Abstract
Objective
Intra-amniotic inflammation is a mechanism of disease implicated in preterm labor, preterm PROM, cervical insufficiency, a short cervix, and idiopathic vaginal bleeding. Determination of interleukin (IL)-6 with immunoassays has been proven for more than 2 decades to be an excellent method for the detection of intra-amniotic inflammation. However, assessment of IL-6 for this indication has been based on immunoassays which are not clinically available, and this has been an obstacle for the implementation of this test in clinical practice. It is now possible to obtain results within 20 minutes with a point of care test which requires minimal laboratory support. This test is based on lateral flow-based immunoassay. The objective of this study was to compare amniotic fluid (AF) IL-6 and interferon-γ –inducible protein 10 (IP-10 or CXCL-10) concentrations determined using lateral flow-based immunoassay or point of care (POC) test and standard enzyme-linked immunosorbent assay (ELISA) techniques.
Material and methods
AF samples were collected from patients with singleton gestations and symptoms of preterm labor (n=20). AF IL-6 and IP-10 concentrations were determined by lateral flow-based immunoassay and ELISA. Intra-amniotic inflammation was defined as AF IL-6 > 2.6 ng/ml. AF IL-6 and IP-10 concentrations between two assays were compared.
Results
1) Lateral flow-based immunoassay point of care AF IL-6 and IP-10 test results were strongly correlated with concentrations of this cytokine/chemokine determined by ELISA (Spearman's ρ =0.92 and 0.83, respectively, both p < 0.0001); 2) AF IL-6 concentrations determined by the lateral flow-based immunoassay test were, on average, 30% lower than those determined by ELISA, and the median difference was statistically significant (p < 0.0001); and 3) in contrast, AF IP-10 concentrations determined by the lateral flow-based immunoassay test were, on average, only 7% lower than those determined by ELISA, and the median difference was not statistically significant (p =0.81).
Conclusion
Amniotic fluid IL-6 and IP-10 concentrations determined using a lateral flow-based immunoassay point of care are strongly correlated with concentrations determined by conventional ELISA. This justifies further studies about the diagnostic indices and predictive values of this point of care test.
Keywords: Amniocentesis, acute chorioamnionitis, chronic chorioamnionitis, lateral flow-based immunoassay, intraamniotic inflammation/infection, interferon-γ –inducible protein 10 (IP-10), MIAC, prematurity, sterile inflammation
Introduction
Intra-amniotic infection and inflammation are causally linked to preterm birth [1-13], which is the leading cause of perinatal morbidity and mortality [14-35]. The gold standard for the diagnosis of intra-amniotic infection has relied on cultivation of bacteria in the amniotic fluid (AF) [36-61]. Amniotic fluid culture detects microbial invasion of the amniotic cavity (MIAC) in approximately 10% of patients with preterm labor and intact membrane [37,38,41,43,47,50,62-80], 30% of patients with preterm prelabor rupture of membrane (PROM) [40,46,49,53,56,60,81-85] and about 50% of pregnant women with acute cervical insufficiency [86-89]. Patients with a short cervix [90,91] or those with idiopathic vaginal bleeding [92] have a frequency of MIAC of approximately 9%.
Several studies have now shown that patients with intra-amniotic inflammation have adverse pregnancy and neonatal outcome, even if there is no evidence of microorganisms in the amniotic cavity, suggesting that the diagnosis of intra-amniotic inflammation is key [57,58,91,93,94].
Multiple biomarkers for the diagnosis of intra-amniotic inflammation have been used, including determinations of cytokines [68,73,94-114], chemokines [115-121], matrix-degrading enzymes [122-129], and other inflammatory mediators [130-140]. Parameters have ranged from a simple amniotic fluid white blood cell (WBC) count [49,70,71,141] to the determination of analytes with immunoassays or bioassays [interleukin-8 (IL-8), chemotaxis] [115,116,142,143]. Amniotic fluid concentrations of IL-6 have been reported by several investigators to be informative and reliable indicators of the prognosis of patients at risk for preterm delivery [49,61,100,144-148]. IL-6 determinations have been performed in most studies, using research immunoassays not available for clinical management. Often, clinical laboratories in hospitals send samples to reference laboratories, and results are not available for days. What is necessary is a rapid test that can inform clinical decision-making. Several investigators have reported a rapid IL-6 test for the diagnosis of adult [149] and neonatal sepsis [150,151], as well as inflammation of the cerebrospinal fluid [152]. Kacerovsky et al. have recently reported the use of a point of care (POC) test for IL-6 in preterm prelabor rupture of membranes (PROM), which uses lateral-flow immunoassays [113]. Other investigators have used determination of IL-6 in vaginal fluid [153,154] as a point of care test.
We have described a new form of intra-amniotic inflammation that occurs in patients with preterm labor, and which is characterized by an elevation of amniotic fluid CXCL-10, rather than IL-6 [155]. This form of intra-amniotic inflammation is associated with chronic chorioamnionitis, anti-fetal HLA maternal sensitization [156], and is thought to represent maternal anti-fetal rejection [157]. Therefore, it may be important to have a rapid test to identify an elevation of CXCL-10 in amniotic fluid.
The objective of this study was to determine the relationship between the amniotic fluid concentrations of IL-6 and CXCL-10 (different markers of intra-amniotic inflammation) determined by lateral-flow immunoassays and conventional enzyme-linked immunosorbent assay (ELISA).
Methods
Study design and participants
A cross-sectional study was conducted by searching the clinical database and bank of biologic samples of Wayne State University, the Detroit Medical Center, and the Perinatology Research Branch of Eunice Kennedy Shriver National Institutes of Child Health and Human Development (NICHD) (Detroit, MI), to identify patients with a diagnosis of spontaneous preterm labor. Patients were included if they met the following criteria: 1) had a singleton gestation; 2) presented with preterm labor; and 3) had a transabdominal amniocentesis performed between 20 and 35 weeks of gestation with microbiologic studies. Patients were excluded from the study if they had: 1) rupture of the chorioamniotic membranes occurred before AF collection; 2) a chromosomal or structural fetal anomaly. In order to have a wide range of IL-6 for the assay comparison, we selected 3 groups of patients in which: 1) preterm labor delivered at term; 2) preterm labor delivered preterm without intra-amniotic infection; and 3) preterm labor and delivered preterm with intra-amniotic infection. All patients provided written informed consent; the use of biologic specimens and clinical data for research purposes was approved by the Institutional Review Boards of NICHD and Wayne State University.
Clinical Definitions
Preterm labor was diagnosed by the presence of at least two regular uterine contractions every 10 minutes in associated with cervical changes in patients with a gestational age between 20 and 36 6/7 weeks which led to preterm delivery (defined as birth prior to the 37th week of gestation). Acute histologic chorioamnionitis was diagnosed based on the presence of neutrophils in the chorionic plate and/or chorioamniotic membranes [158-160]. Intra-amniotic inflammation was diagnosed when IL-6 AF concentration was > 2.6 ng/ml [57]. MIAC was defined according to the results of AF culture. Intra-amniotic infection was defined as a combination of MIAC with intra-amniotic inflammation.
Biological samples and analysis
Patients with preterm labor and intact membranes who underwent transabdominal ultrasound-guided amniocentesis for evaluating possible MIAC (within the standard of care at Hutzel Women's Hospital, Detroit, Michigan) were eligible for the study. AF was transported in a capped sterile syringe to the clinical laboratory where it was cultured for aerobic and anaerobic bacteria, including genital mycoplasmas. Evaluation of white blood cell (WBC) count, glucose concentration, and Gram stain of AF were also performed shortly after collection. AF not required for clinical assessment was centrifuged for 10 min at 4°C shortly after and stored at −70°C until analysis. The presence of intra-amniotic infection inflammation was assessed by determination of AF interleukin-6 (IL-6) concentration by ELISA. AF IL-6 concentrations were determined for research purposes, and such results were not used in patient management.
Analysis of amniotic fluid samples for IL-6 and IP-10 concentrations
AF IL-6 and IP-10 concentrations (ng/ml) were determined both by ELISA and lateral flow-based immunoassay point of care (POC) test. For ELISA, AF concentrations of IL-6 and IP-10 were determined by immunoassays obtained from R&D Systems (Minneapolis, MN, USA). The details of these immunoassays and their performance have been previously described [49,57,96,101,142,161-170]. The point of care determination of AF IL-6 and IP-10 concentrations (ng/ml) was performed using a lateral flow-based immunoassay point of care (POC) test (Milenia QuickLine® IL-6; Milenia Biotec, Bad Nauheim, Germany). Briefly, 100 μL of AF were transferred to the test unit and after 15 min of incubation, 50 μL of buffer was added. In the first step, IL-6 present in the sample binds to a monoclonal anti-human IL-6 antibody (Ab) conjugated to gold particles. The complex of IL-6 and the conjugate continues to migrate through the analytical membrane. A test line and a control line are printed on this membrane. The test line is coated with a second anti-IL-6 Ab directed against a different epitope than the conjugate Ab. Once the complex of IL-6 and the conjugate passes the test line, it forms a sandwich with the coated IL-6 Ab. A band becomes visible PicoScan® densitometry system (Milenia Biotec, Bad Nauheim, Germany). This system measures the intensity of the test band and calculates concentrations according to standard curve. Results are typically available after 20 minutes and can be interpreted both visually and by densitometry. The assay time, volume and other assay characteristics for each method are shown in Table 1.
Table 1.
