Abstract
Objectives
We examined prevalence of major medical conditions and extent of disease burden among patients with and without substance use disorders (SUDs) in an integrated healthcare system serving 3.8 million members.
Methods
Medical conditions and SUDs were extracted from electronic health records in 2010. Patients with SUDs (n = 45,461; alcohol, amphetamine, barbiturate, cocaine, hallucinogen, and opioid) and demographically matched patients without SUDs (n = 45,461) were compared on the prevalence of nineteen major medical conditions. Disease burden was measured as a function of 10-year mortality risk using the Charlson Comorbidity Index. P-values were adjusted using Hochberg's correction for multiple-inference testing within each medical condition category.
Results
The most frequently diagnosed SUDs in 2010 were alcohol (57.6%), cannabis (14.9%), and opioid (12.9%). Patients with these SUDs had higher prevalence of major medical conditions than non-SUD patients (alcohol use disorders—85.3% vs. 55.3%; cannabis use disorders—41.9% vs. 23.0%; and opioid use disorders—44.9% vs. 26.1%; all p < .001). Patients with these SUDs also had higher disease burden than non-SUD patients; patients with opioid use disorders (M = 0.48; SE = 1.46) had particularly high disease burden (M = 0.23; SE = 0.09), (p < .001).
Conclusions
Common SUDs, particularly opioid use disorders, are associated with substantial disease burden for privately insured individuals without significant impediments to care. This signals the need to explore the full impact SUDs have on the course and outcome of prevalent conditions and initiate enhanced service engagement strategies to improve disease burden.
Keywords: Substance Use Disorder, Medical Comorbidity, Disease Burden, Behavioral Healthcare, Integrated Healthcare
The prevalence rates of alcohol, cannabis, and opioid use disorders are substantial in the United States (Substance Abuse and Mental Health Services Administration [SAMHSA], 2015). Studies of these substance use disorders (SUDs) report high rates of polysubstance use disorders (Degenhardt and Hall, 2012; Whiteford et al., 2013; Schuckit, 2009). Polysubstance use disorders are associated with a number of major medical conditions (Weisner et al., 2001; Mertens et al., 2003), and they place individuals with alcohol, cannabis, and opioid use disorders who have these conditions at an elevated risk for poor health outcomes, including high morbidity and early mortality (Schuckit, 2009; Hall and Degenhardt, 2009; Volkow et al., 2014). These studies signal a need to identify the medical conditions that raise the risk of poor health outcomes across these SUDs, so that strategies can be developed to reduce the burden of disease.
Studies have reported important differences regarding the medical conditions that are associated with alcohol, cannabis, and opioid use disorders, which has contributed to variability in the risk of poor health outcomes. First, alcohol use disorders are associated with high rates of cardiovascular disease, cancers, injuries, stroke, and cirrhosis, each of which increases the risk of poor health outcomes, including alcohol-related early mortality (Schuckit, 2009). Alcohol-related early mortality contributes to 2-4% of all adult deaths (Schuckit, 2009), and has been shown to raise the early death rate up to four times (Mann et al., 2005; Nordstrom, 2004). Second, opioid use disorders are associated with high rates of arthritis, chronic pain, headaches, hepatitis C, musculoskeletal disorders, and opioid-related overdose (Edlund et al., 2007; White et al., 2009; Rice et al., 2012). These medical conditions can each increase the risk of poor health outcomes in those with opioid use disorders, yet the elevated risk of early mortality is largely attributable to opioid-related overdose deaths (Volkow et al., 2014), increasing nearly fourfold from 1999 to 2013, and claiming about 44 lives per day by 2013 (Centers for Disease Control, 2015). Finally, cannabis use disorders are associated with high rates of respiratory deficits (Tetault et al., 2007), cardiovascular disease (Hall and Degenhardt, 2009), and risk of lung cancers (Aldington et al., 2008; Berthiler et al., 2008). These medical conditions can each increase the risk of poor health outcomes in individuals with cannabis use disorders; however, current evidence is insufficient to support such medical conditions independently elevate the risk of early mortality (Degenhardt et al., 2013). While these studies highlight several medical conditions that can raise the risk of poor health outcomes for individuals with alcohol, cannabis, and opioid use disorders, whether these findings persist in integrated healthcare, where such patients have broad access to specialty SUD treatment and medical care is largely unknown.
To date, research on the extent of medical conditions and disease burden in individuals with alcohol, cannabis, and opioid use disorders has largely focused on single SUDs (Schukit, 2009; Hall and Degenhardt, 2009; Whiteford et al., 2013; Rehm et al., 2009), narrowly defined patient samples (e.g., age/gender distinguished; psychiatric patients) (Kronik et al., 2009; Clark et al., 2009;), or has used data aggregated at the population-level (Rehm et al., 2009; Degenhardt and Hall, 2012; Degenhardt et al., 2013) or selected from publicly insured patient samples (e.g., Medicaid or Medicare) (Boyd et al., 2010; Sorace et al., 2011). There is little individual-level data on the extent of medical conditions and disease burden for those with alcohol, cannabis, and opioid use disorders, who have private insurance and access to integrated health services. This gap is notable, given that SUDs negatively affect individuals across the socioeconomic spectrum and because integrated healthcare systems are becoming critical settings for connecting patients with SUDs to requisite medical services as healthcare reform in the U.S. increases access to insurance coverage (Mark et al., 2014).
