Abstract
Several limitations existed in previous studies which suggested that diabetic patients have increased risk of stroke. We conducted this study to better understand the stroke risk and poststroke outcomes in patients with diabetes.
From the claims data of Taiwan's National Health Insurance, we identified 24,027 adults with new-diagnosed diabetes and 96,108 adults without diabetes between 2000 and 2003 in a retrospective cohort study. Stroke events (included hemorrhage, ischemia, and other type of stroke) during the follow-up period of 2000 to 2008 were ascertained and adjusted risk of stroke associated with diabetes was calculated. A nested cohort study of 221,254 hospitalized stroke patients (included hemorrhage, ischemia, and other type of stroke) between 2000 and 2009 was conducted. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for adverse events after stroke hospitalization in patients with and without diabetes.
The incidences of stroke in cohorts with and without diabetes were 10.1 and 4.5 per 1000 person-years, respectively. During the follow-up period, diabetic patients had an increased risk of stroke (adjusted hazard ratio: 1.75; 95% CI: 1.64–1.86) than those without diabetes. Associations between diabetes and stroke risk were significant in both sexes and all age groups. Previous diabetes was associated with poststroke mortality (OR: 1.33; 95% CI: 1.19–1.49), pneumonia (OR: 1.30; 95% CI: 1.20–1.42), and urinary tract infection (OR: 1.66; 95% CI: 1.55–1.77). The impact of diabetes on adverse events after stroke was investigated particularly in those with diabetes-related complications.
Diabetes was associated with stroke risk, and diabetic patients had more adverse events and subsequent mortality after stroke.
INTRODUCTION
As the global prevalence of diabetes is predicted to reach 4.4% in all age groups by 2030, diabetes is clearly a pandemic chronic disease causing widespread disability and death worldwide.1 Costs associated with diabetes in the United States were estimated to reach as high as $245 billion in 2012.2 Although the epidemiology, pathogenesis, prevention, and treatment of diabetes have been well established over the past 2 centuries,3 complications after diabetes require further study.
Stroke is one of the major causes of disability and mortality worldwide.4,5 Although global mortality from stroke fell in the past 2 decades (1990–2010), an increased incidence of stroke in low-income and middle-income countries was investigated.5 An international multicentre study identified stroke risk factors including cardiac disease, hypertension, diabetes, smoking, alcohol intake, unhealthy diet, abdominal obesity, lack of exercise, psychosocial stress and depression, and said these factors could explain 90% of stroke risk.4
A systematic review with meta-analysis and several previous epidemiological reports suggested that patients with diabetes had increased risk of stroke.6–18 The impact of diabetes on outcomes after stroke was also investigated.19–28 However, these previous studies may have bias because they were limited by several factors, including case-control study design,9 reporting only a single type of stroke,7,8,10,12,15,19,21,22,24,25,27,28 a small sample of diabetic patients,8,11,12,24,26,27 a focus on a specific population,9,14,17,23,25 not distinguishing separate subtypes of diabetes,7–13,15–28 inadequate adjustment for potential confounders,8,12,13,15,16,18,26,28 and lack of appropriate comparison groups.11,13
We used Taiwan's National Health Insurance reimbursement claims to investigate the incidence and risk of stroke after adjustment for potential confounding factors for adults with diabetes in a nationwide retrospective cohort study. More importantly, we conducted a nested cohort study to investigate the impact of diabetes on poststroke outcomes.
PARTICIPANTS AND METHODS
Data Collection
This study's data came from medical claims in the National Health Insurance Research Database established by the National Health Research Institutes in Taiwan. Taiwan implemented a universal-care National Health Insurance system (included inpatient and hospitalization medial cares) in March 1995 that covers >99% of the country's 23 million residents. The available information used in this study including diagnoses for admission and discharge, treatments, medications, characteristics of medical institutions where care was accessed, medical expenditures, and all the services physicians provided. For the purpose of data management, research, and administration, Taiwan's National Health Research Institutes released a random-selected database consisting 1 million medical beneficiaries (including all age groups) that represents ∼4.3% of Taiwan's insurance enrollees.29–31 In addition, the All Stroke Database used in this study was also extracted from Taiwan National Health Insurance Research Database obtained between 1996 and 2010.