Comparison of assay characteristics between ELISA and lateral flow-based immunoassay point of care test (POC)
| Interleukin-6 ELISA | Interleukin-6 point of care test | IP-10 ELISA | IP-10 point of care test | |
|---|---|---|---|---|
| Assay time | 5 hours | 20 minutes | 5 hours | 20 minutes |
| Sample volume | 12 μL | 100 μL | 10 μL | 100 μL |
| Sensitivity | < 0.70 pg/ml | 50 pg/ml | 1.67 pg/ml | 100 pg/ml |
| Range of detection | 3.13-300 pg/ml | 50-10,000 pg/ml | 7.8-500 pg/ml | 50-10,000 pg/ml |
| Intra-assay coefficients of variation | 2.9% | 12.1% | 2.8% | 12.1% |
| Inter-assay coefficients of variation | 2.8% | 15.5% | 3.5% | 15.5% |
IP-10 or CXCL-10: interferon-γ –inducible protein 10
ELISA: enzyme-linked immunosorbent assay
Statistical Analysis
The Kolmogorov-Smirnov test was used to assess normality of arithmetic data distributions. The Kruskal-Wallis test for comparisons and the Mann-Whitney U test were used to make comparisons among and between groups for arithmetic variables. Chi-square was used for comparisons of categorical variables. Correlation between AF IL-6 concentrations determined by lateral flow-based immunoassay point of care (POC) and ELISA was assessed using Spearman's correlation coefficients. Bland-Altman plots were constructed to assess between-assay agreement. General linear models were fit to determine coefficients of determination (r2). Statistical analysis was performed using SPSS 19 (IBM Corp, Armonk, NY, USA) and SAS 9.4 (Cary, NC, USA). A p value < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of the study population are displayed in Table 2. Ten of the 20 patients with preterm labor delivered at term. Three of the remaining ten patients who delivered preterm had intra-amniotic infection, and each was delivered at < 32 weeks of gestation. Organisms identified in the AF of these three patients included Gram negative bacilli, Ureaplasma urealyticum and Gemella Morbillorum.
Table 2.
Characteristics of study populations
| Preterm labor (n=20) | |
|---|---|
| Age (years) | 22 (20-25) |
| Parity | 40% (8/20) |
| Body mass index (kg/m2) | 23.3 (21.1-32.3) |
| Gestational age at amniocentesis (weeks) | 30.5 (28.3-31) |
| Gestational age at delivery (weeks) | 26.3 (31.5-39.2) |
| Birthweight (grams) | 2617(1,718-3,002) |
| Amniotic fluid glucose (mg/dl) | 25 (17-30) |
| Amniotic fluid white blood cell (cell/mm) | 0 (0-5) |
| Amniotic fluid IL-6 ELISA (ng/ml) | 1.2 (0.5-6.9) |
| Amniotic fluid IL-6 point of care test (ng/ml) | 0.4 (0.2-1.6) |
| Amniotic fluid IP-10 ELISA (ng/ml) | 1.8 (0.9-3.8) |
| Amniotic fluid IP-10 point of care test (ng/ml) | 1.8 (1.3-3.2) |
| Placental lesions associated with amniotic fluid infection^ | 42% (8/19) |
Data presented as % (N) or median (interquartile range), IL: interleukin, IP: interferon-γ –inducible protein 10 or CXCL 10, MIAC: microbial invasion of the amniotic cavity microbial; ELISA: enzyme-linked immunosorbent assay
placental lesions associated with amniotic fluid infection include acute chorioamnionitis and funisitis.
Correlation among amniotic fluid IL-6 concentrations determined by point of care and standard ELISA techniques
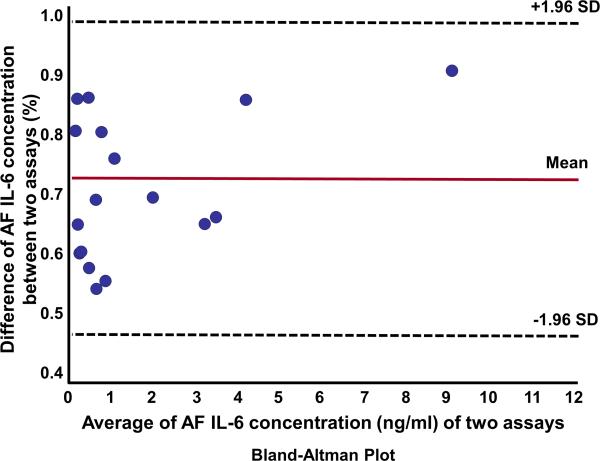
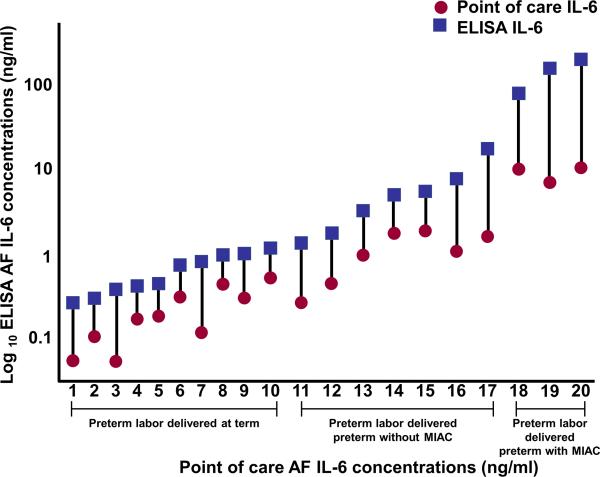
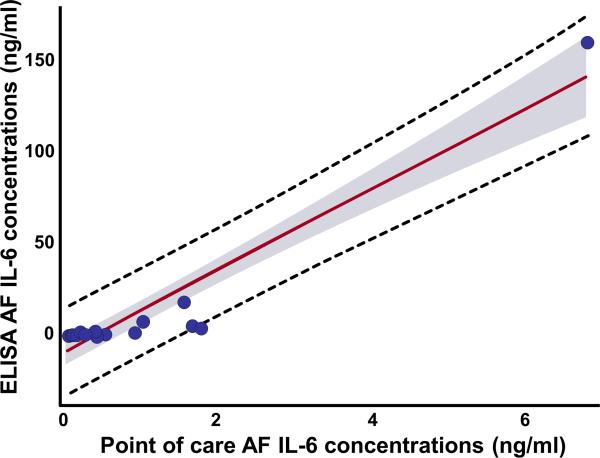
All of the samples had IL-6 concentrations above the lowest limit of detection (sensitivity) for both assays. Two samples from patients with microorganisms in the amniotic cavity had AF IL-6 concentrations that were above the standard threshold of the lateral flow-based immunoassay POC test (concentrations were high and precise calculation would have needed dilution of the sample and a new assay). Excluding these two patients, AF IL-6 concentrations determined using ELISA and the lateral flow-based immunoassay POC test were strongly correlated (Spearman ρ =0.92; p= <0.0001). The Bland-Altman plot analysis (Figure 1) shows that AF IL-6 concentrations determined by the POC test were, on average, approximately 30% lower than those determined by ELISA (Sign rank test for median difference, p < 0.0001). Figure 2 shows that this was a systematic observation, as it was consistent among patients. Overall, 92% of the variability in AF IL-6 as determined by ELISA was explained by the lateral flow-based immunoassay POC test results (r2 0.92, β=21.9, standard error=1.66, p <0.0001) (Figure 3).
Figure 1.
Bland-Altman plot: direct comparison between enzyme-linked immunosorbent assay (ELISA) and lateral flow-based immunoassay point of care (POC) amniotic fluid (AF) interleukin-6 (IL-6) techniques. AF IL-6 concentrations from three patients with preterm labor with microbial invasion of the amniotic cavity (MIAC) were excluded. SD=standard deviation.
Figure 2.
Amniotic fluid (AF) concentrations of interleukin-6 (IL-6) determined by enzyme-linked immunosorbent assay (ELISA) (square) and a lateral flow-based immunoassay point of care (POC) test (circle) of patients with preterm labor. Lateral flow-based immunoassay point of care (POC) AF IL-6 concentrations were significantly lower than those of ELISA in every pair samples.
Figure 3.
Amniotic fluid (AF) interleukin-6 (IL-6) scatter diagram with linear regression line (red line). Dashed line indicates 95% confidence interval. AF IL-6 concentrations from three patients with preterm labor with microbial invasion of the amniotic cavity (MIAC) were excluded.
