Abstract
Transition of young adults with sickle cell disease (SCD) from pediatric to adult medical care is an important priority, given medical advances that have transformed SCD into a lifelong chronic condition, rather than a disease of childhood. Successful transfer from pediatric to adult care has its foundation in collaboration among the young adult, the family, and the health care system to support building skills in positive disease management and independent living. Systemic issues in transition from pediatric to adult care for individuals with SCD include limited access to adult providers with the skills and/or interest in caring for people with SCD; poor communication and follow-up between pediatric and adult providers; and insurance coverage and reimbursement for care coordination. Family and patient issues in transition include lack of skill development for successful transition into adulthood; absence of financial independence; fear of the unknown; and increasing morbidity with age. The design and evaluation of successful transition programming in SCD requires clarity in conceptual frameworks and consistent measurement, both before and after transfer to adult care. Strategies used by three SCD transition programs and future directions for research and program development are presented.
Over the last three decades, sickle cell disease (SCD) has been characterized as a lifelong chronic condition, rather than as a disease of childhood [1,2]. The majority of children with SCD in developed countries now survive well into adulthood given the availability of prophylactic penicillin, vaccinations, and such therapies as hydroxyurea [3,4]. However, health care delivery systems that support the optimal transfer from pediatric to adult care for youth with SCD have not kept pace with the growing adult population. Although many young adults with SCD are able to navigate adult systems of care after the transfer from pediatric care, others experience significant difficulty with this transition [5,6].
Transition should be considered a process occurring over time and not a cross-sectional event [7]. For the purpose of research presented in this article, transition is conceptualized as a dynamic process [8] with a beginning, middle, and an end. The beginning phase refers to the decision to begin or prepare for the transition. The middle phase, “transition readiness,” refers to logistical and other efforts of preparation for and implementation of the transition. Transition readiness is defined as the specific decisions made and actions taken in building the capacity of the adolescent and those in his/her primary medical microsystems (parental caretakers/family and providers) to prepare for, begin, continue, and finish the process of transition [9,10]. Because an increasing number of adolescents with SCD are surviving into adulthood and ready for transfer from pediatric to adult care, transition has become a critical issue [9,10]. The final or end stage occurs when the adolescent or young adult not only transfers to an adult care setting, but is actively participating in adult care activities, such as working with providers to plan their own medical care, or deciding if the provider[s] he/she is referred to is someone he/she can work with or if an available alternative needs to be chosen. Given the chronicity of SCD, this transition encompasses both medical and life transition and is defined as the process involved in the movement of adolescents from a focus on pediatric life skill issues to adult life skill issues, including transfer from pediatric or child-centered care to adult health care services [11].
The challenges faced by youth with SCD, their families, and their health care systems during the transition into adulthood are not unique to the population [5] [6,12,13]. All youth must navigate rapid physical, social, and psychological changes in the journey to independence, and all youth require support in making good choices as they head toward adulthood. Many youth with SCD and other special health care needs require additional support from their families and medical staff as they adjust to the need to take on increased responsibility for management of their condition, and as they plan for a future that entails living with a chronic condition. Medical complications and concomitant functional disabilities can create social, emotional, and behavioral difficulties that impede the health care transition process [14]. However, most of the functional life of youth and young adults with SCD takes place at home, in school, and in the community, not in the hospital or clinic setting.
Transition research in SCD
Findings on barriers to successful SCD health care transition are consistent with the body of literature on overall health care transition [2,15]. Telfair et al. [10] conducted the first empirical study of SCD health care transition, investigating issues, concerns, and expectations of adolescents, young adults, and parents/guardians related to transfer to adult care. Youth and young adults aged 13–30 years and parents/guardians participated in a cross-sectional study. This study found that adolescents and young adults were primarily concerned with how they would pay for medical care and how they would be treated in adult settings. The primary concerns of parents were the youth's ability to take on responsibility for self-care and cope successfully in the adult health care system.
A multisite study of SCD transition included adolescents (mean age, 17 years) seen in sickle cell centers and community-based SCD programs [16]. Participants were assessed on responsibility for self-care, communication effectiveness, perceived future difficulties with SCD, and independence. The majority of participants voiced a fear of leaving their pediatric health care providers, expressing concern that adult care providers might not understand their needs and might not believe their complaints of pain. The youth also expressed concerns about having limited information about transition and about adult health care programs.
