Abstract
The aim of our large, population-based, cohort study was to explore the risk factors of acute renal failure (ARF) after liver transplant (LT) in Taiwan.
From the Taiwanese National Health Insurance Research Database, 2862 patients who had undergone LT without pretransplant dialysis between July 1, 1998, and December 31, 2012, were identified. Preoperative, operative, and perioperative risks factors were considered and analyzed using logistic regression analysis, after adjusting for age and sex. All patients were followed up until the study endpoint or death.
The final dataset included 214 patients with ARF and 2648 without ARF post-LT. Preoperative cerebrovascular diseases were the most important identifiable risk factor for ARF post-LT. Comparison of outcomes for patients “with” and “without” ARF indicated higher incidence rates of bacteremia, pneumonia, and postoperative bleeding, as well as longer stays in both intensive care unit and hospital. Kaplan–Meier mortality curves identified higher rates of mortality for patients’ developing ARF at 1-year post-LT and overall at 14.5 years postsurgery.
We provide evidence of a high incidence of ARF post-LT in Taiwan, with documented association of ARF with higher incidence rates of morbidity and mortality in this clinical population. The most important identifiable risk factor for ARF in our study was cerebrovascular diseases.
INTRODUCTION
Acute renal failure (ARF) is a serious and frequent clinical problem associated with liver transplantation (LT) surgery. The incidence of post-LT ARF has been reported to range between 17% and 95% in different studies,1–4 with renal replacement treatment required in 8% to 17% of patients who develop ARF post-LT.4,5 Patients requiring renal replacement therapy have a higher mortality rate than patients not requiring renal replacement therapy,5,6 as well as being at higher risk for health complications, such as sepsis, encephalopathy, and coagulopathy.1
Several factors have been associated with the development of ARF post-LT surgery, including pre-LT health status; type and volume of fluid transfused; duration of the surgery; medications used during the surgery; release of toxic free radicals; and cold or warm ischemia times.5,7–10 Effective therapies to lower the risk for the development of ARF post-LT include the prudent selection of candidates for LT, careful adjustment of drug doses and maintenance of electrolyte balance during surgery, and admission of patients at high risk for ARF to the intensive care post-LT.11 A more complete identification of the risk factors associated with post-LT ARF would assist transplant physicians in assessing the risk for comorbidities in their prospective LT recipients and, thereby, optimize preoperative and perioperative care to lower the risk for post-LT complications and improve patients’ prognosis.
The primary purpose of this study was to identify the independent risk factors for ARF in patients undergoing LT and to elucidate the long-term effects of post-LT ARF on patient outcomes. In this study, we evaluated ARF outcomes in patients who had undergone LT in Taiwan, between 1998 and 2012, and required post-LT dialysis.
MATERIALS AND METHODS
Data Collection
We conducted a retrospective, population-based, cohort study using Taiwan's National Health Insurance (NHI) database. De-identified and computerized data was provided by the Bureau of National Health Insurance (BNHI) which organized the claim data in the entire NHI system and established the National Health Insurance Research Database (NHIRD). The NHIRD contains basic patient information, medical data of the raw hospital medical claims, including clinical diagnostic codes based on the International Classification of Disease, Revision 9, Clinical Modification (ICD-9-CM). According to the NHI program, the diagnosis for LT must be provided by a transplant surgeon or gastroenterologist.
This study was evaluated and approved by the NHIRD research committee (NHIRD-103–103) and the institutional review board of Chang Gung Memorial Hospital.
Patient Identification and Selection
The flowchart for patient identification and selection is shown in Figure 1. LT patients were identified from the NHIRD using the ICD-9-CM codes V427 (LT status) and 996.82 (complications of transplanted liver), between July 1998, when LT was first covered by health insurance in Taiwan, and December 2012. Over this period, 4086 post-LT patients were registered in the NHIRD. This prospective group of patients was reviewed and LT recipients who did not undergo transplantation in Taiwan were excluded. Applying this criteria, 1148 patients were excluded due to the absence of an LT surgery code (505, 75020A, or 75020B). Another 76 patients, who received dialysis (ICD-9-CM 38.95, 39.27, 39.42, 39.95, 39.43, and 54.98) before LT surgery, were also excluded. The final study cohort consisted of 2862 LT recipients.