Correlation among amniotic fluid IP-10 concentrations determined by point of care and standard ELISA techniques
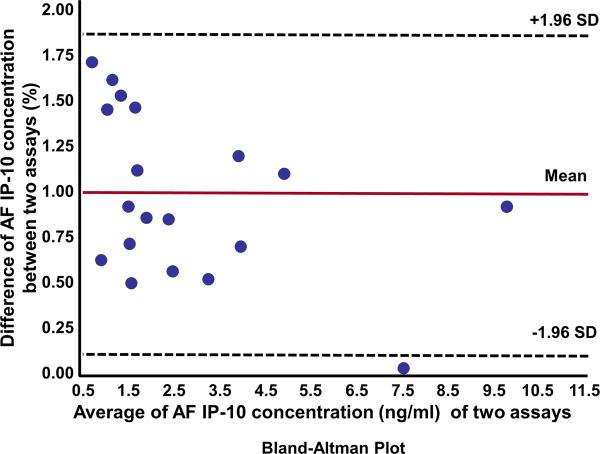
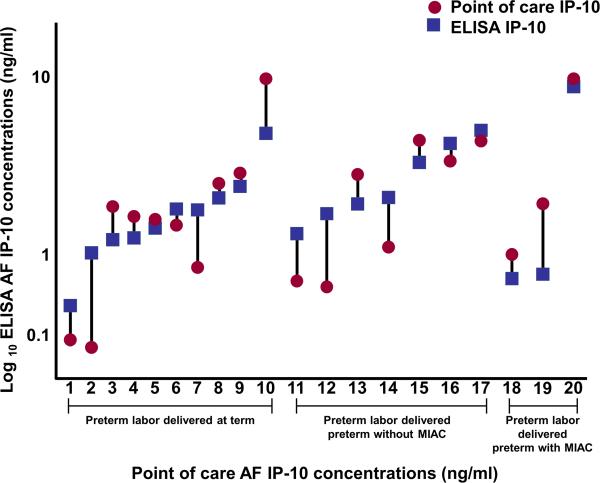
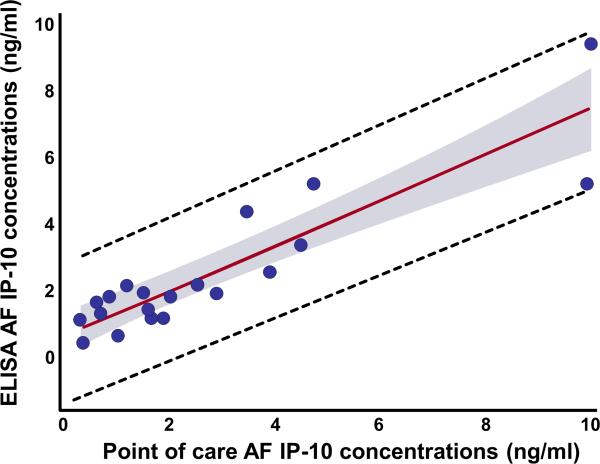
AF IP-10 concentrations determined using the POC test were strongly correlated with those determined by ELISA (Spearman ρ =0.83; p= <0.0001). The Bland-Altman plot for these two assays (Figure 4) shows that IP-10 concentrations were only approximately 7% lower, on average, than those determined by ELISA (Sign rank test for median difference, p = 0.81). Figure 5 demonstrated the actual concentrations in all patients between these 2 techniques. Overall, 80% of the variation in AF IP-10 concentrations determined by ELISA was explained by the lateral flow-based immunoassay POC test results (r2 0.80, β=0.67, standard error=0.08, p <0.0001, Figure 6).
Figure 4.
Bland-Altman plot: direct comparison between enzyme-linked immunosorbent assay (ELISA) and lateral flow-based immunoassay point of care (POC) amniotic fluid (AF) interferon-γ –inducible protein 10 (IP-10 or CXCL 10) techniques. SD=standard deviation.
Figure 5.
Amniotic fluid (AF) concentrations of interferon-γ –inducible protein 10 (IP-10 or CXCL-10) determined by enzyme-linked immunosorbent assay (ELISA) (square) and lateral flow-based immunoassay point of care (POC) test (circle) of patients with preterm labor.
Figure 6.
Amniotic fluid (AF) interferon-γ –inducible protein 10 (IP-10 or CXCL-10) scatter diagram with linear regression line (red line). Dashed line indicates 95% confidence interval.
Discussion
Principal findings of the study
1) The lateral flow-based immunoassay point of care amniotic fluid IL-6 and IP-10 test results were strongly correlated with concentrations determined by ELISA; 2) AF IL-6 concentrations determined by the lateral flow-based immunoassay were, on average, 30% lower than those determined by ELISA, and the median difference between assays was statistically significant (p < 0.0001); and 3) in contrast, AF IP-10 concentrations determined by the lateral flow-based immunoassay POC test were, on average, only 7% lower than those determined by ELISA, and the median difference between assays was not statistically significant (p =0.81). These findings justify the need for further studies about the diagnostic indices and predictive values of these point of care tests.
Point of care test for amniotic fluid IL-6
A large body of evidence indicates that patients with intra-amniotic inflammation are at greater risk for impending preterm delivery and other adverse outcomes, even when the results of AF culture are negative for microorganisms [57,58,91,93,94]. Our group has previously shown that an AF IL-6 concentration ≥ 11.3 ng/ml has a sensitivity of 93% and a specificity of 92% for the identification of positive AF culture, and also that it is predictive of preterm delivery, amniocentesis-to-delivery interval and neonatal morbidity and mortality [50]. Subsequently, the AF IL-6 cut-off of 2.6 ng/ml was proposed to diagnose intra-amniotic inflammation that is associated with a shorter amniocentesis-to-delivery interval, and also with significantly higher risks of adverse neonatal outcomes, even among patients with a negative AF culture [57]. The cut-off of 2.6 ng/ml has been extensively used in the literature by other investigators to identify those at risk for adverse pregnancy outcome in patients with preterm labor and intact membranes [129,171-173].
Patients with an elevated IL-6 but no evidence of microorganisms with cultivation methods and molecular microbiologic techniques are considered to have sterile intra-amniotic inflammation, and are at high risk for adverse pregnancy outcome in the context of preterm labor with intact membranes [58,59], preterm PROM [60], and a short cervix [91]. Therefore, the detection of an elevated IL-6 seems to be clinically important.
In the present study, we demonstrated that AF IL-6 concentrations measured using a lateral flow-based immunoassay POC test were strongly correlated with those determined using the conventional ELISA technique. These observations are consistent with findings of studies involving adult [149]/neonatal sepsis [150,151] and subarachnoid hemorrhage [152], which also reported that IL-6 concentrations measured with a point of care test correlated strongly with those measured by ELISA.
In addition, prior studies with this point of care test for IL-6 have shown that results correlate with the microbial burden of Ureaplasma sp in AF from patients with preterm PROM [113], and that a cut-off of 1,000 pg/ml had a 50% sensitivity and a 95% specificity for the identification of MIAC or both MIAC and acute histological chorioamnionitis in these patients [113]. A high negative predictive value (97%) has also been reported for a point of care vaginal fluid IL-6 concentration in identifying intra-amniotic inflammation in patients with rupture of membranes [154].
The ELISA method was chosen for the comparison since this technique is currently considered the gold standard for IL-6 determination. However, ELISA results are not practical, because they are not available in time for clinical decision-making. In contrast, the point of care IL-6 assay allows IL-6 determinations within 20 minutes and might be useful in some institutions that are not able to perform IL-6 ELISA rapidly. The assay characteristics are different; the point of care test can measure IL-6 between 0.05–10 ng/ml for AF IL-6, while the IL-6 ELISA has a range between 0.003 ng/ml and 0.3 ng/ml. Although the assay sensitivity of the latter is much higher, repeated assays with further sample dilutions would take more time to obtain valid assay values. The standard threshold of IL-6 point of care test is 10 ng/ml, however, from a clinical perspective this threshold is acceptable, since most patients with intra-amniotic inflammation and adverse perinatal outcomes have AF IL-6 concentrations > 2.6 ng/ml. Moreover, there would be no difference in the clinical management of patients with an IL-6 +/− 10.
Amniotic fluid IP-10 and preterm labor: a point of care test for the identification of intra-amniotic inflammation
We have previously reported that a subset of patients with preterm labor have a different form of intra-amniotic inflammation that is associated with elevated AF IP-10 concentrations [155] and a higher prevalence of chronic chorioamnionitis, the most common placental lesion in late spontaneous preterm birth. This lesion is characterized by maternal T-cell infiltration of the chorion laeve and amnion, and resembles allograft rejection [157]. We have reported that chronic chorioamnionitis is associated with anti-fetal HLA maternal sensitization [156] and complement deposition in umbilical vein endothelium [155], which is associated with a novel form of fetal systemic inflammation characterized by overexpression of T cell chemokines, such as IP-10 or CXCL-10 [174]. An elevation of mid-trimester AF IP-10 concentration is associated with late (but not early) spontaneous preterm delivery [170]. Thus, it is possible that patients with an elevated CXCL-10/IP-10 are at increased risk for spontaneous preterm delivery. Similar to IL-6, ELISA is currently the gold standard for assessment of AF IP-10. Our observations in this study support that AF IP-10 determined by the POC test is strongly correlated with that determined by ELISA. Further studies are warranted to determine the diagnostic performance of IP-10 by the POC test in the identification of adverse obstetrical outcomes.
A point of care test for the identification of intra-amniotic inflammation
A simple definition for point of care testing is: “Diagnostic testing performed at or near the site of patients care” [175]. This testing is designed to be quick, readily available, accurate, and useful for clinical decision making and considered valuable to increase clinical efficiency and improve medical and economic outcomes [175-178]. The AF lateral flow-based immunoassay point of care (POC) fulfills most of the criteria proposed to assess an optimal POC, namely: 1) simple testing methodology; 2) rapid availability of the results (up to 20 minutes); 3) easy interpretation of the results; 4) low maintenance, because the kit can be stored at room temperature; 5) strong correlation with standard laboratory procedures (ELISA); and 6) low cost, because there is no need for capital equipment and the market price can be driven by need. Larger studies are needed to determine whether other criteria pertaining to clinical utility and cost-benefit are satisfied.
Conclusions
A POC test using lateral-flow based immunoassay for the determination of IL-6 and IP-10 concentrations in amniotic fluid yields results that are strongly correlated with those determined by ELISA. Further studies are warranted to determine the diagnostic and prognostic performance of these tests in clinical obstetrics.
Acknowledgement
This research was supported, in part, by the Perinatology Research Branch, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services (NICHD/NIH); and, in part, with Federal funds from NICHD, NIH under Contract No. HHSN275201300006C.
