Abstract
Background
HIV and sexually transmitted infections (STIs) disproportionately affect women who experience intimate partner violence (IPV).
Objective
The current study 1) applied a syndemic framework to study the collective effects of problematic drug use, hazardous drinking, depression, and posttraumatic stress disorder (PTSD) on fear of condom negotiation, condom negotiation, and condom use and 2) evaluated condom negotiation (controlling for fear of condom negotiation) as a mediator of the association between syndemic severity and condom use among low-income IPV-exposed women.
Methods
Participants were 158 women living in the community and experiencing ongoing IPV who completed face-to-face, computer-assisted interviews. Almost three-fourths of the participants reported problematic drug use, hazardous drinking, depression, and/or PTSD; many of these factors were significantly correlated, indicating a syndemic.
Results
Multivariate logistic and linear regression analyses revealed associations between syndemic severity and fear of condom negotiation (OR = 1.57, p = .02), condom negotiation (β = −8.51, p = .001) and condom use (β = −8.26, p = .01). Meditation analyses identified condom negotiation as a mediator of the association between syndemic severity and condom use (Effect = −6.57, SE = 2.01, [95% CI: − 10.66, − 2.77]).
Conclusions
Results fill a critical gap in previous research by identifying condom negotiation as a mechanism through which this syndemic affects condom use. Prevention and intervention programs should consider addressing condom negotiation to reduce sexual risk among this high-risk population. Further, because IPV-exposed women may experience fear related to condom negotiation, it is critical that prevention and intervention efforts for this population offer skills to safely negotiate condom use, increase condom use, and reduce STI and HIV risk.
Keywords: HIV, Intimate partner violence, condom negotiation, condom use, syndemic
Introduction
HIV and other sexually transmitted infections (STIs) disproportionately affect women who experience intimate partner violence (IPV; Gielen et al., 2007). IPV-exposed women are three times more likely to engage in sexual risk behaviors, including condomless sex, than those without a history of IPV (Cavanaugh, Hansen, & Sullivan, 2010; El-Bassel et al., 2007). IPV and sexual risk behaviors seem to be causally related in complex ways. For example, IPV is associated with heightened rates of other conditions such as substance abuse, depression, and posttraumatic disorder (PTSD; Golding, 1999), which independently affect women’s condom negotiation and use (Peasant, Parra, & Okwumabua, 2014). Furthermore, it has been hypothesized that these interconnected experiences may collectively impair condom negotiation and, as a result, increase condomless sex (Meyer, Springer, & Altice, 2011). While research has underscored the independent impact of substance abuse, depression, and PTSD on sexual risk behaviors, little research has examined the collective impact of these factors, which can be referred to as a syndemic, on condom negotiation and condomless sex. A syndemic describes the co-occurrence of interconnected, biological, or psychosocial epidemics that impact the health of a community or population (Singer & Clair, 2003; Singer, 1996). It is important to understand whether substance abuse, depression, and PTSD intersect to create a syndemic that exacerbates the risk of condomless sex among IPV-exposed women. Further, to develop effective interventions, it is important that research explore whether condom negotiation mediates the association between this syndemic and condomless sex.
Given the frequent co-occurrence of substance abuse, depression, and PTSD among IPV-exposed women (Pico-Alfonso et al., 2006; Sullivan & Holt, 2008), it is not accurate to conceptualize these experiences as separate from each other. The interrelated nature of these experiences should be taken into consideration when examining their influence on condom use. To this end, researchers have highlighted the importance of using a syndemic framework to examine the cumulative impact of multiple adverse experiences on condom use (Meyer et al., 2011; Singer, 1996). Though the syndemic framework has historically conceptualized the impact of co-occurring epidemics of substance use, violence, and HIV/AIDS on health outcomes among the urban poor (Singer, 1996), recent research has demonstrated the application of this framework in examining the effects of other co-occurring biological or psychosocial epidemics on sexual risk (Koblin et al., 2015; Pitpitan et al., 2013). However, no published research has examined the influence of the syndemic of substance abuse, depression, and PTSD on sexual risk among IPV-exposed women. Furthermore, no research has identified the mechanisms which underlie the association between these psychosocial syndemics and condom use.
