Abstract
Admission rate and length of stay (LOS) are two hospital performance indicators that affect the quality of care, patients’ satisfaction, bed turnover, and health cost expenditures. The aim of the study was to identify factors associated with higher admission rates and extended average LOS among acutely poisoned children at a single poison center, central Saudi Arabia.
This is a cross-sectional, poison and medical chart review between 2009 and 2011. Exposures were child characteristics, that is, gender, age, body mass index (BMI), health history, and Canadian 5-level triage scale. Poison incident characteristics were, that is, type, exposure route, amount, form, home remedy, and arrival time to center. Admission status and LOS were obtained from records. Chronic poisoning, plant allergies, and venomous bites were excluded. Bivariate and regression analyses were applied. Significance at P < 0.05.
Of the 315 eligible cases, (72%) were toddlers with equal gender distribution, (58%) had normal BMI, and (77%) were previously healthy. Poison substances were pharmaceutical drugs (63%) versus chemical products (37%). Main exposure route was oral (98%). Home remedy was observed in (21.9%), which were fluids, solutes, and/or gag-induced vomiting. Almost (52%) arrived to center >1 h. Triage levels: non-urgent cases (58%), less urgent (11%), urgent (18%), emergency (12%), resuscitative (1%). Admission rate was (20.6%) whereas av. LOS was 13 ± 22 h. After adjusting and controlling for confounders, older children (adj.OR = 1.19) and more critical triage levels (adj.OR = 1.35) were significantly associated with higher admission rates compared to younger children and less critical triage levels (adj.P = 0.006) and (adj.P = 0.042) respectively. Home remedy prior arrival was significantly associated with higher av. LOS (Beta = 9.48, t = 2.99), compared to those who directly visited the center, adj.P = 0.003.
Hospital administrators are cautioned that acutely poisoned children who received home remedies prior arrival are more likely to endure an extended LOS. This non-conventional practice is not recommended.
INTRODUCTION
Promotion of the clinical and economic performances for any healthcare system is an ongoing challenge and demand.1–3 Performance indicators, such as the average length of stay (av. LOS), have been adopted as tools for quality control and improvement to achieve locally and internationally set objectives.2,4 The diagnosis-related group (DRG) is an internationally recognized payment system that links certain clinical diagnoses with an expected admission and LOS.5 A commonly reported DRG at emergency pediatric departments is substance poisoning.6 In 2014, 40% of the reported poison exposure cases in the USA were children (<6 years)7 and in Saudi Arabia 1272 poisoned children (1–15 years) were identified by the eastern regional poison center between 2011 and 2013.8
The admission rate and av. LOS in poisoned children depends on a number of associated factors. Age, body structure, co-morbidities as well as the nature of poison (type, amount, exposure route) are all known to influence the severity of clinical outcomes and subsequently admission rate and LOS.9–13 In addition, one study stated that home remedies provided to orally poisoned toddlers had put them at higher risk for the abnormal physical examination.6 Therefore, substance poisoning is one of the DRGs that are linked to key hospital performance indicators that are sensitive to variant child and poison incident characteristics.
Admission rates and LOS of poisoned children have been reported in a number of studies. LOS among poisoned children ranged from 1 hour to 9 days,14,15 with average between 1.2 ± 1.3 and 3.1 ± 4.4 days,14–16 and median around 1 day.17 On the other hand, a study stated that 46% of admitted, acutely poisoned cases were children,16 whereas others stated that 13.3% of poisoned children visiting emergency departments (EDs) were hospitalized.11 Also, it was noted that 60% to 70% of poisoned children are usually asymptomatic; often released for home observation.18–20
Identifying and attempting to modify variables associated with higher admission rates and extended length of stay of poisoned children will assist hospital administrators in achieving better performance indicators. Other unmodifiable variables such as gender, age category, and poison type may serve as admission predictors for care managers and bed utilization coordinators. In literature, not all associated variables were investigated and tested among poisoned children (home remedies), a nonmedical home initiated practice that still exists in some communities.6
The aim was to assess the admission rate and average length of stay (av. LOS) among children complaining of acute poisoning and to identify their associated factors, at a single poison center, central Saudi Arabia. This was fulfilled by: (1) obtaining the characteristics of children and poison incident, (2) assessing their admission status and LOS, (3) identifying significant factors associated with higher admission rates and extended av. LOS.
METHODS
Study Design
This is a retrospective cross-sectional, poison report and patient medical record review.
