Abstract
AIM
To evaluate sex differences and the effects of oestrogen administration in rat gastric mucosal defence.
METHODS
Sex differences in gastric mucus thickness and accumulation rate, absolute gastric mucosal blood flow using microspheres, the integrity of the gastric mucosal epithelium in response to a chemical irritant and the effects of oestrogen administration on relative gastric mucosal blood flow in an acute setting was assessed in an in vivo rat experimental model. Subsequently, sex differences in the distribution of oestrogen receptors and calcitonin gene related peptide in the gastric mucosa of animals exposed to oestrogen in the above experiments was evaluated using immunohistochemistry.
RESULTS
The absolute blood flow in the GI-tract was generally higher in males, but only significantly different in the corpus part of the stomach (1.12 ± 0.12 mL/min•g in males and 0.51 ± 0.03 mL/min•g in females) (P = 0.002). After removal of the loosely adherent mucus layer the thickness of the firmly adherent mucus layer in males and females was 79 ± 1 µm and 80 ± 3 µm respectively. After 60 min the mucus thickness increased to 113 ± 3 µm in males and 121 ± 3 µm in females with no statistically significant difference seen between the sexes. Following oestrogen administration (0.1 followed by 1 µg/kg•min), mean blood flow in the gastric mucosa decreased by 31% [68 ± 13 perfusion units (PFU)] in males which was significantly different compared to baseline (P = 0.02). In females however, mean blood flow remained largely unchanged with a 4% (5 ± 33 PFU) reduction. The permeability of the gastric mucosa increased to a higher level in females than in males (P = 0.01) after taurocholate challenge. However, the calculated mean clearance increase did not significantly differ between the sexes [0.1 ± 0.04 to 1.1 ± 0.1 mL/min•100 g in males and 0.4 ± 0.3 to 2.1 ± 0.3 mL/min•100 g in females (P = 0.065)]. There were no significant differences between 17β-Estradiol treated males (mean ratio of positive staining ± SEM) (0.06 ± 0.07) and females (0.11 ± 0.11) in the staining of ERα (P = 0.24). Also, there were no significant differences between 17β-Estradiol treated males (0.18 ± 0.21) and females (0.06 ± 0.12) in the staining of ERβ (P = 0.11). Finally, there were no significant differences between 17β-Estradiol treated males (0.04 ± 0.05) and females (0.11 ± 0.10) in the staining of CGRP (P = 0.14).
CONCLUSION
Gastric mucosal blood flow is higher in male than in female rats and is reduced in male rats by oestrogen administration.
Keywords: Sex differences, Gastric mucosal defence, Blood flow, Oestrogen, Gastric physiology, Mucus
Core tip: We report a sex difference in absolute gastric mucosal blood flow using an in vivo rat experimental model. Male rats had approximately twice as high blood flow in the gastric corpus mucosa compared to females. Moreover, relative gastric mucosal blood flow decreased during oestrogen administration in males but not in females and the permeability of the gastric mucosa increased to a higher level in females than in males after taurocholate challenge. However, mean clearance increase, mucus thickness and accumulation rate and the expression of ERα, ERβ or calcitonin gene related peptide in the gastric mucosa did not differ significantly between the sexes.
INTRODUCTION
There is an unexplained difference between the sexes regarding the incidence of several gastric diseases. For instance, there is a male predominance (2-3:1) in the incidence of gastric adenocarcinoma[1] and a hypothesis that these sex differences could be due to a protective effects of female sex-hormones, mainly oestrogens[2]. Moreover, there is a similar male predominance in the incidence of peptic ulcer disease; although this difference has been declining over time[3] and oestrogens are hypothesised to play a role in the protection against gastro-duodenal injury[4,5].
In light of previous epidemiological and experimental studies we hypothesised that a potentially protective effect of oestrogen would be exerted by influencing the mechanisms of gastric mucosal defence. The gastric mucosal integrity is maintained by several defence mechanisms that can be divided into three levels: A pre-epithelial level (mucus-bicarbonate), the epithelial level including tight junctions and fast cell turnover, and a sub-epithelial level, mainly blood flow[6-10].