The male condom is the most effective and accessible form HIV and STI prevention (Ahmed et al., 2001). When condom use is not initiated by male partners, women must negotiate condom use. Therefore, it is important to consider how conditions that are highly prevalent and interrelated among IPV-exposed women, such as substance abuse, depression, and PTSD, effect condom negotiation, and as a result, condomless sex. Research provides support for the independent effects of substance abuse, depression, and PTSD on condom negotiation (Chipman, Palmieri, & Hobfoll, 2011; El-Bassel, Gilbert, Wu, Go, & Hill, 2005). In addition, research has alluded to the fact the condom negotiation may play a role in the syndemic-condom use link (Meyer et al., 2011). However, research has not empirically examined condom negotiation as a potential mediator of the association between syndemics and condom use. The experiences of substance abuse, depression, and PTSD may impair women’s ability or desire to negotiate condom use (Chipman et al., 2011; El-Bassel et al., 2005). Further, this association may be particularly pronounced among IPV-exposed women who may fear the real or perceived consequences of negotiating condom use (e.g., revictimization, abandonment by their partners; El-Bassel et al., 2005; Epperson et al., 2009). Therefore, to inform the development of targeted HIV and STI risk prevention and intervention efforts, it is imperative to understand how the syndemic of substance abuse, depression, and PTSD may impact IPV-exposed women’s negotiation of condom use and, as a result, their use of condoms.
The current study applied a syndemic framework to contribute to existing literature by 1) examining the impact of the syndemic of problematic drug use, hazardous drinking, depression, and PTSD on fear of condom negotiation, condom negotiation, and condom use and 2) evaluating condom negotiation as a mediator of the association between syndemic severity and condom use among IPV-exposed women. We hypothesized that problematic drug use, hazardous drinking, depression, and PTSD would be positively related to each other, indicating a syndemic. We expected that IPV-exposed women who experienced a more severe syndemic (i.e., endorse more factors of the syndemic) would be more fearful of condom negotiation and less likely to negotiate condom use and use condoms. Lastly, we hypothesized that condom negotiation would mediate the effect of syndemic severity on condom use among IPV-exposed women.
Methods
Participants
Participants were women from the greater New Haven community who currently were experiencing IPV and who were a part of a larger study examining the associations among violence, PTSD, and substance use. The final sample was comprised of 212 women. Fifty-six of these women had missing data due to the late inclusion of measures of hazardous drinking and condom negotiation into the assessment. Therefore, 158 participants were included in the current study (see Table 1 for a detailed description).
Table 1.
Sample Characteristics (N = 158)
| Mean (SD)/N (%) | |
|---|---|
| Mean Age (SD) | 36.59 (10.4) |
| Race/Ethnicity, N (%) | |
| Black or African-American | 102 (64.6) |
| White | 39 (24.7) |
| Hispanic/Latina | 12 (7.6) |
| Other | 5 (3.1) |
| Employment, N (%) | |
| Unemployed | 99 (62.7) |
| Part-Time | 42 (26.6) |
| Full-Time | 17 (10.8) |
| Mean Annual Household Income, USD (SD) | 13,939.64 (11,180.5) |
| Mean Years Education (SD) | 12.05 (1.7) |
| Mean Years Relationship Duration (SD) | 6.74 (6.6) |
| Relationship Status | |
| Married or Cohabitating, N (%) | 96 (60.8) |
| Non-cohabitating, N (%) | 62 (39.2) |
| Living with HIV, N (%) | 13 (8.2) |
| Exposed to Physical IPV, N (%) | 158 (100.0) |
| Exposed to Psychological IPV, N (%) | 158 (100.0) |
| Exposed to Sexual IPV, N (%) | 91 (57.6) |
| Drug Use, N (%) | 77 (51.3) |
| Alcohol Use, N (%) | 90 (60.0) |
| Problematic Drug Use, N (%) | 38 (24.8) |
| Hazardous Drinking, N (%) | 48 (30.4) |
| Meets Criteria for Depression, N (%) | 120 (76.0) |
| Meets Criteria for PTSD, N (%) | 60 (38.7) |
| Fear of Condom Negotiation, N (%) | 37 (23.6) |
| Mean Percentage of Condom Negotiation (SD) | 22.47 (40.8) |
| Mean Percentage of Condom Use (SD) | 29.22 (42.9) |
Procedures
Flyers were posted in community establishments (e.g., hair salons, grocery stores, libraries, primary care clinics) in greater New Haven, Connecticut. Women who responded to the recruitment flyers were screened for eligibility over the phone. Eligibility criteria included a) English speaking; b) aged 18 years or older; c) physical victimization from a male partner in the past six months; d) face to face contact with their male partner at least twice per week; e) less than 2 weeks apart from their male partner in the last month; and f) a household income of less than or equal to $4,200 per month.