Footnotes
Declaration of Interest: Authors declare no conflict of interest
References
- 1.Romero R, Mazor M. Infection and preterm labor. Clin Obstet Gynecol. 1988;31:553–584. doi: 10.1097/00003081-198809000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Gibbs RS, Romero R, Hillier SL, et al. A review of premature birth and subclinical infection. Am J Obstet Gynecol. 1992;166:1515–1528. doi: 10.1016/0002-9378(92)91628-n. [DOI] [PubMed] [Google Scholar]
- 3.Romero R, Mazor M, Munoz H, et al. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414–429. doi: 10.1111/j.1749-6632.1994.tb21771.x. [DOI] [PubMed] [Google Scholar]
- 4.Romero R, Gomez R, Mazor M, et al. The preterm labor syndrome. In: Elder MG, Romero R, Lamont RF, editors. Preterm labor. Churchill Livingstone; New York: 1997. pp. 29–49. [Google Scholar]
- 5.Romero R, Gomez R, Chaiworapongsa T, et al. The role of infection in preterm labour and delivery. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):41–56. doi: 10.1046/j.1365-3016.2001.00007.x. [DOI] [PubMed] [Google Scholar]
- 6.Romero R, Espinoza J, Kusanovic JP, et al. The preterm parturition syndrome. BJOG. 2006;113(Suppl 3):17–42. doi: 10.1111/j.1471-0528.2006.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romero R, Espinoza J, Goncalves LF, et al. The role of inflammation and infection in preterm birth. Semin Reprod Med. 2007;25:21–39. doi: 10.1055/s-2006-956773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romero R, Lockwood CJ. Pathogenesis of Spontaneous Preterm Labor. In: Creasy RK, Resnik R, Iams J, editors. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. Sixth ed. Elsevier; Philadelphia: 2009. pp. 521–543. [Google Scholar]
- 10.Kemp MW, Saito M, Newnham JP, et al. Preterm birth, infection, and inflammation advances from the study of animal models. Reproductive sciences. 2010;17:619–628. doi: 10.1177/1933719110373148. [DOI] [PubMed] [Google Scholar]
- 11.Bastek JA, Gomez LM, Elovitz MA. The role of inflammation and infection in preterm birth. Clin Perinatol. 2011;38:385–406. doi: 10.1016/j.clp.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Agrawal V, Hirsch E. Intrauterine infection and preterm labor. Semin Fetal Neonatal Med. 2012;17:12–19. doi: 10.1016/j.siny.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science (accepted) 2014 doi: 10.1126/science.1251816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 15.March of dimes (2009) Premature Birth.
- 16.O'Shea TM, Allred EN, Dammann O, et al. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev. 2009;85:719–725. doi: 10.1016/j.earlhumdev.2009.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deutsch A, Deutsch E, Totten C, et al. Maternal and neonatal outcomes based on the gestational age of midtrimester preterm premature rupture of membranes. J Matern Fetal Neonatal Med. 2010;23:1429–1434. doi: 10.3109/14767051003678069. [DOI] [PubMed] [Google Scholar]
- 18.Picone S, Paolillo P. Neonatal outcomes in a population of late-preterm infants. J Matern Fetal Neonatal Med. 2010;23(Suppl 3):116–120. doi: 10.3109/14767058.2010.509921. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization . Born too soon: the global action report in preterm birth. WHO Library Cataloguing-in-Publication: World Health Organization; 2012. [Google Scholar]
- 20.Bastek JA, Sammel MD, Rebele EC, et al. The effects of a preterm labor episode prior to 34 weeks are evident in late preterm outcomes, despite the administration of betamethasone. Am J Obstet Gynecol. 2010;203:140, e141–147. doi: 10.1016/j.ajog.2010.02.065. [DOI] [PubMed] [Google Scholar]
- 21.Teune MJ, van Wassenaer AG, van Dommelen P, et al. Perinatal risk indicators for long-term neurological morbidity among preterm neonates. Am J Obstet Gynecol. 2011;204:396, e391–396, e314. doi: 10.1016/j.ajog.2011.02.055. [DOI] [PubMed] [Google Scholar]
- 22.Kamath BD, Marcotte MP, DeFranco EA. Neonatal morbidity after documented fetal lung maturity in late preterm and early term infants. Am J Obstet Gynecol. 2011;204:518, e511–518. doi: 10.1016/j.ajog.2011.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 24.Keunen K, Kersbergen KJ, Groenendaal F, et al. Brain tissue volumes in preterm infants: prematurity, perinatal risk factors and neurodevelopmental outcome: a systematic review. J Matern Fetal Neonatal Med. 2012;25(Suppl 1):89–100. doi: 10.3109/14767058.2012.664343. [DOI] [PubMed] [Google Scholar]
- 25.Ferrari F, Gallo C, Pugliese M, et al. Preterm birth and developmental problems in the preschool age. Part I: minor motor problems. J Matern Fetal Neonatal Med. 2012;25:2154–2159. doi: 10.3109/14767058.2012.696164. [DOI] [PubMed] [Google Scholar]
- 26.Gulati S, Agrawal S, Raghunandan C, et al. Maternal serum interleukin-6 and its association with clinicopathological infectious morbidity in preterm premature rupture of membranes: a prospective cohort study. J Matern Fetal Neonatal Med. 2012;25:1428–1432. doi: 10.3109/14767058.2011.638952. [DOI] [PubMed] [Google Scholar]
- 27.Grobman WA, Lai Y, Rouse DJ, et al. The association of cerebral palsy and death with small -for-gestational-age birthweight in preterm neonates by individualized and population-based percentiles. Am J Obstet Gynecol. 2013;209:340, e341–345. doi: 10.1016/j.ajog.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamilton BE, Hoyert DL, Martin JA, et al. Annual summary of vital statistics: 2010-2011. Pediatrics. 2013;131:548–558. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun L, Yue H, Sun B, et al. Estimation of birth population-based perinatal-neonatal mortality and preterm rate in China from a regional survey in 2010. J Matern Fetal Neonatal Med. 2013;26:1641–1648. doi: 10.3109/14767058.2013.794208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Acaia B, Crovetto F, Ossola MW, et al. Predictive factors for neonatal survival in women with periviable preterm rupture of the membranes. J Matern Fetal Neonatal Med. 2013;26:1628–1634. doi: 10.3109/14767058.2013.794206. [DOI] [PubMed] [Google Scholar]
- 31.Strunk T, Inder T, Wang X, et al. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infect Dis. 2014;14:751–762. doi: 10.1016/S1473-3099(14)70710-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawn JE, Blencowe H, Oza S, et al. Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384:189–205. doi: 10.1016/S0140-6736(14)60496-7. [DOI] [PubMed] [Google Scholar]
- 33.Herber-Jonat S, Streiftau S, Knauss E, et al. Long-term outcome at age 7-10 years after extreme prematurity - a prospective, two centre cohort study of children born before 25 completed weeks of gestation (1999-2003). J Matern Fetal Neonatal Med. 2014 doi: 10.3109/14767058.2013.871699. [DOI] [PubMed] [Google Scholar]
- 34.Bastek JA, Weber AL, McShea MA, et al. Prenatal inflammation is associated with adverse neonatal outcomes. Am J Obstet Gynecol. 2014;210:450, e451–410. doi: 10.1016/j.ajog.2013.12.024. [DOI] [PubMed] [Google Scholar]
- 35.Manuck TA, Sheng X, Yoder BA, et al. Correlation between initial neonatal and early childhood outcomes following preterm birth. Am J Obstet Gynecol. 2014;210:426, e421–429. doi: 10.1016/j.ajog.2014.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garite TJ, Freeman RK, Linzey EM, et al. The use of amniocentesis in patients with premature rupture of membranes. Obstet Gynecol. 1979;54:226–230. [PubMed] [Google Scholar]
- 37.Bobitt JR, Hayslip CC, Damato JD. Amniotic fluid infection as determined by transabdominal amniocentesis in patients with intact membranes in premature labor. Am J Obstet Gynecol. 1981;140:947–952. doi: 10.1016/0002-9378(81)90090-9. [DOI] [PubMed] [Google Scholar]
- 38.Wallace RL, Herrick CN. Amniocentesis in the evaluation of premature labor. Obstet Gynecol. 1981;57:483–486. [PubMed] [Google Scholar]
- 39.Minkoff H. Prematurity: infection as an etiologic factor. Obstet Gynecol. 1983;62:137–144. [PubMed] [Google Scholar]
- 40.Cotton DB, Hill LM, Strassner HT, et al. Use of amniocentesis in preterm gestation with ruptured membranes. Obstet Gynecol. 1984;63:38–43. [PubMed] [Google Scholar]
- 41.Leigh J, Garite TJ. Amniocentesis and the management of premature labor. Obstet Gynecol. 1986;67:500–506. [PubMed] [Google Scholar]
- 42.Romero R, Quintero R, Oyarzun E, et al. Intraamniotic infection and the onset of labor in preterm premature rupture of the membranes. Am J Obstet Gynecol. 1988;159:661–666. doi: 10.1016/s0002-9378(88)80030-9. [DOI] [PubMed] [Google Scholar]
- 43.Romero R, Emamian M, Quintero R, et al. The value and limitations of the Gram stain examination in the diagnosis of intraamniotic infection. Am J Obstet Gynecol. 1988;159:114–119. doi: 10.1016/0002-9378(88)90503-0. [DOI] [PubMed] [Google Scholar]
- 44.Romero R, Mazor M, Wu YK, et al. Infection in the pathogenesis of preterm labor. Semin Perinatol. 1988;12:262–279. [PubMed] [Google Scholar]