An international transition study comparing adolescents with SCD in the United Kingdom and in the United States found that older adolescents had more physical and psychological symptoms compared with younger adolescents but also demonstrated better self-management and responsibility for care [17]. Youth with fewer psychological symptoms experienced better SCD knowledge and greater confidence in their medical care. Recently, adolescents with SCD were assessed as low in readiness for transition [18].
Qualitative studies have yielded findings similar to the quantitative research on transition in SCD. In individual or group interviews with patients with SCD aged 13–21 and their parents and health care providers, concerns were expressed about leaving familiar settings, going to providers who may not be familiar with SCD, and establishing new family roles [19]. In another study [20], already transferred patients reported that they had received little preparation for transition and that transition was based on age rather than readiness or needs. They indicated that their follow-up care in the adult medical system had declined since the transfer. Knowledge, disease severity, and family relations were found to operate together to influence independence levels for youth with SCD [21].
Barriers to transition in SCD
The challenges that the health care system poses to successful transition includes a dearth of adult providers with the skills and/or interest in caring for people with SCD, especially in areas with low resources [22,23]. Communication and follow-up between pediatric and adult providers tends to be poor. Insurance coverage may be inadequate overall, and there may not be a seamless transition from what is covered in the pediatric versus what is covered in the adult years. Reimbursement for care coordination is particularly challenging for adult providers, but may be difficult for pediatric providers as well [24]. Finally, adults with chronic conditions may have limited access to the patient-centered medical home model compared with pediatric patients [25,26]. This may result in excessive reliance on receiving care in emergency departments and may be associated with less availability of ancillary support services.
For health care providers, physicians and other multidisciplinary providers may not be prepared for the increased complexity of medical complications as patients with SCD age [27]. In an early study of pain rates, the number of episodes per patient year was found to peak between the ages of 20 and 29 years for male patients with SCD-SS [28]. More recently, it was shown that adults with SCD experience pain on over 50% of days [29]. Some patients, particularly those with SCD-SC and SCD-Sß+ thalassemia, may experience their first medical problems in early adulthood, and then over time continue to encounter more severe problems. Providers may not appreciate the social, psychological, and cultural aspects of the illness and bias concerning issues of pain is significant [11,30]. Expectations of self-management skills may differ between pediatric and adult providers.
Clinicians, clinical researchers, and families have emphasized treatment issues at the expense of fostering independence, life skills, and optimal development. Further, affected individuals and their families have not played a significant role in the determination of the national agenda for SCD research. In present times, there are changes and uncertainties with the health care delivery system for all.
Developing a conceptual framework for transition
Transition is a multifaceted, active process that attends to the medical, psychosocial, and educational/vocational needs of adolescents as they move from the child focused to the adult focused health care system. Health transition facilitates transition in other areas, including work, community, and school. Transition proceeds at different rates for different individuals and families. The goals of transition programs are to provide continuity of care from childhood to adulthood and to adequately prepare youth with SCD to navigate the adult world. Individualized plans for health education and medical care must be determined. Program development and transition research should take place within a conceptual framework. Two potential models for the study of transition include the bio-ecological systems theory [31,32] and the transtheoretical model of stages of change [33].
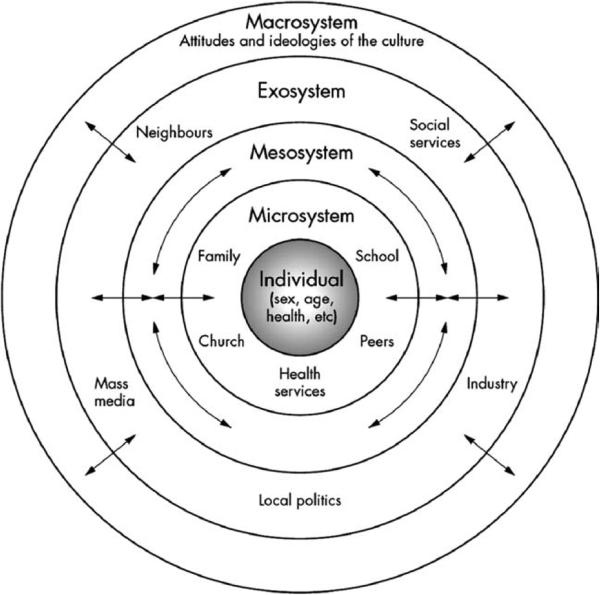
The bio-ecological systems theory emphasizes environmental factors as playing a major role in development [31,32]. The theory identifies five environmental systems (Fig. 1), including the microsystem (the immediate environment involving family, school, peer group, and neighborhood) and the individual's biology, here the diagnosis of SCD. The mesosystem refers to the connections between microsystems or contexts as in the relation of family experiences to school experiences and vocational experiences to interfacing with the health care system, for example. External environmental settings, which only indirectly affect development, are deemed the exosystem. The macrosystem describes the culture in which individuals live. Cultural contexts include how developed one's country is, socioeconomic status, and ethnicity. Finally, the chronosystem describes the patterning of environmental events and transitions over the life course, as well as sociohistorical circumstances. In viewing transition in SCD within an ecological perspective, it is important to consider relationships across and between medical care providers and facilities, as well as across and between educational, social, and employment entities. Medical care providers must consider the role of community-based professionals in the lives of people with SCD. They also may need to consider different paradigms in the involvement of family members in the care of the young person with SCD. Three groups need to be transitioned for the process to be successful: patients before they enter adult care; families and primary caregivers; and pediatric and adult health care providers.
