Abstract
Objectives
Objectives were to: (a) identify the mental health needs of older and younger sexual minority and heterosexual US veterans and (b) examine whether sexual minority status confers vulnerability or resiliency in older adulthood. Support and trauma exposure were examined as potential mechanisms for age by sexual orientation differences.
Method
Participants were a nationally representative sample of 3,095 US veterans (ages 21 to 96 years). Measures included demographics, military characteristics, sexual orientation (lesbian, gay, or bisexual; LGB), social support, trauma, and mental health indicators (lifetime and present depression and posttraumatic stress disorder (PTSD); lifetime anxiety and suicidal ideation).
Results
Younger LGB veterans were most likely to report lifetime depression and/or PTSD and current depression compared to older LGB and younger and older heterosexual veterans. Older LGB veterans had low levels of mental health problems, but they reported the smallest social support networks.
Conclusion
Older and younger LGB veterans have different mental health challenges. Younger LGB veterans are more vulnerable to mental health problems than their older LGB peers. Older LGB veterans are resilient, but they may be at greater risk of social isolation than their younger LGB peers.
Keywords: sexual minority status, veterans, mental health, aging
Sexual minority individuals (e.g., those who identify as lesbian, gay, or bisexual (LGB)) have an increased risk of mental health difficulties [1]. However, there is a debate about whether older age confers LGB adults with greater resiliency or vulnerability to mental health problems. One argument, supported by crisis competence theory, posits that with older age comes more exposure to stigma, inoculating LGB adults against mental health problems by improving their coping ability [2]. Also consistent with crisis competence theory is that younger LGB adults experience more stress than older LGB adults because they are currently dealing with parental and/or peer rejection [3], the stress of concealing and disclosing their sexual orientation [4], and potential workplace discrimination [5]. Older LGB adults have more temporal distance from these stressors, having resolved them earlier in life. On the other hand, accumulation of repeated stigma-related stressors over the lifespan may be overwhelming, increasing older LGB adults’ risk for mental health problems [6]. The present study is the first, to our knowledge, to address this vulnerability versus resiliency debate in a contemporary, nationally representative sample of US veterans—the National Health and Resilience in Veterans Study. Not only does this dataset provide an opportunity to test these competing theories, but it allows for identification of the unique mental health needs of younger and older sexual minority US veterans.
There is a substantial and growing literature examining the impact of sexual orientation on mental health indicators among veterans, with an emphasis on the experiences of young female veterans [7-9]. This research shows that sexual minority veterans are more likely to experience military and childhood trauma, report less social and emotional support, and report worse mental health than heterosexual veterans. However, more research is needed that examines differences between younger and older adults. The older veteran population, the majority of which is male, is increasing rapidly [10]. It is estimated that there are nearly 900,000 lesbian, gay, or bisexual (LGB) US veterans [11], many of whom are over the age of 65 [12]. Mental health interventions for LGB veterans may need to be tailored for younger and older veterans.
The overall aim of the present research was to examine whether there are age differences in the association between veterans’ LGB status and mental health. We also examined differences by age and LGB status in exposure to trauma and perceptions of social support that potentially account for mental health disparities.
Why Might Older Age Confer Mental Health Vulnerability for LGB Veterans?
It has been proposed that LGB individuals experience poorer mental health than heterosexual individuals because of minority stress, defined as the disproportionate stress experienced by socially marginalized group members [13]. Sexual minorities are exposed to stressors induced by a hostile, homophobic culture, which often results in a lifetime of harassment, maltreatment, discrimination, and victimization [13] and may impact access to care [14]. LGB adults are more likely to be exposed to trauma [15] and to have less social support resources (e.g., family support) [6]. This stress can “get under the skin” to influence health through psychological processes such as emotion dysregulation, interpersonal problems, and maladaptive cognitions (e.g., rejection sensitivity, internalized homonegativity) [16].
Recently, there has been a focus on understanding whether sexual minority stress accumulates over the lifespan, potentially increasing vulnerability to mental health problems in older age. Some arguments for added vulnerability are as follows. First, with older age comes a greater incidence of chronic conditions and disability [17]. Second, older adults face age discrimination which has important negative implications for their mental health [18]. Third, older LGB adults have lived longer, giving them more of an opportunity to experience trauma than younger LGB adults [9]. Older LGB adults have lived through historical periods in which there was more discrimination than there is today [6,19]. This may be particularly true in the military [20]. Fourth, older LGB adults have small social support networks, partly because they are less likely to have children than older heterosexual adults [21], and they may live in environments that make it more difficult to connect with sexual minority peers [22]. These arguments suggest that older LGB veterans may have more mental health problems compared to younger LGB veterans and both older and younger heterosexual veterans.