Study Area/Setting
King Abdulaziz Medical City (KAMC) is a distinguished Joint Commission International (JCI) accredited tertiary health care facility established in 1983. KAMC is a certified poison center enlisted under the National Drug & Poison Information Center (NDPIC) and responds to any public or health care professional queries regarding any poison incident. KAMC is dedicated to provide health services to the military community of Saudi National Guards and their dependents. Majority of this community reside in secured well-established compounds nearby KAMC, where primary health clinics, schools, and recreational areas are allocated for them.
Within the vicinity of KAMC, a pediatric ED has an estimate of 85 beds allocated for admissions with various emergency care levels. The pediatric ED has a team of >70 emergency specialized pediatric medical staff who provide services to numerous admissions annually.21 On-call toxicologists or physicians with an advanced training on toxicology are readily available at all times.
Study Subjects and Sampling Technique
By convenience, poison reports and medical charts of children complaining of acute poisoning (medication and/or chemical substance) between 2009 and 2011 were reviewed. Inclusion criteria targeted acutely poisoned children (aged 3 month to 15 years). Cases of chronic poisoning, plant allergies, venomous bites, or stings were excluded.
Data Collection
At KAMC, poisoned children are triaged and attained for by ED physicians and licensed oncall toxicologists. As per hospital policy, a poison report form needs to be filled and signed by the medical staff for each incident. In addition, the child's health progress is recorded electronically on a system called Q-CPR, which is later archived into the hospital medical records. Study investigators incorporated their data collection forms within the hospital poison forms (between 2009 and 2011) based on an agreement with the chairman of the department. This agreement was supported by a research scientific committee, ethics committee, and chief executive office approval memorandums.
Study investigators delivered group training sessions for a team of 35 ED pediatric physicians on how to properly obtain the informed consent and gather study-related information. Two certified clinical research coordinators from King Abdullah International Medical Research Center (KAIMRC) were also assigned and trained to follow-up daily on this process and ensure that the forms are completed properly. The research coordinators used the children's identifiers to track the admission status and calculate their length of hospital stay from Q-CPR.
Noneligible patients or those with unclear contact information were dropped out. Missing variables in the forms were dealt with statistically. Validation of the collected data was done by verifying it with the records and contacting the parents (1–2 days after the incident). Phone calls after discharge were very important as questioning the anxious and stressed parents during the initial ED visit often leads to an inaccurate description of the incident details.22,23
Data Collection Tool
The components of data collection tool were:
Informed consent: name, medical record number, date/time, contact information, signatures.
Child characteristics: age group, gender, medical/psychiatric history, body mass index (BMI) for 2 years and above, plotted on sex-specific growth charts,24 and classified as underweight (<5th percentile), healthy weight (5–85th percentile), overweight (86–94th percentile), and obese (≥95th percentile). Initial ED assessment was based on the Canadian 5-level triage scale: resuscitative (I), emergency (II), urgent (III), less urgent (IV), non-urgent (V).
Poison incident characteristics: substance type, number of agents, estimated amount, form (pill, capsule, liquid, cream), exposure route, arrival time to ED (hours), home remedies provided. This section was sourced out from the reporting forms used by the Saudi Ministry of Health (MOH) and NDPIC.
Performance indicators: children who stayed > 24 h in the ED and/or admitted to any in-hospital ward were accounted as admissions. The admission rate was calculated by dividing the number of admitted poisoned children by the total number of poisoned children multiplied by 100 during the study period. Length of hospital stay was calculated by subtracting the time of discharge from the time of ED triage assessment in hours. Timings were obtained from medical records.
Ethical Considerations
Confidentially of the children's information was preserved by all study personnel as part of their job requirement. A record of child identifier aided in the follow-up on outcomes and validation of data collected. Signed informed consents were stapled to the data collection forms and preserved in charts. Study investigator had no influence on parents self-reporting. This study was approved by the Institutional Review Board of the Ministry of National Guard-Health Affairs (MNG-HA), Riyadh, Saudi Arabia (Protocol#: RR08/019).
Data Management and Analysis
Data entry and analysis were performed using SPSS statistical software (Version 22; SPSS Inc, Chicago, IL). Categorical variables such as gender, BMI group, and others were presented in frequency and percentages, whereas continuous variables such as av. LOS were presented in mean (x), standard deviation ( ± SD), and 95% confidence interval (95% CI). Bi-variate analysis was conducted using Student's t test and one-way ANOVA for continuous outcomes (av. LOS), whereas chi-square was used for categorical outcomes (admission). Binomial regression and multilinear regression were constructed to identify the significant associations with admission status and av. LOS respectively, and control for all possible confounders. Adjusted odds ratio (adj. OR) and 95% confidence interval (95%CI) were obtained. Significance level set at P value <0.05.