Ethics Approval
To protect personal privacy, patient's identifications from National Health Insurance Research Database were decoded and scrambled for any potential research access. This study was approved both by the Taiwan's National Health Research Institutes (NHIRD-103-121) and Taipei Medical University's Institutional Review Board (TMU-JIRB 201505055; TMU-JIRB 201404070) and was exempted from the patient informed consent, which was not required because patients’ identifications have been decoded and scrambled.29-31
Study Design
Excluding people with previous medical records of stroke and/or diabetes within 1996 to 1999 in the insurance data of the 1,000,000 persons, the incident diabetic cohort included 24,027 adults aged ≥20 years was identified in 2000 to 2003 under the definition of >3 visits of ambulatory care or hospitalization for diabetes was required. With the frequency-matching procedure by the age and the gender at the same study time interval, 96,108 adults were selected as nondiabetic cohort who had no medical records of diabetes previously. At the beginning of follow-up, diabetic and nondiabetic cohorts had no history of stroke. We started the follow-up from the beginning of 2000 and lasted until the end of 2008. Incident cases of stroke (included hemorrhage, ischemia, and other type of stroke) were identified during the follow-up period. The purpose of this retrospective cohort study is to report the risk of stroke in patients with diabetes.
Among 221,254 new-onset stroke patients (included hemorrhage, ischemia, and other type of stroke) who were admitted for inpatient care in 2000 to 2009, we identified 9998 stroke patients had history of diabetes. Using this All Stroke Database of Taiwan's National Health Insurance Research Database, complications, consumption of medical resources, and the case fatality within 30 days after stroke were analyzed for diabetic patients and nondiabetic people.
Definitions and Measurements
The low level of income was defined according to the standards income registered in database of Taiwan's Ministry of Health and Welfare. The urbanized definition and category of residential area were based on our previous investigations.30,31 In this study, we considered the use of cardiovascular medications, such as aspirin, anticoagulant, statins, and antihypertension drugs.
Diagnostic codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) were used to define diseases and morbidities in this study, such as diabetes mellitus (250), cerebrovascular diseases (430–438), hypertensive diseases (401–405), mental diseases (290–319), ischemic heart disease (410–414), chronic obstructive pulmonary disease (490–496), hyperlipidemia (272.0, 272.1, and 272.2), liver cirrhosis (571), heart failure (428), atrial fibrillation (427.3), epilepsy (345), head injury (800–804, 850–854), pneumonia (480–486), and urinary tract infection (599.0). Hemodialysis and/or peritoneal dialysis were also recorded by the administrative code. Medications, such as recombinant tissue plasminogen activator, aspirin, anticoagulant, statin, and antihypertension drug, were considered in this study.
Statistical Analysis
We used chi-square tests to examine the distributions of categorical data included age, sex, low income, urbanization, history of diseases, and medications between diabetic and nondiabetic cohorts. Using the multiple Cox proportional hazards models, the hazard ratios (HRs) with 95% confidence intervals (CIs) for stroke risk in diabetic cohort were calculated with the adjustment of all covariates. The subgroup analysis was also performed for the association between diabetes and stroke risk.
In the All Stroke Database, the balances of age, sex, low income, urbanization, history of diseases, and medications between diabetic stroke patients and nondiabetic stroke patients were examined in the chi-square tests. We performed multiple logistic regressions to estimate odds ratios (ORs) and 95% CIs of complications and mortality after stroke in diabetic patients by adjusting sociodemographic factors, history of diseases, and medications. All significance tests were 2-sided using P < 0.05 as the level of significance. All data analyses were performed by the SAS, version 9.1 (SAS Institute Inc., Cary, NC) statistical software.
RESULTS
The distributions of age and sex were balanced between diabetic and nondiabetic cohorts because frequency matching was used in this study (Table 1). The prevalence of low urbanization, low-income, hypertension, mental disorders, ischemic heart disease, chronic obstructive pulmonary disease, hyperlipidemia, liver cirrhosis, congestive heart failure, atrial fibrillation, epilepsy, and renal dialysis were higher in diabetic cohort than in nondiabetic cohort, as well as the use of aspirin, anticoagulants, statins, and antihypertension drugs (all P < 0.0001).
TABLE 1.
Sociodemographic Factors, Coexisting Medical Conditions, and Medication in People With and Without Diabetes

Diabetic cohort had higher incidence of stroke than nondiabetic cohort (10.1 vs 4.5 per 1000 person-years, P < 0.0001) and the corresponding HR of stroke associated with diabetes was 1.75 (95% CI: 1.64–1.86) during the follow-up period (Table 2). Type 2 diabetes (HR: 1.76; 95% CI: 1.65–1.87) was more likely to be associated with stroke risk than type 1 diabetes (HR: 1.50; 95% CI: 1.23–1.83). Diabetes was more associated with stroke risk in women (HR: 1.93; 95% CI: 1.76–2.12) than in men (HR: 1.60; 95% CI: 1.47–1.75). In every age group, diabetes was associated with stroke risk. The adjusted HRs for stroke associated with diabetes in people with 0, 1, 2, and ≥3 medical conditions were 1.56 (95% CI: 1.33–1.84), 1.86 (95% CI: 1.65–2.09), 1.71 (95% CI: 1.51–1.94), and 1.44 (95% CI: 1.28–1.62), respectively.