Figure 1.
Biosocial ecological model of health.
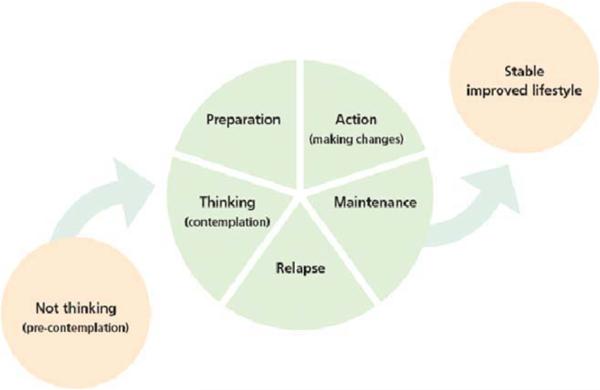
The transtheoretical stages of change model [33,34] assesses an individual's readiness to act on new behaviors that promote health. Stages of change include precontemplation, when individuals are not intending to take action in the foreseeable future; contemplation, when an individual is considering change; preparation, intention to take action in the immediate future; action, where specific lifestyle modifications are being made; and maintenance. The model describes processes that guide the individual through the stages of change and consists of such core constructs as decisional balance and self-efficacy (Fig. 2). These processes suggest strategies that can be applied to effect change, and that are most effective when matched to the individual's stage.
Figure 2.
Stages of change adapted from Prochaska and DiClemente. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Once a conceptual framework is identified, an evidence base for transition issues and effective practices can be developed, as consistent assessment tools and tracking system are applied. In the next section, we describe three model transition programs that were developed after a review of the literature, from an evidence base where possible and from existing promising practices.
Model Transition Programs
Reiss et al. [14] conducted interviews and focus groups with young adults with disabilities and special health care needs, family members, and pediatric- and adult-oriented health care providers. Participants told their stories so that transition attitudes and behaviors were understood in a narrative context. Results supported three phases of transition: future orientation, preparation, and time of transition. The importance of existing therapeutic relationships was emphasized. Individually based obstacles to transition included individual preferences; systems obstacles were rooted in rules and laws that govern the age of majority in access to health insurance; and cultural obstacles resided in the equation of work with insurance coverage and medical education. Results also supported the need for a transition process that starts early. Independence must be practiced and self-management behaviors and skills acquired before adolescence. A planned process needs to be in place for the actual transfer. Families can be encouraged to assume that transition is a normal developmental process, and they can work with the youth to create independence while acknowledging the interdependence that comes with a chronic condition.
The transition program that is under development, based in part on these findings, consists of a team of adult and pediatric physicians, adult and pediatric nurse practitioners, adult and pediatric social workers, an educational coordinator, and a clinical psychologist. Assessment includes self-efficacy; medical, educational, and vocational status; health benefits; and social and independent living skills. Challenges that come with transition are recognized as related to the termination of the relationship with the pediatric provider, suggesting that a more therapeutic termination should take place. As new relationships are established, there must be awareness of the significant emotions that surround transition, including a fear of the unknown. In keeping with the transtheoretical model of behavioral change, aspects of transition are measured, but changes in awareness of the need to change and/or to establish new behaviors are also measured.