RESULTS
Child and Poison Incident Characteristics
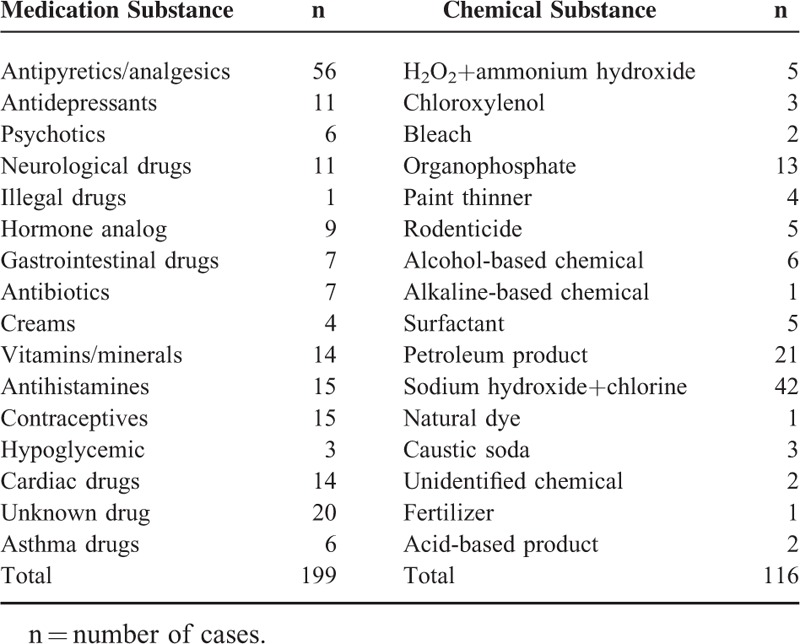
Eligible study participants were 315 (92%), of which the majority (72%) were toddlers (1–3 years) (Table 1). Equal gender distribution was observed (59%:41%). Almost 58% had normal weights, whereas 77% had negative medical/psychiatric history. All their fathers were full-time employees, whereas the majority of mothers were unemployed housewives (91%). The parents’ level of education varied as 22% of fathers had a university degree, whereas 70% had a certain level of school education. Mothers were slightly more educated as 31% had a university degree and 55% had school education. The average family size was 6 members, ranging between 3 and 13. Drug poisoning was observed in 63%, whereas chemical product poisoning was exhibited in 37%. The majority of children were exposed to the poison product accidentally 92%, whereas 6% were due to over dosage of their prescribed medications (mainly in infants) and 2% were suspected cases of child abuse or suicidal attempt. The main exposure route was oral 98%. In the drug poison group, the most common poison agents were antipyretics and analgesics (n = 56), whereas in the