Abstract
Objectives
The aim of this study was to determine if the Affordable Care Act (ACA) Medicaid Expansion was associated with increased census-adjusted heart transplant listing rates for racial/ethnic minorities.
Background
Underinsurance limits access to transplants, especially among racial/ethnic minorities. Changes in racial/ethnic listing rates post the ACA Medicaid Expansion are unknown.
Methods
Using the Scientific Registry of Transplant Recipients, we analyzed 5,651 patients from early adopter states (implemented ACA Medicaid Expansion by 1/2014) and 4,769 patients from non-adopter states (no implementation during study period) from 2012–2015. Piecewise linear models, stratified by race/ethnicity, were fit to monthly census-adjusted rates of heart transplant listings before and after 1/2014.
Results
A significant 30% increase in the rate of heart transplant listings for African-Americans in early adopter states occurred immediately following the ACA Medicaid Expansion on 1/1/2014 [pre 0.15 to post 0.20/100,000, increase 0.05/100,000 (95%Confidence Interval (CI): 0.01,0.08)]; in contrast, the rates for African-Americans in non-adopter states remained constant [pre and post 0.15/100,000, increase 0.006/100,000 (95%CI: −0.03,0.04)]. Hispanics experienced an opposite trend, with no significant change in early adopter states [pre 0.03 to post 0.04/100,000, increase 0.01/100,000 (95%CI: −0.004,0.02)] and a significant increase in non-adopter states [pre 0.03 to post 0.05/100,000, increase 0.02/100,000 (95%CI: 0.002,0.03)]. There were no significant changes in listing rates among Caucasians in either early adopter or non-adopter states.
Conclusions
Implementation of the ACA Medicaid Expansion was associated with increased heart transplant listings in African-Americans but not Hispanics or Caucasians. Broadening of the ACA in states with large African-American populations may reduce disparities in heart transplant listings.
Keywords: racial disparities, healthcare policy, insurance
INTRODUCTION
Racial/ethnic minorities are not listed for heart transplant at equitable levels of disease prevalence.(1–4) Underinsurance is a major contributor to this inequality in heart transplant allocation among racial/ethnic minorities.(1–6) Adequate health insurance or demonstration of ability to pay is a requirement for heart transplantation listing in all programs.(5) Approximately 43% of heart transplant patients have public insurance, and 30% of those patients have Medicaid.(7) Historically, racial/ethnic minorities have had the highest rates of uninsurance.(8) With the implementation of the Affordable Care Act (ACA), many racial/ethnic minorities have improved access to healthcare.(9–11) However, the correlation of ACA Medicaid Expansion with heart transplant listing rates among racial/ethnic minorities is unknown. Medicaid expansion did not occur uniformly, with only 44% of states expanding Medicaid (early ACA adopter states) in 2014.(12) Given the increased number of racial/ethnic minorities insured under Medicaid Expansion, we hypothesized that the census-adjusted heart transplant listing rates for racial/ethnic minorities increased in early adopter ACA Medicaid Expansion states compared with non-adopter states.
METHODS
Data Source
Patients listed for heart transplant were identified in the national Scientific Registry of Transplant Recipients (SRTR) database. The SRTR data system includes data on all donor, wait-listed candidates, and transplant recipients in the U.S., submitted by the members of the Organ Procurement and Transplantation Network. The SRTR database collects data on demographics, including race/ethnicity, comorbidities, clinical data, insurance, education level, and transplant center state, and has been reported elsewhere.(13) SRTR reports <1% of race/ethnicity data as missing over the past decade.(14) The Health Resources and Services Administration, U.S. Department of Health and Human Services provides oversight to the activities of the Organ Procurement and Transplantation Network and SRTR contractors, and sites are periodically audited.
Study Population
Adults 18 years of age or older with a single listing for heart transplant in the U.S. between January 2012 and December 2015 were identified. Patients with a listed race of African-American, Caucasian, or ethnicity of Hispanic were included.
ACA Medicaid Expansion State Stratification
Early adopter states were defined as those that implemented ACA Medicaid Expansion by January 2014 and non-adopter states were defined as those that did not implement by December 2015 (Figure 1). Patients were aggregated into early adopter and non-adopter state groups. Patients who were listed in states that adopted the ACA Medicaid Expansion between February 2014 and December 2015 (n= 5) or states which reduced coverage with adoption were excluded (n=2),(12) since the objective was to compare access to heart transplant listing before and after implementation of the ACA Medicaid Expansion in January 2014.
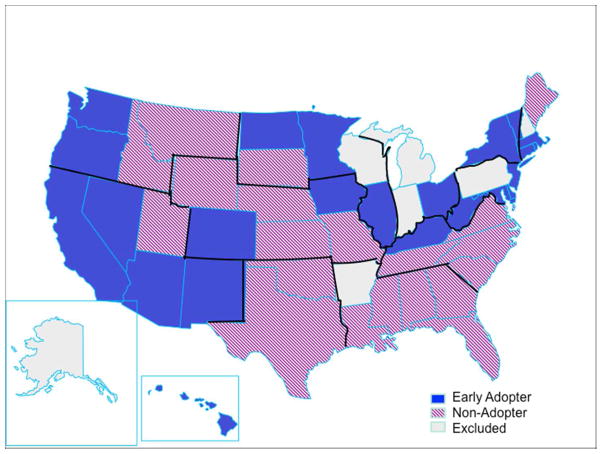
Figure 1. U.S. Map of ACA Medicaid Expansion Status.
States are stratified by ACA Medicaid Expansion adoption status as of January 2014. Blue states indicate early adopter states; Purple striped, non-adopter states from January 2014-December 2015; and gray, states excluded from analysis due to status change or reduced coverage from January 2014- December 2015.
The 11 Organ Procurement Organizations are outlined in black. This figure was created with Presentation Magazine.
Medicaid was partially expanded prior to the federal ACA Medicaid Expansion of 2014 in 19 states and the District of Columbia (Figure 1).(15) However these partial expansions were limited in sized and scope and had substantially lower enrollment than the ACA Medicaid Expansion.(15) Therefore, these states were included in the analysis and we did not control for the timing of the partial pre-ACA Medicaid Expansion.