FIGURE 1.
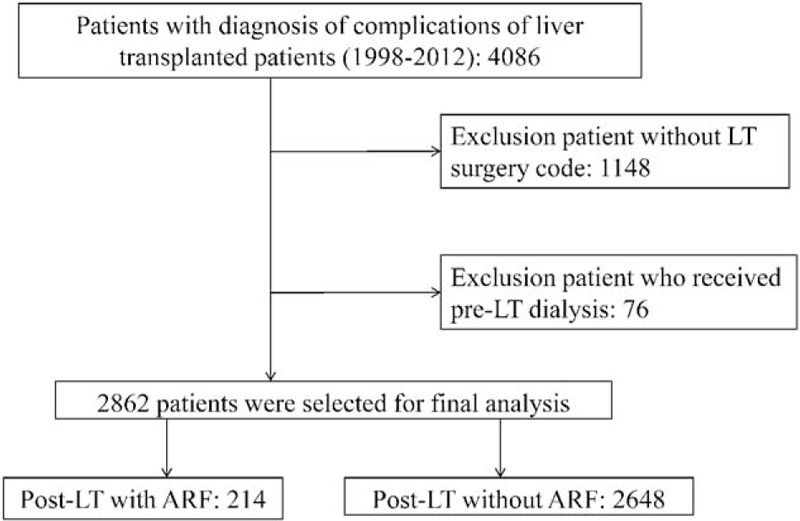
Study design and flowchart of patient selection.
Preoperative medical comorbidities were identified from diagnoses in the medical notes recorded either in the outpatient department (OPD) or the inpatient department (IPD). All diagnoses were verified using the ICD-9-CM codes with the following comorbidities identified among patients in our study cohort: hypertension (ICD-9-CM 401–405), pulmonary diseases (ICD-9-CM 490–496, A323, A325), diabetes mellitus (ICD-9-CM 250, A181), cerebrovascular disease (ICD-9-CM 430–438, A291-A299), coronary heart disease (ICD-9-CM 410–414, A279), congestive heart failure (ICD-9-CM 428, A289), vascular disease (ICD-9-CM 443, 444, A302), chronic hepatitis (ICD-9-CM 070, 571, 573.3, A347), psychosis (ICD-9-CM 300, 301, A214), esophageal varices (ICD-9-CM 456), portal hypertension (ICD-9-CM 572.3), obesity (ICD-9-CM 278), coagulation abnormalities (ICD-9-CM 790.92, 286.7, 286.9), ascites (ICD-9-CM 789.5), hepatic coma (ICD-9-CM 070.0, 070.20, 070.21, 070.31, 070.41, 070.51, 572.2, 348.3), chronic kidney disease (ICD-9-CM 585), cancer of the lymphatic and hematopoietic tissue (ICD-9-CM 200–208), gout (ICD-9-CM 274), and anemia (ICD-9-CM 280–289).
Post-LT ARF was identified from the relevant IDC-9-CM codes (ICD-9-CM 584, 585, V451 and V56) for patients who received dialysis during their admission for LT. Death was defined as the termination of national health insurance or receipt of insurance death codes.
Measurements
The primary outcome was the independent risk factors for post-LT ARF, including demographic and clinical factors. The secondary outcome was adverse effects post-LT, including length of stay in the intensive care unit (ICU), total length of hospital stay, bacteremia, postoperative bleeding, and pneumonia. Primary and secondary outcomes were compared between patients “with” and “without” ARF. Postoperative mortality rates at 30 days, 3 months, 1 year, and overall, defined from the 14.5 years of the study data, were also calculated. The survival time was calculated from the date of LT surgery to the date of death.