chemical group (n = 42) it was sodium hydroxide (a household product) (Table 2). Home remedies were provided to 22% of poisoned children before their visit to ED, which included forcing the child to drink plain water, lemon juice, milk, yogurt, salt/sugar solutes, and/or vomiting by manually induced gag reflex. The time between the incident and arrival to ED was >1 h in 52%. Two-thirds of cases were nonurgent, whereas 1.3% were at the resuscitative level. No fatalities were reported in this study.
TABLE 1.
Child and Poison Incident Characteristics Compared by Admission Rate and Average Length of Stay
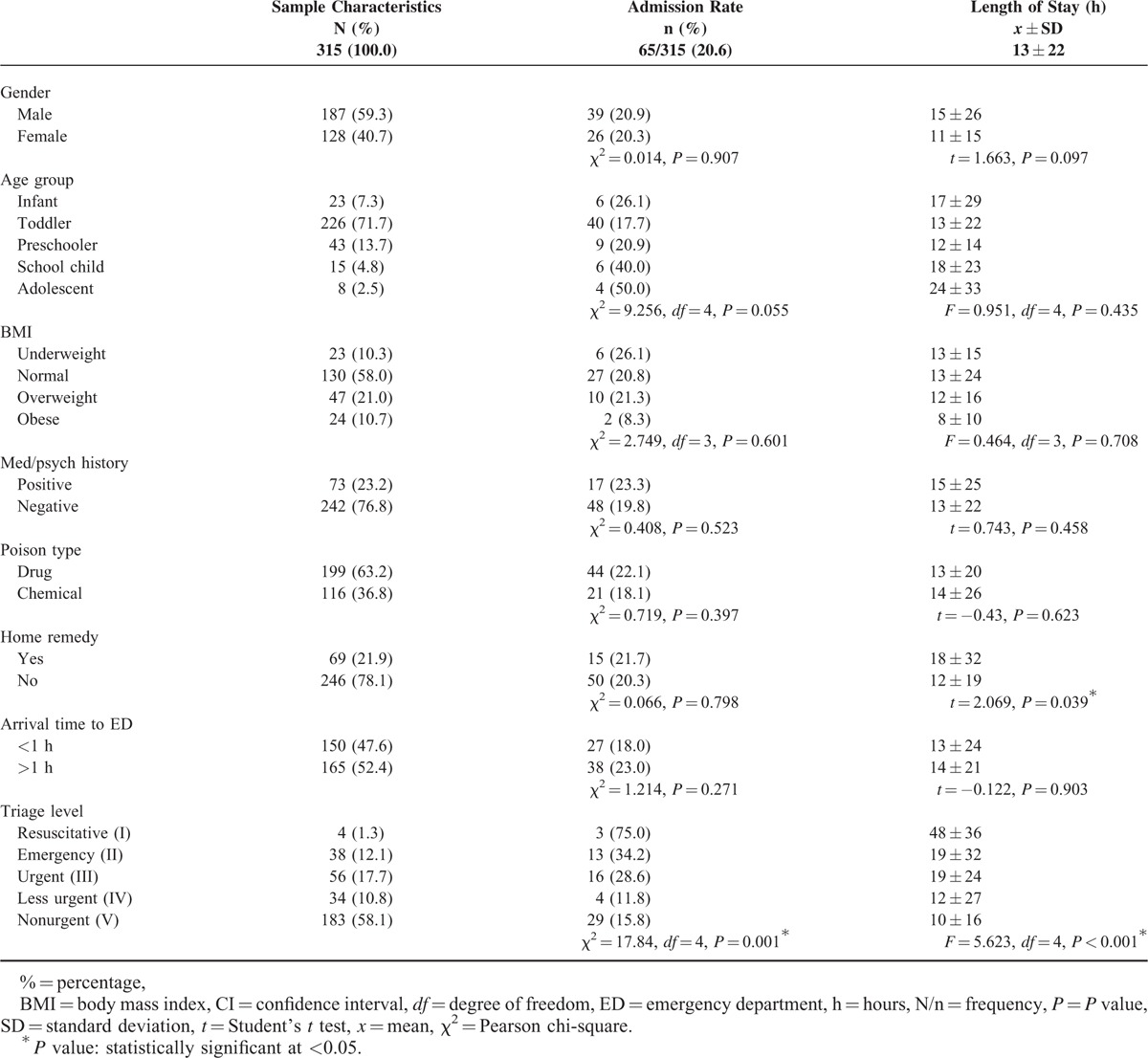
TABLE 2.
Frequency List of Poison Substances (Mutually Exclusive)
Hospital Indicator Characteristics
Over all admission rate was 65/315 (20.6%), whereas the av. LOS was 13 ± 22 h, median was 5 h, and ranged 0.7 h to 7.4 days. Initial analysis showed that more critical triage levels was significantly associated with higher rates of admission (P = 0.001) and a more extended av. LOS (P < 0.001). Home remedies were significantly associated with an extended av. LOS (18 ± 32 h, P = 0.039), compared to children directly visiting the ED post incident (12 ± 19 h) (Table 1).