After providing informed consent, women completed face-to-face, computer-assisted interviews administered by trained female research associates. Women were remunerated $50, debriefed and provided with a list of community resources after the completion of the interview. The university institutional review board approved all study procedures.
Measures
Demographic factors and information to characterize the sample
Questions were used to assess participants’ age, race/ethnicity, education level, employment status, relationship status, and annual income. Questions from the physical assault subscale of the Conflict Tactics Scale – 2 (Straus, Hamby, Boney-McCoy, & Sugarman, 1996) were used to assess participants physical IPV victimization during the last 6 months. The Psychological Maltreatment of Women Inventory (Tolman, 1989) was used to assess psychological IPV victimization during the past 6 months. In addition, a single item was used to assess women’s HIV status.
Syndemic factors
Problematic drug use
The Drug Abuse Screening Test (Skinner, 1982) was used to assess the presence of problematic drug use; the measure was modified to assess the past six months. Consistent with recommendations (Skinner, 1982), women who endorsed ≥ 3 drug use problems were coded as 1 (problematic drug use) and those who endorsed < 3 drug use problems were coded as 0 (non-problematic drug use). Cronbach’s alpha was .80.
Hazardous drinking
The Hazardous Drinking subscale of the Alcohol Use Disorders Identification Test (Saunders et al., 1993) was used to assess patterns of alcohol consumption that increased the risk of harmful consequences; the measure was modified to assess the past six months. Consistent with recommendations (Saunders et al., 1993), women who had scores ≥ 4 were coded as 1 (hazardous drinking) and those with a score < 4 were coded as 0 (non-hazardous drinking). Cronbach’s alpha was .81.
Depression
The Center for Epidemiological Studies-Depression Scale (CES-D; Radloff, 1977) assessed the severity of depressive symptoms in the past six months. Consistent with recommendations (Radloff, 1977), women who had scores of ≥ 16 were coded as 1 (depressed) and those with a score of < 16 were coded as 0 (not depressed). Cronbach’s alpha was .84.
Posttraumatic stress disorder
The Posttraumatic Stress Diagnostic Scale (PDS; Foa, 1995) assessed past six-month PTSD symptoms stemming from IPV. Women who met DSM-IV criteria for PTSD (the presence of a traumatic event; > 1 re-experiencing symptom; > 3 avoidance/numbing symptoms; > 2 hyperarousal symptoms; duration of at least 1 month; impairment in at least two areas of functioning; and the onset of symptoms occurring less than six months after the stressor were coded as 1 and those who did not were coded as 0.
Condom use
Fear of condom negotiation
Fear of condom negotiation was assessed by the question “In the last 6 months, if you had asked your partner to wear a condom, how afraid would you have been that he would become physically abusive?” Responses were recoded such that women who endorsed not being fearful were coded as 0 and those who endorsed any fear (i.e., being just a little frightened, somewhat frightened, or very frightened [i.e., responses of 1, 2 or 3]) were coded as 1.
Condom negotiation
Condom negotiation was assessed by the following items: “In the last 6 months, how many times did you have vaginal or anal sex with your partner?” and “In the last 6 months, how many times did you ask your partner to wear a condom?” Participants’ percentage of condom negotiation was calculated by dividing the number of instances of condom negotiation by the total number of episodes of sexual intercourse, which was then multiplied by 100.
Condom use
Condom use was assessed by the following items: “In the last 6 months, how many times did you have vaginal or anal sex with your partner?” and “How many of those times did you use a condom?” Participants’ percentage of condom use was calculated by dividing the number of instances of condom use by the total number of episodes of sexual intercourse, which was then multiplied by 100.
Covariates
Sexual IPV
Sexual IPV was assessed using the Sexual Experiences Survey (SES; Koss, Gidycz, & Wisniewski, 1987). Consistent with recommendations set forth in the literature (e.g., Gidycz et al., 2007), the Sexual Experiences Survey was dichotomized. Women who endorsed any sexual IPV in the past six months were coded as 1 (Sexual IPV) and those who did not were coded as 0 (No sexual IPV). Cronbach’s alpha was .89.
Childhood sexual abuse
The Childhood Trauma Questionnaire (CTQ; Bernstein et al., 2003; Bernstein & Fink, 1998) was used to assess childhood sexual abuse. Responses were recoded such that women who endorsed no or minimal child sexual abuse were coded as 0 and those who endorsed low to extreme child sexual abuse were coded as 1. Cronbach’s alpha was .84.