Statistical Analysis
Between-group differences in the distribution of demographic data, coexisting medical conditions, use of inpatient medical services (including length of hospitalization and ICU stay), and rates of postoperative complication were evaluated using t test, chi-squared, or Fisher's exact tests, as appropriate for the type and distribution of the data. Kaplan–Meier estimates with log-rank tests were used to compare between-group survival during the follow-up period. For the analyses of mortality, patients were followed up until an event (death) or censoring (loss to follow-up or end of the follow-up period), whichever occurred first. Risk factors for post-LT ARF were evaluated using multivariate logistic regression analysis adjusted for age, sex, and individually adjusted for pre-existing hypertension and cerebrovascular diseases. Odds ratios (OR), with 95% confidence intervals (CIs), were calculated for identified predictive factors. All analyses were performed using SAS software (version 9.3, SAS Institute Inc, Cary, NC), with a 2-sided P value <0.05 considered to be statistically significant.
RESULTS
Study Population and Baseline Characteristics
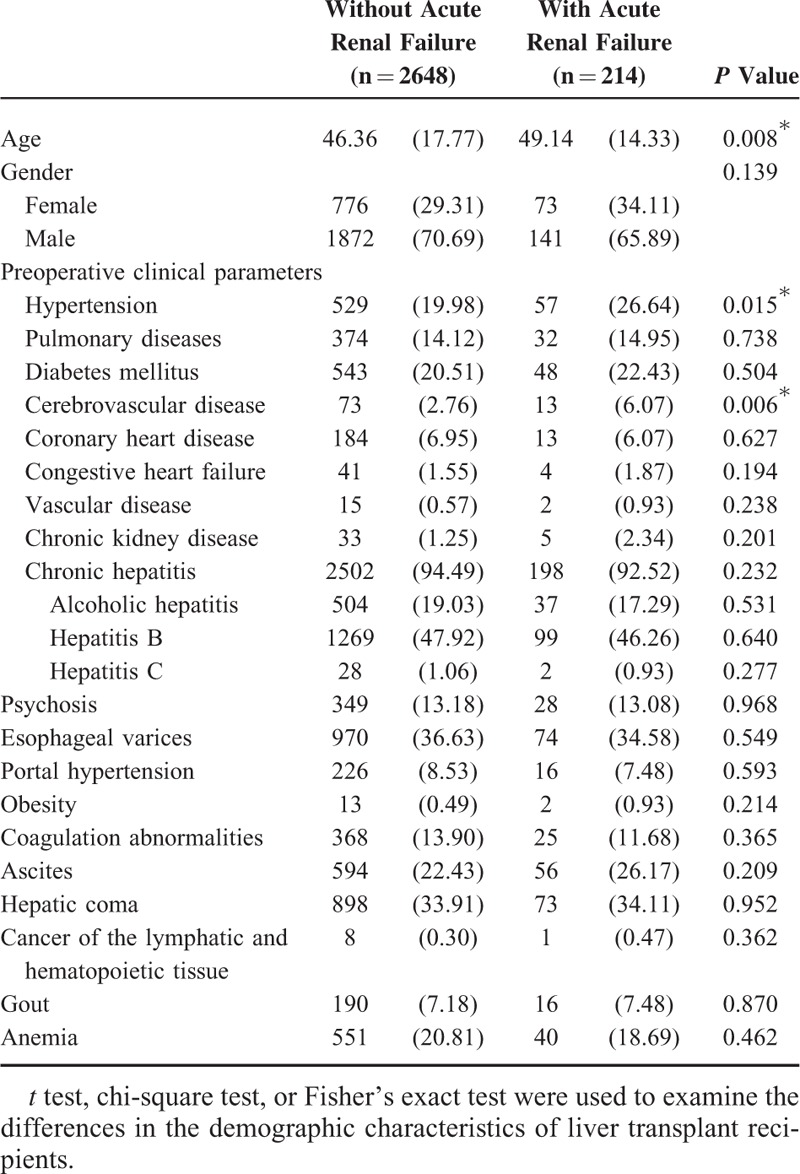
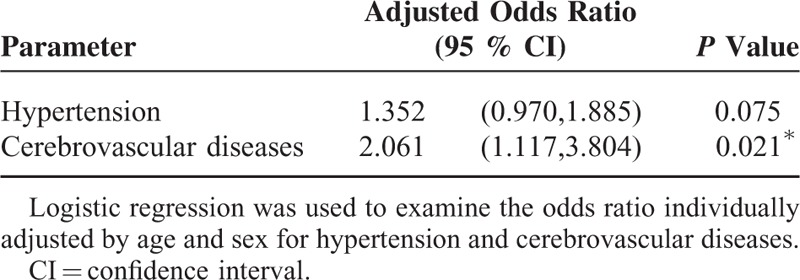
The data from 214 LT patients “with” ARF and 2648 LT patients “without” ARF; relevant demographic information of the study group is reported in Table 1. LT patients with ARF were more likely to be older than LT patients without ARF, and with a higher risk of preoperative hypertension (26.64% vs 19.98%, P = 0.015) and cerebrovascular diseases (6.07% vs 2.76%, P = 0.006). Chronic hepatitis was the most common medical comorbidity in both groups.