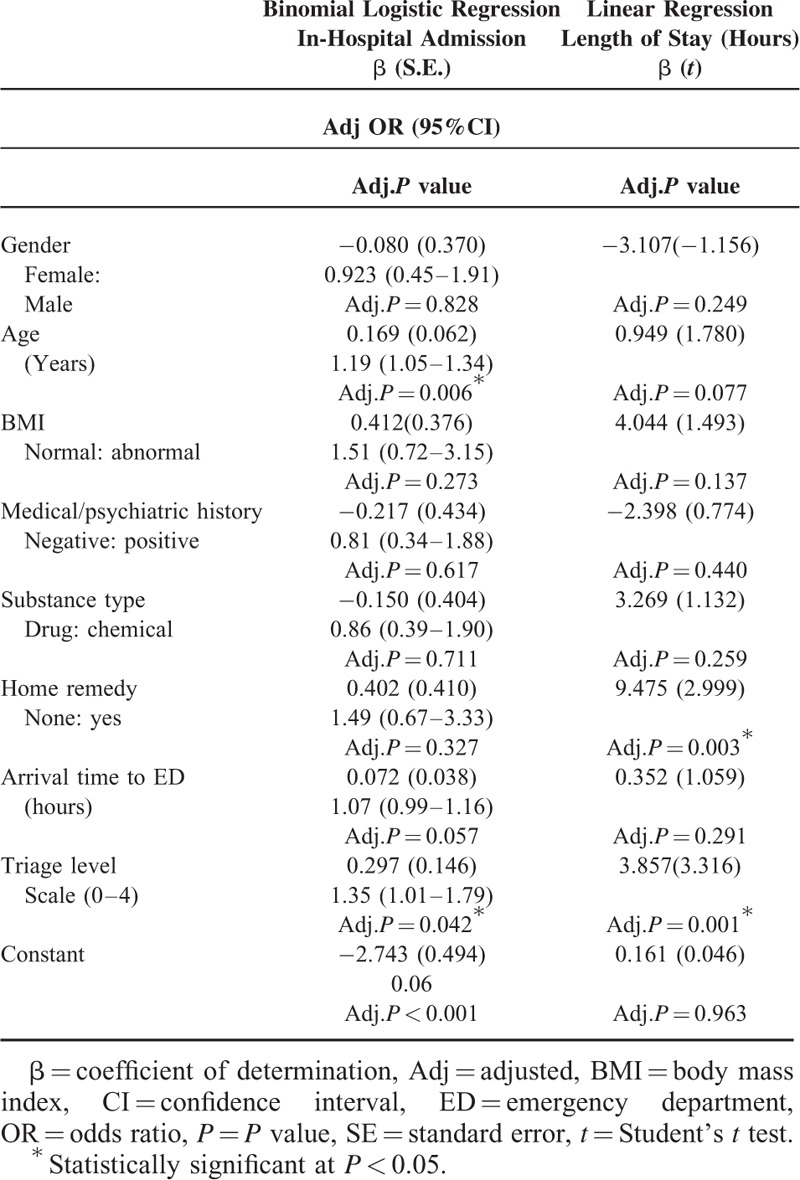
Binary logistic and linear regression models were constructed to further investigate the combined effect of all exposures and adjust for all possible confounders (Table 3). Older children were significantly more likely, adjOR = 1.19(1.05–1.34), to be admitted compared to younger children (adj.P = 0.006). More critical triage levels were more likely, adj.OR = 1.35(1.01–1.79), to be admitted (adj.P = 0.042). Poisoned children receiving home remedies prior ED visit had significantly endured a more extended av. LOS (Beta = 9.48, t = 2.99) compared to those who directly visited the ED (adj.P = 0.003).
TABLE 3.
Significantly Associated Factors With Higher Admission Rates and Extended Length of Stay
DISCUSSION
Length of hospital stay is usually affected by gender, age, arrival time to ED, mode of transport, severity of poisoning, and type of agent among poisoned victims.25 In this setting, poisoned children showed an overall lesser average and range of LOS when compared to other settings in USA, Finland, and an African country.14–16 Findings in this study indicate that the quality of performance indicators was not in favor of children receiving home remedies before their ED visit, even after adjusting for all confounders. The home remedy group has significantly endured an av. LOS (18 ± 32 h) that is a (6 ± 13 h) delay compared to the group directly visiting ED (12 ± 19 h). This rejects the null hypothesis that states such practice (as perceived by parents) improves the clinical and hospital outcomes.
Parents thought that by administering home remedies their children would not be in need for in-hospital admission, whereas in fact it slightly increased the admission rate, but with no statistical significance (20.3% vs 21.7%). More critical triage level children were found to endure higher admission rates and extended av. LOS due to the severity of clinical status. Older children seem to be more likely admitted compared to younger ages (adj.P = 0.006).
The type of reimbursement system or health insurance plan plays a significant role in the patient length of stay at hospitals, because reimbursable hospital services must be medically necessary, actually provided, and accurately documented in the medical records.26 A hospital billing department reported that the 1st hours of hospitalization for any patient admitted encompass the highest patient charges. These are the return profits that hospitals get reimbursed for the diagnostic and therapeutic procedures that patients undergo in the first hours after admission. The percentage of profit will then drop by 40% to 50% per day when a patient's LOS exceeds the average expected for a DRG.27 A delayed child stay at any ED congests the wards and blocks beds against potential admissions. Accelerated discharges are less expensive than standard care on all direct economic measures such as staff time and LOS.28 Therefore, poisoned children exceeding their predicted LOS due to such home remedies are slowing the bed turnover within the healthcare system and decreasing profits.
Patient satisfaction is another great concern that is inseparable from care, quality, and hospital operations.29 Studies stated that shorter length of stay showed more satisfaction and elevated stress off panicking parents after a poisoning incident.29,30 In this study, advising parents to abide with poison management guidelines and refrain from administering home remedies will eventually promote early discharge, minimize the chance of contracting nosocmial infections, and boost patient satisfaction.
