Abstract
Current guidelines recommend management of benign gastric outlet obstruction (GOO) with serial dilations. Self-expanding metal stents are effective, but their use is complicated by high rates of migration. We present two cases from our institution where a uniquely designed, lumen-apposing metal stent (LAMS) was successfully used to alleviate benign GOO without stent migration.
Introduction
Benign gastric outlet obstruction (GOO) due to peptic ulcer disease or anastomotic stricture is a well described cause of morbidity. Patients often present with weight loss, oral intolerance, and abdominal pain. Dilation and metal stents have been used previously to alleviate benign GOO, but their use is complicated by restenosis and stent migration.1 A uniquely designed lumen-apposing metal stent (LAMS) may provide an effective and safe option for the endoscopic management of benign GOO.
Case Report
Case 1: An 86-year-old male with a history of stage 1 bladder cancer was admitted for progressive oral intolerance over 3 months, associated with a 13.5-kg weight loss and cramping abdominal pain. He denied nonsteroidal anti-inflammatory drug use. A computed tomography (CT) scan of the abdomen showed a markedly distended stomach, with a soft tissue focus at the gastric outlet resulting in near total obstruction of the pylorus (Figure 1).
Figure 1.

CT scan showing a markedly distended stomach and near total obstruction of the pylorus.
Esophagogastroduodenoscopy (EGD) demonstrated LA grade D esophagitis, diffuse gastritis with scattered clean-based ulcers, and an ulcerated, edematous pyloric channel. The channel could not be traversed with a standard gastroscope, and an Olympus XGIF-N200H ultrathin endoscope (diameter, 6 mm) was used (Olympus America, Center Valley, PA). The duodenal wall contained further ulcerations, but no mass was observed. Numerous biopsies were negative for Helicobacter pylori and showed reactive gastropathy. No dilation was performed initially, and the patient was started on twice-daily intravenous pantoprazole with the expectation that the edema would resolve and relieve the obstruction enough so that he could tolerate an oral diet. Repeat EGD performed 5 days later demonstrated persistent ulcerative disease and edema with the inability to traverse the pyloric channel.
The pylorus was pneumatically dilated to 8 mm with a through-the-scope (TTS) balloon (5.5 cm in length). Given persistent oral intolerance despite conservative therapy, treatment options were discussed with the patient, including traditional management with acid suppression, serial dilatations, and post-pyloric enteral nutrition versus stenting of the pyloric channel. The patient elected to proceed with stenting. The dumbbell-shaped LAMS was endoscopically placed across the pyloric channel (Figure 2). The self-expanding stent had a 15-mm mid-stent diameter (24 mm on each end) and a length of 10 mm. Post-pyloric placement of the distal end was confirmed fluoroscopically. The patient was continued on twice-daily pantoprazole and was discharged tolerating a full liquid diet.
Figure 2.
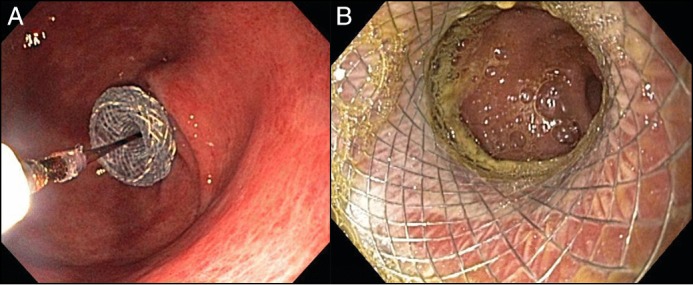
(A) LAMS being deployed into the stenotic pyloric channel via a through-the-scope technique. (B) View through the patent LAMS at 3 weeks post stent placement, showing healing pyloric channel and non-migration.
The patient had mild recurrence of nausea 2.5 weeks following the stent placement. Abdominal X-ray and repeat EGD demonstrated appropriate placement of the stent in the pylorus with a patent lumen and resolution of severe ulcerative disease (Figure 2). He subsequently reported resolution of nausea 2 days later and continued to tolerate oral intake until his abrupt passing 4 weeks later due to reasons unlikely related to his GOO or stent placement. No autopsy or additional imaging was performed post-mortem.