Why Might Older Age Confer Mental Health Resiliency for Veterans?
It has also been proposed that older LGB adults have an advantage over older heterosexual adults and younger LGB adults because they have had to cope with a stigmatized identity, namely their sexual identity, in the past. This may prepare them to cope with age-related and/or sexual status-related stigma when it arises. Friend [2] provides more reasons for why older age may be protective for sexual minorities’ health [6]. First, greater flexibility in gender role definitions may allow older LGB individuals to have developed ways of taking care of themselves that feel comfortable and appropriate. Second, older LGB adults may have successfully redefined the meaning of family (i.e. viewing friends as “family”) and the ways in which support is provided by family members. Third, older LGB adults may have become experts in advocacy, allowing them to overcome institutional and societal barriers. Crisis competence theory [2] explains this stigma-inoculation effect, but to date, limited evidence for this theory.
Consistent with the idea that with old age comes resiliency, past studies have shown that younger LGB adults are more susceptible to mental health issues than older LGB adults. Potential reasons include that they are currently dealing with concealing or disclosing their sexual orientation [4] and experiencing peer and parental rejection [3], stressors from which older LGB adults may have more temporal and emotional distance. Younger adults may be entering into or experiencing discrimination at work; whereas older LGB adults may be retired or have established work environments that are compatible with their identity.
The Present Study
Little is known about age differences in vulnerability and resiliency to mental health problems among LGB and heterosexual civilians; even less is known in veterans. Examining these questions in a veteran sample is especially valuable because LGB veterans are likely to have experienced pronounced stress as they belonged to an institution that overtly discriminated against lesbian, gay, and bisexual people under the policy that was commonly referred to as “Don’t Ask, Don’t Tell” (DADT). For some older veterans, discrimination of sexual minority individuals was even greater and more overt before DADT was established [23]. Sexual minorities, if discovered, were officially banned from the military in the 1940s and were discharged regardless of sexual conduct in subsequent decades [23]. On the other hand, research also shows that sexual minority individuals who are more recently “out” may be more vulnerable to mental health challenges than individuals who have been “distantly out” or “closeted”. As being “out” has only recently been condoned in the military, this may make younger sexual minority veterans more vulnerable than older sexual minority veterans to mental health problems [4]. The National Health and Resilience in Veterans Study (NHRVS), with its contemporary, representative sample of younger and older veterans and assessment of sexual orientation, mental health, and psychosocial factors, provides an unprecedented opportunity to examine age as a moderator of the association between sexual orientation and mental health problems. It also allows for the exploration of potential mediators -- trauma exposure and social support-- proposed pathways in both the vulnerability and resiliency theories.
Method
The Sample
Data were from the National Health and Resilience in Veterans Study (NHRVS), a nationally representative study of 3,157 US veterans conducted in October-December 2011. The NHRVS sample was drawn from KnowledgePanel, a nationally representative research panel of more than 50,000 households that is developed and maintained by GfK Knowledge Networks, Inc., a survey research firm based in Menlo Park, California. Panel members are recruited through national random samples, originally by telephone and now almost entirely by postal mail. Households are provided with access to the Internet and computer hardware if needed. Unlike Internet convenience panels, also known as “opt-in” panels, that include only individuals with Internet access who volunteer themselves for research, KnowledgePanel recruitment uses dual sampling frames that include both listed and unlisted telephone numbers, telephone and non-telephone households, and cell phone- only households and household with and without Internet access.
Inclusion in the NHRVS required that participants self-identified as veterans during their initial assignment to the panel by reporting previous service in the US Armed Forces, Military Reserves, or National Guard. A total of 3,188 individuals in the full Knowledge Networks panel answered “yes” to the initial screening question: “Have you ever served on active duty in the US Armed Forces, Military Reserves, or National Guard?” Of these, 3,157 (99%) completed the survey.
To permit generalizability of study results to the entire population of US veterans, post-stratification weights were computed by GfK statisticians and applied to all inferential statistics based on demographic distributions (i.e., age, gender, race/ethnicity, education, Census region, and metropolitan area) drawn from the most recent (October 2010) Current Population Survey [24]. All participants provided informed consent and the study was approved by the local institutional review board. The NHRVS has been widely used to examine the mental and physical health of US veterans [25-27].
Assessments
Sexual minority status
Sexual minority status was assessed with the question, “Do you consider yourself to be…?” with the following response options: Heterosexual or straight (1), Gay (2), Lesbian (3), Bisexual (4), Other, please specify. Because of the small numbers in each group, we collapsed lesbian, gay, and bisexual individuals into one group for comparison to heterosexuals.