We first evaluated basal sex differences in gastric mucosal blood flow, using the microspheres technique. Secondly, we evaluated the effects of oestrogen on relative gastric mucosal blood flow, using Laser Doppler Flowmetry in a unique in vivo experimental model developed in our laboratory[11,12]. Further, gastric mucus thickness and accumulation rate, and the integrity of the gastric mucosal epithelium in response to a challenge with the nonsteroidal anti-inflammatory drug (NSAID) diclofenac and the bile acid taurocholate were studied in the same in vivo animal model. Finally, we evaluated sex differences in the distribution of oestrogen receptors (ERs) and calcitonin gene related peptide (CGRP), an oestrogen sensitive potent vasodilator[13], in the gastric mucosa using immunohistochemistry.
MATERIALS AND METHODS
Animal preparation
All experiments were approved by the Regional Ethical Committee for Laboratory Animal Experiments in Uppsala. The animal protocol was designed to minimise pain or discomfort to the animals. Male and female 9 wk old Sprague-Dawley rats (both sexes are sexually mature at 8-10 wk) (Taconic M&B A/S, Lille Skensved, Denmark) weighing 250-350 g and 180-225 g respectively were kept in standardised conditions of temperature (21-22 °C) and ambient lighting using a 12 h night and day cycle. Rats were allowed to acclimatise in wide cages with a mesh bottom and free access to pelleted food and tap water for at least seven days before the experiments started. Before each experiment they were fasted for 18-20 h with free access to water. To avoid additional stress the animals were handled as little as possible outside their cages and administered 120 mg/kg of thiobutabarbital sodium (Inactin; Sigma-Aldrich, St Louis, Missouri, United States) intraperitoneally to induce anaesthesia before being returned to the cage. After an appropriate length of time the level of anaesthesia was evaluated by the reactions of the eye-lid and foot to tactile and painful stimulus respectively. If anaesthesia was deemed non-sufficient an additional bolus of thiobutabarbital sodium was administered when necessary during the experimental procedure. No opioids or other analgesics were administered to the animals. Core body temperature was kept at 37-38 °C using a heating pad connected to a rectal thermistor. A PE-200 cannula was inserted into the trachea to facilitate spontaneous breathing. After the end of each experiment all animals were euthanised with an intravenous injection of saturated potassium chloride solution.
Measurement of gastric mucosal blood flow using microspheres
Animal preparation specific for this experiment: A PE-50 cannula containing Heparin (Leo Pharma, Malmö, Sweden; 12.5 IU/mL) dissolved in 0.9% saline was inserted into the ascending aorta via the right carotid artery as well as the right and left femoral artery. The mean systemic arterial blood pressure (MAP) was under continuous measurement by connecting the catheter in the right femoral artery to a pressure transducer whereas the catheter in the left femoral artery was connected to a constant rate withdrawal pump. The position of the carotid catheter just below or above the aortic valve for injection of the microspheres was confirmed at autopsy at the end of the experiments.
Absolute blood flow measurements using microspheres - experimental protocol: After stable blood pressure had been established (less than 10% variation during 10 min) approximately 300000 non-radioactive black microspheres with a mean diameter of 15 µm (E-Z Trac Ultraspheres®; IMT, Stason Labs., Irvine, CA, United States), were suspended in 0.15 mL saline containing 0.01% (v/v) Tween 80 and 0.002% (w/v) Thimerosal, sonicated for 5 min and injected through the carotid artery catheter within 10 s. The catheter was then flushed with 0.3 mL saline for 20 s.
The reference blood sample was withdrawn into a Heparin-containing (Leo Pharma, Malmö, Sweden; 5000 IU/mL) syringe at a constant rate of 0.5 mL/min from the catheter in the left femoral artery starting 10 s before the injection of the microspheres and continuing for 60 s after the injection. Blood pressure was continuously monitored to ensure that this procedure did not affect MAP. Thereafter the animals were euthanised and a piece of the right and left kidney, duodenum, colon, antrum and corpus of the stomach were quickly removed, blotted and weighed. In a pilot study (n = 5), muscularis and mucosa/submucosa of stomach and gastrointestinal tract specimens were dissected and analysed separately. In all these experiments, the flow to the muscularis layer was not possible to measure with this technique due to low number of microspheres (≤ 400). The weight and the blood flow of the muscularis were low compared with the mucosa/submucosa. Therefore, a micro-dissection to remove the muscularis from the mucosa/submucosa layer was not performed in subsequent experiments. The specimens were placed on objective glass and subjected to quick freezing in liquid nitrogen before thawing to help visualise the microspheres. The number of microspheres present in the organs was counted in a light microscope. The microsphere content in the arterial blood reference samples was counted in the same manner after transferring the blood to glass microfiber filters. The organ blood flow was calculated according to the formula:
Qorg = (Norg × Qref)/Nref
Where Qorg = organ blood flow (mL/min), Qref = flow of the reference sample (mL/min), Norg = number of microspheres present in the organ and Nref = number of microspheres present in the reference sample. The value was then converted into blood flow in mL/min•g of tissue by dividing the calculated flow above with the total weight of the tissue in grams. The blood flow values calculated from the microsphere content of the kidneys were used to reassert that the microspheres were sufficiently mixed in the circulation. A difference of less than 10% in the blood flow values was taken to indicate adequate mixing. Only animals with adequate mixing were included in the statistical calculations.