This study sought to address this gap in the literature by examining prevalent medical conditions and disease burden among a large sample of patients with and without SUDs in an integrated healthcare system. We aimed to: (1) describe the extent of polysubstance use disorders among patients with SUDs; (2) examine whether patients with ≥ one of the three most common SUDs (i.e., alcohol, cannabis, and opioid) in this healthcare system had higher prevalence of a number of medical conditions than patients without SUDs; and (3) investigate which patients with such SUDs had greater disease burden (measured as a function of 10-year mortality risk) than those without SUDs.
Methods
Setting
Kaiser Permanente Northern California (KPNC) is a nonprofit, integrated healthcare delivery system with 3.8 million members, who account for 44% of the commercially insured population in the region. About 88% of members are commercially insured, 10% have Medicare, and 2% have Medicaid coverage. KPNC operates over 54 outpatient clinics and is a staff model health system with more than 7,000 physicians. Most behavioral health services, including those provided at specialty clinics for substance use treatment, are provided internally rather than contracted to outside vendors. All individuals included in this study were selected from the KPNC membership. Institutional review board approval was obtained from the Kaiser Foundation Research Institute.
Participants
We used electronic health record (EHR) data that identified all adults aged 18 or older who had at least one of the five most prevalent behavioral health conditions on their diagnosis list (e.g., includes current and preexisting diagnoses) during an outpatient (e.g., includes specialty treatment), inpatient, or emergency department visit to a KPNC facility (11% of adult patients) in 2010. The top five behavioral health conditions included mental health and SUD diagnoses. Each patient with a behavioral health condition was matched to a KPNC patient without a behavioral health condition, on gender, age, and medical home facility. The latter accounted for differences in services, types of conditions, or unobservable differences by geographic region (Young et al., 2015). Due to the low representation of patients with public insurance (e.g., Medicaid or Medicare), such individuals were excluded.
In this secondary analysis, we identified individuals who had at least one SUD diagnosis (i.e., alcohol, cannabis, opioid, amphetamine, barbiturate, and hallucinogen) in 2010 and selected demographically matched controls without SUDs (see Table S1 for relevant ICD-9 codes). We then then identified patients with one of the most common SUDs, including alcohol, cannabis, and opioid disorders; these groups were not mutually exclusive. The final analytical sample consisted of 90,922 patients: 45,461 with SUDs, including 26,220 patients with an alcohol use disorder, 6,787 patients with a cannabis use disorder, 5,710 with an opioid use disorder, and 45,461 without SUDs.
Measures
Patient demographic characteristics
Patient demographic characteristics: age, gender, race/ethnicity and patient's medical home facility were extracted from the EHR. Race/ethnicity were collapsed into five categories: White, Black, Hispanic, Asian (Asian, Native American, or Hawaiian/Pacific Islander), and other/unknown, as in previous studies (Young et al., 2015).
Medical Comorbidities
All medical conditions were determined based on diagnoses noted in the EHR during patient visits made in 2010. As in our prior work with complex patient populations (Young et al., 2015) we examined prevalence of nineteen major medical conditions for patients with SUDs and without SUDs. Dichotomous measures were defined for each of the nineteen conditions studied (1 = present; 0 = none), and we also created an indicator (Any Medical Comorbidity: 1 = present; 0 = else) to identify those with ≥ 1 of the nineteen medical conditions examined. The medical conditions were: acid-peptic disorders (ICD-9: 530-534); arthritis (ICD-9: 710-719); asthma (ICD-9: 493); chronic kidney disease (ICD-9: 585.9, 403, or 585.1-585.5); chronic obstructive pulmonary disease (ICD-9: 490-492); chronic pain (ICD-9: 338.2); congestive heart failure (ICD-9: 402.01, 402.11, 402.91, 404.01, 404.11 or 428); coronary atherosclerosis (ICD-9: 440, 429.2, 410-414); diabetes mellitus (ICD-9: 250); end-stage renal disease (ICD-9: 585.6); headaches (ICD-9: 339, 784.0, or 346); hepatitis C (ICD-9: 0.07.70, 070.74, or 070.75); hypertension (ICD-9: 401-405); injuries, poisonings, and overdoses (ICD-9: 800-999); ischemic heart disease (ICD-9: 410-414); obesity (ICD-9: 278); osteoporosis (ICD-9: 733.3); pneumonia (ICD-9: 770, 480-486); and stroke (ICD-9: 345).
Disease Burden
Disease burden was operationalized as a function of 10-year mortality risk as computed by the Charlson Comorbidity Index (Charlson et al., 2008), a commonly used measure of disease burden for SUD patients (Young et al., 2015; Edlund et al., 2010). This measure yields a weighted score predicting 10-year mortality risk for patients who present for treatment with a range of diagnosis-based comorbid medical conditions (Charlson et al., 2008).