TABLE 2.
Incidence and Risk of Stroke for Cohorts With and Without Diabetes||
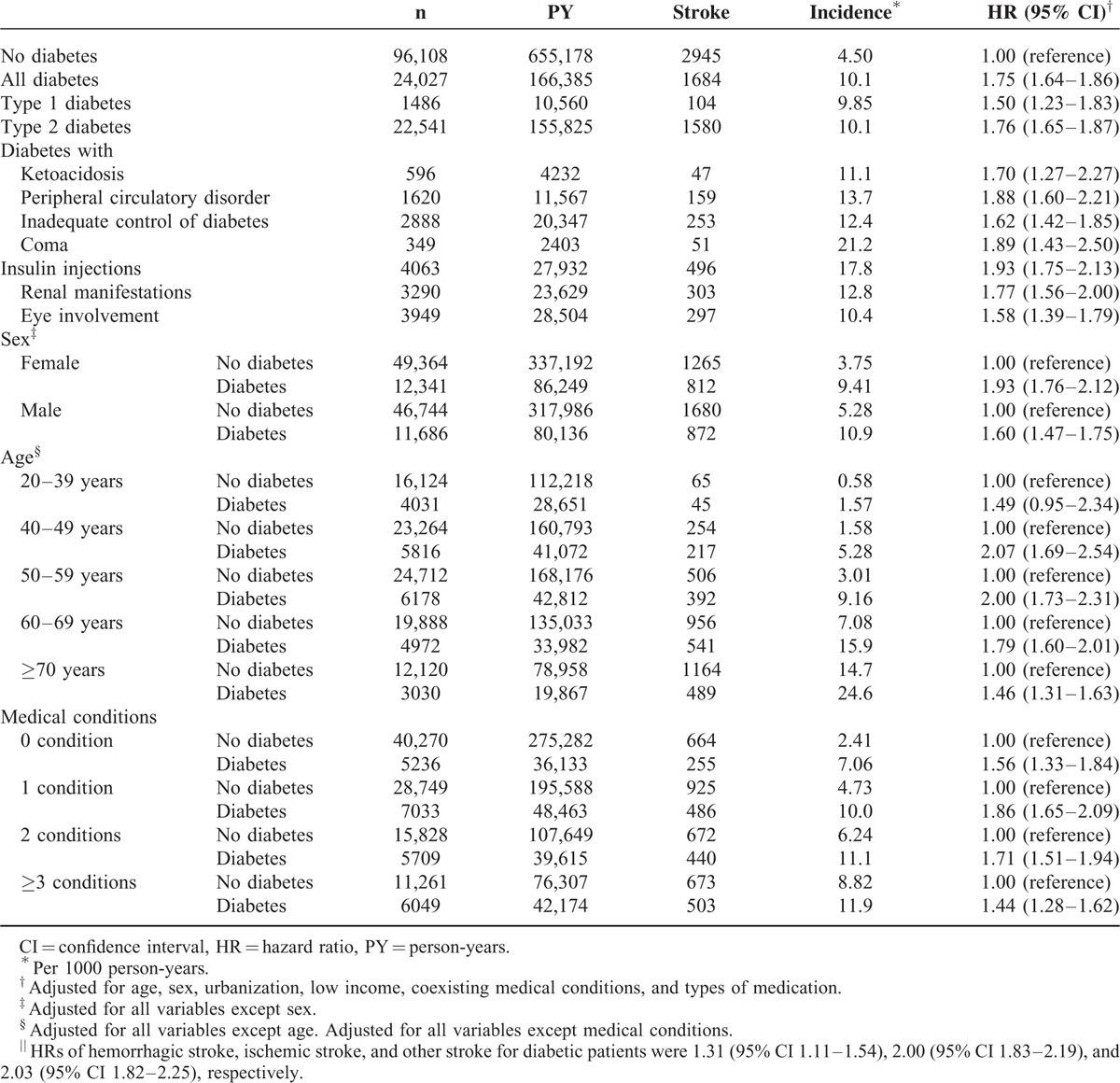
Diabetes-related indicators, such as peripheral circulatory disorder (HR: 1.88; 95% CI: 1.60–2.21), coma (HR: 1.89; 95% CI: 1.43–2.50), and insulin injections (HR: 1.93; 95% CI: 1.75–2.13) were more significant associated with risk of stroke. HRs of hemorrhagic stroke, ischemic stroke, and other stroke for diabetic patients were 1.31 (95% CI 1.11–1.54), 2.00 (95% CI 1.83–2.19), and 2.03 (95% CI 1.82–2.25), respectively.