Outcome
The primary outcome of interest was the census-adjusted rate of heart transplant listing. The listing rate was chosen as the outcome rather than heart transplantation rate since insurance is directly related to the initial step of heart transplant listing. After a patient is listed, insurance type has little association with likelihood of transplantation.
The state level census data were obtained from the annual projected U.S. Census Bureau estimates and were used to calculate census-adjusted rates of heart transplant listing by state, race, and ethnicity. Census data were not available for year 2015; therefore, 2014 census data were used to adjust heart transplant listings from 2014–2015. All other census years were available for adjustment. The state level census was chosen as the denominator since statewide data on the at-risk end-stage heart failure population who may be eligible for heart transplant are not available. In addition, the racial/ethnic populations differ significantly in early adopter and non-adopter states. The U.S. census has been used as the denominator in previous studies to demonstrate transplantation rates.(16)
Statistical Analysis
Baseline patient characteristics were compared in ACA early adopter and non-adopter states using chi-square tests for categorical variables and Wilcoxon-Mann-Whitney tests for continuous variables.
Piecewise linear models were fit to monthly census-adjusted rates of heart transplant listings in order to test the impact of ACA Medicaid Expansion implementation. The piecewise linear models incorporate parameters for changes in heart transplant listings over time, and they permit the slopes to differ between early adopter and non-adopter states prior to and post-ACA Medicaid Expansion. This approach was chosen over pre-test/post-test design because the data did not appear to satisfy the parallel trends assumption. Most importantly, piecewise linear models allow for estimation of an instantaneous change in rate, which we set at January 2014, concurrent with ACA Medicaid Expansion. Piecewise models have been used to estimate the association between policy implementation and patient outcomes in previous studies.(17, 18) To implement this model, binary factors were specified for ACA Medicaid Expansion (prior to and after January 2014) and for early adopter states versus non-adopter states. Models were stratified by race/ethnicity. In a secondary analysis, models were specified for the most populated insurance groups (Medicaid, private, and Medicare), in a similar fashion. Statistical analyses were performed using SAS 9.4 (Cary, NC) and R.
RESULTS
Patient Characteristics
Between 2012 and 2015, there were 5,651 patients listed in 23 early adopter states plus the District of Columbia and 4,769 listed in 20 non-adopter states (Table 1, Figure 1). The majority of patients listed for transplant were Caucasian in both early adopter and non-adopter states (62.8% and 60.2% respectively), followed by African-Americans (20.9% and 29.3% respectively) and Hispanics (9.7% and 7.8% respectively). Compared with 2012 census demographics, listing proportions were similar for Caucasians from both early adopter (62.8% listed, 60.1% census) and non-adopter states (60.2% listed, 61.3% census). Among African-Americans, listing proportions were higher than census demographics in both early adopter (20.9% listed, 9.3% census) and non-adopter (29.3% listed 16.9% census) states. Among Hispanics, listing proportions were lower than census demographics in both early adopter (9.7% listed, 20.1% census) and non-adopter (7.8% listed, 16.5% census) states.
Table 1.
Characteristics of Patients Listed for Transplant Stratified by Early Adopter and Non-Adopter States 2012–2015
| Early Adopter N=5,651 | Non-Adopter N=4,769 | p-value | |||
|---|---|---|---|---|---|
| N | (%) | N | (%) | ||
| Age, Median (IQR) | 56 | (46–63) | 56 | (46–63) | 0.82 |
|
| |||||
| Age | 0.45 | ||||
|
| |||||
| 18–34 | 566 | (10.0) | 443 | (9.3) | |
|
| |||||
| 35–49 | 1210 | (21.4) | 1047 | (22.0) | |
|
| |||||
| 50–64 | 2839 | (50.2) | 2434 | (51.0) | |
|
| |||||
| 65+ | 1036 | (18.3) | 845 | (17.7) | |
|
| |||||
| Gender | 0.40 | ||||
|
| |||||
| Female | 1459 | (25.8) | 1197 | (25.1) | |
|
| |||||
| Race | <0.0001 | ||||
|
| |||||
| Caucasian | 3550 | (62.8) | 2871 | (60.2) | |
|
| |||||
| African- American | 1182 | (20.9) | 1395 | (29.3) | |
|
| |||||
| Hispanic | 549 | (9.7) | 374 | (7.8) | |
|
| |||||
| Other | 370 | (6.5) | 129 | (2.7) | |
|
| |||||
| Insurance category | <0.0001 | ||||
|
| |||||
| Private | 2842 | (50.3) | 2432 | (51.0) | |
|
| |||||
| Medicaid | 892 | (15.8) | 393 | (8.2) | |
|
| |||||
| Medicare | 1699 | (30.1) | 1727 | (36.2) | |
|
| |||||
| Other | 218 | (3.9) | 217 | (4.6) | |
|
| |||||
| Diagnosis | <0.0001 | ||||
|
| |||||
| Ischemic | 1917 | (33.9) | 1794 | (37.6) | |