Covariates
All participants answered questions about socio-demographic (e.g., gender, education) and military (e.g., branch) characteristics (Table 1). Combat exposure was assessed by asking, “Did you ever serve in a combat or war zone?” We also included the number of self-reported medical conditions using items developed for the NHRVS (e.g., arthritis, cancer, diabetes, heart disease, asthma; range 0-14).
Table 1.
Veteran demographic and military characteristics by sexual orientation
| LGB raw n (weighted %) or mean (SD) n=102 (2.8%) |
Heterosexual raw n (weighted %) or mean (SD) n=2,993 (97.2%) |
Test of difference F(1,2991) or X2(1) |
P value | |
|---|---|---|---|---|
| Socio-demographic characteristics | ||||
| Age* | 55.5 (17.0; range=23-89) | 60.4 (15.0; range=21-96) | 5.81 | 0.016 |
| Male sex* | 78 (76.1%) | 2,703 (91.2%) | 23.14 | <0.001 |
| Caucasian race/ethnicity | 83 (75.0%) | 2,501 (76.3%) | 0.08 | 0.78 |
| Some college or higher education* | 92 (87.5%) | 2,527 (66.0%) | 17.81 | <0.001 |
| Married/living with partner* | 56 (59.1%) | 2,379 (76.1%) | 13.43 | <0.001 |
| Retired* | 34 (31.8%) | 1,413 (43.8%) | 4.96 | 0.026 |
| Household income≥$60K | 48 (53.4%) | 1,568 (43.5%) | 3.39 | 0.066 |
| Military characteristics | ||||
| Enlisted in military | 93 (97.3%) | 2,572 (87.6%) | 3.63 | 0.057 |
| Branch of service* | 11.31 | 0.023 | ||
| Air Force | 35 (34.5%) | 749 (22.2%) | ||
| Army | 34 (29.9%) | 1,213 (38.6%) | ||
| Navy | 24 (27.6%) | 685 (24.0%) | ||
| Marines | 6 (4.6%) | 245 (11.4%) | ||
| Other | 3 (3.4%) | 95 (3.8%) | ||
| Combat Veteran | 32 (36.4%) | 1,054 (34.5%) | 0.13 | 0.72 |
| Number of years in military | 5.7 (5.7) | 7.0 (7.4) |
Note. SD=standard deviation.
Groups differ significantly, p<0.05.
Continuous variables were compared using analyses of variance (degrees of freedom [df]=1,2991); and categorical variables were compared using chi-squared tests (df=1).
Current and lifetime mental health difficulties
The current mental health difficulties assessment included positive screens for (1) depression, (2) generalized anxiety (Patient Health Questionnaire-4 [28]) and/or (3) posttraumatic stress disorder on a past-month version of the Posttraumatic Stress Disorder Checklist [29]).
Lifetime history of depression and/or PTSD was operationalized as a positive screen for (1) lifetime Major Depressive Disorder (Mini International Neuropsychiatric Interview [M.I.N.I.][30]) and/or (2) PTSD, defined as a positive screen (score of 44 and higher on a lifetime version of the PCL)[29].
Lifetime suicide attempt was assessed by asking, “Have you ever tried to kill yourself?”. Current suicidal ideation was assessed with two items from the Patient Health Questionnaire-9 [31], “How often have you been bothered by thoughts you might be better off dead?” and “How often have you been bothered by thoughts of hurting yourself in some way?” Responses were not at all, several days, more than half the days, or nearly every day. A dichotomous variable (not at all vs. any) was created from these responses.
Social support
Structural social support was assessed with the question: “About how many close friends and relatives do you have—people you feel at ease with and can talk to about what is on your mind?” This was scored as a count, ranging from 0-90. Functional social support was assessed with a five-item version of the Medical Outcomes Study social support survey [32]. Participants were asked “How often each of the following kinds of support are available to you if you need it?” on a 5 point scale from (1) none of the time to (5) all of the time. Examples of items were: “Someone to confide in or talk about your problems” and “Someone to get together with for relaxation”. Scores range from 5-25, with higher scores indicative of greater social support.
Exposure to trauma
Number of lifetime traumas was a count variable created by summing responses from the Trauma History Screen [33], which assesses the occurrence of 14 traumatic life events across the lifespan, including early life traumas such as physical or sexual assault during childhood as well as traumas that more commonly occur in adulthood, such as motor vehicle accidents, military combat, and unexpected losses of loved ones. The NHRVS added life-threatening illness or injury to the list.