The characteristics of child and poison incidents in this study were comparable to a number of published studies. In the USA, toddlers are indeed the highest risk group among children (73%) which is similar to the figures in this study 226/315 (72 %).11,31 In addition, no gender difference in poison exposures was reported by the Spanish society of pediatric emergencies,9 which was similar to the finding in this study. Studies in the region stated that paracetamol and other analgesics,12,13,32 as well as pesticides and household products12 were the most common ingested substances. In this study, antipyretics were indeed the most common, but the most common chemical was sodium hydroxide products followed by petroleum products. In literature, oral poison ingestion remains a leading exposure route,13 likewise in this study (98%). Majority of study participants upon triage were classified as non to less urgent (68%) which is comparable to the Irish 2013 poison center report stating that 70% of their cases were symptomless.12
Home remedies are non-medical practices that still exist in some communities despite the fact that it is not recommended by poison management guidelines.10,33 The 2 main types of home remedies performed by parents were orally administered fluids and/or gag triggered vomiting. Food and beverages can have a profound impact on many medications taken in therapeutic doses,34–37 but little is known on its desired effects to treat toxic dosages in poisoning. Gag triggered vomiting in this study was a risky and unpleasant practice that exerted physical and psychological stress on children.38 Moreover, some chemical substances ingested are irritating and may damage the lining of the esophagus, pharynx, and oral mucosal surface during vomiting.
Limitations
The present study was conducted in a single poison center that serves a military community and their dependents; therefore it might limit its generalizability. Data collection was executed over a 2-year period. Further eligible cases would have been recruited to increase the statistical power of the sample, but study investigators had to abide with the approved time limit of data collection as per the agreement with the IRB and ED personnel.
The amount of poison ingested was not accounted for as a potential risk factor due to the diverse nature and forms of the substances ingested (powder, cream, fluid, pills, capsules, etc). Amounts of these diverse substances could not be quantified using a standard measuring unit and it was reported by parents in rough estimates. The fact that home remedies were self-reported practices by parents who were under stress and fear at the time of incident is another concern. Authors suspected a recall and/or a cognitive bias from parents who were reluctant to admit the details of such practice during the initial ED visit. This was overcome by phone calling the parent at a later time to revalidate the reported practice.
CONCLUSIONS
Home remedies provided to poisoned children before their visit to this center significantly delayed the av. length of stay, one of the key performance indicators for hospitals and reimbursing bodies. A significant association was found among poisoned children of older age and higher admission rates. The severity of clinical triage assessment was also a significantly associated factor with higher admission rates and extended av. LOS.
RECOMMENDATIONS
The av. LOS is a simple and important indicator for care management and effectiveness in child poisoning scenarios. This study measured the av. LOS as a parameter for such a DRG so that, in the future, it is benchmarked locally and/or internationally. Cases with delayed av. LOS beyond this study finding may trigger further investigations to identify and modify other associated factors. Care coordinators and other health practitioners in EDs are now able to predict and anticipate an in-hospital admission and LOS based on the child and poison incident characteristics highlighted in this study.
Parents are recommended to adhere to the local and international poison management guidelines. Community awareness campaigns aid in orienting them on the importance of notifying a nearby poison center upon any incident. A unified hotline poison control number in Saudi Arabia is essential and its placement at homes will definitely cut-off delays in seeking treatments. Environmental characteristics, such the storage of poison products and safety seals on poisons, were questioned during the phone calls. Almost 25% of chemical products were placed in unlocked cabinets, whereas 17% were placed in living rooms, bedrooms, and kitchen floors during the incident. This necessitates the importance of launching poison awareness campaigns to orient parents on safely storing and disposing potentially poisonous products. Due to the fact that such practice does exist in the community and testing it in randomized control trials is not scientifically and ethically applicable, poison centers need to inquire further on such data from parents who commit such practice. Therefore, it is advisable to incorporate it within the Saudi MOH and NDPIC reporting forms for drug over dosage or chemical poisoning, to further investigate the spread and outcomes of such practice.
Acknowledgments
The authors would like to thank the Research office and the IRB (Prof. Amin Kashmeery and Prof. Abdulhaleem Sawas) for their tremendous support. They owe special thanks to Prof Mostafa Abolfotouh and Dr. Essam Al Banyan for their advisory role, as well as Mr. Mohammed Al-Sahly for assisting the team through medical records. The efforts of the pediatric emergency department, medical and nursing, at King Abdulaziz Medical City are well appreciated.