Analytic Approach
Preliminary analyses
SPSS version 21 was used to conduct all analyses. Descriptive statistics were computed. Based on previous research (Pitpitan et al., 2013), measures of the syndemic (problematic drug use, hazardous drinking, depression, and PTSD) were dichotomized in order to create count variables and to model the collective effects of each variable. Correlational analyses were then conducted to examine the relations among demographic and psychosocial characteristics and the outcomes (i.e., fear of condom negotiation, condom negotiation, and condom use). Variables that were significantly associated with the outcomes were included as covariates.
Using logistic regression, we examined the bivariate relations among the factors of the syndemic. Further, using logistic and linear regression, we evaluated bivariate associations among the factors of the syndemic and fear of condom negotiation, condom negotiation, and condom use.
Primary analyses
Syndemic severity
Consistent with previous research (Parsons, Grov, & Golub, 2012; Pitpitan et al., 2013), we created a syndemic severity score to reflect the extent to which each woman experienced each factor of the syndemic (i.e., problematic drug use, hazardous drinking, depression, and PTSD). Women received a score of 1 for each factor of the syndemic they experienced. Thus, syndemic severity scores ranged from 0 to 4.
Syndemic severity and condom use factors
We assessed the association between the syndemic severity score and fear of condom negotiation, condom negotiation, and condom use. Multivariate logistic regression analysis was used for the dichotomous outcome (fear of condom negotiation) and multivariate linear regression analyses were used for continuous outcomes (condom negotiation and use). Then, we tested whether condom negotiation mediated the relation between the syndemic severity score and condom use. Using PROCESS (Hayes, 2012), ordinary least squares regression and bootstrapping methods were used to estimate the direct and indirect effects of the hypothesized associations, after controlling for covariates and fear of condom negotiation. A bootstrapping sample of 5,000 was used to estimate the standard errors of parameter estimates and the bias-corrected 95% confidence intervals of the indirect effects were used to determine mediation. Confidence intervals that did not contain zero indicated a significant effect (Hayes, 2012).
Results
Characteristics of the Study Sample
This sample of IPV-exposed women was comprised of a majority of African American women (65%), followed by White women (25%), Hispanic women (8%), and women who identified as another race/ethnicity (3%). The average age of the participants was 36.59 (SD = 10.4). Most of the participants were unemployed (63%), while smaller percentages were employed part-time (27%) and full-time (11%). The average number of years of education was 12.05 (SD = 1.7) and the mean annual household income was $13,939.64 (SD = 11,180.50). The average number of years in their current relationship was 6.74 (SD = 6.6). Approximately 8% of the women in this sample reported that they were living with HIV, 58% reported experiencing sexual IPV, 100% reported psychological IPV, and 47% reported childhood sexual abuse; per the inclusion criteria, all women experienced physical IPV.
Problematic drug use (25%), hazardous drinking (31%), depression (76%), and PTSD (39%) were prevalent among the women in this study (see Table 1). The following demographic variables were significantly associated with fear of condom negotiation, condom negotiation, and condom use and were therefore included as covariates in subsequent analyses: age, HIV status, history of child sexual abuse, and exposure to sexual IPV.
Table 2 presents bivariate associations among factors of the syndemic. Women with (versus without) problematic drug use were more likely to endorse hazardous drinking and more likely to report depression and PTSD. Women with (versus without) depression were more likely to report PTSD. The significant associations among many of the syndemic factors provide evidence supportive of a syndemic.
Table 2.