Data Analysis
Statistical analyses proceeded in four steps. First, the prevalence of LGB veterans in the NHRVS sample was calculated, and differences by sexual orientation in socio-demographic (e.g. gender, marital status) and military characteristics were examined using chi square tests. Variables demonstrating statistically significant differences by sexual orientation were included as covariates in subsequent statistical analyses. Number of medical conditions was additionally included as a covariate in analyses in order to distinguish mental from physical health problems1. Second, bivariate differences in mental health outcomes by sexual orientation were examined using chi square tests. Adjusted logistic regression analyses were used to examine associations between sexual orientation and mental health variables, while differences by sexual orientation with regards to trauma and social support were examined using analysis of covariance (ANCOVA). Third, the interactive effects of age and sexual orientation on mental health, social support, and trauma variables were examined by adding an age (continuous variable) by sexual orientation interaction term to each of the logistic regression and ANCOVA models. Age and number of medical conditions were mean-centered. To visualize statistically significant age by sexual orientation interactions, we plotted scores on dependent variables in younger (-1 standard deviation for age distribution in sample) and older (+1 standard deviation for age distribution in sample) LGB and heterosexual veterans.
Results
Personal characteristics of LGB versus heterosexual veterans
In the overall sample of 3,157 veterans, 102 (weighted 2.8%) individuals identified as a sexual minority and 2,993 (97.2%) identified as heterosexual. More specifically, 39 (1.1%) identified as gay, 12 (0.4%) as lesbian, and 51 (1.4%) as bisexual. These numbers align with population-based estimates [11]. Sixteen individuals (0.6%) in the overall sample reported being “other.” Of the 16 veterans who reported “other”, one veteran specified “transgendered”; one “nonsexual”; one “metrosexual”, and one “uncertain”. Seven left the specification blank, and five responded with unusable comments. There were 45 (0.9%) missing responses. Data from “other” and missing responses were excluded from the present analysis, resulting in a final sample of n=3,095 veterans.
Table 1 shows differences between LGB and heterosexual veterans on socio-demographic and military characteristics. LGB veterans were younger. Fewer LGB veterans than heterosexual veterans were male, married or living with their partners, and retired. A higher proportion of LGB veterans than heterosexual veterans had completed some college or higher.
Did age moderate the association between LGB status and current and lifetime indicators of mental health and suicidal ideation and attempts?
As shown in Table 2, although LGB veterans had higher rates of lifetime depression, PTSD, and suicide attempt, and current suicidal ideation in bivariate analyses; these differences were not significant in the final models, which adjusted for significant covariates identified in Table 1 and number of medical conditions.
Table 2.
Veteran mental health, support, and trauma by sexual orientation
| Bivariate analyses | Multivariate analyses | |||
|---|---|---|---|---|
|
| ||||
| LGB Raw n (weighted %) |
Heterosexual Raw n (weighted %) |
LGB (Mean [SE] or AOR [95% CI]) |
Heterosexual (Mean [SE] or AOR [95% CI]) |
|
| Primary outcomes | ||||
| Lifetime Depression and/or PTSD*** | 43 (38.6%) | 571 (20.5%) | 1.44 (0.87-2.36) | 1.00 |
| Depression*** | 41 (34.1%) | 462 (16.5%) | 1.65 (0.99-2.73) | 1.00 |
| PTSD* | 17 (19.3%) | 282 (10.9%) | 0.97 (0.53-1.78) | 1.00 |
| Lifetime Suicide Attempt** | 20 (14.8%) | 140 (6.6%) | 1.54 (0.80-2.97) | 1.00 |
| Current Depression, PTSD, or Anxiety | 18 (16.3%) | 283 (11.6%) | 0.83 (0.43-1.59) | |
| Depression | 14 (12.5%) | 194 (12.5%) | 0.95 (0.47-1.93) | 1.00 |
| GAD | 10 (11.4%) | 188 (8.0%) | 0.81 (0.39-1.70) | 1.00 |
| PTSD | 8 (4.7%) | 148 (6.9%) | 0.37 (0.13-1.04) | 1.00 |
| Current Suicidal ideation* | 15 (16.1%) | 211 (9.4%) | 1.37 (0.74-2.55) | 1.00 |
| Potential mediatorsa | ||||
| Structural support*** | - | - | 13.37 (1.06) | 8.24 (0.33) |
| Functional support | - | - | 17.81 (0.54) | 18.36 (0.17) |
| Number of lifetime traumas | - | - | 3.59 (0.30) | 3.25 (0.09) |
Note. ANCOVAs for continuous variables (df=1,2919) and logistic regression analyses for dichotomous dependent variables (df=1) were used to compare the groups. Significant bivariate association with sexual orientation:
p<.05,
p<.01,
p<.001.