Measurement of mucus thickness and accumulation rate
Animal and tissue preparation specific for this experiment: The femoral artery was catheterised with a PE-50 cannula containing Heparin (12.5 IU/mL) dissolved in 0.9% saline and connected to a pressure transducer for continuous measurement of MAP. The femoral vein was cannulated for drug administration and a continuous infusion of a modified Ringer's solution (25 mmol/L NaHCO3, 120 mmol/L NaCl, 2.5 mmol/L KCl and 0.75 mmol/L CaCl2) at a rate of 1 mL per hour.
The gastric preparation for mucus thickness measurements has been described previously in detail[11,14]. In brief, the abdomen was opened through a midline incision and the stomach was exteriorised. The fore-stomach was opened along the greater curvature and the rat was placed on its left side on an in-house built Lucite microscope stage. The corpus of the stomach was everted and draped over a truncated cone with the luminal side up. A mucosal chamber with a hole in the bottom was placed over the stomach, exposing approximately 1.2 cm2 of the mucosal surface and the junction was sealed with silicone grease. The mucosal chamber was filled with un-buffered 0.9% saline (5 mL) and kept at 37-38 °C by warm water perfusing the bottom of the chamber. The saline was changed every 10 min and pH was measured. The animal was allowed to recover for at least 1 h after surgical preparation until systemic blood pressure stabilised.
Mucus thickness measurements - experimental protocol: Mucus thickness and accumulation rate was measured using micropipettes connected to a micromanipulator as described previously in detail[12,14,15]. In brief the epithelial cell surface of the mucus gel was visualised using carbon particles (extra pure activated charcoal; Merck Inc., Darmstadt, Germany). A micropipette was pushed into the mucus gel at an angle (α) of 25-35° to the epithelial surface and the distance (D) travelled by the micropipette from the luminal surface of the mucus gel to the epithelial cell surface was measured by a digimatic indicator (IDC Series 543; Mitutoyo Corp., Tokyo, Japan) connected to the micromanipulator. Mucus gel thickness (T) was calculated using the formula T = D(sin α). A mean value from four or five measurements at different locations was used. Removal of the outer loosely adherent mucus layer was performed by suction with a thin catheter. The inner firmly adherent mucus layer remained and the thickness of this was measured. The accumulation of mucus was studied by measuring the mucus thickness every 20 min for 60 min at which point the loosely adherent mucus layer was removed again and the firmly adherent mucus layer was measured a second time.
Measurements of gastric mucosal blood flow using Laser Doppler Flowmetry before and after oestrogen administration
Animal and tissue preparation specific for this experiment: The preparations in this experiment are identical to those described briefly in section B and in detail elsewhere[11].
Blood flow measurement - laser doppler flowmetry: Laser doppler flowmetry (LDF) (PeriFlux 4001 Master and PeriFlux PF3; PeriMed AB, Stockholm, Sweden) was used to measure gastric mucosal blood flow. The helium neon laser (wavelength 635 nm) was guided to the gastric mucosa by an optical fibre and back-scattered light was detected by a pair of fibres separated by 0.25-0.5 mm. The Doppler shift from an illuminated tissue depends on the velocity and the number of moving red blood cells[16]. The accuracy of the LDF method for gastrointestinal applications has been described previously[17,18]. The laser probe was mounted on a micromanipulator and maintained at a distance of about 0.5 mm from the gastric mucosa in the chamber solution. Because the recorded signal is known to decrease exponentially with distance from the probe and 70% of the total blood flow in the gastric wall is mucosal[6] the recorded signal was considered to be mainly mucosal in origin. Using this technique blood flow was determined as a voltage output and expressed as perfusion units (PFU). Changes in blood flow were expressed as a percentage of baseline values and mean blood flow changes were calculated from the area under the curve during 10 min periods.