Bivariate Associations between Syndemic Variables and Sexual Risk
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Problematic Drug Use | --- | ||||||
| 2. Hazardous Drinking | OR=4.45*** (2.04, 9.68) |
--- | |||||
| 3. Depression | OR= 3.57* (1.17, 10.83) |
OR = 1.88 (0.79, 4.46) |
--- | ||||
| 4. PTSD | OR = 2.90** (1.36, 6.18) |
OR = 1.97† (0.99, 3.95) |
OR = 16.16*** (3.72, 70.35) |
--- | |||
| 5. Fear Condom Negotiation | OR = 2.89* (1.29, 6.46) |
OR = 1.36 (0.60, 2.87) |
OR = 2.43† (0.87, 6.76) |
OR = 3.92** (1.79, 8.58) |
--- | ||
| 6. Condom Negotiation % | β = −1.02 (SE = 7.83) |
β = −15.25* (SE = 6.99) |
β = −7.98 (SE = 7.60) |
β = −12.36† (SE = 6.79) |
β = 0.72*** (SE = 0.56) |
--- | |
| 7. Condom Use % | Β = −3.74 (SE = 8.40) |
β = −14.17† (SE =7.59) |
β = −22.44** (SE = 8.14) |
β = −18.84** (SE = 7.28) |
OR = 0.99 (0.98, 1.00) |
OR= 1.00 (0.99, 1.01) |
--- |
Note,
p ≤ .001,
p ≤ .01,
p ≤ .05,
p ≤ .10
Regarding relations among factors of the syndemic, fear of condom negotiation, condom negotiation, and condom use (see Table 2), problematic drug use and PTSD were positively associated with fear of condom negotiation. Hazardous drinking was negatively related to condom negotiation. Depression and PTSD were negatively associated with condom use.
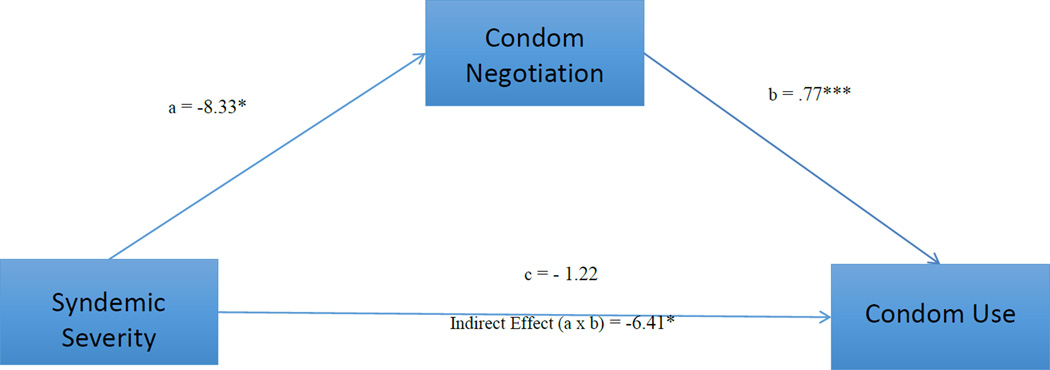
Effects of the Syndemic on Condom Use
Approximately 17% of the women were not experiencing any factors of the syndemic; 28% were experiencing one factor, 29% two factors, 17% three factors, and 8% all four factors. Women with higher syndemic severity scores were more likely to fear condom negotiation and less likely to negotiate and use condoms (see Table 3). As shown in Figure 1, the direct effect of syndemic severity on condom use was not statistically significant (β = −1.22, SE = 2.11, p = .56, [95% CI: − 5.40, 2.99]). The direct effect of syndemic severity on condom negotiation was significant (β = −8.33, SE = 2.79, p = .003, [95% CI: −13.84, −2.82]). The indirect effect of syndemic severity on condom use through condom negotiation was significant (Effect = − 6.41, SE = 2.13, [95% CI: − 10.71, −2.31]). These findings provide support for the mediating role of condom negotiation in the association between syndemic severity and condom use.
Table 3.
Multivariate and Logistic Regression Models with Syndemic Severity Predicting Fear of Condom Negotiation, Condom Negotiation, and Condom Use
| Independent Variables | Dependent Variables | ||
|---|---|---|---|
| Fear of Negotiation | Condom Negotiation % | Condom Use % | |
| Age | OR = 1.06* (1.01, 1.04) |
β = −0.35 SE = 0.28 |
β = −0.20 SE = 0.33 |
| HIV Status | OR = 1.11 (0.24, 4.98) |
β = 41.50*** SE = 10.93 |
β = 62.84*** SE= 13.16 |
| Child Abuse | OR = 2.55* (1.10, 5.89) |
β = 12.46* SE = 5.76 |
β = 5.72 SE = 6.64 |
| Sexual IPV | OR = 2.27† (0.89, 5.81) |
β = 20.95*** SE = 6.16 |
β = 4.11 SE = 6.99 |
| Syndemic Severity | OR = 1.57* (1.09, 2.27) |
β = −8.51*** SE = 2.58 |
β = −8.26** SE = 2.96 |
Note.
p ≤ .001,
p ≤ .01,
p ≤ .05,
p ≤ .10
Figure 1.
Meditation Analysis: Standardized Regression Coefficients and Indirect Effect for the Associations among Syndemic Severity and Condom Use as Mediated by Condom Negotiation.