TABLE 1.
General Demographics of the Study Subjects
Post-LT Outcomes
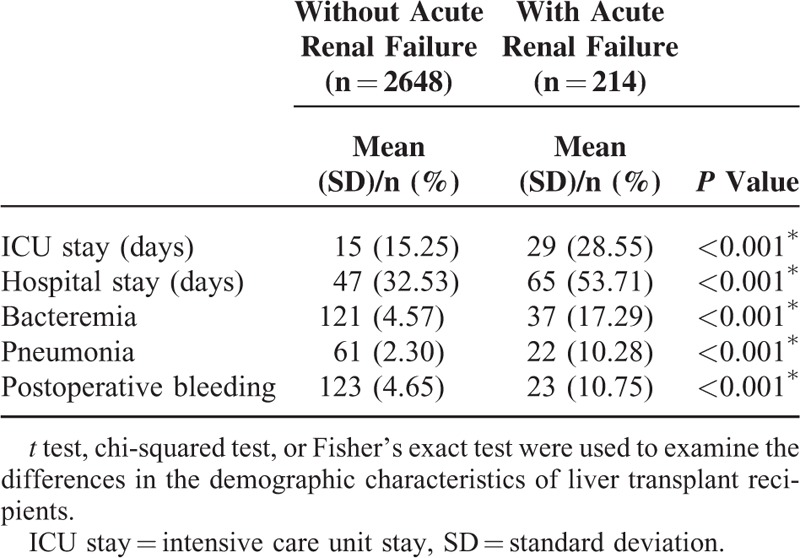
Clinical variables identified by univariate analysis as being associated with post-LT ARF are reported in Table 2. The length of ICU stay and duration of hospitalization were both longer in LT patients with ARF, compared to those without ARF (P < 0.001). The incidence rates of bacteremia, pneumonia, and postoperative bleeding were also higher in patients with ARF (P < 0.001).
TABLE 2.
Outcome Characteristics of Liver Transplant Recipients “With” or “Without” Acute Renal Failure
Mortality Rates
Mortality rates at 30 days, 3 months, 1 year, and overall (14.5 years), reported in Table 3, were higher in the LT patients with ARF, compared to those without ARF (P < 0.001). A total of 411 patients died during the study period. Unadjusted Kaplan–Meier survival curves, shown in Figure 2, indicated a 1-year post-LT survival rate of 71.96% for patients with ARF, compared to 94.07% for patients without ARF (P < 0.001). The overall 14.5 year survival rate, shown in Figure 3, was 64.02% for patients with ARF and 87.49% for those without ARF (P < 0.001).
TABLE 3.