- 45.Asrat T, Nageotte MP, Garite TJ, et al. Gram stain results from amniocentesis in patients with preterm premature rupture of membranes--comparison of maternal and fetal characteristics. Am J Obstet Gynecol. 1990;163:887–889. doi: 10.1016/0002-9378(90)91089-u. [DOI] [PubMed] [Google Scholar]
- 46.Dudley J, Malcolm G, Ellwood D. Amniocentesis in the management of preterm premature rupture of the membranes. Aust N Z J Obstet Gynaecol. 1991;31:331–336. doi: 10.1111/j.1479-828x.1991.tb02814.x. [DOI] [PubMed] [Google Scholar]
- 47.Romero R, Quintero R, Nores J, et al. Amniotic fluid white blood cell count: a rapid and simple test to diagnose microbial invasion of the amniotic cavity and predict preterm delivery. Am J Obstet Gynecol. 1991;165:821–830. doi: 10.1016/0002-9378(91)90423-o. [DOI] [PubMed] [Google Scholar]
- 48.Romero R, Mazor M, Morrotti R, et al. Infection and labor. VII. Microbial invasion of the amniotic cavity in spontaneous rupture of membranes at term. Am J Obstet Gynecol. 1992;166:129–133. doi: 10.1016/0002-9378(92)91845-2. [DOI] [PubMed] [Google Scholar]
- 49.Romero R, Yoon BH, Mazor M, et al. A comparative study of the diagnostic performance of amniotic fluid glucose, white blood cell count, interleukin-6, and gram stain in the detection of microbial invasion in patients with preterm premature rupture of membranes. Am J Obstet Gynecol. 1993;169:839–851. doi: 10.1016/0002-9378(93)90014-a. [DOI] [PubMed] [Google Scholar]
- 50.Romero R, Yoon BH, Mazor M, et al. The diagnostic and prognostic value of amniotic fluid white blood cell count, glucose, interleukin-6, and gram stain in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 1993;169:805–816. doi: 10.1016/0002-9378(93)90009-8. [DOI] [PubMed] [Google Scholar]
- 51.Romero R, Nores J, Mazor M, et al. Microbial invasion of the amniotic cavity during term labor. Prevalence and clinical significance. J Reprod Med. 1993;38:543–548. [PubMed] [Google Scholar]
- 52.Gomez R, Romero R, Galasso M, et al. The value of amniotic fluid interleukin-6, white blood cell count, and gram stain in the diagnosis of microbial invasion of the amniotic cavity in patients at term. Am J Reprod Immunol. 1994;32:200–210. doi: 10.1111/j.1600-0897.1994.tb01115.x. [DOI] [PubMed] [Google Scholar]
- 53.Blackwell SC, Berry SM. Role of amniocentesis for the diagnosis of subclinical intra-amniotic infection in preterm premature rupture of the membranes. Curr Opin Obstet Gynecol. 1999;11:541–547. doi: 10.1097/00001703-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 54.Jacobsson B, Mattsby-Baltzer I, Andersch B, et al. Microbial invasion and cytokine response in amniotic fluid in a Swedish population of women in preterm labor. Acta Obstet Gynecol Scand. 2003;82:120–128. doi: 10.1034/j.1600-0412.2003.00047.x. [DOI] [PubMed] [Google Scholar]
- 55.Jacobsson B, Mattsby-Baltzer I, Andersch B, et al. Microbial invasion and cytokine response in amniotic fluid in a Swedish population of women with preterm prelabor rupture of membranes. Acta Obstet Gynecol Scand. 2003;82:423–431. doi: 10.1034/j.1600-0412.2003.00157.x. [DOI] [PubMed] [Google Scholar]
- 56.Broekhuizen FF, Gilman M, Hamilton PR. Amniocentesis for gram stain and culture in preterm premature rupture of the membranes. Obstet Gynecol. 1985;66:316–321. [PubMed] [Google Scholar]
- 57.Yoon BH, Romero R, Moon JB, et al. Clinical significance of intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2001;185:1130–1136. doi: 10.1067/mob.2001.117680. [DOI] [PubMed] [Google Scholar]
- 58.Romero R, Miranda J, Chaiworapongsa T, et al. Sterile Intra-Amniotic Inflammation is More Frequent than Microbial-Associated Intra-amniotic Inflammation in Preterm Labor with Intact Membranes. Am J Reprod Immunol (Submitted) 2014 doi: 10.1111/aji.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Romero R, Miranda J, Chaiworapongsa T, et al. A novel molecular microbiologic technique for the rapid diagnosis of microbial invasion of the amniotic cavity and intra-amniotic infection in preterm labor with intact membranes. Am J Reprod Immunol. 2014;71:330–358. doi: 10.1111/aji.12189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Romero R, Miranda J, Chaemsaithong P, et al. Sterile and Microbial-associated Intra-amniotic Inflammation in Preterm Prelabor Rupture of Membranes. J Matern Fetal Neonatal Med (submitted) 2014 doi: 10.3109/14767058.2014.958463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Romero R, Kadar N, Miranda J, et al. The diagnostic performance of the Mass Restricted (MR) score in the identification of microbial invasion of the amniotic cavity or intra-amniotic inflammation is not superior to amniotic fluid interleukin-6. J Matern Fetal Neonatal Med. 2014;27:757–769. doi: 10.3109/14767058.2013.844123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miller JM, Jr., Pupkin MJ, Hill GB. Bacterial colonization of amniotic fluid from intact fetal membranes. Am J Obstet Gynecol. 1980;136:796–804. doi: 10.1016/0002-9378(80)90458-5. [DOI] [PubMed] [Google Scholar]
- 63.Wahbeh CJ, Hill GB, Eden RD, et al. Intra-amniotic bacterial colonization in premature labor. Am J Obstet Gynecol. 1984;148:739–743. doi: 10.1016/0002-9378(84)90558-1. [DOI] [PubMed] [Google Scholar]
- 64.Hameed C, Tejani N, Verma UL, et al. Silent chorioamnionitis as a cause of preterm labor refractory to tocolytic therapy. Am J Obstet Gynecol. 1984;149:726–730. doi: 10.1016/0002-9378(84)90111-x. [DOI] [PubMed] [Google Scholar]
- 65.Gravett MG, Hummel D, Eschenbach DA, et al. Preterm labor associated with subclinical amniotic fluid infection and with bacterial vaginosis. Obstet Gynecol. 1986;67:229–237. doi: 10.1097/00006250-198602000-00013. [DOI] [PubMed] [Google Scholar]
- 66.Romero R, Sirtori M, Oyarzun E, et al. Infection and labor. V. Prevalence, microbiology, and clinical significance of intraamniotic infection in women with preterm labor and intact membranes. Am J Obstet Gynecol. 1989;161:817–824. doi: 10.1016/0002-9378(89)90409-2. [DOI] [PubMed] [Google Scholar]
- 67.Skoll MA, Moretti ML, Sibai BM. The incidence of positive amniotic fluid cultures in patients preterm labor with intact membranes. Am J Obstet Gynecol. 1989;161:813–816. doi: 10.1016/0002-9378(89)90407-9. [DOI] [PubMed] [Google Scholar]
- 68.Romero R, Avila C, Santhanam U, et al. Amniotic fluid interleukin 6 in preterm labor. Association with infection. J Clin Invest. 1990;85:1392–1400. doi: 10.1172/JCI114583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Romero R, Jimenez C, Lohda AK, et al. Amniotic fluid glucose concentration: a rapid and simple method for the detection of intraamniotic infection in preterm labor. Am J Obstet Gynecol. 1990;163:968–974. doi: 10.1016/0002-9378(90)91106-m. [DOI] [PubMed] [Google Scholar]
- 70.Gauthier DW, Meyer WJ, Bieniarz A. Correlation of amniotic fluid glucose concentration and intraamniotic infection in patients with preterm labor or premature rupture of membranes. Am J Obstet Gynecol. 1991;165:1105–1110. doi: 10.1016/0002-9378(91)90480-f. [DOI] [PubMed] [Google Scholar]
- 71.Coultrip LL, Grossman JH. Evaluation of rapid diagnostic tests in the detection of microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 1992;167:1231–1242. doi: 10.1016/s0002-9378(11)91694-9. [DOI] [PubMed] [Google Scholar]
- 72.Watts DH, Krohn MA, Hillier SL, et al. The association of occult amniotic fluid infection with gestational age and neonatal outcome among women in preterm labor. Obstet Gynecol. 1992;79:351–357. doi: 10.1097/00006250-199203000-00005. [DOI] [PubMed] [Google Scholar]
- 73.Gomez R, Romero R, Ghezzi F, et al. The fetal inflammatory response syndrome. Am J Obstet Gynecol. 1998;179:194–202. doi: 10.1016/s0002-9378(98)70272-8. [DOI] [PubMed] [Google Scholar]
- 74.Hussey MJ, Levy ES, Pombar X, et al. Evaluating rapid diagnostic tests of intra-amniotic infection: Gram stain, amniotic fluid glucose level, and amniotic fluid to serum glucose level ratio. Am J Obstet Gynecol. 1998;179:650–656. doi: 10.1016/s0002-9378(98)70059-6. [DOI] [PubMed] [Google Scholar]
- 75.Rizzo G, Capponi A, Vlachopoulou A, et al. Ultrasonographic assessment of the uterine cervix and interleukin-8 concentrations in cervical secretions predict intrauterine infection in patients with preterm labor and intact membranes. Ultrasound Obstet Gynecol. 1998;12:86–92. doi: 10.1046/j.1469-0705.1998.12020086.x. [DOI] [PubMed] [Google Scholar]
- 76.Yoon BH, Chang JW, Romero R. Isolation of Ureaplasma urealyticum from the amniotic cavity and adverse outcome in preterm labor. Obstet Gynecol. 1998;92:77–82. doi: 10.1016/s0029-7844(98)00122-7. [DOI] [PubMed] [Google Scholar]
- 77.Elimian A, Figueroa R, Canterino J, et al. Amniotic fluid complement C3 as a marker of intra-amniotic infection. Obstet Gynecol. 1998;92:72–76. doi: 10.1016/s0029-7844(98)00123-9. [DOI] [PubMed] [Google Scholar]