Footnotes
Abbreviations: adj.OR = Adjusted odds ratio, adj.P = adjusted P value, BMI = body mass index, CI = confidence interval, ED = emergency department, JCI = Joint Commission International, KAIMRC = King Abdullah International Medical Research Center, KAMC = King Abdulaziz Medical City, LOS = length of stay, MNG-HA = Ministry of National Guard-Health Affairs, MOH = Ministry of Health, MRN = Medical record number, NDPIC = National Drug & Poison Information Center, SFDA = Saudi Food and Drug Authority.
Funding: this study was initiated and funded by King Abdullah International Medical Research Center, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
Authors’ contributions: MQA, MJ and MS conceptualized and designed the study. FA and MJ supervised the conduct of the study and data collection. MHA and LYA undertook and supervised the recruitment of patients and managed the data. MJ and MS were accounted for the quality control and provided statistical advice on study design and analyzed the data. All authors drafted the manuscript and contributed substantially to its revision as submitted and agree to be accountable for all aspects of the work.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Raeisi AR, Yarmohammadian MH, MohammadiBakhsh R, et al. The performance indicators based on Iranian balanced scorecard model in Al-Zahra hospital of Isfahan University of Medical Science. Health Inf Manage 2013; 10:601–610. [Google Scholar]
- 2.Rapoport J, Teres D, Zhao Y, et al. Length of stay data as a guide to hospital economic performance for ICU patients. Med Care 2003; 41:386–397. [DOI] [PubMed] [Google Scholar]
- 3.Borghans I, Heijink R, Kool T, et al. Benchmarking and reducing length of stay in Dutch hospitals. BMC Health Serv Res 2008; 8:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahimi H, Khammar-nia M, Kavosi Z, et al. Indicators of hospital performance evaluation: a systematic review. Int J Hosp Res 2014; 3:199–208. [Google Scholar]
- 5.Mathauer I, Wittenbecher F. Hospital payment systems based on diagnosis-related groups: experiences in low-and middle-income countries. Bull World Health Organization 2013; 91:746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alanazi MQ, Al-Jeraisy MI, Salam M. Comparative outcome analysis of home-initiated non-medical interventions among toddlers with orally ingested substances. Ital J Pediatr 2015; 41:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National capital poison center for the Washington, DC Metro Area. Poison Statistics 2014; Available at: http://www.poison.org/poison-statistics-wash-dc-metro-area Accessed on 16 Dec 2015. [Google Scholar]
- 8.Ragab A, Al-Mazroua M. Pattern of pediatric toxicity in Saudi Arabia-eastern province incidence, demographics and predisposing factors. Pediat Therapeut 2015; 5:2161–2665.doi:10.4172/2161-0665.1000220. [Google Scholar]
- 9.Azkunaga B, Mintegi S, Bizkarra I, et al. Toxicology surveillance system of the Spanish Society of Paediatric Emergencies: first-year analysis. Eur J Emerg Med 2011; 18:285–287. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health, Singapore. Management of poisoning: MOH clinical practice guidelines. 2011; pp. 36–61. ISBN 978-981-08-9904-2. [Google Scholar]
- 11.Franklin RL, Rodgers GB. Unintentional child poisonings treated in United States hospital emergency departments: national estimates of incident cases, population-based poisoning rates, and product involvement. Pediatrics 2008; 122:1244–1251. [DOI] [PubMed] [Google Scholar]
- 12.Annual Report 2013. Dublin: National Poisons Information Centre. Available at: http://www.poisons.ie/docs/NPIC_AnnualReport2013.pdf 2013; pp. 2–10. Accessed on 15 Dec 2015. [Google Scholar]
- 13.Al-Barraq A, Farahat F. Pattern and determinants of poisoning in a teaching hospital in Riyadh, Saudi Arabia. Saudi Pharm J 2011; 19:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dao L, Yé D, Fayama Z, et al. Les intoxications aiguës accidentelles de l’enfant: aspects épidémiologiques, étiologiques et évolutifs au CHU pédiatrique Charles-de-Gaulle de Ouagadougou (Burkina Faso). Cahiers d’études et de recherches francophones/Santé 2009; 19:55–59. [DOI] [PubMed] [Google Scholar]