Based on existing evidence and theories of change, this transition training program focuses on health literacy, disease self-management skills, interaction and communication with providers, and life planning. The program establishes timelines and behavioral expectations. Health care providers, youth with SCD, and family members are encouraged to think of transition as a process rather than an episode. The success of the program is measured both in terms of readiness for transition as well as outcomes post-transition. The program looks at the process of transition at 6-month intervals using existing measures of self-efficacy, attitudes toward SCD, quality of life, knowledge about SCD, and attitudes, beliefs, and behaviors in relation to transition. A SCD health behavior survey and a questionnaire based on the transtheoretical model of change are still under development.
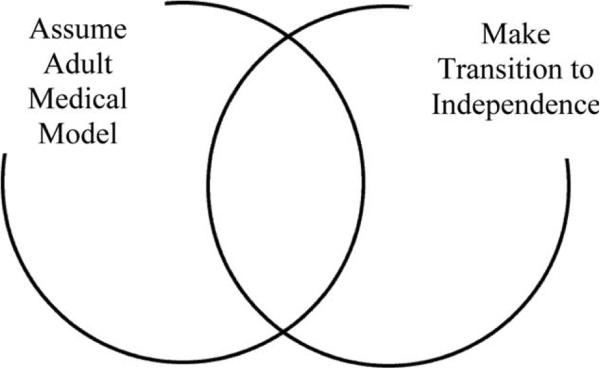
The second program focuses on tasks of transition (Fig. 3). The patient is helped to assume the adult medical model. Transition services are provided to families until the youth is 17, with a focus on preparing the youth and family for the changes between adult and pediatric care. Patients are seen in a centralized facility to reduce travel and inconsistencies in care that might come with numerous health care providers. To assume the adult medical model, youth are assisted in assuming control of their medical care as well as responsibility for their physical, psychological, social, educational, and vocational well-being. There is a focus on using psychoeducation to provide the youth with tools to improve their knowledge, attitude, skills, and confidence in dealing with their own health. Neuropsychological, and career and vocational assessments inform the youth, family, and medical team about what expectations for the youth's future are realistic.
Figure 3.
Conceptual model of the tasks of transition. There are many overlapping tasks as youth assume the adult medical model and transition to independence in other areas.
Potential assessment tools for annual evaluations can be found in Table I. Areas covered include medical, educational/vocational, health benefits, social, independent living, feelings, sickle-cell stress, and self-efficacy. A health care skills checklist reviews the basics of the individual's understanding of their hemoglobin type; their usual hemoglobin level; and their ability to prevent and manage sickle cell-related complications. Patients’ ability to track medical appointments and medications and their ability to communicate with their health care providers is assessed. Knowledge topics include understanding of inheritance of SCD and understanding of how drugs, alcohol, and tobacco use affect SCD. Patients indicate whether or not they are working on a medical transition plan for care when they leave the pediatric program.
TABLE I.
Potential Tools for Annual Assessment
| Health care skills checklist1 |
| Educational and vocation skills checklist1 |
| Health benefits checklist1 |
| Social support checklist1 |
| Independent living checklist1 |
| Feelings, stress, and strengths checklist2 |
| Sickle cell stress1 |
| Sickle cell disease self-efficacy2 [38] |
For information or to obtain a copy of the above referenced tools please contact:
Shirley Johnson, Virginia Commonwealth University, sjohnson42@vcu.edu
Joseph Telfair, University of North Carolina, j_telfai@email.uncg.edu
An educational and vocational skills checklist asks whether the patient has a vision for the future, whether they have a viable formal individualized education plan, and whether they participate in their individualized education program planning. Youth describe their plans with regard to graduation from high school or obtaining a GED, plans to attend college or to obtain post-high school training, and practice with regard to job interview skills. The transition program uses educational workshops where youth support one another while learning from peers and professionals. The workshop curriculum includes the history of SCD; review of inheritance/genetics; communication strategies (how to talk with one's health care providers); financial information; and academic and vocational choices. The delivery of education occurs quarterly and can be reinforced using computer modules made available during medical appointments. Individualized education builds on workshop content.
The third model program focused on the needs of transition age youth, families, and their pediatric and adult health care providers. The transition team was again multidisciplinary, including social workers, psychologists, vocational rehabilitation counselors, child life specialists, nurses, pediatric and adult hematologists, and their support staff. The health care system in which transition is taking place included four sites; thus, it focused initially on developing a strong structure within one of the sites before expanding. The program emphasized the need for institutional support and appropriate facilities, in addition to a committed group of providers and older persons affected with SCD who have successfully completed the transition process. A needs assessment was conducted to determine what the youth, families, and providers wanted and needed.
