia. New Directions for Mental Health Services. 1994;1994(62):13–22. doi: 10.1002/yd.23319946204. [DOI] [PubMed] [Google Scholar]
- Meyer PS, Johnson DP, Parks A, Iwanski C, Penn DL. Positive living: A pilot study of group positive psychotherapy for people with schizophrenia. The Journal of Positive Psychology. 2012;7:239–248. doi: 10.1080/17439760.2012.677467. [DOI] [Google Scholar]
- Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial treatments for schizophrenia. Annual Review of Clinical Psychology. 2013;9:465–497. doi: 10.1146/annurev-clinpsy-050212-185620. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Glynn SM. Behavioral Family Therapy for Psychiatric Disorders. New Harbinger Publications; 1999. [Google Scholar]
- Mueser KT, Glynn SM, Liberman RP. Behavioral family management for serious psychiatric illness. New Dir Ment Health Serv. 1994;(62):37–50. doi: 10.1002/yd.23319946206. [DOI] [PubMed] [Google Scholar]
- Ryan P. Integrated theory of health behavior change: Background and intervention development. Clinical Nurse Specialist. 2009;23:161–172. doi: 10.1097/NUR.0b013e3181a42373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues in Mental Health Nursing. 2011;32:589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- Smith JD, Baillie J, Baglin T, Griffiths GO, Casbard A, Cohen D, Noble SI. A feasibility study to inform the design of a randomized controlled trial to identify the most clinically and cost effective anticoagulation length with low molecular weight heparin in the treatment of cancer associated thrombosis (ALICAT): study protocol for a mixed-methods study. Trials. 2014;15:122. doi: 10.1186/1745-6215-15-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon P. Rapid assessment of existing HIV prevention programming in a community mental health center. Journal of Prevention & Intervention in the Community. 2007;33:137–151. doi: 10.1300/J005v33n01_11. [DOI] [PubMed] [Google Scholar]
- Sorkin DH, Mavandadi S, Rook KS, Biegler KA, Kilgore D, Dow E, Ngo-Metzger Q. Dyadic collaboration in shared health behavior change: the effects of a randomized trial to test a lifestyle intervention for high-risk Latinas. Health Psychology. 2014;33:566–575. doi: 10.1037/hea0000063. http://dx.doi.org/10.1037/hea0000063. [DOI] [PubMed] [Google Scholar]
- Stokols D. Social ecology and behavioral medicine: implications for training, practice, and policy. Behavoiral Medicine. 2000;26:129–138. doi: 10.1080/08964280009595760. [DOI] [PubMed] [Google Scholar]
- Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, Grady D. Weight loss to treat urinary incontinence in overweight and obese women. New England Journal of Medicine. 2009;360:481–490. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorup A, Petersen L, Jeppesen P, Ohlenschlaeger J, Christensen T, Krarup G, Nordentoft M. Social network among young adults with first-episode schizophrenia spectrum disorders: results from the Danish OPUS trial. Social Psychiatry and Psychiatric Epidemiology. 2006;41:761–770. doi: 10.1007/s00127-006-0098-3. [DOI] [PubMed] [Google Scholar]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychology. 2007;26:521–532. doi: 10.1037/0278-6133.26.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. Journal of Consulting & Clinical Psychology. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- Wing RR, Leahey T, Jeffery R, Johnson KC, Hill JO, Coday M, Espeland MA. Do weight loss and adherence cluster within behavioral treatment groups? Obesity. 2014;22:638–644. doi: 10.1002/oby.20526. [DOI] [PMC free article] [PubMed] [Google Scholar]