Mortality Rates of Liver Transplant Recipients “With” or “Without” Acute Renal Failure
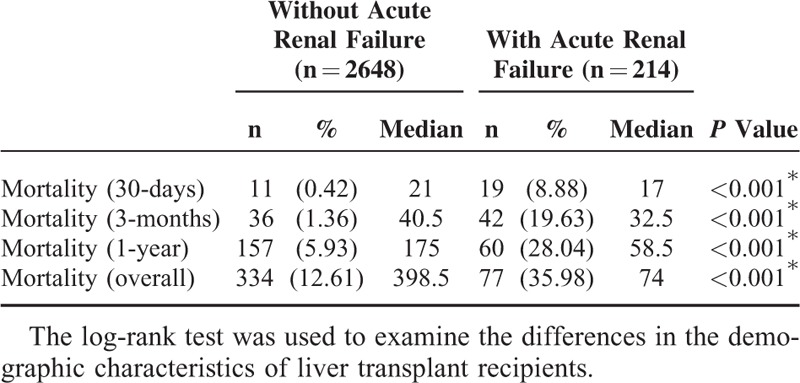
FIGURE 2.
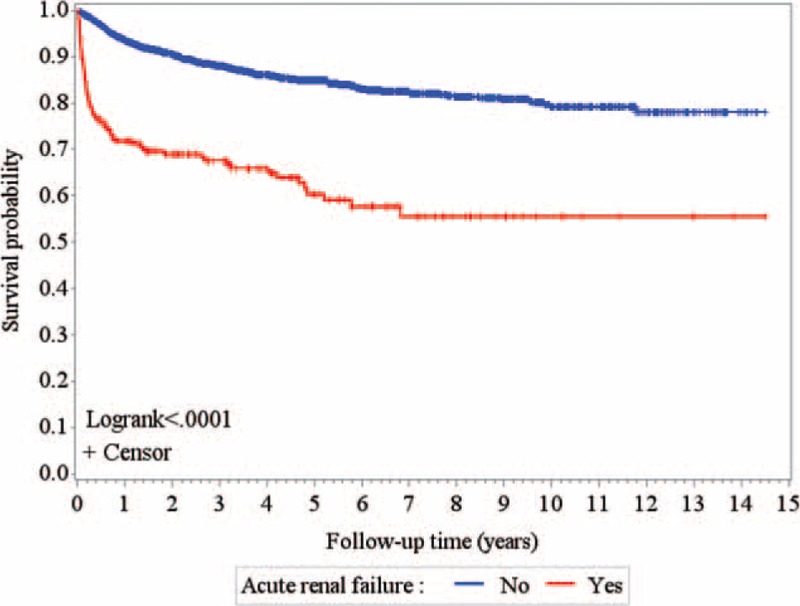
Unadjusted Kaplan–Meier survival curves after liver transplantation over the past 14.5 years.
FIGURE 3.
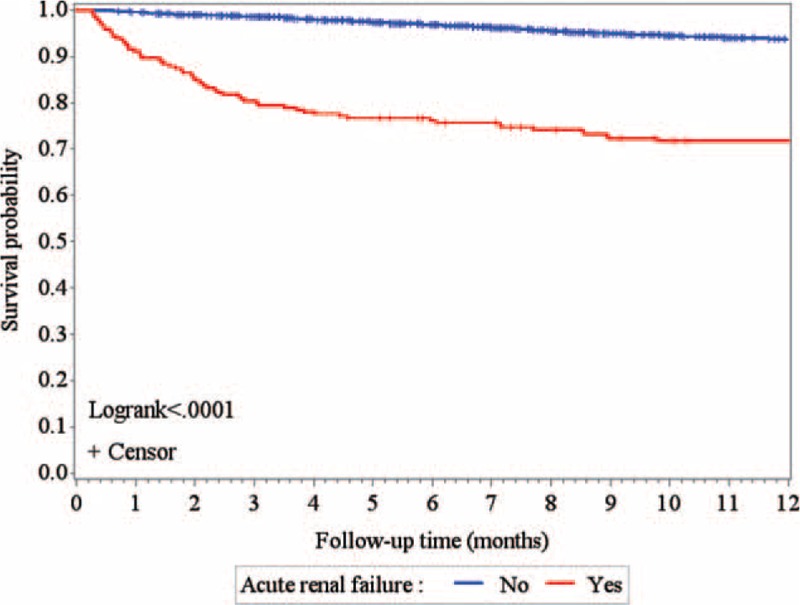
Unadjusted Kaplan–Meier survival curves of first-year patient survival after liver transplantation among liver transplantation recipients over the past 14.5 years.