SE=standard error; AOR=Adjusted Odds Ratio. Analyses are adjusted for gender, age, education, marital status, retired status, and number of medical conditions.
Potential mediators for the age x sexual orientation interaction predicting mental health problems.
Next, we examined interactions between age and LGB status predicting each outcome. There was a significant interaction between age and LGB status predicting lifetime diagnosis of depression and/or PTSD (Wald X2(1)=4.87, p=0.027; AOR=1.03, 95% CI =1.01-1.06), such that younger LGB veterans were most likely to screen positive for lifetime depression and/or PTSD than younger heterosexual veterans (Figure 1). There was also a significant LGB status X age interaction in predicting current depression (Wald X2(1)=3.94, p=0.047; AOR=0.95, 95% CI=0.91-0.99), such that young LGB veterans had greater prevalence of depression compared to heterosexual veterans. There were no significant interactions between age and sexual orientation predicting lifetime suicide attempt (Wald X2(1)=0.35, p=0.55; AOR=1.01, 95% CI=0.97-1.05) and current GAD (Wald X2(1)=0.32, p=0.57; AOR=0.99, 95% CI=0.94-1.03), PTSD (Wald X2(1)=0.34, p=0.56; AOR=1.01, 95% CI=0.97-1.05), or suicide ideation (Wald X2(1)=3.73, p=0.053; AOR=0.96, 95% CI=0.92-1.00).
Figure 1.
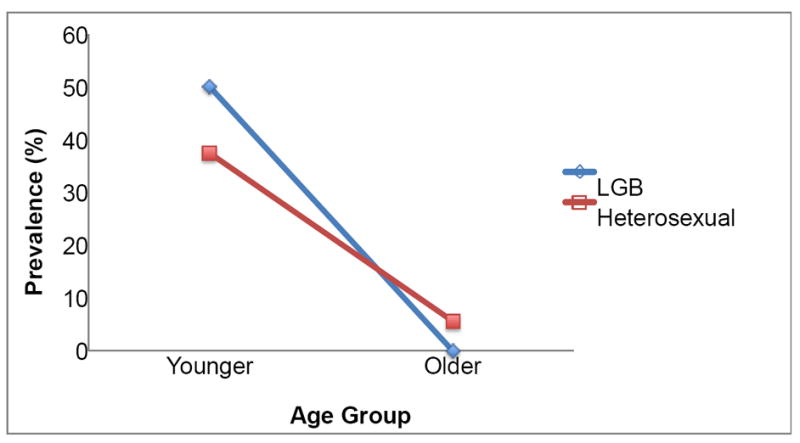
Sexual Minority Status Predicting Lifetime History of Depression and/or PTSD in Younger and Older Veterans
Note. Younger veterans are those aged <50 (mean=38.5, SD=7.8, range=21-49), which represents -1 SD of the mean age for the full sample; Older veterans are those aged >=75 (mean=79.5, SD=3.9, range=75-96), which represents +1 SD of the mean of age for the full sample. The figure represents the following sample sizes: younger LGB veterans=34; older LGB veterans=8; younger heterosexual veterans=487; older heterosexual veterans=510.
Did trauma exposure and perceptions of structural and functional social support mediate the age X sexual orientation interaction on mental health?
As shown in Table 2, there was a main effect such that LGB veterans reported greater structural support than heterosexual veterans. There was also a significant interaction between age and LGB status predicting structural support (F(df=1)= 6.28, p=.012) such that younger LGB veterans reported the largest social support networks and older LGB veterans reported the smallest support networks (Figure 2).
Figure 2.
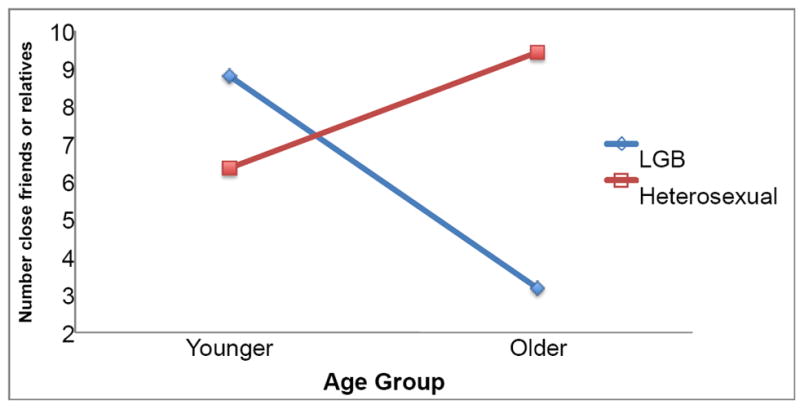
Sexual Minority Status Predicting Structural Support for Younger and Older Veterans
Note. Younger veterans are those aged <50 (mean=38.5, SD=7.8, range=21-49), which represents -1 SD of the mean age for the full sample; Older veterans are those aged >=75 (mean=79.5, SD=3.9, range=75-96), which represents +1 SD of the mean of age for the full sample. The figure represents the following sample sizes: younger LGB veterans=34; older LGB veterans=8; younger heterosexual veterans=487; older heterosexual veterans=510.