|
| |||||
| Dilated | 3035 | (53.7) | 2558 | (53.6) | |
|
| |||||
| Hypertrophic | 128 | (2.3) | 66 | (1.4) | |
|
| |||||
| Restrictive | 226 | (4.0) | 113 | (2.4) | |
|
| |||||
| Valvular | 104 | (1.8) | 55 | (1.2) | |
|
| |||||
| Congenital | 167 | (3.0) | 123 | (2.6) | |
|
| |||||
| Other | 74 | (1.3) | 60 | (1.3) | |
|
| |||||
| Education | 0.006 | ||||
|
| |||||
| Less than HS | 205 | (3.6) | 141 | (3.0) | |
|
| |||||
| HS or GED | 1981 | (35.1) | 1840 | (38.6) | |
|
| |||||
| Attended college | 1463 | (25.9) | 1330 | (27.9) | |
|
| |||||
| College grad | 1035 | (18.3) | 839 | (17.6) | |
|
| |||||
| Post-college grad | 479 | (8.5) | 376 | (7.9) | |
|
| |||||
| Other/ unknown | 488 | (8.6) | 243 | (5.1) | |
|
| |||||
| Listing status | <0.0001 | ||||
|
| |||||
| Status 1A | 1639 | (29.0) | 1056 | (22.1) | |
|
| |||||
| Status 1B | 2055 | (36.4) | 2371 | (49.7) | |
|
| |||||
| Status 2 | 1764 | (31.2) | 1142 | (23.9) | |
|
| |||||
| Temp Inactive | 193 | (3.4) | 200 | (4.2) | |
|
| |||||
| ABO blood group | 0.54 | ||||
|
| |||||
| A | 2108 | (37.3) | 1737 | (36.4) | |
|
| |||||
| AB | 299 | (5.3) | 248 | (5.2) | |
|
| |||||
| B | 843 | (14.9) | 678 | (14.2) | |
|
| |||||
| O | 2394 | (42.4) | 2100 | (44.0) | |
|
| |||||
| Unknown | 7 | (0.1) | 6 | (0.1) | |
|
| |||||
| PA, mmHg Med(IQR) | 21 | (15–28) | 20 | (14–26) | <0.0001 |
|
| |||||
| Creatinine, Med (IQR) | 1.20 | (0.95– 1.50) | 1.20 | (0.96–1.50) | 0.69 |
|
| |||||
| Prior cardiac surgery | 2239 | (39.6) | 1949 | (40.9) | 0.28 |
|
| |||||
| Unknown | 55 | (1.0) | 23 | (0.5) | |
|
| |||||
| COPD | 177 | (3.1) | 195 | (4.1) | 0.37 |
|
| |||||
| Unknown | 2434 | (43.1) | 1528 | (32.0) | |
|
| |||||
| Diabetes | 1654 | (29.3) | 1472 | (30.9) | 0.12 |
|
| |||||
| Unknown | 51 | (0.9) | 10 | (0.2) | |
|
| |||||
| Hypertension | 2066 | (36.6) | 1953 | (41.0) | 0.65 |
|
| |||||
| Unknown | 2204 | (39.0) | 1481 | (31.1) | |
|
| |||||
| IV Inotropes | 1588 | (28.1) | 1759 | (36.9) | <0.0001 |
|
| |||||
| Albumin<3.5 g/dL | 962 | (17.0) | 1142 | (23.9) | <0.0001 |
|
| |||||
| Unknown | 2406 | (42.6) | 1519 | (31.9) | |
|
| |||||
| Obesity | 1898 | (33.6) | 1731 | (36.3) | 0.004 |
|
| |||||
| Unknown | 5 | (0.1) | 6 | (0.1) | |
|
| |||||
| Prior tobacco use | 2633 | (46.6) | 2416 | (50.7) | 0.0001 |
|
| |||||
| Unknown | 40 | (0.7) | 3 | (0.1) | |
|
| |||||
| ECMO | 93 | (1.6) | 42 | (0.9) | 0.0006 |
|
| |||||
| ICD | 4340 | (76.8) | 3837 | (80.5) | <0.0001 |
|
| |||||
| Unknown | 67 | (1.2) | 23 | (0.5) | |
|
| |||||
| IABP | 220 | (3.9) | 252 | (5.3) | 0.0007 |
|
| |||||
| Ventilator | 106 | (1.9) | 69 | (1.4) | 0.09 |
|
| |||||
| VAD | 0.0002 | ||||
|
| |||||
| LVAD | 1413 | (25.0) | 1194 | (25.0) | |
|
| |||||
| RVAD | 5 | (0.1) | 2 | (0.0) | |
|
| |||||
| TAH | 46 | (0.8) | 33 | (0.7) | |
|
| |||||
| LVAD+RVAD | 115 | (2.0) | 51 | (1.1) | |
|
| |||||
| LVAD/RVAD/ TAH Unspecified | 119 | (2.1) | 69 | (1.4) | |
|
| |||||
| Unknown | 26 | (0.5) | 3 | (0.1) | |
|
| |||||
| Functional status | <0.0001 | ||||
|
| |||||
| Disabled | 2455 | (43.4) | 1905 | (39.9) | |
|
| |||||
| Some assistance | 1388 | (24.6) | 1238 | (26.0) | |
|
| |||||
| Unknown | 285 | (5.0) | 80 | (1.7) | |
|
| |||||
| Working for income | 624 | (11.0) | 518 | (10.9) | 0.54 |
|
| |||||
| Unknown | 224 | (4.0) | 105 | (2.2) | |
COPD indicates chronic obstructive pulmonary disease; ECMO, extracorporeal membrane oxygenation; GED, general education development; Grad, graduate; HS, high school; IABP, intra-aortic balloon pump; ICD, implantable cardioverter defibrillator; IQR, interquartile range; IV, intravenous; Med, median; PA, pulmonary artery; p, p-value; TAH, total artificial heart; Temp, temporary inactive; VAD, ventricular assist device (LVAD, left VAD; RVAD, right VAD).
The proportion of patients listed for heart transplant based upon insurance type included private insurance in 50.3% of early adopter states and 51.0% of non-adopter states, Medicaid in 15.8% of early adopter states and 8.2% of non-adopter states, and Medicare in 30.1% of early adopter states and 36.2% of non-adopter states. Approximately half of patients listed in non-adopter states were status 1b. Patients from early adopter states were split into thirds at status 1a, 1b, and 2. The patterns were similar among Caucasians for each state group. (Supplemental Table 1) However among African-Americans and Hispanics from both state groups, a larger proportion were listed as status 1b and a smaller proportion were listed as 2.
Outcome
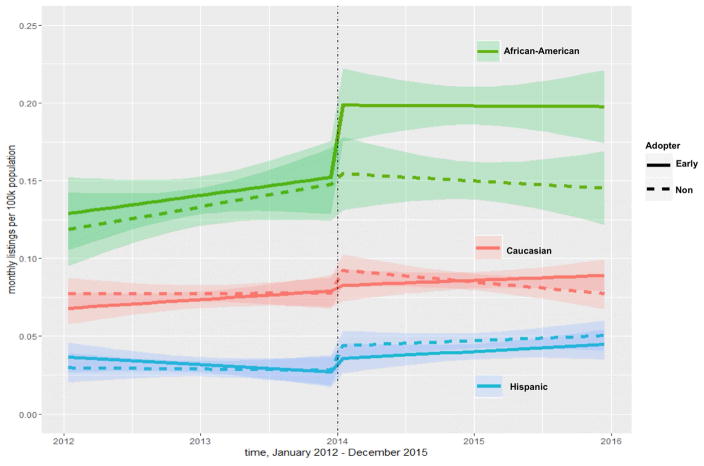
The census-adjusted heart transplant listing rates were highest in African-Americans throughout the study period, followed by Caucasians, and Hispanics (Figure 2, Supplemental Figure). Within each race/ethnicity, heart transplant listing rates were similar in early and non-adopter states before the ACA Medicaid Expansion (Figure 2, Table 2).