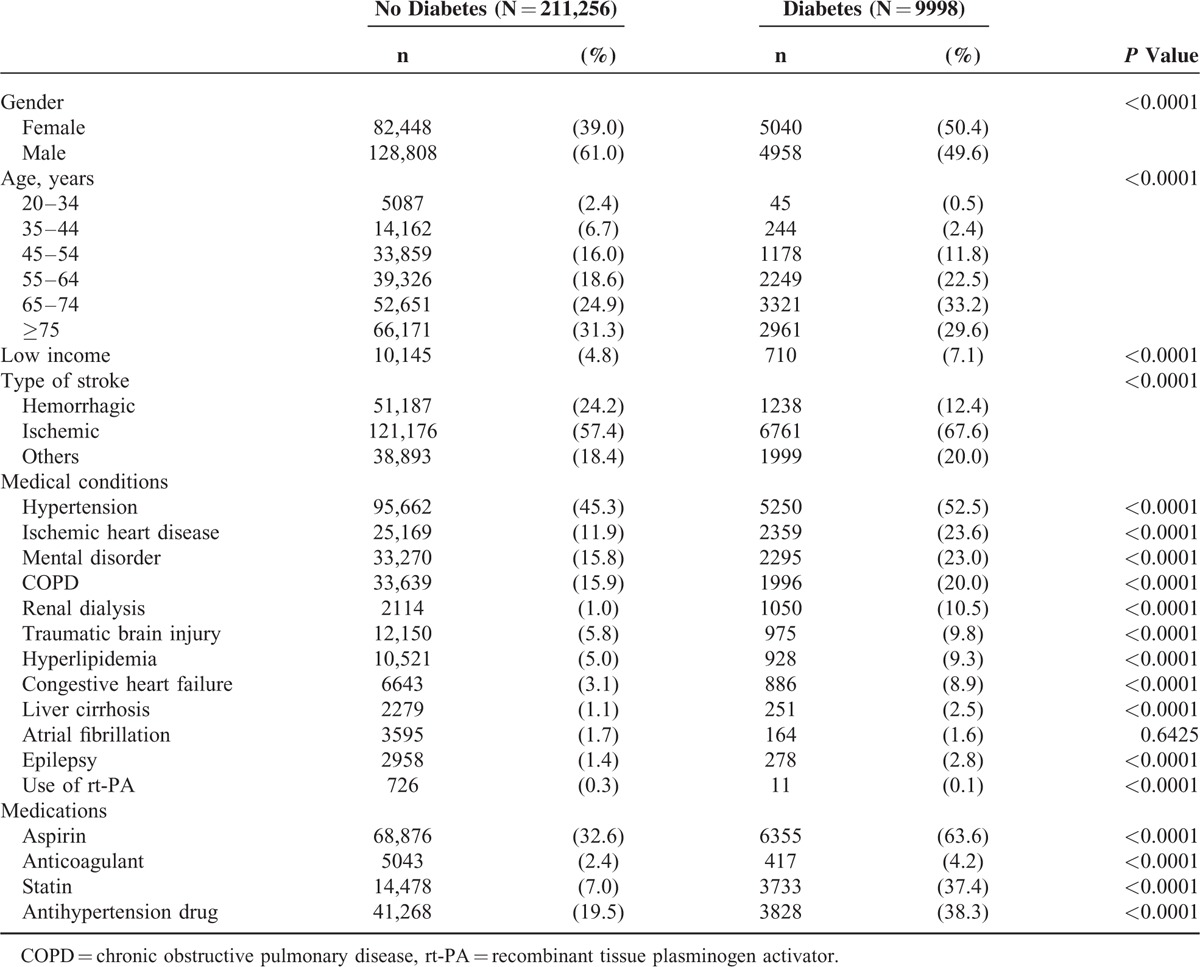
Among 221,254 patients with stroke (Table 3), diabetic patients had higher proportions of women (P < 0.0001), older people (P < 0.0001), low income (P < 0.0001), hypertension (P < 0.0001), ischemic heart disease (P < 0.0001), mental disorders (P < 0.0001), chronic obstructive pulmonary disease (P < 0.0001), atherosclerosis (P < 0.0001), renal dialysis (P < 0.0001), hyperlipidemia (P < 0.0001), congestive heart failure (P < 0.0001), liver cirrhosis (P < 0.0001), epilepsy (P < 0.0001), and use of cardiovascular medication (anticoagulants, antiplatelet agents, or lipid-lowering agents) compared with nondiabetic patients.
TABLE 3.