Pre-Liver Transplant Predictors of Acute Renal Failure
To determine the independent factors which discriminated between patients with and without ARF post-LT, significant factors identified by univariate analysis, namely hypertension and cerebrovascular diseases, were further analyzed by logistic regression, with models adjusted for age and sex (Table 4). Cerebrovascular diseases were retained a unique risk factor for post-LT AFR.
TABLE 4.
Pre-Liver Transplant Predictors of Postoperative Acute Renal Failure by Multivariate Analysis
DISCUSSION
We performed a retrospective, population-based, cohort study of patients who received a LT between 1998 and 2012, with the aim of describing the incidence, risk factors, and outcomes associated with post-LT ARF.
Key Findings
We found that 7.5% of patients receiving an LT in Taiwan developed post-operative ARF. The most important identifiable risk factor for ARF was cerebrovascular diseases. Patients developing postoperative ARF also had a higher rate of bacteremia, pneumonia, postoperative bleeding, and longer ICU and hospital stays. Finally, the 1-year and overall mortality rate was higher in patients who developed ARF post-LT.
Comparison With Previous Studies and Interpretation of Results
Our incidence rate of post-LT ARF is lower than previously reported incidence rates.1–4 This difference in incidence rate may be explained by differences in the definition of the severity of ARF among studies. As an example of this inconsistency in definition, in 2002, Acute Dialysis Quality Group proposed a change in diagnostic criteria from ARF to acute kidney injury (AKI).12,13 As the NHIRD is a large secondary database, information on lab-based measures of kidney function, such as serum creatinine, urine output, and glomerular filtration rate, were not available to include in our retrospective analysis. We identified patients who developed ARF post-LT uniquely from the ICD-9-CM codes for ARF and dialysis entered in the medical chart during the admission period for LT. As this is a specific definition of ARF, it is possible that the true incidence rate of ARF post-LT may have been underestimated. It is important to note, however, that other studies have reported incidence rates of ARF requiring renal replacement therapy after LT of 8% to 17%,4,5 which is comparable to our study outcomes.
Cabezuelo et al14 proposed that the risk for ARF post-LT was associated with specific underlying factors: age, sex, pre-transplant comorbidities, indications for LT, and Child-Pugh stage. Of these, the following pre-operative potential risks for ARF were available in the NHIRD: age, sex, and pre-transplantation comorbidities. Of these pre-transplantation risk factors, only cerebrovascular diseases was identified as having a significant impact on postoperative renal failure after LT, after adjusting for age and sex.
Compared to patients who did not develop ARF post-LT, significantly higher proportion of patients with ARF suffered from bacteremia, pneumonia, and postoperative bleeding. The bidirectional interaction between ARF and sepsis has previously been described15 and probably results from immune dysfunction induced by ARF.16 The mechanism linking ARF and surgical complications could plausibly be related to longer durations of ICU and hospital admission.11,14,17 Our data also confirm that postoperative ARF has an important modifying influence on long-term patient survival.18 The postoperative mortality was higher in patients with ARF than in those without ARF, not only at 1-year post-LT but also overall at 14.5 years.
Limitations
Our large retrospective population-based cohort study has several limitations that warrant consideration. Foremost, the NHIRD is a secondary database and, therefore, does not include actual medical examination data, such as findings of the physical examination, laboratory results, and specific etiological data of the end-stage liver disease leading to LT,19–21 or intra-operative data, such as hemodynamics, operative time, and medications used during the surgery7,15,22,23 which may be closely linked with the development of ARF after LT. Our cohort included patients over a 14.5 year period, back to 1998, and, therefore, the data includes differences and variation in the selection criteria for LT, the type of liver donor (deceased or living donor), and immunosuppressive regimens therapy.24–26 Therefore, generalizability of our study may be limited. Despite these limitations, our population-based cohort analysis of all identified patients who developed ARF post-LT in Taiwan over a 14.5-year period is important in view of the paucity of contemporary literature on post-LT ARF at a population-based level. In addition, the chronological relation between ARF and variables during the hospitalization for liver transplant was not clearly identified. There is no explanation for the identification of timing of each comorbidity or the development of ARF. Previous studies have shown that preoperative model for end-stage liver disease (MELD) score and renal function are predisposing factors for AKI following LT.27–28 As MELD score and renal function were not collected, it remains to be the limitation of the study.