The transition plan consisted of quarterly programs for young adults aged 12 through 21 that was systematically rolled out for 17–21-year-olds, then 14–16-year-olds, and finally 12–13-year-olds and rotated through the four sites of the network. The Teen Scene program agenda (targeting the 17–21-year-olds) included a tour of the adult facility followed by a short presentation comparing and contrasting pediatric and adult clinical care “worlds” for SCD; a session on financial planning; separate sessions for males, females, and parent/caregivers; presentations from vocational rehabilitation; and a period of open discussion. The program ended with a discussion of the “Ten Commandments of Sickle Cell Disease,” which was a product of the aforementioned pediatric–adult round table events with significant input from successfully transitioned adults with SCD. These commandments focused on specific “precepts” or “life philosophies” that were thought to address some of the challenges specific to SCD transition success. As an example, the first commandment states “Accept Your Disease, Don't Try To Ignore It. Respect it, don't fear it. Learn how to master it; do not let it master you.”
A critical feature of the program was the implementation of monthly “adult–pediatric hematology roundtables” where barriers and perceptions from both sides were addressed and relationships were built between the adult and pediatric SCD providers. It became clear that both pediatrics and adult medicine providers had preconceived ideas about the others’ practices. Pediatric providers mistrusted that their patients will be well cared for once transitioned, and adult providers expect that the young adult will be poorly prepared to function in their setting. The roundtables provided for improved knowledge about each specialty and the building of trust.
Educational presentations make ample use of multimedia. Families are provided with transportation to the program, snacks, and meals for the program that lasts about 5 hours and a medical excuse to take back to teachers and/or employers, as needed. Youth officially “graduated” into the adult program in October of their 18th year. They received public recognition for achieving this milestone in the form of a certificate and a gift, and their medical transfer summary. Graduates of the pediatric program are recruited to mentor younger patients. At the same time, the program attempts to modify and adapt to the realities of life, coordinating dates with the school calendar to minimize school absences.
Summary
The transition to adulthood represents a critical turning point in the life course [35]. The ability of youth with SCD to participate fully in society and live productive lives as adults depends on their ability to navigate the transition period successfully. However, successful transition remains elusive for many young adults with SCD. In designing interventions to improve SCD self-management and transition from pediatric to adult care, and remembering transition is a process that is both developmentally and temporally dependent, it is important to identify who is at risk for poor outcomes so that interventions can be developmentally applied efficiently and cost-effectively.
It is now recognized that transition should begin at birth, with the encouragement of the family to envision a future for the child with special health care needs [36]. There must be a whole life perspective, where clinical care and management includes the ecology of the youth's and young adult's life. However, as programs begin to focus on formal transition services for youth with SCD, target ages tend to be between 14 and 21 years. Areas to emphasize in transition programming include preparing pediatric patients for the culture of adult medicine, promoting self-advocacy in obtaining support from schools and employers, and addressing issues of funding of health care services. Patients must be empowered, but it should be noted that sometimes the youth feels more ready than the family and the health care provider to transition. Transition preparation might include peer education or community-based settings that provide youth with practical strategies in navigating the realities that they will face in advocating for themselves. Portable medical histories must be provided.
Health care providers must also be taught how to tailor strategies to meet individual patient and family needs. The process of successful transition develops at different rates for individuals, families, and programs. A disease management program that promotes successful transition must address common knowledge and skills for the range of ages and abilities within the transition period, while using teaching strategies that are relevant for each developmental stage. The youth's context must be considered, i.e., neighborhoods, schools, and health care systems (Sickle Cell Center, primary care, and health maintenance organization). Successful transition depends not just on the youth's ability to use coping strategies to reduce stress in the short term [37], but on the ability to continue to learn and grow in the face of multiple stressors that accompany the interactions with the adult health care system and with the experience of SCD itself, as greater challenges in maintaining health emerge with age.
There is urgency to improve the responsiveness of the health care system to the needs of adults with special health care needs, including the extension of the patient-centered medical home model beyond the pediatric years [5]. Although these system changes are necessary, young people and their families cannot wait for these changes. They must be prepared for transition now.
Research Agenda for Transition in SCD
There is a need for evidence, efficacy, and a more collaborative and shared approach to transition training and evaluation. We need to understand the transition process itself but also understand prospectively what factors contribute to and impede the process of successful transition. There is very little evidence of what works and what does not work in the process of transition and what actually changes in the process of successful transition.