Statistical Analyses
The analytic approach focused on: prevalence of polysubstance use disorders among patients with SUDs; differences in demographic characteristics, medical conditions, and disease burden between patients with and without SUDs. Analyses were carried out in R version 2.14.2 (R Development Core Team, 2015), and began by employing frequencies to examine the extent of polysubstance use disorders within the SUD sample. Next, χ2 tests (categorical variables) or independent t-tests (continuous variables) were used to examine differences between patients with and without SUDs with regard to demographic characteristics, medical conditions, and disease burden. We examined such associations among patients with at least one SUD vs. non-SUD patients, and separately, between SUD patients who had an alcohol, cannabis, or opioid use diagnosis and matched non-SUD patients. SUD patients had an abuse/dependence diagnosis based on ICD-9 codes (Table S1). As we are examining multiple chronic medical condition categories, Hochberg's (Hochberg, 1988) correction was used to adjust for multiple inference testing within each of the chronic condition categories examined. Using this method, all p-values were multiplied by 20 (i.e., the total number of chronic conditions examined and the overall “any” medical condition measure) and only those resulting values which were <= .05 were considered significant. Statistical significance for all tests was defined at p < .05.
Results
Prevalence of substance use disorder diagnoses and polysubstance use disorders
Among the 45,461 patients with SUDs, alcohol (57.6%), cannabis (14.9%), and opioid (12.5%) use disorders were the three most common. As can be seen in Table 1, 68.5% of the SUD sample had at least two SUDs. Notably, while alcohol, opioid, and cannabis use disorders were highly comorbid with each other, patients with alcohol use disorders were more likely to have polysubstance use disorders (>1 SUD = 83.7%) than all other groups (Table 1).
Table 1. Polysubstance use disorders among patients with the three most common substance use disorders.
| Alcohol Use Disorders | Cannabis Use Disorders | Opioid Use Disorders | Any SUD | |
|---|---|---|---|---|
|
|
|
|
|
|
| Variable | n = 26,220 | n = 6,787 | n = 5,710 | n = 45,461 |
| SUD —% | ||||
| Alcohol | - | 32.3 | 21.6 | 57.6 |
| Cannabis | 8.3 | - | 12.5 | 14.9 |
| Opioid | 4.7 | 10.5 | - | 12.5 |
| Amphetamine | 3.4 | 9.3 | 6.2 | 5.8 |
| Cocaine | 3.2 | 6.2 | 3.9 | 3.5 |
| Barbiturate | 1.6 | 2.9 | 9.5 | 2.1 |
| Hallucinogen | 0.1 | 0.8 | 0.3 | 0.2 |
| Polysubstance use disorder —% | ||||
| >1 SUD | 83.7 | 55.1 | 63.3 | 68.5 |
| >2 SUD | 12.1 | 31.8 | 23.2 | 9.5 |
Note. SUD = substance use disorder. SUD diagnoses are not mutually exclusive therefore, between-group comparisons cannot be made.
Patient demographic characteristics
We then examined demographic characteristics in the overall sample (data not shown) as well as differences in such characteristics between patients with and without the three most common SUDs (Table 2). In the overall sample, 62.9% of patients were male and the average age was 44 (SD = 14.47). Fifty-four percent of the sample was White, 17.1% Hispanic, 11.3% Asian, 9.8% Black, and 7.0% unknown. Compared to their non-SUD counterparts, more patients with alcohol use disorders were White (59.8% vs. 48.7%) or Black (9.8% vs. 8.0%) and fewer were Asian (6.0% vs. 17.4%) (all p < .001). Alternatively, fewer patients with cannabis use disorders were Hispanic (16.3% vs. 19.8%) or Asian (4.9% vs. 18.0%) and more were White (54.3% vs. 43.7%) or Black (18.1% vs. 8.8%) than patients without SUDs (all p < .001). Fewer patients with opioid use disorders were Hispanic (13.0% vs. 18.2%) or Asian (2.6% vs. 15.8%) and more were White (72.6% vs. 50.7%) than patients without SUDs (all p < .001). There was no evidence of gender or age differences among those with and without alcohol, cannabis, or opioid use disorders as the sample was matched on these characteristics (Table 2).
Table 2. Characteristics of patients who had at least one of the three most common substance use disorders in 2010 and their demographically matched counterparts.