Sociodemographic Factors, Coexisting Medical Conditions, and Medication in Hospitalized Stroke Patients With and Without Diabetes
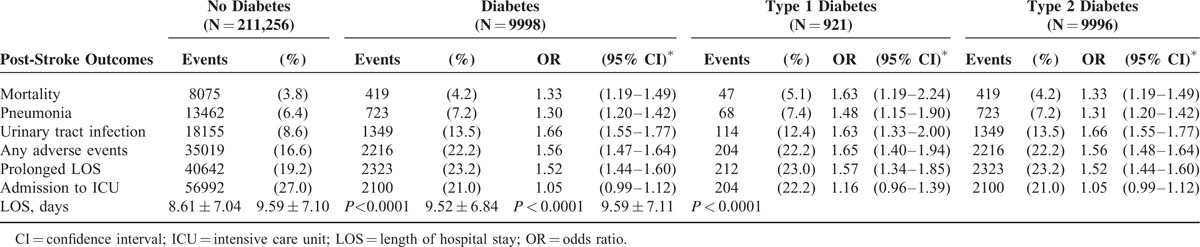
In Table 4, diabetic patients had higher risk of mortality (OR: 1.33; 95% CI: 1.19–1.49), pneumonia (OR: 1.30; 95% CI: 1.20–1.42), and urinary tract infection (OR: 1.66; 95% CI: 1.55–1.77) after stroke compared with those without diabetes in the nested stroke cohort study. Previous diabetes was also associated with poststroke prolonged length of stay (OR: 1.52; 95% CI: 1.44–1.60). The mean of length of stay for stroke patients with and without diabetes were 9.59 ± 7.10 days and 8.61 ± 7.04 days, respectively (P < 0.0001). Poststroke pneumonia, urinary tract infection, adverse events, prolonged length of hospital stay, and mortality were associated with type 1 and type 2 diabetes.
TABLE 4.
Risks of Adverse Outcomes in Hospitalized Stroke Patients With and Without Previous Diabetes
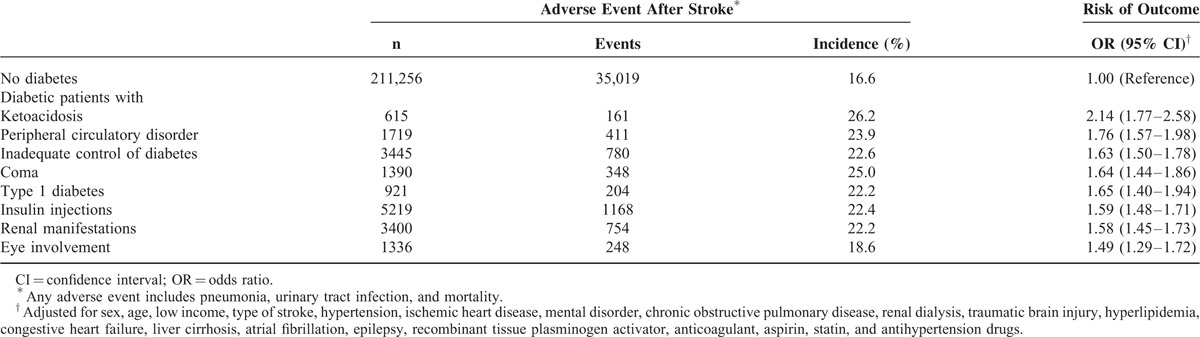
In Table 5, diabetes-related clinical characteristics were associated with poststroke adverse events, such as ketoacidosis (OR: 2.14; 95% CI: 1.77–2.58), peripheral circulatory disorder (OR: 1.76; 95% CI: 1.57–1.98), inadequate control of diabetes (OR: 1.63; 95% CI: 1.50–1.78), coma (OR: 1.64; 95% CI: 1.44–1.86), type 1 diabetes (OR: 1.65; 95% CI: 1.40–1.94), insulin injections (OR: 1.59; 95% CI: 1.48–1.71), renal manifestations (OR: 1.58; 95% CI: 1.45–1.73), and eye involvement (OR: 1.49; 95% CI: 1.29–1.72).
TABLE 5.
Risks of In-hospital Complications and Mortality During Stroke Admission for Patients With Diabetes
DISCUSSION
Using the claims data of Taiwan's National Health Insurance, we validated the long-term increased risk for all types of stroke in type 1 or type 2 diabetes adult patients in this nationwide retrospective cohort study. Another nested cohort study showed that patients with diabetes had increased rates of pneumonia, urinary tract infection, and mortality during stroke hospitalization. The impact of diabetes on adverse events after stroke was investigated particularly in those with diabetes-related complications.