There is a need to apply consistent measurement across programs;
Interventions should be multifactorial, whereas a clear conceptual framework for each component of the program should be articulated;
Prospective studies of developmental, medical, and life skills of adolescents and young adults with SCD and other chronic conditions are needed to inform programs and policy.
Acknowledgments
The authors acknowledge the attendees at the workshop (Transition Educational Session, Co-chairs Joseph Telfair, Dr. Ph and Marsha Treadwell PhD, 4th Annual Sickle Cell Disease Research and Educational Symposium & Grant Writing Institute (GWI) and Annual National Sickle Cell Disease Scientific Meeting, 18 February 2010); multidisciplinary team members of the transition programs at the University of Florida; Virginia Commonwealth University; and Emory University.
Footnotes
Conflict of interest: Nothing to report.
References
- 1.Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 2.Scal P, Evans T, Blozis S, et al. Trends in transition from pediatric to adult health care services for young adults with chronic conditions. J Adolesc Health. 1999;24:259–264. doi: 10.1016/s1054-139x(98)00127-x. [DOI] [PubMed] [Google Scholar]
- 3.Morris CR, Singer ST, Walters MC. Clinical hemoglobinopathies: Iron, lungs and new blood. Curr Opin Hematol. 2006;13:407–418. doi: 10.1097/01.moh.0000245685.24462.4e. [DOI] [PubMed] [Google Scholar]
- 4.Steinberg MH, Barton F, Castro O, et al. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: Risks and benefits up to 9 years of treatment. JAMA. 2003;289:1645–1651. doi: 10.1001/jama.289.13.1645. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics AAoFPaACoP-ASoIM A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–1306. [PubMed] [Google Scholar]
- 6.Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics. 2005;115:1607–1612. doi: 10.1542/peds.2004-0458. [DOI] [PubMed] [Google Scholar]
- 7.White PH. Success on the road to adulthood. Issues and hurdles for adolescents with disabilities. Rheum Dis Clin North Am. 1997;23:697–707. doi: 10.1016/s0889-857x(05)70353-7. [DOI] [PubMed] [Google Scholar]
- 8.Transition From Child to Adult Health Care Services: A National Survey. University of Minnesota; Minneapolis, MN: 1995. [Google Scholar]
- 9.NIH . The Management of Sickle Cell Disease. NIH publication No. 95-2117. NIH; Bethesda, MD: 2002. [Google Scholar]
- 10.Telfair J, Myers J, Drezner S. Transfer as a component of the transition of adolescents with sickle cell disease to adult care: Adolescent, adult, and parent perspectives. J Adolesc Health. 1994;15:558–565. doi: 10.1016/1054-139x(94)90139-t. [DOI] [PubMed] [Google Scholar]
- 11.Haywood C, Jr, Beach MC, Lanzkron S, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022–1033. doi: 10.1016/s0027-9684(15)31069-5. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy A, Sawyer S. Transition from pediatric to adult services: Are we getting it right? Curr Opin Pediatr. 2008;20:403–409. doi: 10.1097/MOP.0b013e328305e128. [DOI] [PubMed] [Google Scholar]
- 13.McLaughlin SE, Diener-West M, Indurkhya A, et al. Improving transition from pediatric to adult cystic fibrosis care: Lessons from a national survey of current practices. Pediatrics. 2008;121:e1160–e1166. doi: 10.1542/peds.2007-2217. [DOI] [PubMed] [Google Scholar]
- 14.Reiss JG, Gibson RW, Walker LR. Health care transition: Youth, family, and provider perspectives. Pediatrics. 2005;115:112–120. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 15.Flume PA, Anderson DL, Hardy KK, et al. Transition programs in cystic fibrosis centers: Perceptions of pediatric and adult program directors. Pediatr Pulmonol. 2001;31:443–450. doi: 10.1002/ppul.1073. [DOI] [PubMed] [Google Scholar]
- 16.Telfair J, Ehiri JE, Loosier PS, et al. Transition to adult care for adolescents with sickle cell disease: Results of a national survey. Int J Adolesc Med Health. 2004;16:47–64. doi: 10.1515/ijamh.2004.16.1.47. [DOI] [PubMed] [Google Scholar]
- 17.Anie KA, Telfair J. Multi-site study of transition in adolescents with sickle cell disease in the United Kingdom and the United States. Int J Adolesc Med Health. 2005;17:169–178. doi: 10.1515/ijamh.2005.17.2.169. [DOI] [PubMed] [Google Scholar]