Figure 2. Heart Transplant Listing Rates Per Capita in Early and Non-Adopter ACA Medicaid Expansion States.
Predicted monthly heart transplant listing rates from the piecewise linear regression models are presented with shaded 95% CI bands. The solid line indicates early adopter states. Dashed indicates non-adopter states. Green represents African-Americans; red, Caucasian; and blue, Hispanic. The vertical dashed line indicates the time of implementation of the ACA Medicaid Expansion.
Table 2.
Fitted Monthly Heart Transplant Listing Rates and Rate Changes Per 100,000 Population
| Pre-ACA | ACA Medicaid Expansion | Post-ACA | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Change in rate over time | Final Rate December 2014 | Change in rate January 1, 2014 | Change in rate over time | Final Rate December 2015 | ||
| African- American | Early Adopter | 0.001/month (−0.001, 0.003) | 0.15 (0.13, 0.18) | 0.05* (0.01, 0.08) | −0.00004/month (−0.002, 0.002) | 0.20 (0.18, 0.23) |
|
|
||||||
| Estimate (95% CI) | Non- Adopter | 0.001/month (−0.0005, 0.003) | 0.15 (0.12, 0.17) | 0.006 (−0.03, 0.04) | −0.0004/month (−0.002, 0.001) | 0.15 (0.12, 0.17) |
|
|
||||||
|
Caucasian
Estimate (95% CI) |
Early Adopter | 0.001/month (−0.0003, 0.001) | 0.08 (0.07, 0.09) | 0.004 (−0.01, 0.02) | 0.0003/month (−0.0005, 0.001) | 0.09 (0.08, 0.10) |
|
|
||||||
| Non- Adopter | 0.00002/month (−0.001, 0.001) | 0.08 (0.07, 0.09) | 0.01 (−0.001, 0.03) | −0.0006/month (−0.001, 0.0001) | 0.08 (0.07, 0.09) | |
|
|
||||||
| Hispanic Estimate (95% CI) | Early Adopter | −0.0004/month (−0.001, 0.0003) | 0.03 (0.02, 0.04) | 0.01 (−0.004, 0.02) | 0.0004/month (−0.0003, 0.001) | 0.04 (0.04, 0.05) |
|
|
||||||
| Non- Adopter | −0.0001/month (−0.001, 0.001) | 0.03 (0.02, 0.04) | 0.02* (0.002, 0.03) | 0.0003/month (−0.0004, 0.001) | 0.05 (0.04, 0.06) | |
indicates significance p<0.05 for a rate change
Immediately following the ACA Medicaid Expansion, the heart transplant listing rate increased significantly by 30% in African-Americans in early adopter states [pre 0.15 to post 0.20/100,000, increase 0.05/100,000 (95%CI: 0.01, 0.08)]. Rates were constant among African-Americans in non-adopter states [pre and post 0.15/100,000, increase 0.006/100,000 (95%CI: −0.03, 0.04) Figure 2, Table 2]. Rates increased in Hispanics from both early adopter and non-adopter states, but the change was only significant in non-adopter states [early adopter: pre 0.03 to post 0.04/100,000, increase 0.01/100,000 (95%CI: −0.004, 0.02); non-adopter: pre 0.03 to post 0.05/100,000, increase 0.02/100,000 (95%CI: 0.002, 0.03)]. Rates did not change significantly among Caucasians from either early adopter or non-adopter states [early adopter: pre 0.08 to post 0.09, increase 0.004/100,000 (95%CI: −0.01, 0.02); non-adopter: pre and post 0.08, increase 0.01/100,000 (95%CI: −0.001, 0.03)]. Heart transplant listing rates stabilized after initial changes post-ACA Medicaid Expansion. From 2014–2015, the rate of change over time was similar within each race/ethnicity (Figure 2, Table 2, Supplemental Table 2).