| Alcohol Use Disorders | Cannabis Use Disorders | Opioid Use Disorders | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| SUD | Non-SUD | SUD | Non-SUD | SUD | Non-SUD | ||||||||||
| n = 26,220 | n = 26,220 | n = 6,787 | n = 6,787 | n = 5,710 | n = 5,710 | ||||||||||
|
|
|||||||||||||||
| Variable | N | % | N | % | pa | N | % | N | % | pa | N | % | N | % | pa |
| Race/ Ethnicity | |||||||||||||||
| White | 15,686 | 59.8 | 12,795 | 48.7 | <.001 | 3,692 | 54.3 | 2,967 | 43.7 | <.001 | 4,147 | 72.6 | 2,895 | 50.7 | <.001 |
| Hispanic | 4,682 | 17.8 | 4,564 | 17.4 | .180 | 1,111 | 16.3 | 1,346 | 19.8 | <.001 | 745 | 13.0 | 1,044 | 18.2 | <.001 |
| Asian | 1,595 | 6.0 | 4,581 | 17.4 | <.001 | 339 | 4.9 | 1,224 | 18.0 | <.001 | 151 | 2.6 | 904 | 15.8 | <.001 |
| Black | 2,590 | 9.8 | 2,104 | 8.0 | <.001 | 1,235 | 18.1 | 604 | 8.8 | <.001 | 451 | 7.8 | 433 | 7.5 | .552 |
| Unknown | 1,667 | 6.3 | 2,176 | 8.2 | <.001 | 410 | 6.0 | 646 | 9.5 | <.001 | 216 | 3.7 | 434 | 7.6 | <.001 |
| Male | 17,879 | 68.1 | 17,882 | 68.1 | .985 | 4,257 | 62.7 | 4,258 | 62.7 | .100 | 2,909 | 50.9 | 2,908 | 50.9 | .100 |
| Age M, SD (years) | 45.8 | 15.2 | 46.1 | 15.3 | .218 | 34.1 | 13.6 | 34.4 | 13.7 | .219 | 41.7 | 14.3 | 42.1 | 14.3 | .216 |
Note. SUD = substance use disorder; Non-SUD = patients without substance use disorders; Non-SUD patients were matched one-to-one with SUD patients on gender, age, and medical home facility. SUD diagnoses are not mutually exclusive.
χ2 test or independent samples t-test (two-tailed).
Medical conditions and disease burden
Compared to patients without SUDs, patients with an alcohol use disorder (85.3% vs. 55.3%), cannabis use disorder (41.9% vs. 23.0%) and opioid use disorder (44.9% vs. 26.1%; all p < .001) were more likely to have one or more major medical conditions (Table 3). This pattern was consistent across all medical conditions examined (all p < .001), with the exception that there was no evidence of a difference for those with and without cannabis use disorders with regard to osteoporosis diagnoses (0.0% vs. 0.1%; p = .700). Among those with any SUD, the five most common medical conditions were arthritis (10.1%), acid-peptic disorders (15.5%), chronic pain (15.5%), hypertension (33.0%), and injuries, poisonings and overdoses (34.9%); all were significantly more prevalent among those with a SUD compared to those without a SUD (all p < .001). Patients with opioid use disorders had the greatest difference in prevalence of acid-peptic disorders (15.5% vs. 8.0%), chronic pain (15.5% vs. 2.7%), and injuries, poisonings and overdoses (36.6% vs. 21.8%; all p < .001) compared with non-SUD patients.
Table 3. Medical conditions among patients with any SUD, and patients who had at least one of the three most common SUDs in 2010 and their demographically matched counterparts without an SUD.
| Alcohol Use Disorders | Cannabis Use Disorders | Opioid Use Disorders | Any SUD | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| SUD | Non-SUD | SUD | Non-SUD | SUD | Non-SUD | SUD | Non-SUD | |
| Variable | n = 26,220 | n = 26,220 | n = 6,787 | n = 6,787 | n = 5,710 | n = 5,710 | n = 45,461 | n = 45,461 |
| Condition —% | ||||||||
| Any Medical Condition | 85.3 | 55.3*** | 41.9 | 23.0*** | 44.9 | 26.1*** | 42.9 | 27.0*** |
| Acid-peptic disorders | 15.0 | 8.4*** | 11.9 | 5.2*** | 19.5 | 7.2*** | 15.5 | 8.0*** |
| Arthritis | 19.0 | 15.1*** | 7.8 | 5.3*** | 14.0 | 6.8*** | 10.1 | 7.2*** |
| Asthma | 10.2 | 6.7*** | 14.6 | 0.7*** | 15.9 | 7.0*** | 12.1 | 7.1*** |
| Chronic Kidney Disease | 1.8 | 1.2*** | 1.0 | 0.4*** | 1.8 | 0.7*** | 2.0 | 1.1*** |
| COPD | 8.2 | 2.9*** | 5.4 | 1.8*** | 10.1 | 2.3*** | 8.4 | 2.7*** |