- 78.Oyarzun E, Yamamoto M, Kato S, et al. Specific detection of 16 micro-organisms in amniotic fluid by polymerase chain reaction and its correlation with preterm delivery occurrence. Am J Obstet Gynecol. 1998;179:1115–1119. doi: 10.1016/s0002-9378(98)70115-2. [DOI] [PubMed] [Google Scholar]
- 79.Gonzalez-Bosquet E, Cerqueira MJ, Dominguez C, et al. Amniotic fluid glucose and cytokines values in the early diagnosis of amniotic infection in patients with preterm labor and intact membranes. J Matern Fetal Med. 1999;8:155–158. doi: 10.1002/(SICI)1520-6661(199907/08)8:4<155::AID-MFM3>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 80.Locksmith GJ, Clark P, Duff P, et al. Amniotic fluid matrix metalloproteinase-9 levels in women with preterm labor and suspected intra-amniotic infection. Obstet Gynecol. 1999;94:1–6. doi: 10.1016/s0029-7844(99)00011-3. [DOI] [PubMed] [Google Scholar]
- 81.Garite TJ, Freeman RK. Chorioamnionitis in the preterm gestation. Obstet Gynecol. 1982;59:539–545. [PubMed] [Google Scholar]
- 82.Zlatnik FJ, Cruikshank DP, Petzold CR, et al. Amniocentesis in the identification of inapparent infection in preterm patients with premature rupture of the membranes. J Reprod Med. 1984;29:656–660. [PubMed] [Google Scholar]
- 83.Feinstein SJ, Vintzileos AM, Lodeiro JG, et al. Amniocentesis with premature rupture of membranes. Obstet Gynecol. 1986;68:147–152. [PubMed] [Google Scholar]
- 84.Romero R, Emamian M, Wan M, et al. The value of the leukocyte esterase test in diagnosing intra-amniotic infection. Am J Perinatol. 1988;5:64–69. doi: 10.1055/s-2007-999657. [DOI] [PubMed] [Google Scholar]
- 85.Yoon BH, Jun JK, Park KH, et al. Serum C-reactive protein, white blood cell count, and amniotic fluid white blood cell count in women with preterm premature rupture of membranes. Obstet Gynecol. 1996;88:1034–1040. doi: 10.1016/s0029-7844(96)00339-0. [DOI] [PubMed] [Google Scholar]
- 86.Romero R, Gonzalez R, Sepulveda W, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol. 1992;167:1086–1091. doi: 10.1016/s0002-9378(12)80043-3. [DOI] [PubMed] [Google Scholar]
- 87.Mays JK, Figueroa R, Shah J, et al. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95:652–655. doi: 10.1016/s0029-7844(99)00633-x. [DOI] [PubMed] [Google Scholar]
- 88.Lee SE, Romero R, Park CW, et al. The frequency and significance of intraamniotic inflammation in patients with cervical insufficiency. Am J Obstet Gynecol. 2008;198:633, e631–638. doi: 10.1016/j.ajog.2007.11.047. [DOI] [PubMed] [Google Scholar]
- 89.Bujold E, Morency AM, Rallu F, et al. Bacteriology of amniotic fluid in women with suspected cervical insufficiency. J Obstet Gynaecol Can. 2008;30:882–887. doi: 10.1016/S1701-2163(16)32967-X. [DOI] [PubMed] [Google Scholar]
- 90.Hassan S, Romero R, Hendler I, et al. A sonographic short cervix as the only clinical manifestation of intra-amniotic infection. J Perinat Med. 2006;34:13–19. doi: 10.1515/JPM.2006.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Romero R, Miranda J, Chaiworapongsa T, et al. Rapid Diagnosis of Microbial Invasion of the Amniotic Cavity in Asymptomatic Patients with a Sonographic Short Cervix. J Matern Fetal Neonatal Med (submitted) 2014 [Google Scholar]
- 92.Gomez R, Romero R, Nien JK, et al. Idiopathic vaginal bleeding during pregnancy as the only clinical manifestation of intrauterine infection. J Matern Fetal Neonatal Med. 2005;18:31–37. doi: 10.1080/14767050500217863. [DOI] [PubMed] [Google Scholar]
- 93.Lee SE, Romero R, Jung H, et al. The intensity of the fetal inflammatory response in intraamniotic inflammation with and without microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 2007;197:294, e291–296. doi: 10.1016/j.ajog.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 94.Combs CA, Gravett M, Garite TJ, et al. Amniotic fluid infection, inflammation, and colonization in preterm labor with intact membranes. Am J Obstet Gynecol. 2014;210:125, e121–125, e115. doi: 10.1016/j.ajog.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 95.Romero R, Manogue KR, Mitchell MD, et al. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am J Obstet Gynecol. 1989;161:336–341. doi: 10.1016/0002-9378(89)90515-2. [DOI] [PubMed] [Google Scholar]
- 96.Romero R, Sepulveda W, Kenney JS, et al. Interleukin 6 determination in the detection of microbial invasion of the amniotic cavity. Ciba Found Symp. 1992;167:205–220. doi: 10.1002/9780470514269.ch13. discussion 220-203. [DOI] [PubMed] [Google Scholar]
- 97.Romero R, Mazor M, Sepulveda W, et al. Tumor necrosis factor in preterm and term labor. Am J Obstet Gynecol. 1992;166:1576–1587. doi: 10.1016/0002-9378(92)91636-o. [DOI] [PubMed] [Google Scholar]
- 98.Romero R, Mazor M, Brandt F, et al. Interleukin-1 alpha and interleukin-1 beta in preterm and term human parturition. Am J Reprod Immunol. 1992;27:117–123. doi: 10.1111/j.1600-0897.1992.tb00737.x. [DOI] [PubMed] [Google Scholar]
- 99.Hillier SL, Witkin SS, Krohn MA, et al. The relationship of amniotic fluid cytokines and preterm delivery, amniotic fluid infection, histologic chorioamnionitis, and chorioamnion infection. Obstet Gynecol. 1993;81:941–948. [PubMed] [Google Scholar]
- 100.Romero R, Yoon BH, Kenney JS, et al. Amniotic fluid interleukin-6 determinations are of diagnostic and prognostic value in preterm labor. Am J Reprod Immunol. 1993;30:167–183. doi: 10.1111/j.1600-0897.1993.tb00618.x. [DOI] [PubMed] [Google Scholar]
- 101.Yoon BH, Romero R, Kim CJ, et al. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol. 1995;172:960–970. doi: 10.1016/0002-9378(95)90028-4. [DOI] [PubMed] [Google Scholar]
- 102.Romero R, Gomez R, Ghezzi F, et al. A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am J Obstet Gynecol. 1998;179:186–193. doi: 10.1016/s0002-9378(98)70271-6. [DOI] [PubMed] [Google Scholar]
- 103.Athayde N, Romero R, Maymon E, et al. Interleukin 16 in pregnancy, parturition, rupture of fetal membranes, and microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 2000;182:135–141. doi: 10.1016/s0002-9378(00)70502-3. [DOI] [PubMed] [Google Scholar]
- 104.Leslie KK, Lee SL, Woodcock SM, et al. Acute intrauterine infection results in an imbalance between pro- and anti-inflammatory cytokines in the pregnant rabbit. Am J Reprod Immunol. 2000;43:305–311. doi: 10.1111/j.8755-8920.2000.430510.x. [DOI] [PubMed] [Google Scholar]
- 105.Blank V, Hirsch E, Challis JR, et al. Cytokine signaling, inflammation, innate immunity and preterm labour - a workshop report. Placenta. 2008;29(Suppl A):S102–104. doi: 10.1016/j.placenta.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 106.Ilievski V, Hirsch E. Synergy between viral and bacterial toll-like receptors leads to amplification of inflammatory responses and preterm labor in the mouse. Biol Reprod. 2010;83:767–773. doi: 10.1095/biolreprod.110.085464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cobo T, Kacerovsky M, Palacio M, et al. Intra-amniotic inflammatory response in subgroups of women with preterm prelabor rupture of the membranes. PLoS One. 2012;7:e43677. doi: 10.1371/journal.pone.0043677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cobo T, Kacerovsky M, Holst RM, et al. Intra-amniotic inflammation predicts microbial invasion of the amniotic cavity but not spontaneous preterm delivery in preterm prelabor membrane rupture. Acta Obstet Gynecol Scand. 2012;91:930–935. doi: 10.1111/j.1600-0412.2012.01427.x. [DOI] [PubMed] [Google Scholar]
- 109.Kacerovsky M, Musilova I, Jacobsson B, et al. Cervical and vaginal fluid soluble Toll-like receptor 2 in pregnancies complicated by preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2014:1–25. doi: 10.3109/14767058.2014.944859. [DOI] [PubMed] [Google Scholar]
- 110.Cobo T, Jacobsson B, Kacerovsky M, et al. Systemic and local inflammatory response in women with preterm prelabor rupture of membranes. PLoS One. 2014;9:e85277. doi: 10.1371/journal.pone.0085277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kacerovsky M, Musilova I, Jacobsson B, et al. Vaginal fluid IL-6 and IL-8 levels in pregnancies complicated by preterm prelabor membrane ruptures. J Matern Fetal Neonatal Med. 2014:1–7. doi: 10.3109/14767058.2014.917625. [DOI] [PubMed] [Google Scholar]
- 112.Kacerovsky M, Musilova I, Jacobsson B, et al. Cervical fluid IL-6 and IL-8 levels in pregnancies complicated by preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2014 doi: 10.3109/14767058.2014.908179. [DOI] [PubMed] [Google Scholar]
- 113.Kacerovsky M, Musilova I, Hornychova H, et al. Bedside assessment of amniotic fluid interleukin-6 in preterm prelabor rupture of membranes. Am J Obstet Gynecol. 2014 doi: 10.1016/j.ajog.2014.03.069. [DOI] [PubMed] [Google Scholar]
- 114.Kacerovsky M, Musilova I, Andrys C, et al. Prelabor rupture of membranes betwee n 34 and 37 weeks: the intraamniotic inflammatory response and neonatal outcomes. Am J Obstet Gynecol. 2014;210:325, e321–325, e310. doi: 10.1016/j.ajog.2013.10.882. [DOI] [PubMed] [Google Scholar]