Although the association between diabetes and risk of stroke is not a novel finding, previous studies had many limitations that may lead to bias.7–28 Large sample size (reduced selection bias), cohort study design (more evidence in causal inference), multivariate adjustment (reduced confounding bias), including all types of stroke and diabetes (providing more comprehensive information), and not being restricted by specific populations (reduced selection bias) are the strengths of this investigation.
Sex, age, low income, and urbanization were associated with stroke as well as with diabetes.3,6,29–31 Therefore, these sociodemographics should be considered as potential confounding factors when investigating the association between diabetes and stroke. To investigate risk and outcomes of stroke in diabetic patients in this study, we adjusted these sociodemographic characteristics in the multivariate Cox proportional hazard regression models and logistic regression models.
Patients with diabetes mellitus were more likely to have stroke compared with those without diabetes.6–18 Hypertension, mental disorders, ischemic heart disease, chronic obstructive pulmonary disease, hyperlipidemia, liver cirrhosis, congestive heart failure, atrial fibrillation, epilepsy, traumatic brain injury, and renal dialysis have been shown to be independently associated with higher risk of stroke.4,29–31 These medical conditions also commonly coexist with diabetes.3,6–18,19–28 However, previous studies were limited by inadequate control of coexisting medical conditions when investigating the association between diabetes and stroke.8,12,13,15,16,18,26,28 To avoid the confounding bias from these coexisting medical conditions, the present study used a multivariate regression model to adjust for these medical confounders.
The burden of infections among people with diabetes remains an important issue.32 Previous studies also demonstrated diabetic patients’ increased risk of infectious diseases after stroke.26 Therefore, it is not surprising that we found diabetic patients had higher risks of pneumonia and urinary tract infections after suffering from stroke compared with controls in this study. These infections were also contributors for the poststroke mortality in diabetic patients.
Type 1 diabetes, inadequate control of glucose, ketoacidosis, coma, renal manifestations, eye involvement, and peripheral circulatory disorder were considered as severity-related indicators for diabetic patients.3,19 Our nested cohort study shows these severity-related diabetes indicators caused significant poststroke mortality. This original finding provides useful information for clinical scenarios and was not reported previously.19–28
To clarify associations between diabetes and stroke risk, some possible reasons may be stated. First, damaged vascular function in diabetic patients (such as pulse wave velocity, plaque, and carotid intima-media thickness) causes atherosclerosis, a significant predictor for stroke.33,34 A second possible explanation is diabetic patients’ hypoglycemic coma (due to inadequate control for glucose), obesity, cataract, glaucoma, retinopathy, osteoporosis, cognitive dysfunction, and mental illness that were also found as risk factors for fracture and traumatic brain injury.35 Strong evidence also suggests that patients with hip fracture or traumatic brain injury were more likely to have stroke.31 Third, less physical activity, unhealthy lifestyle factors such as smoking and drinking alcohol to excess were also contributors for developing stroke in patients with diabetes.36,37 Fourth, people with diabetes may have poor knowledge, attitudes, and practices regarding disease prevention,38 which were considered factors associated with the development of stroke. In addition, diabetes was associated with increased levels of inflammation-sensitive plasma proteins identified as a contributor to risk of stroke and cardiovascular diseases.39 Finally, we considered the side effect of medication in patients with type 2 diabetes also has partial contribution for risk of stroke, because a previous study suggested that thiazolidinedione treatment increased progression of subclinical atherosclerosis in patients with type 2 diabetes.40 However, this point needs future further human or animal trials to provide biochemical mechanisms.
Readers should be cautioned against overinterpretation of our findings because of study limitations. First, there was no information on detailed sociodemographic factors, lifestyle, clinical risk scores of stroke, and the results of blood or urine tests in the National Health Insurance Research Database. Second, the histories of diseases for study subjects were identified by people who visited medical care services. We admitted that the misclassification may exist in this study because patients had impaired fasting glycemia or diabetes without symptoms might not visit medical care services. Therefore, the underestimated risk of stroke in diabetic cohort is possible. Third, the validation of codes of diseases may be one of limitations for this study even though many studies based on National Health Insurance were accepted by important journals.29–31 Finally, the confounding effects remains a possible limitation of this study although several potential confounding factors were controlled by multiple regression models.
In conclusion, these 2 nationwide cohort studies showed the impact of diabetes on risk of stroke and poststroke adverse events such as pneumonia, urinary tract infection, and mortality. Poorly controlled diabetes and diabetes-related complications contributed to mortality after stroke. This analysis provides comprehensive assessment of stroke risk and poststroke outcomes in patients with diabetes. Further studies are needed to develop specific strategies to decrease stroke risks and poststroke adverse outcomes for this patient population.
Acknowledgments
This study is based in part on data from the National Health Insurance Research Database provided by the National Health Insurance Administration, Ministry of Health and Welfare and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of National Health Insurance Administration, Ministry of Health and Welfare or National Health Research Institutes.