Case 2: A 60-year-old female with a history of peptic ulcer disease with a remote antrectomy with Billroth II re-configuration for perforated peptic ulcer disease was admitted for failure to thrive, abdominal pain, and postprandial nausea. She reported tobacco and ibuprofen use. Her body mass index was 11.3 kg/m2. CT scan showed a markedly distended stomach with a narrow gastrojejunal anastomosis causing GOO (Figure 3). EGD revealed LA grade D esophagitis, erythematous gastric mucosa with an ulcer in the body, which was clipped due to bleeding on contact, and a severely stenotic gastrojejunal anastomosis (Figure 4). Intubation of the anastomosis was not attempted given its narrow diameter and her altered anatomy. Biopsies showed chronic and active gastritis and were negative for H. pylori and malignancy. She was started on twice daily intravenous pantoprazole. Given the severe narrowing, persistent ulcerative disease, and her poor nutritional state, the patient decided to proceed with dilation and stenting of the stricture. Endoscopy was repeated, and the anastomotic stricture was dilated to 6 mm with a balloon under fluoroscopic guidance. The LAMS was then placed across the anastomosis. Post-stent balloon dilation was performed with a 12-mm balloon. Immediate passage of an ultrathin endoscope across the anastomosis showed a normal-appearing jejunum.
Figure 3.
CT scan showing a distended stomach, severely narrowed anastomosis (arrow), and a small amount of fluid entering the decompressed jejunum.
Figure 4.
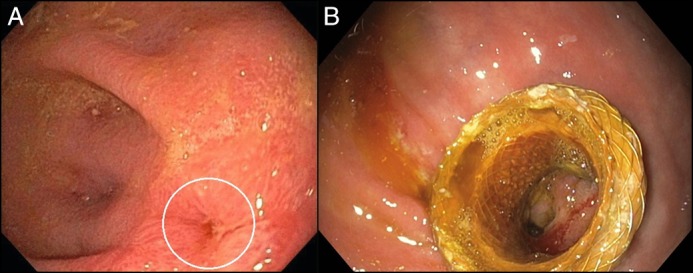
(A) Initial EGD demonstrating the severely stenotic gastrojejunal anastomosis (circle). (B) Follow-up EGD at 3 months showing that the LAMS remained in place and fully patent.
The patient was able to immediately tolerate a full liquid diet, and her nausea and discomfort subsided. She was discharged on twice-daily esomeprazole. Follow-up endoscopy performed 1 week after stent placement demonstrated self-expansion to its maximal diameter (15 mm). At 3 months post placement, endoscopy showed appropriate stent location and patent lumen (Figure 4). The stent was removed without complication. The estimated diameter of the anastomosis was 18 mm with no further need for dilation. At time of this writing, 21 months from intervention, she has had no recurrence of symptoms of GOO, and her body mass index has improved to 18.5 kg/m2.