- 115.Romero R, Ceska M, Avila C, et al. Neutrophil attractant/activating peptide-1/interleukin-8 in term and preterm parturition. Am J Obstet Gynecol. 1991;165:813–820. doi: 10.1016/0002-9378(91)90422-n. [DOI] [PubMed] [Google Scholar]
- 116.Cherouny PH, Pankuch GA, Romero R, et al. Neutrophil attractant/activating peptide-1/interleukin-8: association with histologic chorioamnionitis, preterm delivery, and bioactive amniotic fluid leukoattractants. Am J Obstet Gynecol. 1993;169:1299–1303. doi: 10.1016/0002-9378(93)90297-v. [DOI] [PubMed] [Google Scholar]
- 117.Romero R, Gomez R, Galasso M, et al. Macrophage inflammatory protein-1 alpha in term and preterm parturition: effect of microbial invasion of the amniotic cavity. Am J Reprod Immunol. 1994;32:108–113. doi: 10.1111/j.1600-0897.1994.tb01101.x. [DOI] [PubMed] [Google Scholar]
- 118.Cohen J, Ghezzi F, Romero R, et al. GRO alpha in the fetomaternal and amniotic fluid compartments during pregnancy and parturition. Am J Reprod Immunol. 1996;35:23–29. doi: 10.1111/j.1600-0897.1996.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 119.Hsu CD, Meaddough E, Aversa K, et al. The role of amniotic fluid L-selectin, GRO-alpha, and interleukin-8 in the pathogenesis of intraamniotic infection. Am J Obstet Gynecol. 1998;178:428–432. doi: 10.1016/s0002-9378(98)70414-4. [DOI] [PubMed] [Google Scholar]
- 120.Esplin MS, Romero R, Chaiworapongsa T, et al. Monocyte chemotactic protein-1 is increased in the amniotic fluid of women who deliver preterm in the presence or absence of intra-amniotic infection. J Matern Fetal Neonatal Med. 2005;17:365–373. doi: 10.1080/14767050500141329. [DOI] [PubMed] [Google Scholar]
- 121.Gotsch F, Romero R, Kusanovic JP, et al. The anti-inflammatory limb of the immune response in preterm labor, intra-amniotic infection/inflammation, and spontaneous parturition at term: a role for interleukin-10. J Matern Fetal Neonatal Med. 2008;21:529–547. doi: 10.1080/14767050802127349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Athayde N, Edwin SS, Romero R, et al. A role for matrix metalloproteinase-9 in spontaneous rupture of the fetal membranes. Am J Obstet Gynecol. 1998;179:1248–1253. doi: 10.1016/s0002-9378(98)70141-3. [DOI] [PubMed] [Google Scholar]
- 123.Maymon E, Romero R, Pacora P, et al. Evidence for the participation of interstitial collagenase (matrix metalloproteinase 1) in preterm premature rupture of membranes. Am J Obstet Gynecol. 2000;183:914–920. doi: 10.1067/mob.2000.108879. [DOI] [PubMed] [Google Scholar]
- 124.Maymon E, Romero R, Pacora P, et al. Human neutrophil collagenase (matrix metalloproteinase 8) in parturition, premature rupture of the membranes, and intrauterine infection. Am J Obstet Gynecol. 2000;183:94–99. doi: 10.1067/mob.2000.105344. [DOI] [PubMed] [Google Scholar]
- 125.Maymon E, Romero R, Pacora P, et al. Matrilysin (matrix metalloproteinase 7) in parturition, premature rupture of membranes, and intrauterine infection. Am J Obstet Gynecol. 2000;182:1545–1553. doi: 10.1067/mob.2000.107652. [DOI] [PubMed] [Google Scholar]
- 126.Maymon E, Romero R, Pacora P, et al. A role for the 72 kDa gelatinase (MMP-2) and its inhibitor (TIMP-2) in human parturition, premature rupture of membranes and intraamniotic infection. J Perinat Med. 2001;29:308–316. doi: 10.1515/JPM.2001.044. [DOI] [PubMed] [Google Scholar]
- 127.Helmig BR, Romero R, Espinoza J, et al. Neutrophil elastase and secretory leukocyte protease inhibitor in prelabor rupture of membranes, parturition and intra-amniotic infection. J Matern Fetal Neonatal Med. 2002;12:237–246. doi: 10.1080/jmf.12.4.237.246. [DOI] [PubMed] [Google Scholar]
- 128.Park KH, Chaiworapongsa T, Kim YM, et al. Matrix metalloproteinase 3 in parturition, premature rupture of the membranes, and microbial invasion of the amniotic cavity. J Perinat Med. 2003;31:12–22. doi: 10.1515/JPM.2003.002. [DOI] [PubMed] [Google Scholar]
- 129.Kim KW, Romero R, Park HS, et al. A rapid matrix metalloproteinase-8 bedside test for the detection of intraamniotic inflammation in women with preterm premature rupture of membranes. Am J Obstet Gynecol. 2007;197:292, e291–295. doi: 10.1016/j.ajog.2007.06.040. [DOI] [PubMed] [Google Scholar]
- 130.Romero R, Quintero R, Emamian M, et al. Arachidonate lipoxygenase metabolites in amniotic fluid of women with intra-amniotic infection and preterm labor. Am J Obstet Gynecol. 1987;157:1454–1460. doi: 10.1016/s0002-9378(87)80243-0. [DOI] [PubMed] [Google Scholar]
- 131.Romero R, Emamian M, Wan M, et al. Prostaglandin concentrations in amniotic fluid of women with intra-amniotic infection and preterm labor. Am J Obstet Gynecol. 1987;157:1461–1467. doi: 10.1016/s0002-9378(87)80245-4. [DOI] [PubMed] [Google Scholar]
- 132.Romero R, Wu YK, Sirtori M, et al. Amniotic fluid concentrations of prostaglandin F2 alpha, 13,14-dihydro-15-keto-prostaglandin F2 alpha (PGFM) and 11-deoxy-13,14-dihydro-15-keto-11, 16-cyclo-prostaglandin E2 (PGEM-LL) in preterm labor. Prostaglandins. 1989;37:149–161. doi: 10.1016/0090-6980(89)90038-5. [DOI] [PubMed] [Google Scholar]
- 133.Mazor M, Wiznitzer A, Maymon E, et al. Changes in amniotic fluid concentrations of prostaglandins E2 and F2 alpha in women with preterm labor. Isr J Med Sci. 1990;26:425–428. [PubMed] [Google Scholar]
- 134.Mazaki-Tovi S, Romero R, Kusanovic JP, et al. Visfatin/Pre-B cell colony-enhancing factor in amniotic fluid in normal pregnancy, spontaneous labor at term, preterm labor and prelabor rupture of membranes: an association with subclinical intrauterine infection in preterm parturition. J Perinat Med. 2008;36:485–496. doi: 10.1515/JPM.2008.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Soto E, Romero R, Richani K, et al. Evidence for complement activation in the amniotic fluid of women with spontaneous preterm labor and intra-amniotic infection. J Matern Fetal Neonatal Med. 2009;22:983–992. doi: 10.3109/14767050902994747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Vaisbuch E, Romero R, Erez O, et al. Fragment Bb in amniotic fluid: evidence for complement activation by the alternative pathway in women with intra-amniotic infection/inflammation. J Matern Fetal Neonatal Med. 2009;22:905–916. doi: 10.1080/14767050902994663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Cobo T, Palacio M, Martinez-Terron M, et al. Clinical and inflammatory markers in amniotic fluid as predictors of adverse outcomes in preterm premature rupture of membranes. Am J Obstet Gynecol. 2011;205:126, e121–128. doi: 10.1016/j.ajog.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 138.Kacerovsky M, Musilova I, Khatibi A, et al. Intraamniotic inflammatory response to bacteria: analysis of multiple amniotic fluid proteins in women with preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2012;25:2014–2019. doi: 10.3109/14767058.2012.671873. [DOI] [PubMed] [Google Scholar]
- 139.Kacerovsky M, Drahosova M, Krejsek J, et al. Amniotic fluid CD200 levels in pregnancies complicated by preterm prelabor rupture of the membranes. J Matern Fetal Neonatal Med. 2013;26:1416–1424. doi: 10.3109/14767058.2013.785517. [DOI] [PubMed] [Google Scholar]
- 140.Andrys C, Kacerovsky M, Drahosova M, et al. Amniotic fluid soluble Toll-like receptor 2 in pregnancies complicated by preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med. 2013;26:520–527. doi: 10.3109/14767058.2012.741634. [DOI] [PubMed] [Google Scholar]
- 141.Gauthier DW, Meyer WJ. Comparison of gram stain, leukocyte esterase activity, and amniotic fluid glucose concentration in predicting amniotic fluid culture results in preterm premature rupture of membranes. Am J Obstet Gynecol. 1992;167:1092–1095. doi: 10.1016/s0002-9378(12)80044-5. [DOI] [PubMed] [Google Scholar]
- 142.Yoon BH, Romero R, Jun JK, et al. Amniotic fluid cytokines (interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8) and the risk for the development of bronchopulmonary dysplasia. Am J Obstet Gynecol. 1997;177:825–830. doi: 10.1016/s0002-9378(97)70276-x. [DOI] [PubMed] [Google Scholar]
- 143.Ghezzi F, Gomez R, Romero R, et al. Elevated interleukin-8 concentrations in amniotic fluid of mothers whose neonates subsequently develop bronchopulmonary dysplasia. Eur J Obstet Gynecol Reprod Biol. 1998;78:5–10. doi: 10.1016/s0301-2115(97)00236-4. [DOI] [PubMed] [Google Scholar]
- 144.Coultrip LL, Lien JM, Gomez R, et al. The value of amniotic fluid interleukin-6 determination in patients with preterm labor and intact membranes in the detection of microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 1994;171:901–911. doi: 10.1016/s0002-9378(94)70057-5. [DOI] [PubMed] [Google Scholar]