Oestrogen administration and experimental protocol: 17β-Estradiol (Sigma Chemical, St Louis, MO, United States) was dissolved in 100% ethanol to form a stock solution which was initially diluted to 2% ethanol in saline with a concentration of 1 mmol/L that could be stored at -20 °C. Subsequently this stock was further diluted to a final concentration of 0.1 mmol/L which was stored at +4 °C without precipitation. On the day of the experiment these solutions were further diluted in phosphate-buffered saline (PBS) to 10 and 1 nmol/L respectively as described by Binko et al[19]. Previous studies have shown that maximal 17β-Estradiol levels achieved in cycling rodents is approximately 0.1 nmol/L[20]. A two-step dose regimen for intravenous administration was then adopted influenced by Philp et al[21]. However, based on the fact that this group only found antiarrhythmic effects in the higher dose regimens and in order to elucidate if any response would be seen at all as well as to reduce the number of animals required we decided to adopt a regimen with a higher starting dose and a steeper dose-response curve corresponding to approximately 30 and 300 times the physiologic serum concentration seen in female rats. This was done using an initial intravenous bolus dose of 1 and 10 µg/kg (0.17 mL) respectively, administered to both intact males and females, followed by a continuous one hour long infusion of first 0.1 (E1) and finally 1 (E2) µg/kg•min (6 and 60 µg/kg•h) at a rate of 1 mL per hour. Moreover, a few pilot experiments confirmed that an initial bolus dose of 0.1 µg/kg followed by a continuous one hour long infusion of 0.01 µg/kg•min (0.6 µg/kg•h), did not cause any significant changes in blood flow (LDF) in either of the sexes (data not shown). Each animal is its own control and all results in this study are thus based on differences in mean changes from the baseline. During the course of the 2 h protocol, MAP and gastric mucosal blood flow were measured continuously.
Data management: Each hour of infusion was divided into six 10 min periods and the changes in MAP and LDF during each period was calculated as a mean value. To compare the different doses of oestrogen a mean value was calculated using the last 30 min (i.e., three 10 min periods) of each infusion period. In one of the female rats the experiment was stopped before the entire last period was finished due to a reduction in blood pressure. In that case the last 10 min period was used as an approximation.
Measurements of gastric mucosal permeability
Animal and tissue preparation specific for this experiment: The preparations in these experiments are identical to those described briefly in section B.
Mucosal permeability: The blood-to-lumen clearance of 51chromium-labeled EDTA (51CrEDTA; DuPont-NEN, Boston, MA) was studied before, during and after a chemical challenge to the gastric mucosa in both male and female rats to evaluate any sex differences in gastric mucosal permeability. These experiments were conducted as described in detail by Petersson et al[22] and presented in Figure 1. In brief, after the animal had been allowed to stabilise after surgery and 60 min before the start of the experiment an intravenous bolus dose of 50-75 µCi 51CrEDTA in Ringer's solution was given followed by an infusion of 10-30 µCi per hour (1 mL per hour) during the entire experimental procedure. At the start of the experiment a blood sample of 0.2 mL was drawn and compensated for by an equal volume of 7% BSA (Sigma-Aldrich Chemie, Steinheim, Germany). Blood samples were also taken at 60 min into the experiment and at 160 min at the end of the experimental protocol. All blood samples were centrifuged and 50 µL of plasma was removed for measurement of radioactivity in counts per minute (cpm). During the experiments the gastric mucosa was covered with 5 mL of isotonic saline or 5 mL of 10 mmol/L HCl. This luminal solution and blood samples were analysed for activity in a gamma counter (1282 Compugamma Cs; Pharmacia, Uppsala, Sweden). Each clearance value was calculated by dividing the luminal cpm value by the corresponding plasma cpm value according to the formula: Lumen sample (cpm/mL) × Sample volume (mL) × 100/Plasma (cpm/mL) × Tissue weight (g) × Time (min). Clearance was calculated in this way every ten minutes during the experiment. If there was a deviation of less than 10% between the three different blood sample counts a mean plasma cpm/mL value was calculated and used for all clearance calculations. If there was a deviation of more than 10% the activity was plotted against time and a straight line was drawn between the two nearest values.