Footnotes
Abbreviations: CI = confidence interval, HR = hazard ratio, ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification, OR = odds ratio.
Funding: this study was partly supported by a grant from Shuang Ho Hospital, Taipei Medical University (104TMU-SHH-23) and Ministry of Science and Technology, Taiwan (MOST104-2314-B-038-027-MY2; NSC102-2314-B-038-021-MY3). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27:1047–1053. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes. Care 2013; 36:1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polonsky KS. The past 200 years in diabetes. N Engl J Med 2012; 367:1332–1340. [DOI] [PubMed] [Google Scholar]
- 4.O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010; 376:112–123. [DOI] [PubMed] [Google Scholar]
- 5.Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health 2013; 1:e259–e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 2014; 383:1973–1980. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee C, Moon YP, Paik MC, et al. Duration of diabetes and risk of ischemic stroke: the Northern Manhattan Study. Stroke 2012; 43:1212–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khoury JC, Kleindorfer D, Alwell K, et al. Diabetes mellitus: a risk factor for ischemic stroke in a large biracial population. Stroke 2013; 44:1500–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuusisto J, Mykkänen L, Pyörälä K, et al. Non-insulin-dependent diabetes and its metabolic control are important predictors of stroke in elderly subjects. Stroke 1994; 25:1157–1164. [DOI] [PubMed] [Google Scholar]
- 10.Iso H, Imano H, Kitamura A, et al. Type 2 diabetes and risk of non-embolic ischaemic stroke in Japanese men and women. Diabetologia 2004; 47:2137–2144. [DOI] [PubMed] [Google Scholar]
- 11.Tanizaki Y, Kiyohara Y, Kato I, et al. Incidence and risk factors for subtypes of cerebral infarction in a general population: the Hisayama study. Stroke 2000; 31:2616–2622. [DOI] [PubMed] [Google Scholar]
- 12.Boden-Albala B, Cammack S, Chong J, et al. Diabetes, fasting glucose levels, and risk of ischemic stroke and vascular events: findings from the Northern Manhattan Study (NOMAS). Diabetes Care 2008; 31:1132–1137. [DOI] [PubMed] [Google Scholar]
- 13.Hart CL, Hole DJ, Smith GD. Comparison of risk factors for stroke incidence and stroke mortality in 20 years of follow-up in men and women in the Renfrew/Paisley Study in Scotland. Stroke 2000; 31:1893–1896. [DOI] [PubMed] [Google Scholar]
- 14.Janghorbani M, Hu FB, Willett WC, et al. Prospective study of type 1 and type 2 diabetes and risk of stroke subtypes: the Nurses’ Health Study. Diabetes Care 2007; 30:1730–1735. [DOI] [PubMed] [Google Scholar]
- 15.Folsom AR, Rasmussen ML, Chambless LE, et al. Prospective associations of fasting insulin, body fat distribution, and diabetes with risk of ischemic stroke. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. Diabetes Care 1999; 22:1077–1083. [DOI] [PubMed] [Google Scholar]
- 16.Almdal T, Scharling H, Jensen JS, et al. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Arch Intern Med 2004; 164:1422–1426. [DOI] [PubMed] [Google Scholar]
- 17.Cui R, Iso H, Yamagishi K, et al. Diabetes mellitus and risk of stroke and its subtypes among Japanese: the Japan public health center study. Stroke 2011; 42:2611–2614. [DOI] [PubMed] [Google Scholar]
- 18.Jeerakathil T, Johnson JA, Simpson SH, et al. Short-term risk for stroke is doubled in persons with newly treated type 2 diabetes compared with persons without diabetes: a population-based cohort study. Stroke 2007; 38:1739–1743. [DOI] [PubMed] [Google Scholar]
- 19.Nikneshan D, Raptis R, Pongmoragot J, et al. Predicting clinical outcomes and response to thrombolysis in acute stroke patients with diabetes. Diabetes Care 2013; 36:2041–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Icks A, Claessen H, Morbach S, et al. Time-dependent impact of diabetes on mortality in patients with stroke: survival up to 5 years in a health insurance population cohort in Germany. Diabetes Care 2012; 35:1868–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jia Q, Zhao X, Wang C, et al. Diabetes and poor outcomes within 6 months after acute ischemic stroke: the China National Stroke Registry. Stroke 2011; 42:2758–2762. [DOI] [PubMed] [Google Scholar]