- 145.Greci LS, Gilson GJ, Nevils B, et al. Is amniotic fluid analysis the key to preterm labor? A model using interleukin-6 for predicting rapid delivery. Am J Obstet Gynecol. 1998;179:172–178. doi: 10.1016/s0002-9378(98)70269-8. [DOI] [PubMed] [Google Scholar]
- 146.El-Bastawissi AY, Williams MA, Riley DE, et al. Amniotic fluid interleukin-6 and preterm delivery: a review. Obstet Gynecol. 2000;95:1056–1064. [PubMed] [Google Scholar]
- 147.Wei SQ, Fraser W, Luo ZC. Inflammatory cytokines and spontaneous preterm birth in asymptomatic women: a systematic review. Obstet Gynecol. 2010;116:393–401. doi: 10.1097/AOG.0b013e3181e6dbc0. [DOI] [PubMed] [Google Scholar]
- 148.Conde-Agudelo A, Papageorghiou AT, Kennedy SH, et al. Novel biomarkers for the prediction of the spontaneous preterm birth phenotype: a systematic review and meta-analysis. BJOG. 2011;118:1042–1054. doi: 10.1111/j.1471-0528.2011.02923.x. [DOI] [PubMed] [Google Scholar]
- 149.Schefold JC, Hasper D, von Haehling S, et al. Interleukin-6 serum level assessment using a new qualitative point-of-care test in sepsis: A comparison with ELISA measurements. Clin Biochem. 2008;41:893–898. doi: 10.1016/j.clinbiochem.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 150.Meem M, Modak JK, Mortuza R, et al. Biomarkers for diagnosis of neonatal infections: A systematic analysis of their potential as a point-of-care diagnostics. J Glob Health. 2011;1:201–209. [PMC free article] [PubMed] [Google Scholar]
- 151.Batfalsky A, Lohr A, Heussen N, et al. Diagnostic value of an interleukin-6 bedside test in term and preterm neonates at the time of clinical suspicion of early- and late-onset bacterial infection. Neonatology. 2012;102:37–44. doi: 10.1159/000336632. [DOI] [PubMed] [Google Scholar]
- 152.Dengler J, Schefold JC, Graetz D, et al. Point-of-care testing for interleukin-6 in cerebro spinal fluid (CSF) after subarachnoid haemorrhage. Med Sci Monit. 2008;14:BR265–268. [PubMed] [Google Scholar]
- 153.Vousden N, Chandiramani M, Seed P, et al. Interleukin-6 bedside testing in women at high risk of preterm birth. J Matern Fetal Neonatal Med. 2011;24:1301–1304. doi: 10.3109/14767058.2011.558954. [DOI] [PubMed] [Google Scholar]
- 154.Berthiaume M, Rousseau E, Rola-Pleszczynski M, et al. Rapid evaluation of the absence of inflammation after rupture of membranes. J Matern Fetal Neonatal Med. 2014;27:865–869. doi: 10.3109/14767058.2013.829814. [DOI] [PubMed] [Google Scholar]
- 155.Kim CJ, Romero R, Kusanovic JP, et al. The frequency, clinical significance, and pathological features of chronic chorioamnionitis: a lesion associated with spontaneous preterm birth. Mod Pathol. 2010;23:1000–1011. doi: 10.1038/modpathol.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lee J, Romero R, Xu Y, et al. Maternal HLA panel-reactive antibodies in early gestation positively correlate with chronic chorioamnionitis: evidence in support of the chronic nature of maternal anti-fetal rejection. Am J Reprod Immunol. 2011;66:510–526. doi: 10.1111/j.1600-0897.2011.01066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lee J, Kim JS, Park JW, et al. Chronic chorioamnionitis is the most common placental lesion in late preterm birth. Placenta. 2013;34:681–689. doi: 10.1016/j.placenta.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 158.Pacora P, Chaiworapongsa T, Maymon E, et al. Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. J Matern Fetal Neonatal Med. 2002;11:18–25. doi: 10.1080/jmf.11.1.18.25. [DOI] [PubMed] [Google Scholar]
- 159.Redline RW, Heller D, Keating S, et al. Placental diagnostic criteria and clinical correlation--a workshop report. Placenta. 2005;26(Suppl A):S114–117. doi: 10.1016/j.placenta.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 160.Redline RW. Inflammatory responses in the placenta and umbilical cord. Semin Fetal Neonatal Med. 2006;11:296–301. doi: 10.1016/j.siny.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 161.Santhanam U, Avila C, Romero R, et al. Cytokines in normal and abnormal parturition: elevated amniotic fluid interleukin-6 levels in women with premature rupture of membranes associated with intrauterine infection. Cytokine. 1991;3:155–163. doi: 10.1016/1043-4666(91)90037-e. [DOI] [PubMed] [Google Scholar]
- 162.Romero R, Galasso M, Gomez R, et al. A comparative study of the value of amniotic fluid interleukin-6, white blood cell count and gram stain in the diagnosis of microbial invasion of the amniotic cavity in patients with spontaneous labor at term.. Annual Meeting of the Society of Perinatal Obstetricians; Las Vegas, NV. 1994. p. A250. [DOI] [PubMed] [Google Scholar]
- 163.Andrews WW, Hauth JC, Goldenberg RL, et al. Amniotic fluid interleukin-6: correlation with upper genital tract microbial colonization and gestational age in women delivered after spontaneous labor versus indicated delivery. Am J Obstet Gynecol. 1995;173:606–612. doi: 10.1016/0002-9378(95)90290-2. [DOI] [PubMed] [Google Scholar]
- 164.Yoon BH, Romero R, Park JS, et al. Microbial invasion of the amniotic cavity with Ureaplasma urealyticum is associated with a robust host response in fetal, amniotic, and maternal compartments. Am J Obstet Gynecol. 1998;179:1254–1260. doi: 10.1016/s0002-9378(98)70142-5. [DOI] [PubMed] [Google Scholar]
- 165.Yoon BH, Romero R, Moon JB, et al. The frequency and clinical significance of intra-amniotic inflammation in patients with a positive cervical fetal fibronectin. Am J Obstet Gynecol. 2001;185:1137–1142. doi: 10.1067/mob.2001.118162. [DOI] [PubMed] [Google Scholar]
- 166.Yoon BH, Romero R, Lim JH, et al. The clinical significance of detecting Ureaplasma urealyticum by the polymerase chain reaction in the amniotic fluid of patients with preterm labor. Am J Obstet Gynecol. 2003;189:919–924. doi: 10.1067/s0002-9378(03)00839-1. [DOI] [PubMed] [Google Scholar]
- 167.DiGiulio DB, Romero R, Amogan HP, et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One. 2008;3:e3056. doi: 10.1371/journal.pone.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.DiGiulio DB, Gervasi M, Romero R, et al. Microbial invasion of the amniotic cavity in preeclampsia as assessed by cultivation and sequence-based methods. J Perinat Med. 2010;38:503–513. doi: 10.1515/JPM.2010.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Madan I, Romero R, Kusanovic JP, et al. The frequency and clinical significance of intra-amniotic infection and/or inflammation in women with placenta previa and vaginal bleeding: an unexpected observation. J Perinat Med. 2010;38:275–279. doi: 10.1515/JPM.2010.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gervasi MT, Romero R, Bracalente G, et al. Midtrimester amniotic fluid concentrations of interleukin-6 and interferon-gamma-inducible protein-10: evidence for heterogeneity of intra-amniotic inflammation and associations with spontaneous early (<32 weeks) and late (>32 weeks) preterm delivery. J Perinat Med. 2012;40:329–343. doi: 10.1515/jpm-2012-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gomez R, Ghezzi F, Romero R, et al. Premature labor and intra-amniotic infection. Clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol. 1995;22:281–342. [PubMed] [Google Scholar]
- 172.Lee J, Oh KJ, Yang HJ, et al. The importance of intra-amniotic inflammation in the subsequent development of atypical chronic lung disease. J Matern Fetal Neonatal Med. 2009;22:917–923. doi: 10.1080/14767050902994705. [DOI] [PubMed] [Google Scholar]
- 173.Kim SM, Romero R, Lee J, et al. The frequency and clinical significance of intra-amniotic inflammation in women with preterm uterine contractility but without cervical change: do the diagnostic criteria for preterm labor need to be changed? J Matern Fetal Neonatal Med. 2012;25:1212–1221. doi: 10.3109/14767058.2011.629256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lee J, Romero R, Chaiworapongsa T, et al. Characterization of the fetal blood transcriptome and proteome in maternal anti-fetal rejection: evidence of a distinct and novel type of human fetal systemic inflammatory response. Am J Reprod Immunol. 2013;70:265–284. doi: 10.1111/aji.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Gutierres SL, Welty TE. Point-of-care testing: an introduction. Ann Pharmacother. 2004;38:119–125. doi: 10.1345/aph.1D212. [DOI] [PubMed] [Google Scholar]
- 176.Kost GJ, Tran NK. Point-of-Care Testing and Cardiac Biomarkers: The Standard of Care and Vision for Chest Pain Centers. Cardiol Clin. 2005;23:467–490. vi. doi: 10.1016/j.ccl.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 177.Lewandrowski K. Point-of-care testing: an overview and a look to the future (circa 2009, United States). Clin Lab Med. 2009;29:421–432. doi: 10.1016/j.cll.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 178.Pfafflin A, Schleicher E. Inflammation markers in point-of-care testing (POCT). Anal Bioanal Chem. 2009;393:1473–1480. doi: 10.1007/s00216-008-2561-3. [DOI] [PubMed] [Google Scholar]