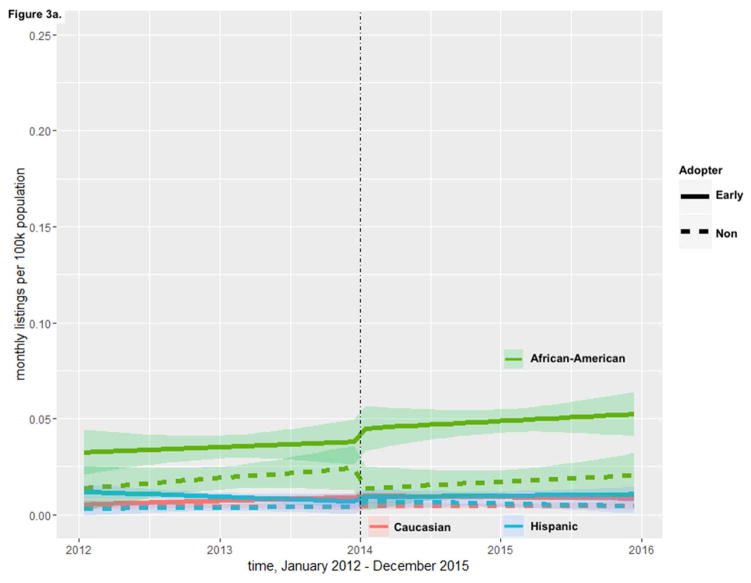
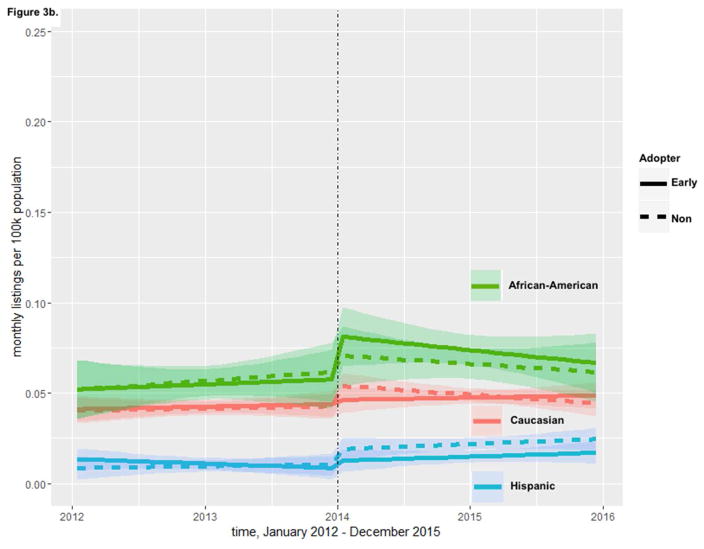
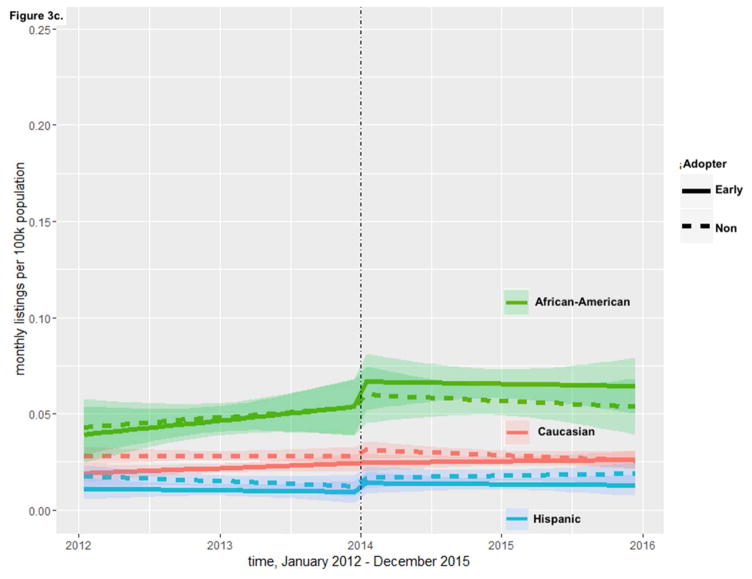
In a secondary analysis, we evaluated changes in racial/ethnic listing rates post the ACA Medicaid Expansion among each subgroup of insurance. Among those with Medicaid, African-American patients had somewhat higher heart transplant listing rates pre-ACA Medicaid Expansion in early adopter states compared to non-adopter states. When the ACA Medicaid Expansion was implemented, rates further diverged in African-Americans with Medicaid, and were significantly higher in early adopter states from 2014 to 2015 (Figure 3a, non-overlapping confidence intervals). Among those with Medicaid, no change in listing rates was observed pre and post-ACA in other racial groups. Among patients with private insurance and among those with Medicare, listing rates increased in African-Americans at the time of the ACA Medicaid Expansion in both early adopter and non-adopter states, but with no significant differences in rates between the two. Among the other racial groups with private insurance and Medicare, no significant differences in listing rates were observed in either early adopter or non-adopter states following ACA Medicaid Expansion (Figures 3b and 3c, overlapping confidence intervals). In all insurance groups, rates were highest post-ACA Medicaid Expansion in African-Americans in early adopter states.
Figure 3. Heart Transplant Listing Rates Per Capita in Early and Non-Adopter ACA Medicaid Expansion States Based Upon Insurance Group.
Predicted monthly heart transplant listing rates from the piecewise linear regression models are presented with shaded 95% CI bands for insurance groups: 3a.Medicaid, 3b.Private, and 3c.Medicare. The solid line indicates early adopter states. Dashed indicates non-adopter states. Green represents African-Americans; red, Caucasian; and blue, Hispanic. The vertical dashed line indicates the time of implementation of the ACA Medicaid Expansion.
DISCUSSION
The ACA Medicaid Expansion was associated with a significant increase in heart transplant listings in African-Americans, but not among Hispanics or Caucasians. These findings suggest that improved access to insurance may be a partial solution to reducing racial/ethnic disparities in organ allocation in the United States.
To our knowledge, this is the first study to evaluate the association between the ACA and racial/ethnic listings for heart transplant. This study is strengthened by using census-adjusted rates that account for racial/ethnic state-wide differences in population rather than comparing count data reflected in the proportions. Although listing rates for African-Americans are higher than for Caucasians and Hispanics, rates of heart transplant listings remain lower than anticipated for African-Americans. African-Americans are at highest risk for heart failure, have 2–3 fold higher prevalence of heart failure than Caucasians before age 75, and have the highest rates of death from heart failure.(19–21) The factors that contribute to this disparity are numerous, including referral patterns, comorbidities, social support, education, patient-centered decisions, and adherence.(2, 3, 22–24) Because the evaluation and treatment course for heart transplantation is expensive, one of the greatest factors associated with disparities in heart transplantation is underinsurance and uninsurace.(2, 5, 24) A recent research letter by Oliveira et al. demonstrated that the ACA Medicaid Expansion was associated with increased heart transplant listings in early adopter versus non-adopter states.(25) Our findings suggest that expanding insurance coverage may improve racial/ethnic equity in access to heart transplantation, a life-saving treatment.