Discussion
GOO due to benign causes has been well described.2 The first endoscopic therapy for GOO was dilation.3 Dilation, however, can be complicated by recurrent stenosis in 22–84% of patients treated for malignant and benign causes of stricture.4,5 Endoscopically placed self-expanding metal stents (SEMS) proved to be more effective at relieving GOO.6 In a study of SEMS used in benign pyloric obstruction, 18 of 22 patients (81.8%) experienced early symptom improvement, but at 6–8-week follow-up intervals, 15 of the 22 patients (68.1%) had stent migration.7 A study of partially covered SEMS used in benign pyloric obstruction demonstrated early symptomatic improvement (10 of 10 patients, 100%) and a lower migration rate (2 of 10 patients, 20%).2 However, stent adherence to adjacent mucosa occurred in 1 of 10 patients in the partially covered stent study versus 1 out of 22 patients in the fully covered stents.2,7
The LAMS used in our cases is a fully covered, self-expanding metal stent approved by the U.S. Food and Drug Administration for use in the drainage of pancreatic pseudocysts. Its novel design, which is dumbbell-shaped, was fashioned to prevent leakage and migration and likely reduces the risk of migration in the setting of GOO due to its wide (24mm) anchoring flanges. The first published case report demonstrated the successful use of this LAMS in a patient with a gastrojejunal anastomotic stricture refractory to repeat dilation.8 A recent retrospective study, which included 19 patients who underwent placement of LAMS for gastrojejunal or pyloric stenosis for benign GOO, showed clinical success in 12 of these patients (63%). Stent migration occurred in 2 of the stents placed for GOO (12%). Adverse events included pain requiring stent removal (12%), proximal stricture (6%), and bleeding (6%).9 Another case series using the LAMS in the same fashion for benign GOO was successful in 3 patients without any reported migration or adverse events at 3 months.10
While the use of this novel, fully covered, lumen-apposing, metal stent in benign GOO is not currently standard of care, the growing pool of data suggests that LAMS may provide a new option for the effective endoscopic management of benign GOO. Further investigation with a multicenter prospective case-control study or a randomized controlled trial comparing LAMS to repeat dilation or other SEMS is needed to determine the most clinically effective and cost-conscious approach to manage benign GOO.
Disclosures
Author contributions: R. Pinson wrote the manuscript and is the article guarantor. I. Pathirana, J. Magulick, J. Domanski, E. Okoh, and C. Womeldorph reviewed the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Disclaimer: The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Air Force, the Department of the Army, or the Department of Defense or the U.S. Government.
References
- 1.Fukami N, Anderson MA, Khan K, et al. . The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011; 74(1):13–21. [DOI] [PubMed] [Google Scholar]
- 2.Heo J, Min Kyu J. Safety and efficacy of a partially covered self-expandable metal stent in benign pyloric obstruction. World J Gastroenterol. 2016; 20(44):16721–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin SB, Cattau EL, Glass RL. . Balloon dilation of the pylorus: Therapy for gastric outlet obstruction. Gastrointest Endosc. 1982; 28(4):253–4. [DOI] [PubMed] [Google Scholar]
- 4.Solt J, Bajor J, Szabó M, Horváth OP. Long-term results of balloon catheter dilation for benign gastric outlet stenosis. Endoscopy. 2003; 35(6):490–5. [DOI] [PubMed] [Google Scholar]
- 5.Kuwada SK, Glenn LA. Long-term outcome of endoscopic dilation of nonmalignant pyloric stenosis. Gastrointest Endosc. 1995; 41(1):15–7. [DOI] [PubMed] [Google Scholar]
- 6.Binkert CA, Jost R, Steiner A, Zollikofer CL. Benign and malignant stenoses of the stomach and duodenum: Treatment with self-expanding metallic endoprostheses. Radiology. 1996; 199(2):335–8. [DOI] [PubMed] [Google Scholar]
- 7.Choi WJ, Park JJ, Park J, et al. . Effects of the temporary placement of a self-expandable metallic stent in benign pyloric stenosis. Gut Liver. 2013; 7(4):417–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uchima H, Abu-Suboh M, Mata A, Cruz M, Espinos J. Lumen-apposing metal stent for the treatment of refractory gastrojejunal anastomotic stricture after laparoscopic gastric bypass. Gastrointest Endosc. 2016; 83(1):251. [DOI] [PubMed] [Google Scholar]
- 9.Irani S, Jalaj S, Ross A, Larsen M, Grimm IS, Baron TH. Use of a lumen-apposing metal stent to treat GI strictures. Gastrointest Endosc. 2016; 12 Sept. 2016 [e-pub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 10.Majumder S, Buttar N, Gostout C, et al. . Lumen-apposing covered self-expanding metal stent for management of benign gastrointestinal strictures. Endosc Int Open. 2015; 4(1):E96–E101. [DOI] [PMC free article] [PubMed] [Google Scholar]