CONCLUSION
Cerebrovascular diseases are the most important, identifiable risk factor for ARF post-LT. The development of ARF post-LT is associated to higher rates of morbidity and mortality in this clinical population. Early identification, and possible management, of risk factors for ARF could improve outcomes of LT and lower the risk for patient comorbidities postsurgery.
Footnotes
Abbreviations: ARF = acute renal failure, ICD-9-CM = International Classification of Disease Revision 9 Clinical Modification, IPD = inpatient department, LT = liver transplantation, LTR = liver transplant recipient, MELD = model for end-stage liver disease, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, OPD = outpatient department.
Contributions: conception and design: H-P Chen, H-P Yu; acquisition of data: H-PC, Y-FT; data analysis and interpretation: J-RL, H-PC, F-CL, H-PY; manuscript drafting and critical revising: H-PC, J-RL, H-PY; final approval of manuscript: all authors.
The authors have no conflicts of interest to disclose.
This study was based in part on data from the NHIRD provided by the Bureau of National Health Insurance, Department of Health, and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent the views of the Bureau of National Health Insurance, Department of Health, or National Health Research Institutes.
REFERENCES
- 1.Fraley DS, Burr R, Bernardini J, et al. Impact of acute renal failure on mortality in end-stage liver disease with or without transplantation. Kidney Int 1998; 54:518–524. [DOI] [PubMed] [Google Scholar]
- 2.McCauley J, Van Thiel DH, Starzl TE, et al. Acute and chronic renal failure in liver transplantation. Nephron 1990; 55:121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lima EQ, Zanetta DM, Castro I, et al. Risk factors for development of acute renal failure after liver transplantation. Ren Fail 2003; 25:553–560. [DOI] [PubMed] [Google Scholar]
- 4.Bilbao I, Charco R, Balsells J, et al. Risk factors for acute renal failure requiring dialysis after liver transplantation. Clin Transplant 1998; 12:123–129. [PubMed] [Google Scholar]
- 5.Gonwa TA, Mai ML, Melton LB, et al. Renal replacement therapy and orthotopic liver transplantation: the role of continuous veno-venous hemodialysis. Transplantation 2001; 71:1424–1428. [DOI] [PubMed] [Google Scholar]
- 6.Ishitani M, Wilkowski M, Stevenson W, et al. Outcome of patients requiring hemodialysis after liver transplantation. Transplant Proc 1998; 25:1762–1763. [PubMed] [Google Scholar]
- 7.Gainza FJ, Valdivieso A, Quintanilla N, et al. Evaluation of acute renal failure in the liver transplantation perioperative period: incidence and impact. Transplant Proc 2002; 34:250–251. [DOI] [PubMed] [Google Scholar]
- 8.Gonwa TA, McBride MA, Anderson K, et al. Continued influence of preoperative renal function on outcome of orthotopic liver transplant (OLTX) in the US: where will MELD lead us? Am J Transplant 2006; 6:2651–2659. [DOI] [PubMed] [Google Scholar]
- 9.Nuno J, Cuervas-Mons V, Vicente E, et al. Renal failure after liver transplantation: analysis of risk factors in 139 liver transplant recipients. Transplant Proc 1995; 27:2319–2320. [PubMed] [Google Scholar]
- 10.Contreras G, Garces G, Quartin AA, et al. An epidemiologic study of early renal replacement therapy after orthotopic liver transplantation. J Am Soc Nephrol 2002; 13:228–233. [DOI] [PubMed] [Google Scholar]