Results of this study add to a body of literature that suggests that economic and racial/ethnic barriers to healthcare can be reduced with insurance.(11, 26, 27) The ACA increased access to insurance for all citizens and especially African-Americans.(8) All race/ethnicities had reductions in the proportion of uninsured populations after the ACA Medicaid Expansion, and the largest decline was seen in African-Americans.(28) In the National Health Interview Survey, the ACA was associated with significantly improved access to insurance, reduction in delay of care, and increased likelihood of pursuing necessary care among African-Americans and Hispanics.(29) Similarly, state-based analyses of the ACA implementation have revealed reductions in racial/ethnic disparities for healthcare in Massachusetts, California, and Oregon, with the greatest gains in African-Americans compared to other groups.(30–32) These reductions in disparities were seen despite known higher comorbidities among African-Americans.(21)
Our finding that Hispanics from early adopter states did not have increased probability of being listed for a heart transplant is consistent with other work demonstrating that healthcare disparities have not been universally reduced under the ACA.(11, 33, 34) There are various possible explanations for this finding. First, the risk of heart failure is higher in Hispanics than in Caucasians,(19) but the risk of death from heart failure is lower.(20) Therefore, the prevalence of end-stage heart failure may be lower than expected in this population. Second, longer follow-up may be needed to assess the full change in healthcare access associated with the ACA Medicaid Expansion, although the time trends available in our data suggest immediate rather than gradual changes. Third, the state of Texas accounted for most of the variability among non-adopter states, and Texas had a notable decrease in the proportion of uninsured non-elderly Hispanics from 37% in 2012 to 32% in 2014.(35) This could be related to federally mandated, non-Medicaid Expansion ACA changes in policy and could account for the marginal increase in heart transplant listings among non-adopter states in 2014. However, no increase in listings rates among Hispanics with private insurance was observed in either state group. Finally, an important factor may be that undocumented individuals are ineligible for insurance coverage through the ACA.(33, 34, 36, 37) The three states with the most undocumented individuals include California (6%), which accounts for most of the variability of results of early adopter states, and 2 non-adopter states, Texas (6%) and Florida (4%).(38) Over 70% of undocumented individuals from California and Texas are Mexican, and 19% from Florida are Mexican.(38) Given these factors, it should not be surprising that health policy changes for heart failure care do not manifest the same across racial/ethnic groups.
Because the number of donor hearts is limited, it is critical that different racial and ethnic groups have equitable access to this scarce resource.(39) The heart transplant matching process is changing to increase allocation of suitable organs to patients who are deemed to have the greatest need.(39) This could be beneficial to racial/ethnic minorities who were more likely to be listed if an inotrope was indicated in their care.(40) However guidelines for transplantation are not concrete. Conservative transplantation programs may place greater weight on insurance type when deciding which candidates should be listed for transplantation. In some states, patients with basic healthcare coverage like Medicaid may not be given equitable candidacy as patients with Medicare and private insurance since Medicaid programs will not universally cover costs of transplantation.(41) It is paramount to avoid increasing racial/ethnic disparities as the selection process is calibrated particularly among politically divided Organ Procurement Organizations. The main alternative to transplant- left ventricular assist devices (LVADs)- are also disproportionately allocated at lower rates to racial/ethnic minorities.(42, 43) Thus, further study of the impact of the ACA Medicaid Expansion on access to all advanced heart failure therapies would provide necessary additional context for understanding racial/ethnic disparities in advanced heart failure.
Alternate explanations for the increase in heart transplant listing among African-Americans from early adopter states should be considered. First, in addition to implementation of the ACA-Medication Expansion on January 1, 2014, other relevant ACA policy changes included implementation of the following: Health Insurance Exchanges in all 50 states through either state or federally-based marketplaces, prohibition of annual limits on health insurance coverage, and penalties for being a citizen without healthcare insurance.(44) State-based marketplaces were prepared to begin enrollment January 1, 2014; states without marketplace plans were defaulted to federally-based marketplaces.(45) Many of the state-based marketplace programs were in early adopter states of ACA Medicaid Expansion, and likewise many of the federally-based marketplaces were in non-adopter states.(45) While differences in care and outcomes for state versus federally operated marketplaces are not known, it is plausible that patients within states with planned marketplace programs had increased knowledge of policy changes and increased immediate access to insurance on the implementation date. Indeed, transplant center teams include financial coordinators who prospectively evaluate patients for sources of payment prior to listing, help patients identify payment sources, and seek rapid insurance approval for therapies.(46) Second, the U.S. unemployment rate decreased throughout the study period,(47) and a corresponding increase in private insurance may have impacted the results. However, no sudden change in the unemployment rate was observed in 2014,(47) and the increase in heart transplant listings among African-Americans with private insurance was not significant. Third, variation in transplant center density over time was considered as a factor. Although the data for this study had aggregate listings per states with de-identified center data, publicly-reported data revealed no major changes in the number of active transplant centers during the study (111 centers in 2012 and 105 centers in 2015).(48) Similarly, there were no major differences between the two most populous states, which account for a large fraction of the data (Supplemental Table 2), California (11 centers in 2012, 9 centers in 2013, 10 centers in 2014, and 11 centers in 2015) an early adopter state and Texas (9 centers in 2012, 10 centers in 2013–2015) a non-adopter state.(48)
Study Limitations
Several limitations should be considered. First, the number of patients with end-stage heart failure who are eligible for heart transplant is not currently available. Thus, the U.S. census was used as the denominator for rate of heart transplant listing. Second, we do not control for the 15 early adopter states and the District of Columbia and the 4 non-adopter states that partially expanded Medicaid prior to January 1, 2014 full ACA Medicaid Expansion. Excluding these states would have removed a large proportion of patients from the analysis. Therefore, the effects of the ACA Medicaid Expansion may be underestimated. Third, Medicaid insurance has high variability in state level scope of service, quality of care, and reimbursement. This further impacts the ability to achieve equity in access to heart transplant listings. Fourth, the ACA has not been in existence long enough to evaluate long-term outcomes such as wait-list mortality.
CONCLUSION
The rate of heart transplant listings following ACA Medicaid Expansion differed by race and ethnicity. The census-adjusted rate of heart transplant listings for African-Americans increased significantly in early ACA Medicaid Expansion adopting states compared to non-adopting states in January 2014. Listing rates increased marginally in Hispanics in non-adopter states possibly due to ineligibility of undocumented Hispanics for the ACA Medicaid Expansion. There were no changes in rates of heart transplant listings in Caucasians at the time of ACA Medicaid Expansion. This suggests that broader expansion of the ACA may help mitigate racial/ethnic disparities in access to care.
Supplementary Material
Clinical Perspectives.
Competency in Medical Knowledge
Underinsurance limits access to heart transplants especially among racial/ethnic minorities. Broadening insurance access with the ACA Medicaid Expansion was associated with increased heart transplant listing in African-Americans but not Hispanics or Caucasians.