| Chronic Pain | 8.8 | 2.8*** | 11.1 | 2.0*** | 48.4 | 2.7*** | 15.5 | 2.7*** |
| Congestive Heart Failure | 3.0 | 0.8*** | 0.8 | 0.1*** | 1.6 | 0.2*** | 1.6 | 0.3*** |
| Coronary Atherosclerosis | 2.7 | 1.6*** | 1.6 | 0.5*** | 2.4 | 0.8*** | 2.8 | 1.4*** |
| Diabetes Mellitus | 10.7 | 9.4*** | 3.3 | 2.1*** | 5.0 | 3.6*** | 5.4 | 4.3*** |
| End Stage Renal Disease | 0.2 | 0.1** | 0.2 | 0.0*** | 0.1 | 0.0** | 0.1 | 0.0*** |
| Headaches | 3.4 | 2.2*** | 5.1 | 2.3*** | 9.7 | 2.8*** | 5.0 | 2.3*** |
| Hepatitis C | 3.4 | 0.6*** | 2.6 | 0.3*** | 8.0 | 0.4*** | 4.3 | 0.5*** |
| Hypertension | 36.7 | 23.0*** | 17.8 | 10.5*** | 29.6 | 17.6*** | 33.0 | 21.3*** |
| Injury, poisoning/ overdose | 35.5 | 21.1*** | 34.6 | 22.3*** | 36.6 | 21.8*** | 34.9 | 21.3*** |
| Ischemic heart disease | 5.1 | 3.2*** | 3.0 | 1.1*** | 4.6 | 1.6*** | 5.3 | 2.8*** |
| Pneumonia | 3.3 | 1.3*** | 2.5 | 0.8*** | 5.3 | 1.0*** | 3.6 | 1.1*** |
| Obesity | 6.0 | 4.1*** | 6.6 | 3.7*** | 8.0 | 4.6*** | 6.9 | 4.2*** |
| Osteoporosis | 0.5 | 0.4*** | 0.1 | 0.0 | 0.7 | 0.3*** | 0.6 | 0.3*** |
| Stroke | 2.0 | 0.4*** | 0.5 | 0.1*** | 0.6 | 0.1*** | 1.0 | 0.1*** |
Note. SUD = Substance use disorder. Non-SUD = patients without SUDs; Non-SUD patients were matched one-to-one with SUD patients on gender, age, and medical home facility. COPD = chronic obstructive pulmonary disease. Substance use disorder diagnoses are not mutually exclusive. P-values were adjusted using Hochberg's (1988) correction for multiple inference testing within each medical condition category.
p< .05;
p<.01;
p < .001
We then explored the number of co-occurring medical comorbidities between SUD patients and their non-SUD counterparts. As shown in Table 4, patients with a SUD had a higher number of medical comorbidities than non-SUD patients across all groups examined. Those with opioid use disorders had the highest prevalence of multiple medical conditions.
Table 4. Extent of multiple medical comorbidities among patients with any SUD, and patients with at least one of the three most common SUDs in 2010 and their demographically matched controls without an SUD.
| Alcohol Use Disorders | Cannabis Use Disorders | Opioid Use Disorders | Any SUD | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| SUD | Non-SUD | SUD | Non-SUD | SUD | Non-SUD | SUD | Non-SUD | |
| Variable | n = 26,220 | n = 26,220 | n = 6,787 | n = 6,787 | n = 5,710 | n = 5,710 | n = 45,461 | n = 45,461 |
| Medical comorbidities —% | ||||||||
| >1 medical conditions | 45.9 | 22.7*** | 37.6 | 14.9*** | 63.4 | 20.7*** | 45.9 | 22.7*** |
| >2 medical conditions | 22.0 | 8.1*** | 15.6 | 4.4*** | 39.3 | 7.0*** | 22.0 | 8.1*** |
| >3 medical conditions | 9.3 | 2.6*** | 5.4 | 1.0*** | 18.9 | 1.9*** | 9.3 | 2.6*** |
| >4 medical conditions | 3.6 | 0.8*** | 1.9 | 0.2*** | 7.2 | 0.7*** | 3.6 | 0.8*** |
| >5 medical conditions | 1.1 | 0.2*** | 0.6 | 0.0*** | 2.2 | 0.3*** | 1.1 | 0.2*** |
Note. SUD = Substance use disorder. Non-SUD = patients without substance use disorders; Non-SUD patients were matched one-to-one with SUD patients on gender, age, and medical home facility. Substance use disorder diagnoses are not mutually exclusive. P-values were adjusted using Hochberg's (1988) correction for multiple inference testing within each multiple medical comorbidity category.
p < .001
Differences between patients with and without SUDs regarding the burden of disease is shown in Figure 1. Across all groups, patients with a SUD had significantly higher disease burden compared with non-SUD patients (Figure 1); patients with (M = 0.48; SE = 1.46) vs. without (M = 0.23; SE = 0.09) opioid use disorders had particularly high burden of disease (p < .001).
Figure 1.