Discussion
This study used a syndemic framework to examine the collective effects of problematic drug use, hazardous drinking, depression, and PTSD on fear of condom negotiation, condom negotiation, and condom use among IPV-exposed community women. Our findings extend the literature by demonstrating an association between this syndemic and condom negotiation and use. Further, our results are the first, to our knowledge, to identify condom negotiation as a mechanism through which this syndemic influences condom use, indicating that condom negotiation may be a key target for intervention among this vulnerable population.
Our findings have important implications for the treatment of substance use and psychiatric disorders among IPV-exposed women. Specifically, results underscore the need for interventions that address the comorbidity among substance abuse, depression, and PTSD in this population. Though interventions have been designed to address these co-morbid disorders (Najavits & Hien, 2013), many of these treatments are contraindicated for women currently experiencing IPV (Warshaw, Sullivan, & Rivera, 2013). Other interventions have been developed specifically for IPV-exposed women (Gilbert et al., 2006; Wechsberg, Browne, Ellerson, & Zule, 2010). For instance, Relapse Prevention and Relationship Safety (RPRS) targets sexual risk behavior (including condom negotiation), drug use, depression, and PTSD among IPV-exposed women (Gilbert et al., 2006). Yet, results of a pilot study suggest that, whereas RPRS decreases IPV, drug use, depression, and sex under the influence of drugs, it does not result in significant increases in condom use (Gilbert et al., 2006). Another intervention, the Women’s CoOp, has demonstrated efficacy in reducing unprotected sex, increasing condom negotiation, decreasing violence, and decreasing drug use among high-risk women (Wechsberg, Luseno, Kline, Browne, & Zule, 2010; Wechsberg, Luseno, Lam, Parry, & Morojele, 2006; Wechsberg et al., 2010). However, this intervention does not focus on the reduction of mental health symptoms such as depression and PTSD. Thus, future research is needed develop or modify interventions to reduce co-occurring substance abuse and mental health challenges among women experiencing IPV and increase condom negotiation and use among this population (Warshaw et al., 2013).
Our findings suggest that the collective effects of problematic drug use, hazardous drinking, depression, and PTSD impact condom negotiation and use among IPV-exposed women. IPV-exposed women who experienced a more severe syndemic were more likely to fear negotiating condom use and less likely to negotiate and use condoms compared to women who experienced a less severe syndemic. Future research should explore how IPV-exposed women negotiate condom use in order to better understand the process of condom negotiation within a violent relational context. Specifically, research should attempt to identify safe and effective strategies that women can employ to negotiate condom use in relationships characterized by IPV.
Finally, the current study demonstrated that women who reported experiencing a more severe syndemic were less likely to negotiate condom use, which resulted in a lower percentage of condom use. This finding also supports the inclusion of condom negotiation skills training in interventions targeted toward women experiencing IPV. However, because for some women condom negotiation may result in additional violence (El-Bassel et al., 2005), interventions should assess the real and perceived danger of condom negotiation and work with women individually to decide if and how they can negotiate condom use with their partners. For IPV-exposed women who are able to negotiate condom use, it is important to identify strategies that both facilitate condom use and avoid the threat of violence. Condom negotiation strategies that are less likely to provoke aggression, such as using seductive techniques, may address concerns about safety (Otto-Salaj et al., 2008; Otto-Salaj et al., 2010). Alternatively, women may benefit from women-controlled methods of pregnancy and disease prevention that do not require them to notify their partners, such as pre-exposure prophylaxis (i.e., PrEP) and long-acting reversible contraception (i.e., LARC). Still, for other women, substance abuse or mental health treatment may be the key to facilitating condom use. Indeed, effective condom negotiation may be difficult when a woman is actively using substances (Maisto, Carey, Carey, & Gordon, 2002). It is likely that a combination of condom negotiation skills training and substance abuse and mental health treatment is needed for IPV-exposed women to reduce their sexual risk.