Translational Outlook
Further study of racial/ethnic changes in LVAD implantation post the ACA Medicaid Expansion is warranted.
Abbreviations
- ACA
Affordable Care Act
- LVAD
Left Ventricular Assist Device
- SRTR
Scientific Registry of Transplant Recipients
- U.S
United States
Footnotes
Disclosures: Dr. Breathett received support from a T32 training grant (5T32 HL116276-02) from the National Institute of Health (NIH) and the University of Colorado, Department of Medicine, Health Services Research Development Grant Award. Dr. Allen discloses grant funding from NIH (K23 HL105896), the Patient Centered Outcomes Research Institute (CDR-1310-06998), and the American Heart Association (AHA) (#16SFRN29640000); has served as consultant for J&J, Novartis, St. Jude, and ZS Pharma. Dr. Daugherty discloses grant funding from the National Heart, Lung, and Blood Institute (K08 HL103776) and the AHA (#2515963). Otherwise there are no disclosures. The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the authors(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mitchell JE, Ferdinand KC, Watson KE, et al. Treatment of heart failure in African Americans--a call to action. J Natl Med Assoc. 2011;103:86–98. doi: 10.1016/s0027-9684(15)30257-1. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. Disparities in Solid Organ Transplantation for Ethnic Minorities. [Accessed August 17, 2015];Medscape. Available at: http://www.medscape.com/viewarticle/547386.
- 3.Singh TP, Givertz MM, Semigran M, DeNofrio D, Costantino F, Gauvreau K. Socioeconomic Position, Ethnicity, and Outcomes in Heart Transplant Recipients. Am J Cardiol. 2010;105:1024–1029. doi: 10.1016/j.amjcard.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Pinney SP. Understanding and Eliminating Racial Disparities in TransplantationStill a Ways to Go*. J Am Coll Cardiol. 2013;62:2316–2317. doi: 10.1016/j.jacc.2013.07.070. [DOI] [PubMed] [Google Scholar]
- 5.Thibodeau JT, Rao MP, Gupta C, et al. Health insurance as a requirement to undergo cardiac transplantation: a national survey of transplant program practices. Transplant Proc. 2013;45:360–363. doi: 10.1016/j.transproceed.2012.05.074. [DOI] [PubMed] [Google Scholar]
- 6.Morris AA, Kalogeropoulos AP, Zhao L, et al. Race and ethnic differences in the epidemiology and risk factors for graft failure after heart transplantation. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2015;34:825–831. doi: 10.1016/j.healun.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Morris AA, Cole RT, Laskar SR, et al. Improved Outcomes for Women on the Heart Transplant Wait List in the Modern Era. J Card Fail. 2015;21:555–560. doi: 10.1016/j.cardfail.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Abdus S, Mistry KB, Selden TM. Racial and Ethnic Disparities in Services and the Patient Protection and Affordable Care Act. Am J Public Health. 2015;105(Suppl 5):S668–675. doi: 10.2105/AJPH.2015.302892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenthal D, Abrams M, Nuzum R. The Affordable Care Act at 5 Years. N Engl J Med. 2015;372:2451–2458. doi: 10.1056/NEJMhpr1503614. [DOI] [PubMed] [Google Scholar]
- 10.Shane DM, Ayyagari P. Will health care reform reduce disparities in insurance coverage?: Evidence from the dependent coverage mandate. Med Care. 2014;52:528–534. doi: 10.1097/MLR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 11.McMorrow S, Long SK, Kenney GM, Anderson N. Uninsurance Disparities Have Narrowed For Black And Hispanic Adults Under The Affordable Care Act. Health Aff Proj Hope. 2015;34:1774–1778. doi: 10.1377/hlthaff.2015.0757. [DOI] [PubMed] [Google Scholar]
- 12.Anonymous. [Accessed January 6, 2016];Status of State Action on the Medicaid Expansion Decision. Available at: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 13.Leppke S, Leighton T, Zaun D, et al. Scientific Registry of Transplant Recipients: Collecting, analyzing, and reporting data on transplantation in the United States. Transplant Rev. 2013;27:50–56. doi: 10.1016/j.trre.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Anonymous. 2012 Annual Data Report US Department of Health and Human Services. 2014 Available at: http://srtr.transplant.hrsa.gov/annual_reports/2012/Default.aspx.
- 15.Anonymous. [Accessed August 21, 2015];Total Monthly Medicaid and CHIP Enrollment. Available at: http://kff.org/health-reform/state-indicator/total-monthly-medicaid-and-chip-enrollment/
- 16.Axelrod DA, Guidinger MK, Finlayson S, et al. RAtes of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA. 2008;299:202–207. doi: 10.1001/jama.2007.50. [DOI] [PubMed] [Google Scholar]
- 17.Hardy R. Commentary: Are piecewise mixed effects models useful in epidemiology? Int. J Epidemiol. 2001;30:1341–1342. doi: 10.1093/ije/30.6.1341. [DOI] [PubMed] [Google Scholar]
- 18.Chen C, Scheffler G, Chandra A. Readmission penalties and health insurance expansions: A dispatch from Massachusetts. J Hosp Med. 2014;9:681–687. doi: 10.1002/jhm.2213. [DOI] [PubMed] [Google Scholar]
- 19.Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the Incidence of Congestive Heart Failure by Ethnicity. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anonymous. [Accessed May 1, 2016];Products - Data Briefs - Number 231. 2015 Dec; Available at: http://www.cdc.gov/nchs/products/databriefs/db231.htm.