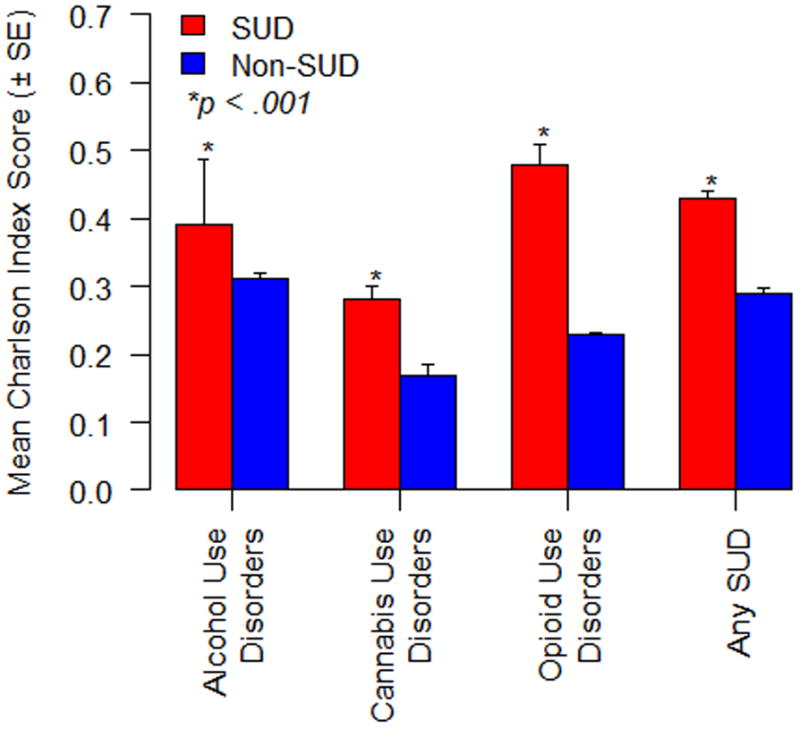
Disease burden measured as a function of 10-year mortality risk for patients with any SUD, and patients with at least one of the three most common SUDs in 2010 and their demographically matched counterparts without SUDs.
Discussion
This study of medical conditions and disease burden was the first to our knowledge to examine differences between patients with and without SUDs in a large integrated health system that mostly serves patients with employment-based health insurance. Results revealed that the overall prevalence of SUD diagnoses in this integrated healthcare system were largely consistent with the U.S. general population (SAMHSA, 2015); alcohol use disorder was diagnosed the most frequently, followed by cannabis use disorder, and opioid use disorder. As in prior studies, we found substantial prevalence of polysubstance use disorders among patients with SUDs (Edlund et al., 2007; Hall and Degenhardt, 2009; Schuckit, 2009; Brady et al., in press), and patients with alcohol, cannabis, and opioid use disorders were significantly more likely to have one or more medical conditions than their non-SUD counterparts (Weisner et al., 2001; Mertens et al., 2003). We also found higher disease burden estimates for SUD patients compared to patients without SUDs; those with opioid use disorders had particularly high disease burden. Thus, similar to investigations conducted with other populations and in other types of healthcare systems (Kronik et al., 2009; Clark et al., 2009; Boyd et al., 2010; Sorace et al., 2011), our results show that medical comorbidities are not only common among patients with prevalent SUDs, but are associated with substantial disease burden even for those with access to private insurance and integrated medical and SUD treatment services. Given that integrated healthcare systems are becoming increasingly more common in the post-Affordable Care Act environment (Barry and Huskamp, 2011), our results highlight the important role of such health systems in developing strategies to improve health outcomes for patients with SUDs.
Findings have several implications for future research and patient care. Research has previously shown that patients with SUDs suffer disproportionately from medical conditions associated with or exacerbated by substance use (Mertens et al., 2003; Weisner et al., 2001; Ray et al., 2000). Similar to this, we found a number of these medical conditions, including injuries, overdoses, hypertension, ischemic heart disease, acid-peptic disorders, pneumonia, and chronic obstructive pulmonary disease, were strikingly more common in patients with SUDs than those without SUDs. However, for patients with SUDs, many of the medical conditions worsened by substance use improve as patients' substance use outcomes improve (Weisner et al., 2001). Prior studies have also found that patients with SUDs and comorbid medical conditions have better alcohol and drug use outcomes when SUD treatment is integrated with primary care (Weisner et al., 2001; Friedmann et al., 2003). Primary care settings also serve as ideal venues for providers to screen for and treat medical conditions, identify risk or relapse of SUD, as well as offer brief treatment or refer patients to SUD treatment when needed (Institute of Medicine, 2006). This evidence suggests that enhancing primary care-based services for this population may help patients with SUDs and medical comorbidities worsened by substance use acquire needed SUD treatment and improve health outcomes.
Enhancing healthcare service coordination with patients' providers may help reduce the high prevalence of polysubstance use disorders and medical conditions, as well as offset the high burden of disease in patients with SUDs. Collaborative care approaches to delivering integrated healthcare services include models in which multidisciplinary teams are tasked with screening, tracking, and treating the patient's SUD and comorbid medical conditions in primary care and other medical service settings (Dickinson and Miller, 2010; Future of Family Medicine Project Leadership Committee, 2004). Such comprehensive approaches to service delivery may not only help facilitate the early detection of a number of medical conditions for patients with SUDs but may also help reduce the risk of poor health outcomes, as well as mitigate the higher costs that are often associated with treating these conditions (Kronik et al., 2009; Clark et al., 2009; Barry and Huskamp, 2011; Parthasarthy et al., 2003). Considerable excess costs (e.g., medical and prescription) have been associated with opioid use disorders (Birnbaum et al., 2011). Since we found a number of complex and costly medical conditions, including injuries, overdoses, and hypertension (Ray et al., 2000), were most prominent in opioid use disorders, these patients, in particular, may benefit from the development and subsequent implementation of collaborative care approaches to delivering integrated services in primary care settings.