- 11.Junge G, Schewior LV, Kohler S, et al. Acute renal failure after liver transplantation: incidence, etiology, therapy, and outcome. Transplant Proc 2006; 38:723–724. [DOI] [PubMed] [Google Scholar]
- 12.Webb S, Dobb G. ARF, ATN or AKI? It's now acute kidney injury. Anaesth Intensive Care 2007; 35:843–844. [DOI] [PubMed] [Google Scholar]
- 13.Schrier RW. ARF, AKI, or ATN. Nat Rev Nephrol 2010; 6:125. [DOI] [PubMed] [Google Scholar]
- 14.Cabezuelo JB, Ramirez P, Rios A, et al. Risk factors of acute renal failure after liver transplantation. Kidney Int 2006; 69:1073–1080. [DOI] [PubMed] [Google Scholar]
- 15.Kaido T, Mori A, Ogura Y, et al. Pre- and perioperative factors affecting infection after living donor liver transplantation. Nutrition 2012; 28:1104–1108. [DOI] [PubMed] [Google Scholar]
- 16.Kurts C, Panzer U, Anders HJ, et al. The immune system and kidney disease: basic concepts and clinical implications. Nat Rev Immunol 2013; 13:738–753. [DOI] [PubMed] [Google Scholar]
- 17.Neau-Cransac M, Morel D, Bernard PH, et al. Renal failure after liver transplantation: outcome after calcineurin inhibitor withdrawal. Clin Transplant 2002; 16:368–373. [DOI] [PubMed] [Google Scholar]
- 18.Yalavarthy R, Edelstein CL, Teitelbaum I. Acute renal failure and chronic kidney disease following liver transplantation. Hemodial Int 2007; 11:S7–12. [DOI] [PubMed] [Google Scholar]
- 19.Ferraz-Neto BH, Zurstrassen MP, Hidalgo R, et al. Analysis of liver transplantation outcome in patients with MELD Score>or=30. Transplant Proc 2008; 40:797–799. [DOI] [PubMed] [Google Scholar]
- 20.Akyildiz M, Karasu Z, Arikan C, et al. Impact of pretransplant MELD score on posttransplant outcome in living donor liver transplantation. Transplant Proc 2004; 36:1442–1444. [DOI] [PubMed] [Google Scholar]
- 21.Jacob M, Copley LP, Lewsey JD, et al. UK, Ireland Liver Transplant Audit. Pretransplant MELD score and post liver transplantation survival in the UK and Ireland. Liver Transpl 2004; 10:903–907. [DOI] [PubMed] [Google Scholar]
- 22.Barreto AG, Daher EF, Silva Junior GB, et al. Risk factors for acute kidney injury and 30-day mortality after liver transplantation. Ann Hepatol 2015; 14:688–694. [PubMed] [Google Scholar]
- 23.Sirivatanauksorn Y, Taweerutchana V, Limsrichamrern S, et al. Recipient and perioperative risk factors associated with liver transplant graft outcomes. Transplant Proc 2012; 44:505–508. [DOI] [PubMed] [Google Scholar]
- 24.Volk ML, Biggins SW, Huang MA, et al. Decision making in liver transplant selection committees: a multicenter study. Ann Intern Med 2011; 155:503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zarrinpar A, Busuttil BW. Liver transplantation: past, present and future. Nat Rev Gastroenterol Hepato 2013; 10:434–440. [DOI] [PubMed] [Google Scholar]
- 26.Strasberg SM, Howard TK, Molmenti EP, et al. Selecting the donor liver: risk factors for poor function after orthotopic liver transplantation. Hepatology 1994; 20:829–838. [DOI] [PubMed] [Google Scholar]
- 27.Wong F, Nadim MK, Kellum JA, et al. Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut 2011; 60:702–709. [DOI] [PubMed] [Google Scholar]
- 28.Hilmi IA, Damian D, AI-Khafaji A, et al. Acute kidney injury following orthotopic liver transplantation: incidence, risk factors, and effects on patient and graft outcomes. Br J Anaesth 2015; 114:919–926. [DOI] [PubMed] [Google Scholar]