We did not examine mediation effects of trauma or social support for the interaction between age and sexual orientation predicting mental health problems because the age by sexual orientation effect was not significant for traumatic life events (F[1,2969]=1.69, p=0.19). Also, the age by sexual orientation interaction effect predicting social support was not in the same direction as the effect for mental health (F[1,2918]=0.29, p=0.59) [34]. In other words, because we found that younger LGB veterans had worse mental health but large social networks, the conditions for our hypothesis for social support as a mediator were not satisfied.
Discussion
Using data from a contemporary, nationally representative sample of U.S. military veterans, this study found mixed support for the vulnerability and resiliency theories. On one hand, older LGB veterans were more resilient to mental health problems than younger LGB veterans. On the other hand, older LGB veterans had the smallest social support networks. The present findings add support to an age-based, lifespan model of sexual orientation disparities in health, whereby LGB adults have different needs across the life course, as demonstrated among US veterans.
Our finding that younger LGB veterans were the most vulnerable group to mental health problems, such as current depression and lifetime depression and PTSD, is consistent with and extends recent findings showing that younger LGB adults report the greatest physical health symptoms in large representative samples of civilians [35]. Now it will be important for future research to include questions about stressors that are particularly salient for younger sexual minority veterans, such as perceptions of stigma and parental rejection. Although the effect sizes in this study were small, our findings suggest that mental health screening and interventions that address these topics may be particularly helpful for young veterans.
Although we found that older LGB veterans reported low levels of mental health problems, we did not find evidence that social support or trauma exposure explained these findings, as would be proposed by crisis competence or cumulative stress theories. Future research is needed to examine other mechanisms, such as age-related changes in emotion regulation strategies [36]. It will also be useful to examine accuracy of self-reported mental health problems, as older adults may under-report their symptoms [37].
In line with past findings with older LGB civilians, we found that older LGB veterans had the smallest social support networks [6]. This may reflect their experience of DADT, making them less likely to seek out support from others. However, it is important to note that both LGB and heterosexual older veterans had small networks than younger veterans which is consistent with socio-emotional selectivity theory [36] and also that older adults’ peers are more likely to have died than those of younger peers. This does not mean however that their network members are less emotionally close.
A limitation of this study is that it was cross-sectional and vulnerable to cohort effects. Rather than solely capturing age differences, we may be capturing historical effects. Future research could follow the same group of veterans as young adults into older adulthood to fully capture how sexual minority status and age interact to influence mental health. A comparable sample of civilians and more questions about military characteristics (e.g. era of service, rank) and service-related disabilities would also help us understand the unique experiences of sexual minority veterans. Another limitation was the small number of LGB veterans in this sample, which did not allow for examining differences among lesbian, gay, and bisexual groups or interactions between gender, sexual orientation, and age to explore whether or not male and female sexual minorities differ in their mental health resilience as they age.
Measuring gender identity as well as sexual orientation and including more transgender veterans will also be important in future research [38]. Examining healthcare utilization and participation in screening and prevention activities are also important directions, as previous research suggests that sexual minority veterans may avoid healthcare settings due to stigma [39]. This may be particularly true for younger sexual minority veterans who are not faced with health conditions related to old age and may become more easily disconnected from healthcare. Finally, it will be important to investigate whether particular mental health outcomes are associated with particular types of trauma.
There are many strengths to this study. For example, this is a large nationally representative survey of US veterans that assessed sexual orientation and multiple aspects of mental health. This dataset also accessed a substantial sample of older sexual minority veterans, whose voices are often unheard. Furthermore, this survey included psychosocial variables, allowing us to test potential mediators for the age by sexual orientation interaction predicting mental health problems.