- 22.Reeves MJ, Vaidya RS, Fonarow GC, et al. Quality of care and outcomes in patients with diabetes hospitalized with ischemic stroke: findings from Get With the Guidelines-Stroke. Stroke 2010; 41:e409–e417. [DOI] [PubMed] [Google Scholar]
- 23.Eriksson M, Carlberg B, Eliasson M. The disparity in long-term survival after a first stroke in patients with and without diabetes persists: the Northern Sweden MONICA study. Cerebrovasc Dis 2012; 34:153–160. [DOI] [PubMed] [Google Scholar]
- 24.Desilles JP, Meseguer E, Labreuche J, et al. Diabetes mellitus, admission glucose, and outcomes after stroke thrombolysis: a registry and systematic review. Stroke 2013; 44:1915–1923. [DOI] [PubMed] [Google Scholar]
- 25.Kamalesh M, Shen J, Eckert GJ. Long-term postischemic stroke mortality in diabetes: a veteran cohort analysis. Stroke 2008; 39:2727–2731. [DOI] [PubMed] [Google Scholar]
- 26.Megherbi SE, Milan C, Minier D, et al. Association between diabetes and stroke subtype on survival and functional outcome 3 months after stroke: data from the European BIOMED Stroke Project. Stroke 2003; 34:688–694. [DOI] [PubMed] [Google Scholar]
- 27.Tanaka R, Ueno Y, Miyamoto N, et al. Impact of diabetes and prediabetes on the short-term prognosis in patients with acute ischemic stroke. J Neurol Sci 2013; 332:45–50. [DOI] [PubMed] [Google Scholar]
- 28.Kaarisalo MM, Räihä I, Sivenius J, et al. Diabetes worsens the outcome of acute ischemic stroke. Diabetes Res Clin Pract 2005; 69:293–298. [DOI] [PubMed] [Google Scholar]
- 29.Liao CC, Chang PY, Yeh CC, et al. Stroke risk and outcomes in patients with traumatic brain injury: 2 nationwide studies. Mayo Clin Proc 2014; 89:163–172. [DOI] [PubMed] [Google Scholar]
- 30.Liao CC, Su TC, Sung FC, et al. Does hepatitis C virus infection increase risk for stroke? A population-based cohort study. PLoS One 2012; 7:e31527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liao CC, Chou YC, Yeh CC, et al. Stroke risk and outcomes in patients with traumatic brain injury: 2 nationwide studies. Mayo Clin Proc 2014; 89:163–172. [DOI] [PubMed] [Google Scholar]
- 32.McDonald HI, Nitsch D, Millett ER, et al. New estimates of the burden of acute community-acquired infections among older people with diabetes mellitus: a retrospective cohort study using linked electronic health records. Diabet Med 2014; 31:606–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoshida M, Mita T, Yamamoto R, et al. Combination of the Framingham risk score and carotid intima-media thickness improves the prediction of cardiovascular events in patients with type 2 diabetes. Diabetes Care 2012; 35:178–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maeda Y, Inoguchi T, Etoh E, et al. Brachial-ankle pulse wave velocity predicts all-cause mortality and cardiovascular events in patients with diabetes: the Kyushu Prevention Study of Atherosclerosis. Diabetes Care 2014; 37:2383–2390. [DOI] [PubMed] [Google Scholar]
- 35.Ivers RQ, Cumming RG, Mitchell P, et al. Diabetes and risk of fracture: the Blue Mountains Eye Study. Diabetes Care 2001; 24:1198–1203. [DOI] [PubMed] [Google Scholar]
- 36.Fagour C, Gonzalez C, Pezzino S, et al. Low physical activity in patients with type 2 diabetes: the role of obesity. Diabetes Metab 2013; 39:85–87. [DOI] [PubMed] [Google Scholar]
- 37.Molsted S, Johnsen NF, Snorgaard O. Trends in leisure time physical activity, smoking, body mass index and alcohol consumption in Danish adults with and without diabetes: a repeat cross-sectional national survey covering the years 2000 to 2010. Diabetes Res Clin Pract 2014; 105:217–222. [DOI] [PubMed] [Google Scholar]
- 38.Stark Casagrande S, Ríos Burrows N, Geiss LS, et al. Diabetes knowledge and its relationship with achieving treatment recommendations in a national sample of people with type 2 diabetes. Diabetes Care 2012; 35:1556–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Engström G, Stavenow L, Hedblad B, et al. Inflammation-sensitive plasma proteins, diabetes, and mortality and incidence of myocardial infarction and stroke: a population-based study. Diabetes 2003; 52:442–447. [DOI] [PubMed] [Google Scholar]
- 40.Xiang AH, Peters RK, Kjos SL, et al. Effect of thiazolidinedione treatment on progression of subclinical atherosclerosis in premenopausal women at high risk for type 2 diabetes. J Clin Endocrinol Metab 2005; 90:1986–1991. [DOI] [PubMed] [Google Scholar]