Current estimates indicate that as few as 10% of those who need specialized SUD treatment ever access care (SAMHSA, 2014). As a consequence, patients with SUDs are overrepresented in primary care and trauma center settings (Cherpitel and Yu, 2008). This current problem of SUD treatment underutilization is compounded by the high prevalence of fatal overdoses stemming from the opioid overdose “epidemic” (Volkow et al., 2014). Devoting more resources to delivering SUD-interventions in trauma centers and primary care settings (i.e., including brief behavioral interventions and pharmacological approaches such as naltrexone or buprenorphine that can be initiated outside of specialty SUD treatment settings, and Naloxone availability, as well as screening for opioid use disorder comorbidity) (Cherpitel and Yu, 2008; Brady et al., in press), may help reduce high prevalence of overdose poisonings and improve risk of poor health outcomes associated with early mortality in this population.
This study also has limitations. Our use of provider-assigned diagnoses restricted our sample to those patients who had a SUD assigned during a health care visit, though this did include current and preexisting diagnoses. The selection criteria employed in this study could have affected the representativeness of the sample. However, our results are largely consistent with other studies that have shown that alcohol, cannabis, and opioid use disorders are the most prevalent SUDs (SAMHSA, 2015). Thus, we do not believe that the selection methodology employed in this study has substantially limited the applicability of our results. Patients selected for this research were also insured members of an integrated health plan, and the results may not be generalizable to uninsured populations or other types of health plans. Some patients selected may have met their provider's criteria for a SUD without receiving one of these diagnoses during provider encounters, which could also have unknowingly biased our results. Further, meaningful prevalence comparisons could not be computed between SUD and non-SUD patients for liver cirrhosis, cancers, Hepatitis B, or HIV due to the small number of patients with these conditions; these conditions are known to be associated with elevated risk of poor outcomes and disease burden in patients with SUDs (Rehm et al., 2009; Degenhardt and Hall, 2012; Schukit, 2009; Hall and Degenhardt, 2009). It will be important for future studies with the SUD population to incorporate these conditions into the medical disease burden measure.
While more epidemiological research in this area is needed as enrollment in healthcare systems continue to grow with the Affordable Care Act, we found that medical comorbidities were not only common among patients with SUDs, but also contributed substantially to disease burden even among individuals who have access to private insurance and integrated medical services. Our findings highlight the need for future studies to further examine the full impact SUDs have on the course and outcome of prevalent conditions, as well as for healthcare system development efforts to initiate enhanced service engagement strategies to improve disease burden in this population.
Supplementary Material
Acknowledgments
This study was supported by the Sidney R. Garfield Memorial Fund. This Research was also Supported by NIDA Grant T32DA007250. The content is solely the responsibility of the authors and does not necessarily represent the views of NIDA or the NIH. None of the authors reported a conflict of interest with respect to this project.
References
- Aldington S, Harwood B, Cox B, Weatherall M, Beckert L, Hansell A. Cannabis use and risk of lung cancer: a case—control study. Eur Respir J. 2008;31:280–286. doi: 10.1183/09031936.00065707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Huskamp HA. Moving beyond parity—mental health and addiction care under the ACA. N Engl J Med. 2011;356(11):973–975. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthiller J, Straif K, Boniol M, et al. Cannabis smoking and risk of lung cancer in men: a pooled analysis of three studies in Maghreb. J Thorac Oncol. 2008;3:1398–13403. doi: 10.1097/JTO.0b013e31818ddcde. [DOI] [PubMed] [Google Scholar]
- Birnbaum H, White A, Schiller M, Waldman T, Cleveland J, Roland C. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- Boyd C, Leff B, Weiss C, Wolff J, Hamblin A, Martin L. Clarifying multi-morbidity patterns to improve targeting and delivery of clinical services for Medicaid populations. Center for Health Care Strategies. Inc.; Dec, 2010. [Google Scholar]
- Brady KT, McCauley J, Back SE. Prescription opioid misuse, abuse, and treatment in the United States: An Update. AJP in Advance. doi: 10.1176/appi.ajp.2015.15020262. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. Deaths from Drug Poisoning and Drug Poisoning Involving Opioid Analgesics—United States, 1999-2013—United States, 1999-2013. Atlanta, GA: Centers for Disease Control and Prevention; 2015. Morbidity and Mortality Weekly Report. [Google Scholar]
- Charlson M, Charlson R, Peterson J, Marinopoulos S, Briggs W, Hollenberg J. The Charlson Comorbidity Index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol. 2008;61:1234–1240. doi: 10.1016/j.jclinepi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Yu Y. Drug use and problem drinking associated with primary care and emergency room utilization in the US general population: Data from the 2005 national alcohol survey. Drug Alcohol Depend. 2008;97:226–230. doi: 10.1016/j.drugalcdep.2008.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Samnaliev M, McGovern M. Impact of substance use disorders on medical expenditures for Medicaid beneficiaries with behavioral health disorders. Psychiat Serv. 2009;60(1):35–42. doi: 10.1176/ps.2009.60.1.35. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379:55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Whiteford H, Ferrari H, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1564–1570. doi: 10.1016/S0140-6736(13)61530-5. [DOI] [PubMed] [Google Scholar]