Public Health Implications
The results of this study suggest that among LGB veterans, younger veterans are more vulnerable than older veterans to mental health issues. However, like their heterosexual peers, older LGB veterans have the smallest social support networks; whereas younger LGB veterans have larger networks than older LGB veterans. These findings have important public health implications. For instance, it may be beneficial to engage older LGB adults as a social support resource (e.g. mentoring) to help improve and/or protect the mental health of younger LGB veterans. This may also have positive effects for the older LGB mentors by increasing their social resources. To our knowledge, interventions of this type do not exist. Finally, and more broadly, this study provides evidence for the utility of tailoring interventions to improve sexual minority veterans’ health for older and younger groups, as they may have different social and coping resources [40].
Acknowledgments
This study was funded by the Department of Veterans Affairs National Center for Posttraumatic Stress Disorder. Preparation of this report was supported in part by a Research Career Development Award to Dr. Pietrzak from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (NIA Grant P30AG21342) and in part by National Institutes of Health grants (R01AG032284, R01HL089314) and to Dr. Monin from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (NIA Grant P30AG21342) and in part by National Institutes of Health grant (K01 AG042450).
Footnotes
Although not a central aim of this study, we examined substance abuse as measured by lifetime alcohol and drug use disorder modules of the MINI Neuropsychiatric Interview, Fagerström Test for Nicotine Dependence (Heatherton et al., 1991), and Alcohol Use Disorders Identification Test-Consumption (Bush et al., 1998), which screens for past-year alcohol use disorder, as additional dependence variables. Associations with LGB status were not significant: Lifetime alcohol use disorder: LGB=48.9% vs. Heterosexual=42.1%, X2(1)=1.60, p=0.21; lifetime drug use disorder: LGB=18.2% vs. Heterosexual=13.3%, X2(1)=1.77, p=0.18; lifetime nicotine dependence: LGB=19.3% vs. Heterosexual=19.4%, X2(1)=0.00, p=0.98; past-year alcohol use disorder: 13.6% vs. 15.0%, X2(1)=0.12, p=0.72. Logistic regression analyses of these dependent variables further indicated that none of the LGB x age interactions were statistically significant, all Wald X2(1)<1.76, all p’s>0.18.
There are no disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cochran SD, Sullivan JG, Mays VM. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friend RA. Older Lesbian and Gay People. Journal of Homosexuality. 1991 Mar 31;20(3-4):99–118. doi: 10.1300/j082v20n03_07. [DOI] [PubMed] [Google Scholar]
- 3.Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346–352. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- 4.Pachankis JE, Cochran SD, Mays VM. The mental health of sexual minority adults in and out of the closet: A population-based study. Journal of consulting and clinical psychology. 2015;83(5):890. doi: 10.1037/ccp0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ragins BR, Singh R, Cornwell JM. Making the invisible visible: fear and disclosure of sexual orientation at work. Journal of Applied Psychology. 2007;92(4):1103. doi: 10.1037/0021-9010.92.4.1103. [DOI] [PubMed] [Google Scholar]
- 6.Fredriksen-Goldsen KI, Muraco A. Aging and sexual orientation: A 25-year review of the literature. Research on Aging. 2010;32(3):372–413. doi: 10.1177/0164027509360355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mattocks KM, Sadler A, Yano EM, et al. Sexual victimization, health status, and VA healthcare utilization among lesbian and bisexual OEF/OIF veterans. Journal of general internal medicine. 2013;28(2):604–608. doi: 10.1007/s11606-013-2357-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blosnich JR, Bossarte RM, Silenzio VM. Suicidal ideation among sexual minority veterans: results from the 2005 2010 Massachusetts Behavioral Risk Factor Surveillance Survey. American journal of public health. 2012;102(S1):S44–S47. doi: 10.2105/AJPH.2011.300565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehavot K, Simpson TL. Trauma, posttraumatic stress disorder, and depression among sexual minority and heterosexual women veterans. Journal of counseling psychology. 2014;61(3):392. doi: 10.1037/cou0000019. [DOI] [PubMed] [Google Scholar]
- 10.Projections UCBNP. 2009 [Google Scholar]
- 11.Gates G. Gay men and lesbians in the US military: Estimates from Census 2000. 2004 [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Medicine and science in sports and exercise. 1993 Jan;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among Black men who have sex with men. Journal of the National Medical Association. 2004;96(1):97–107. [PMC free article] [PubMed] [Google Scholar]