Figure 1.
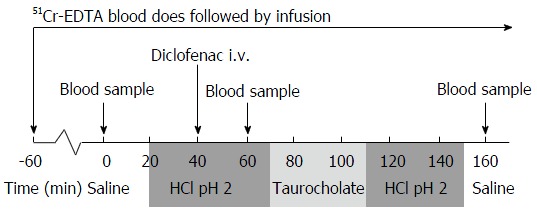
Gastric mucosal permeability; experimental protocol. Time in minutes is given on the X-axis. At -60 (1 h before the start of the experiment but after the animal has been allowed to stabilise after surgery) a bolus dose and a continuous intravenous infusion of 51CrEDTA in Ringer's solution is started. Time 0 marks the start of the experimental procedure. Interventions intravenously are given above the X-axis. Changes in luminal solutions covering the gastric mucosa are given below the X-axis.
Mucosal blood flow: Gastric mucosal blood flow (LDF) and systemic mean arterial pressure were measured and recorded as described under section C only to ensure the stability of the experimental setup. The recorded values were not used in the analysis.
Experimental protocol: The experimental protocol was adapted from Petersson et al[22] (Figure 1). MAP and gastric mucosal blood flow were allowed to remain at steady state for 20-30 min at which point the first blood sample was drawn as described above. Every 10 min during the 160 min of the experimental protocol the 5 mL solution to which the mucosa was exposed to was withdrawn for analysis and instantly replaced. At the start of the experiment the mucosa was exposed to saline for the first 20 min followed by 130 min of 10 mmol/L isotonic HCl and finally to 10 min of saline. Forty minutes into the experiment the COX inhibitor diclofenac (Voltaren; Novartis, Täby, Sweden) was given as an intravenous bolus dose of 5 mg/kg as a "systemic" form of challenge as studies have shown that NSAIDs increase gastric mucosal permeability[23]. Seventy minutes after the start of the experiment the bile salt taurocholate 20 mmol/L (Sigma-Aldrich Chemie) was added to the acidic luminal solution for 40 min as a topical challenge.
In each animal the mean clearance during the last 20 min before the administration of taurocholate was chosen as a control value and the mean clearance during the last 20 min of the taurocholate exposure was chosen as the effect value.
Detection of ERα, ERβ and CGRP in the gastric mucosa by immunohistochemistry
Animal and tissue preparation specific for this experiment: The tissues used in these experiments were collected from the stomachs from all animals that were exposed to oestrogen. The animal and tissue preparation as well as the experimental protocol is given under section C. After each animal was euthanised the stomach was removed and divided into an anterior and posterior half along the greater curvature. One of the halves was fixed in formaldehyde, dehydrated and embedded in 4% wax. Each wax block was cut into 4 µm thick sections and every 10th section was collected, deparaffinized, and rehydrated.
Antibodies: The antibodies used were rabbit polyclonal anti-ERα (MC-20; Santa Cruz Biotechnology), chicken polyclonal anti-ERβ503 (produced at the Department of Biosciences and Nutrition, Karolinska Institutet at Novum Huddinge, Sweden)[24] and rabbit anti-Calcitonin Gene Related Peptide (anti-CGRPC8198) (Sigma). Biotinylated anti-rabbit, anti-chicken antibodies were from Vector Laboratories (Burlingame, CA).
Immunohistochemical staining: Antigens were retrieved by microwave 650 W in 10 mmol/L citrate buffer (pH 7.0) for 15 min. The sections were incubated in 0.5% H2O2 in PBS for 30 min at room temperature to quench endogenous peroxidase, then incubated in 0.5% Triton X-100 in PBS for 15 min. To block the nonspecific binding, sections were incubated in BlockAce (Dai-Nippon Pharmaceutical, Japan) for 40 min at room temperature. Sections were incubated with the following antibodies and dilutions: anti-ERα (1:250), anti-ERβ (1:500) and anti-CGRP (1:5000) in PBS overnight at 4 °C. After washing, sections were incubated with biotinylated corresponding secondary antibodies (all in 1:200 dilutions) for 1 h at room temperature. The Vectastain avidin-biotin complex (ABC) kit (Vector) was used for the ABC method according to the manufacturers' instructions. Peroxidase activity was visualized with 3,3'-diaminobenzidine (DAKO). The sections were mounted on slides and lightly counterstained with haematoxylin. Negative controls were incubated without primary antibody.