This study fills important gaps in the literature. However, there are some limitations that should be addressed in future research. First, all the women in this study reported experiencing physical and psychological IPV perpetrated by their current partner in the past six months. As a result, there was no variability in regard to women’s experiences of these forms of IPV. Therefore, we could not model various forms of IPV as factors of the syndemic. Second, participants reported on key variables during the past six months. Given the length of the recall period and the risk of social desirability, it is possible that participants overestimated or underestimated the rate and severity of the factors of the syndemic and condom use. However, research suggests that self-reported sexual behavior related to the past six months can be moderately reliable (Saltman, Stoddard, McCusker, Moon, & Mayer, 1987). Third, HIV status was self-reported and may represent an underestimation of the proportion of women with HIV in the sample. Fourth, the current study utilized a small sample of non-clinical IPV-exposed women recruited from a small urban community in the northeast. Therefore, future research should attempt to replicate our findings among a larger, more representative sample in order to generalize these findings to other populations of IPV-exposed women such as those who are actively seeking services. Finally, data used in this study were cross-sectional; therefore, causality cannot be inferred. Future research should utilize longitudinal methodology to assess the temporal relationships of this syndemic and sexual risk.
Despite these limitations, this study has important implications for HIV and STI prevention and intervention programs for IPV-exposed women. First, there is a need to identify IPV-exposed women who experience substance abuse, depression, and/or PTSD, because of their heightened sexual risk. Second, HIV and STI prevention strategies that target IPV-exposed women who experience substance abuse, depression, and/or PTSD should include or enhance condom negotiation skills training to reduce sexual risk. Finally, syndemic theory suggests that disease is not only the manifestation of epidemics that interact, but also the social ties that bring those epidemics together in the first place (Singer & Clair, 2003). Therefore, policymakers and advocates should consider establishing social contexts that are conducive to the sexual health of IPV-exposed women. Social policies to reduce HIV and STIs in this population must address access to substance abuse and mental health services for these women. Research also suggests that substance abuse, IPV, and mental health challenges among IPV-exposed women should be addressed at a community and structural level. Services that indirectly influence their experiences of IPV, substance abuse, and mental health challenges such as affordable housing, job placement, and access to adequate health care (as we have seen with the provisions for IPV-exposed women in the Patient Protection and Affordable Care Act [2010]) may significantly reduce the prevalence and severity this syndemic (El-Bassel, Caldeira, Ruglass, & Gilbert, 2009; El-Bassel, Gilbert, Witte, Wu, & Vinocur, 2010). It is only by addressing both individual and structural determinants of health that we can start to dismantle this syndemic and improve the sexual health of IPV-exposed women.
References
- Ahmed S, Lutalo T, Wawer M, Serwadda D, Sewankambo NK, Nalugoda F, Kigozi G. HIV incidence and sexually transmitted disease prevalence associated with condom use: A population study in Rakia, Uganda. AIDS. 2001;15(16):2171–2179. doi: 10.1097/00002030-200111090-00013. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test: Guidelines for use in primary care. Geneva, Switzerland: World Health Organization Department of Mental Health and Substance Dependence; 2001. (No. WHO/MSD/MSB/01.6a) [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Desmond D. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Manual for the childhood trauma questionnaire: A retrospective self-report. The Psychological Corporation; 1998. [Google Scholar]
- Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among lowincome women experiencing intimate partner violence: The role of posttraumatic stress disorder. AIDS and Behavior. 2010;14(2):318–327. doi: 10.1007/s10461-009-9623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chipman KJ, Palmieri PA, Hobfoll SE. The impact of posttraumatic stress disorder symptoms on women's safer sex negotiation: Influence of ethnicity. Psychological Trauma: Theory, Research, Practice, and Policy. 2011 doi: 10.1037/a0020589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Caldeira NA, Ruglass LM, Gilbert L. Addressing the unique needs of African American women in HIV prevention. American Journal of Public Health. 2009;99:996. doi: 10.2105/AJPH.2008.140541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Chang M, Gomes C, Vinocur D, Spevack T. Intimate partner violence prevalence and HIV risks among women receiving care in emergency departments: Implications for IPV and HIV screening. Emergency Medicine Journal: EMJ. 2007;24(4):255–259. doi: 10.1136/emj.2006.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Witte S, Wu E, Vinocur D. African Americans and HIV/AIDS. Springer; 2010. Countering the surge of HIV/STIs and co-occurring problems of intimate partner violence and drug abuse among African American women: Implications for HIV/STI prevention; pp. 113–130. [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Go H, Hill J. HIV and intimate partner violence among methadone-maintained women in New York City. Social Science & Medicine. 2005;61(1):171–183. doi: 10.1016/j.socscimed.2004.11.035. doi: http://dx.doi.org/10.1016/j.socscimed.2004.11.035. [DOI] [PubMed] [Google Scholar]