- Dickinson W, Miller B. Comprehensiveness and continuity of care and the inseparability of mental and behavioral health from the patient-centered medical home. Fam Syst Health. 2010;28:348–355. doi: 10.1037/a0021866. [DOI] [PubMed] [Google Scholar]
- Edlund M, Martin B, Fan M, Devries A, Braden J, Sullivan M. Risks for Opioid Abuse and Dependence Among Recipients of Opioid Therapy: Results from the TROUP Study. Drug Alcohol Depend. 2010;112(1-2):90–98. doi: 10.1016/j.drugalcdep.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund M, Steffick D, Hudson T, Harris K, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129(3):355–362. doi: 10.1016/j.pain.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Zhang Z, Hendrickson J, Stein MD, Gerstein D. Effect of Primary Medical Care on Addiction and Medical Severity in Substance Abuse Treatment Programs. J Gen Int Med. 2003;18:1–8. doi: 10.1046/j.1525-1497.2003.10601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Future of Family Medicine Project Leadership Committee. The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004;2(Suppl. 1):S3–S32. doi: 10.1370/afm.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374:1383–1391. doi: 10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- Hocherg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–803. [Google Scholar]
- Institute of Medicine. Improving the Quality of Health Care for Mental and Substance Use Conditions: Quality Chasm Series. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- Kronik R, Bella M, Gilmer T. The faces of Medicaid III: refining the portrait of people with chronic conditions. Center for Health Care Strategies. Inc.; Oct, 2009. [Google Scholar]
- Mann K, Schafer D, Langle G, Ackermann K, Croissant B. The long-term course of alcoholism, 5, 10 and 16 years after treatment. Addiction. 2005;100:797–805. doi: 10.1111/j.1360-0443.2005.01065.x. 2005. [DOI] [PubMed] [Google Scholar]
- Mark T, Levit K, Yee T, Chow C. Spending on mental and substance use disorders projected to grow more slowly than all health spending through 2010. Health Affair. 2014;8:1407–1415. doi: 10.1377/hlthaff.2014.0163. [DOI] [PubMed] [Google Scholar]
- Mertens J, Lu Y, Parthasarathy S, Moore C, Weisner C. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- Nordstrom T. Per capita alcohol consumption and all-cause mortality in Canada, 1950-1998. Addiction. 2004;99:1274–1278. doi: 10.1111/j.1360-0443.2004.00849.x. [DOI] [PubMed] [Google Scholar]
- Parthasarthy S, Mertens J, Moore C, Weisner C. Utilization and cost impact of integrating substance abuse treatment and primary care. Med Care. 2003;41(3):357–367. doi: 10.1097/01.MLR.0000053018.20700.56. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R Foundation for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. R: A language and environment for statistical computing. (Version 2.14.2) [Computer Software] [Google Scholar]
- Ray GT, Collin F, Lieu T. The cost of health conditions in a health maintenance organization. Med Care Res Rev. 2000;57(1):92–109. doi: 10.1177/107755870005700106. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorcharoesap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rice J, White A, Birnbaum H, Schiller M, Brown D, Roland C. A model to identify patients at risk for prescription opioid abuse, dependence and misuse. Pain Med. 2012;13(9):1162–1173. doi: 10.1111/j.1526-4637.2012.01450.x. [DOI] [PubMed] [Google Scholar]
- Schuckit M. Alcohol-use disorders. Lancet. 2009;373:493–501. doi: 10.1016/S0140-6736(09)60009-X. [DOI] [PubMed] [Google Scholar]
- Sorace J, Wong H, Worrall C, Kelman J, Saneinejad S, MaCurdy T. The complexity of disease combinations in Medicare population. Popul Health Manag. 2011;14(4):161–166. doi: 10.1089/pop.2010.0044. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Results from the 2014 National Survey on Drug Use and Health: Summary of National Findings (HHS Publication No. SMA 15-4927, NSDUH Series H-50) 2015 Retrieved from http://www.samhsa.gov/data/
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: Substance Use and Mental Health Estimates from the 2013 National Survey on Drug Use and Health: Overview of Findings. Rockville, MD: 2014. Sep 4, [PubMed] [Google Scholar]
- Tetault J, Crothers K, Moore B, Mehra C, Fiellin D. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167:221–228. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N, Frieden T, Hyde P, Stephen S. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Birnbaum H, Schiller M, Tang J, Katz N. Analytic models to identify patients at risk for prescription opioid abuse. Am J Manag C. 2009;15(12):897–906. [PubMed] [Google Scholar]
- Whiteford H, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Young JQ, Kline-Simon AH, Mordecai DJ, Weisner C. Prevalence of behavioral health disorders and associated chronic disease burden in a commercially insured health system: findings of a case-control study. Gen Hosp Psychiat. 2015;37:101–108. doi: 10.1016/j.genhosppsych.2014.12.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