- 15.Altyar A, Kordi L, Skrepnek G. Clinical and economic characteristics of emergency department visits due to acetaminophen toxicity in the USA. BMJ Open 2015; 5:e007368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoikka M, Liisanantti J, Dunder T. Acute poisoning in children under the age of six: a two-decade study of hospital admissions and trends. Acta Paediatrica 2013; 102:e329–e333. [DOI] [PubMed] [Google Scholar]
- 17.Konstantelos D, Koulouri A, Giannakopoulou P, et al. 725 The epidemiology of acute child poisonings in Kalamata, Greece: a 3 year study. Pediatr Res 2010; 68:368. [Google Scholar]
- 18.Lamireau T, Llanas B, Kennedy A, et al. Epidemiology of poisoning in children: a 7-year survey in a paediatric emergency care unit. Eur J Emerg Med 2002; 9:9–14. [DOI] [PubMed] [Google Scholar]
- 19.Kivistö JE, Arvola T, Parkkari J, et al. Paediatric poisonings treated in one Finnish main university hospital between 2002 and 2006. Acta Paediatrica 2008; 97:790–794. [DOI] [PubMed] [Google Scholar]
- 20.Mintegi S, Fernández A, Alustiza J, et al. Emergency visits for childhood poisoning: a 2-year prospective multicenter survey in Spain. Pediatr Emerg Care 2006; 22:334–338. [DOI] [PubMed] [Google Scholar]
- 21.Alanazi MQ, Al-Jeraisy MI, Salam M. Prevalence and predictors of antibiotic prescription errors in an emergency department, Central Saudi Arabia. Drug Healthc Patient Saf 2015; 7:103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lapus RM, Slattery AP, King WD. Effects on a Poison Center's (PC) triage and follow-up after implementing the no ipecac use policy. J Med Toxicol 2010; 6:122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dart RC, Erdman AR, Olson KR, et al. Acetaminophen poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol 2006; 44:1–18. [DOI] [PubMed] [Google Scholar]
- 24.El Mouzan M, Al Herbish A, Al Salloum A, et al. Comparison of the 2005 growth charts for Saudi children and adolescents to the 2000 CDC growth charts. Ann Saudi Med 2008; 28:334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Satar S, Seydaoglu G. Analysis of acute adult poisoning in a 6-year period and factors affecting the hospital stay. Adv Ther 2005; 22:137–147. [DOI] [PubMed] [Google Scholar]
- 26.Frakes MA, Evans T. An overview of Medicare reimbursement regulations for advanced practice nurses. Nurs Econ 2006; 24:59. [PubMed] [Google Scholar]
- 27.Salam MM. Are peripherally inserted central catheters better alternatives than peripheral venous catheters and central lines? AUB 2010. 21–22. [Google Scholar]
- 28.Barker KL, Reilly KA, Minns Lowe C, et al. Patient satisfaction with accelerated discharge following unilateral knee replacement. Int J Ther Rehab 2006; 13:247–253. [Google Scholar]
- 29.Gares D. The relationship of acute inpatient hospital length of stay and patient satisfaction: Medical University of South Carolina-College of Health Professions; 2011; pp. 4–6. [Google Scholar]
- 30.Quintana JM, González N, Bilbao A, et al. Predictors of patient satisfaction with hospital health care. BMC Health Serv Res 2006; 6:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chien C, Marriott J, Ashby K, et al. Unintentional ingestion of over the counter medications in children less than 5 years old. J Paediatr Child Health 2003; 39:264–269. [DOI] [PubMed] [Google Scholar]
- 32.Bakhaidar M, Jan S, Farahat F, et al. Pattern of drug overdose and chemical poisoning among patients attending an emergency department, western Saudi Arabia. J Community Health 2014; 40:57–61. [DOI] [PubMed] [Google Scholar]
- 33.Ressel GW. AAP releases policy statement on poison treatment in the home. Am Fam Physician 2004; 69:741. [PubMed] [Google Scholar]
- 34.Graedon J, Graedon T. The People's Guide to Deadly Drug Interactions: How to Protect Yourself From Life-Threatening Drug–Drug, Drug–Food, Drug–Vitamin Combinations. UK: Macmillan; 1997. [Google Scholar]
- 35.Hetal T, Bindesh P, Sneha T. A review on techniques for oral bioavailability enhancement of drugs. Int J Pharm Sci Rev Res 2010; 4:203–223. [Google Scholar]
- 36.Bailey DG. Fruit juice inhibition of uptake transport: a new type of food–drug interaction. Br J Clin Pharmacol 2010; 70:645–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bareuther C. Dangerous food-drug interactions. Aging Well, Vol.10 No.4. Available at: http://www.todaysgeriatricmedicine.com/archive/101308pe.shtml 2008; Accessed on 15 Dec 2015. [Google Scholar]
- 38.Grilo CM, Mitchell JE. The Treatment of Eating Disorders: A Clinical Handbook. New York City: Guilford Press; 2011. [Google Scholar]