- 15.Brown LS, Pantalone D. Lesbian, gay, bisexual, and transgender issues in trauma psychology: A topic comes out of the closet. 2011 [Google Scholar]
- 16.Hatzenbuehler ML. How Does Sexual Minority Stigma “Get Under the Skin”? A Psychological Mediation Framework. Psychological bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability Trends Among Older Americans: National Health and Nutrition Examination Surveys 1988–1994 and 1999–2004. American Journal of Public Health. 2010;100(1):100–107. doi: 10.2105/AJPH.2008.157388. 05/02/accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levy BR. Mind matters: Cognitive and physical effects of aging self-stereotypes. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2003;58(4):P203–P211. doi: 10.1093/geronb/58.4.p203. [DOI] [PubMed] [Google Scholar]
- 19.Roberts AL, Austin SB, Corliss HL, Vandermorris AK, Koenen KC. Pervasive Trauma Exposure Among US Sexual Orientation Minority Adults and Risk of Posttraumatic Stress Disorder. American Journal of Public Health. 2010 Dec 01;100(12):2433–2441. doi: 10.2105/AJPH.2009.168971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shilts R. Conduct unbecoming: Gays and lesbians in the US military. Macmillan; 2005. [Google Scholar]
- 21.Fredriksen-Goldsen KI, Emlet CA, Kim H-J, et al. The Physical and Mental Health of Lesbian, Gay Male, and Bisexual (LGB) Older Adults: The Role of Key Health Indicators and Risk and Protective Factors. The Gerontologist. 2013 Aug 1;53(4):664–675. doi: 10.1093/geront/gns123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stein GL, Beckerman NL, Sherman PA. Lesbian and Gay Elders and Long-Term Care: Identifying the Unique Psychosocial Perspectives and Challenges. Journal of Gerontological Social Work. 2010 Jul 08;53(5):421–435. doi: 10.1080/01634372.2010.496478. [DOI] [PubMed] [Google Scholar]
- 23.Garland KJ. An exploratory study of lesbian, gay, bisexual and transgender veterans of recent US conflicts. 2007 [Google Scholar]
- 24.Bureau UC. Current Population Survey. 2010 Oct; Available at: http://www.census.gov/cps/
- 25.Pietrzak RH, Cook JM. Psychological resilience in older US veterans: results from the national health and resilience in veterans study. Depression and anxiety. 2013;30(5):432–443. doi: 10.1002/da.22083. [DOI] [PubMed] [Google Scholar]
- 26.Pietrzak RH, Tsai J, Kirwin PD, Southwick SM. Successful Aging Among Older Veterans in the United States. The American Journal of Geriatric Psychiatry. 2014 Jun;22(6):551–563. doi: 10.1016/j.jagp.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 27.Kuwert P, Knaevelsrud C, Pietrzak RH. Loneliness Among Older Veterans in the United States: Results from the National Health and Resilience in Veterans Study. The American Journal of Geriatric Psychiatry. 2014 Jun;22(6):564–569. doi: 10.1016/j.jagp.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 29.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility; Paper presented at: Annual Convention of the International Society for Traumatic Stress Studies; 1993. [Google Scholar]
- 30.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of clinical psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The Phq-9. Journal of general internal medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 33.Carlson EB, Smith SR, Palmieri PA, et al. Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment. 2011;23(2):463–477. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication monographs. 2009;76(4):408–420. [Google Scholar]
- 35.Bränström R, Hatzenbuehler ML, Pachankis JE. Sexual orientation disparities in physical health: Age and gender effects in a population-based study. Social psychiatry and psychiatric epidemiology. 2015:1–13. doi: 10.1007/s00127-015-1116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carstensen LL. Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychology and Aging. 1992;7(3):331–338. doi: 10.1037//0882-7974.7.3.331. [DOI] [PubMed] [Google Scholar]
- 37.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: Results from the baltimore epidemiological catchment area study. JAMA Psychiatry. 2014;71(3):273–280. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blosnich JR, Brown GR, Shipherd PJC, Kauth M, Piegari RI, Bossarte RM. Prevalence of Gender Identity Disorder and Suicide Risk Among Transgender Veterans Utilizing Veterans Health Administration Care. American Journal of Public Health. 2013 Oct 01;103(10):e27–e32. doi: 10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simpson TL, Balsam KF, Cochran BN, Lehavot K, Gold SD. Veterans administration health care utilization among sexual minority veterans. Psychological Services. 2013;10(2):223–232. doi: 10.1037/a0031281. [DOI] [PubMed] [Google Scholar]
- 40.Mattocks KM, Kauth MR, Sandfort T, Matza AR, Sullivan JC, Shipherd JC. Understanding health-care needs of sexual and gender minority veterans: how targeted research and policy can improve health. LGBT health. 2014;1(1):50–57. doi: 10.1089/lgbt.2013.0003. [DOI] [PubMed] [Google Scholar]