- 18.McPherson M, Thaniel L, Minniti CP. Transition of patients with sickle cell disease from pediatric to adult care: Assessing patient readiness. Pediatr Blood Cancer. 2009;52:838–841. doi: 10.1002/pbc.21974. [DOI] [PubMed] [Google Scholar]
- 19.Hauser ES, Dorn L. Transitioning adolescents with sickle cell disease to adult-centered care. Pediatr Nurs. 1999;25:479–488. [PubMed] [Google Scholar]
- 20.Wojciechowski EA, Hurtig A, Dorn L. A natural history study of adolescents and young adults with sickle cell disease as they transfer to adult care: A need for case management services. J Pediatr Nurs. 2002;17:18–27. doi: 10.1053/jpdn.2002.30930. [DOI] [PubMed] [Google Scholar]
- 21.Newland JA. Factors influencing independence in adolescents with sickle cell disease. J Child Adolesc Psychiatr Nurs. 2008;21:177–185. doi: 10.1111/j.1744-6171.2008.00149.x. [DOI] [PubMed] [Google Scholar]
- 22.Telfair J, Haque A, Etienne M, et al. Rural/urban differences in access to and utilization of services among people in Alabama with sickle cell disease. Public Health Rep. 2003;118:27–36. doi: 10.1093/phr/118.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haque A, Telfair J. Socioeconomic distress and health status: The urban-rural dichotomy of services utilization for people with sickle cell disorder in North Carolina. J Rural Health. 2000;16:43–55. doi: 10.1111/j.1748-0361.2000.tb00435.x. [DOI] [PubMed] [Google Scholar]
- 24.Antonelli RC, Antonelli DM. Providing a medical home: The cost of care coordination services in a community-based, general pediatric practice. Pediatrics. 2004;113:1522–1528. [PubMed] [Google Scholar]
- 25.Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K. Closing the divide: how medical homes promote equity in health care: results from The Commonwealth Fund 2006 Health Care Quality Survey. The Commonwealth Fund. 2007 Jun; http://www.commonwealthfund.org/publications/doc_id=506814.
- 26.Kelly AM, Kratz B, Bielski M, et al. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110:1322–1327. [PubMed] [Google Scholar]
- 27.Prabhakar H, Haywood C, Jr, Molokie R. Sickle cell disease in the United States: Looking back and forward at 100 years of progress in management and survival. Am J Hematol. 2010;85:346–353. doi: 10.1002/ajh.21676. [DOI] [PubMed] [Google Scholar]
- 28.Platt OS, Thorington BD, Brambilla DJ, et al. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991;325:11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- 29.McClish DK, Levenson JL, Penberthy LT, et al. Gender differences in pain and healthcare utilization for adult sickle cell patients: The PiSCES Project. J Womens Health (Larchmt) 2006;15:146–154. doi: 10.1089/jwh.2006.15.146. [DOI] [PubMed] [Google Scholar]
- 30.Tanabe P, Artz N, Mark Courtney D, et al. Adult emergency department patients with sickle cell pain crisis: A learning collaborative model to improve analgesic management. Acad Emerg Med. 2010;17:399–407. doi: 10.1111/j.1553-2712.2010.00693.x. [DOI] [PubMed] [Google Scholar]
- 31.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University; Cambridge, MA: 1979. [Google Scholar]
- 32.Santrock JW. A Topical Approach to Life-Span Development. McGraw-Hill; New York, NY: 2007. [Google Scholar]
- 33.Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of Psychotherapy Integration. Oxford University Press; New York, NY: 2005. pp. 141–171. [Google Scholar]
- 34.Prochaska JO, Butterworth S, Redding CA, et al. Initial efficacy of MI, TTM tailoring and HRI's with multiple behaviors for employee health promotion. Prev Med. 2008;46:226–231. doi: 10.1016/j.ypmed.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Halfon N, Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–479. iii. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reiss J GR. Health Care Transition Initiative. Institute for Child Health Policy and Department of Pediatrics, University of Florida; Gainesville, FL: 2005. [Google Scholar]
- 37.Fournet DL, Wilson KL, Wallander JL. Growing or just getting along? Technical and adaptive competence in coping among adolescents. Child Dev. 1998;69:1129–1144. [PubMed] [Google Scholar]