- Epperson MW, Platais I, Valera P, Barbieri R, Gilbert L, El-Bassel N. Fear, trust, and negotiating safety HIV risks for Black female defendants. Affilia. 2009;24:257–271. doi: 10.1177/0886109909337377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E. The posttraumatic diagnostic scale (PDS) manual. Minneapolis, MN: National Computer Systems; 1995. [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O'Campo P. HIV/AIDS and intimate partner violence: Intersecting women's health issues in the United States. Trauma, Violence & Abuse. 2007;8(2):178–198. doi: 10.1177/1524838007301476. doi:8/2/178 [pii] [DOI] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Manuel J, Wu E, Go H, Golder S, Sanders G. An integrated relapse prevention and relationship safety intervention for women on methadone: Testing short-term effects on intimate partner violence and substance use. Violence and Victims. 2006;21(5):657–672. [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf. [Google Scholar]
- Koblin BA, Grant S, Frye V, Superak H, Sanchez B, Lucy D, Escamilia G. HIV sexual risk and syndemics among women in three urban areas in the United States: Analysis from HVTN 906. Journal of Urban Health. 2015:1–12. doi: 10.1007/s11524-015-9944-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Gidycz CA, Wisniewski N. The scope of rape: Incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. Journal of Consulting and Clinical Psychology. 1987;55(2):162. doi: 10.1037//0022-006x.55.2.162. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. Journal of Studies on Alcohol. 2002;63(4):476. doi: 10.15288/jsa.2002.63.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: A literature review of the syndemic. Journal of Women's Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM, Hien D. Helping vulnerable populations: A comprehensive review of the treatment outcome literature on substance use disorder and PTSD. Journal of Clinical Psychology. 2013;69(5):433–479. doi: 10.1002/jclp.21980. [DOI] [PubMed] [Google Scholar]
- Otto-Salaj LL, Reed B, Brondino MJ, Gore-Felton C, Kelly JA, Stevenson LY. Condom use negotiation in heterosexual African-American adults: Responses to types of social power-based strategies. Journal of Sex Research. 2008;45(2):150. doi: 10.1080/00224490801987440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otto-Salaj LL, Traxel N, Brondino MJ, Reed B, Gore-Felton C, Kelly JA, Stevenson LY. Reactions of heterosexual African American men to women's condom negotiation strategies. Journal of Sex Research. 2010;47(6):539–551. doi: 10.1080/00224490903216763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peasant C, Parra GR, Okwumabua TM. Condom negotiation: findings and future directions. Journal of Sex Research. 2015;52(4):470–483. doi: 10.1080/00224499.2013.868861. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. Journal of Women's Health. 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Watt MH, Pieterse D. Co-occurring psychosocial problems and HIV risk among women attending drinking venues in a South African township: A syndemic approach. Annals of Behavioral Medicine. 2013;45(2):153–162. doi: 10.1007/s12160-012-9420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente, Juan R, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Singer M, Clair S. Syndemics and public health: Reconceptualizing disease in bio-social context. Medical Anthropology Quarterly. 2003;17(4):423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;28(1):13–24. [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby S, Warren W. The conflict tactics scales handbook: Revised conflict tactics scale (CTS2) and CTS: Parent-child version (CTSPC) Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Sullivan TP, Holt LJ. PTSD symptom clusters are differentially related to substance use among community women exposed to intimate partner violence. Journal of Traumatic Stress. 2008;21(2):173–180. doi: 10.1002/jts.20318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolman RM. The development of a measure of psychological maltreatment of women by their male partners. Violence and Victims. 1989;4(3):159–177. [PubMed] [Google Scholar]
- Warshaw C, Sullivan CM, Rivera EA. A systematic review of trauma-focused interventions for domestic violence survivors. Chicago, IL: National Center on Domestic Violence, Trauma & Mental Health; 2013. [Google Scholar]
- Wechsberg WM, Luseno WK, Kline TL, Browne FA, Zule WA. Preliminary findings of an adapted evidence-based woman-focused HIV intervention on condom use and negotiation among at-risk women in Pretoria, South Africa. Journal of Prevention & Intervention in the Community. 2010;38(2):132–146. doi: 10.1080/10852351003640799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Lam WK, Parry CD, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS and Behavior. 2006;10(2):131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Browne FA, Ellerson RM, Zule WA. Adapting the evidence-based women's CoOp intervention to prevent human immunodeficiency virus infection in North Carolina and international settings. North Carolina Medical Journal. 2010;71(5):477–481. [PMC free article] [PubMed] [Google Scholar]