- 21.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics—2016 Update A Report From the American Heart Association. Circulation. 2015 doi: 10.1161/CIR.0000000000000350. CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 22.Philbin EF, Jenkins PL. Differences between patients with heart failure treated by cardiologists, internists, family physicians, and other physicians: Analysis of a large, statewide database. Am Heart J. 2000;139:491–496. doi: 10.1016/s0002-8703(00)90093-0. [DOI] [PubMed] [Google Scholar]
- 23.Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol. 2001;87:1367–1371. doi: 10.1016/s0002-9149(01)01554-5. [DOI] [PubMed] [Google Scholar]
- 24.Digiorgi PL, Reel MS, Thornton B, Burton E, Naka Y, Oz MC. Heart transplant and left ventricular assist device costs. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2005;24:200–204. doi: 10.1016/j.healun.2003.11.397. [DOI] [PubMed] [Google Scholar]
- 25.Oliveira GH, Al-Kindi SG, Simon DI. IMplementation of the affordable care act and solid-organ transplantation listings in the united states. [Accessed August 10, 2016];JAMA Cardiol. 2016 doi: 10.1001/jamacardio.2016.2067. Available at: http://dx.doi.org/10.1001/jamacardio.2016.2067. [DOI] [PubMed]
- 26.Roundtable on the Promotion of Health Equity and the Elimination of Health Disparities, Board on Population Health and Public Health Practice, Institute of Medicine, National Academies of Sciences, Engineering, and Medicine. Achieving Health Equity via the Affordable Care Act: Promises, Provisions, and Making Reform a Reality for Diverse Patients: Workshop Summary. Washington (DC): National Academies Press (US); 2015. [Accessed May 1, 2016]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK338191/ [PubMed] [Google Scholar]
- 27.Collins SR, Robertson R, Garber T, Doty MM. The income divide in health care: how the Affordable Care Act will help restore fairness to the U. . health system. Issue Brief Commonw Fund. 2012;3:1–24. [PubMed] [Google Scholar]
- 28.Anonymous. [Accessed June 30, 2016];Percent Change in Number of Uninsured by Race/Ethnicity, 2013–2014. Available at: http://kff.org/other/state-indicator/percent-change-in-uninsured-rate-by-raceethnicity-2013-2014/
- 29.Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and Ethnic Disparities in Health Care Access and Utilization Under the Affordable Care Act. Med Care. 2016;54:140–146. doi: 10.1097/MLR.0000000000000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sommers BD, Chua K-P, Kenney GM, Long SK, McMorrow S. California’s Early Coverage Expansion under the Affordable Care Act: A County-Level Analysis. Health Serv Res. 2015 doi: 10.1111/1475-6773.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heintzman J, Bailey SR, DeVoe J, et al. Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon. J Racial Ethn Health Disparities. 2016 doi: 10.1007/s40615-016-0232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tinsley LJ, Hall SA, McKinlay JB. Has Massachusetts health care reform worked for the working poor? Results from an analysis of opportunity. Ann Epidemiol. 2014;24:312–318. doi: 10.1016/j.annepidem.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ortega AN, Rodriguez HP, Vargas Bustamante A. Policy dilemmas in Latino health care and implementation of the Affordable Care Act. Annu Rev Public Health. 2015;36:525–544. doi: 10.1146/annurev-publhealth-031914-122421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang J, Qiao Y, Shih Y-CT, et al. Potential Health Implications of Medication Therapy Management Eligibility Criteria in the Patient Protection and Affordable Care Act Across Racial and Ethnic Groups. J Manag Care Spec Pharm. 2015;21:993–1003. doi: 10.18553/jmcp.2015.21.11.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anonymous. Texas health insurance exchange / marketplace: Obamacare enrollment. [Accessed October 5, 2016];Health Insur Resour Cent. 2016 Available at: https://www.healthinsurance.org/texas-state-health-insurance-exchange/
- 36.McMorrow S, Kenney GM, Goin D. Determinants of receipt of recommended preventive services: implications for the Affordable Care Act. Am J Public Health. 2014;104:2392–2399. doi: 10.2105/AJPH.2013.301569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Breen JO. Lost in Translation — ¿Cómo se dice, “Patient Protection and Affordable Care Act”? N. Engl J Med. 2012;366:2045–2047. doi: 10.1056/NEJMp1202039. [DOI] [PubMed] [Google Scholar]
- 38.Passel JS, Cohn D. 2. State unauthorized immigrant populations. [Accessed October 5, 2016];Pew Res Cent Hisp Trends Proj. 2016 Available at: http://www.pewhispanic.org/2016/09/20/2-state-unauthorized-immigrant-populations/
- 39.Anonymous. [Accessed May 1, 2016];Adult heart allocation changes 2016 - OPTN. Available at: https://optn.transplant.hrsa.gov/governance/public-comment/adult-heart-allocation-changes-2016/
- 40.Singh TP, Almond CS, Taylor DO, Milliren CE, Graham DA. Racial and ethnic differences in wait-list outcomes in patients listed for heart transplantation in the United States. Circulation. 2012;125:3022–3030. doi: 10.1161/CIRCULATIONAHA.112.092643. [DOI] [PubMed] [Google Scholar]
- 41.Allen JE, Unit ANM. Arizona Medicaid Cuts Transplants. [Accessed July 30, 2015];ABC News. 2010 Available at: http://abcnews.go.com/Health/Health_Care/medicaid-cuts-make-organ-transplants-unaffordable/story?id=12177059.
- 42.Joyce DL, Conte JV, Russell SD, Joyce LD, Chang DC. Disparities in access to left ventricular assist device therapy. J Surg Res. 2009;152:111–117. doi: 10.1016/j.jss.2008.02.065. [DOI] [PubMed] [Google Scholar]
- 43.Breathett K, Allen LA, Ambardekar AV. Patient-centered care for left ventricular assist device therapy: current challenges and future directions. Curr Opin Cardiol. 2016:1. doi: 10.1097/HCO.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anonymous. [Accessed June 15, 2016];Health Reform Implementation Timeline. Available at: http://kff.org/interactive/implementation-timeline/
- 45.Anonymous. Health Insurance Exchanges and State Decisions. [Accessed June 15, 2016];Health Aff - Health Policy Briefs. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=96.
- 46.Anonymous. [Accessed June 30, 2016];Learn about the Transplant Team - OPTN. Available at: https://optn.transplant.hrsa.gov/learn/about-transplantation/the-transplant-team/
- 47.Anonymous. [Accessed June 16, 2016];Bureau of Labor Statistics Data. Available at: http://data.bls.gov/timeseries/LNS14000000.
- 48.Anonymous. [Accessed October 4, 2016];SRTR -- Scientific Registry of Transplant Recipients. Available at: http://www.srtr.org/csr/archives/default.aspx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.