Immunohistochemical assessment: Immunohistochemical slides were evaluated by YO, blinded to animal sex status, using light microscopy. A total of 16 male and 6 female rats were investigated after exposure to 17β-Estradiol. As our focus was on the changes in blood flow in the stomach, we hypothesised that endothelial cells would be the most important targets of oestrogen treatment. Therefore, all further assessment was made on the basis of this hypothesis.
All endothelial cells of arteries in the samples were investigated and the number of stained and non-stained cells on the slides was counted. To examine the effects of 17β-Estradiol treatment, the ratio of stained cells to the total number of endothelial cells were calculated and applied to statistical analysis. This was initially done by using proportion scores and intensity scores as described by Allred et al[25]. However, after viewing all the slides the staining intensity in all samples was found to be week (intensity score = 1) or absent (intensity score = 0) and a negligible number of cells showed intermediate staining (intensity score = 2). In the light of this observation the intensity scoring was scrapped and a scoring of either negative (0) or positive (1) staining was adopted and the percentage of staining was calculated as the number of stained cells in one sample divided by the total number of such cells in the sample.
Statistical analysis
All data are expressed as means ± SE. Data was checked for normality using the Shapiro-Wilk test. In microsphere experiments (A) unpaired t-tests with Welch's correction was used for comparisons between groups. Two-way repeated measurements ANOVA with Dunnett's multiple comparisons test were used in mucus and blood flow experiments (B&C). Both paired (before and after challenge) and unpaired (between the sexes) t-tests were used in permeability experiments (D). Unpaired t-test was used in immunohistochemistry experiments (E). All tests were two-tailed and a P value of < 0.05 was considered statistically significant. GraphPad Prism version 6.00 for Windows, GraphPad Software, San Diego, CA, United States was used for statistical calculations.
RESULTS
Gastric mucosal blood flow using microspheres
The absolute blood flow in the GI-tract was generally higher in males than in females, but only significantly different in the corpus part of the stomach [1.12 ± 0.12 mL/min•g in males (n = 8) and 0.51 ± 0.03 mL/min•g in females (n = 5)] (P = 0.002) (Figure 2).
Figure 2.
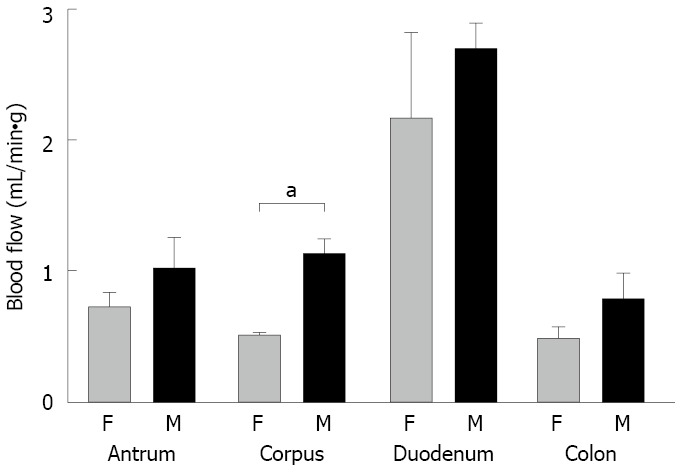
Absolute blood flow in the GI-tract of the rat. Absolute (means ± SE) blood flow (mL/min•g) in the GI-tract of male (M) (n = 32 for all experiments) and female (F) (n = 24 for all experiments) animals, measured with the microspheres technique. The absolute blood flow in the GI-tract was generally higher in males, but only significantly different (a) in the corpus part of the stomach.
Mucus thickness and accumulation rate
After removal of the loosely adherent mucus layer the thickness of the firmly adherent mucus layer in males and females was 79 ± 1 µm (n = 11) and 80 ± 3 µm (n = 8) respectively. After 60 min the mucus thickness increased to 113 ± 3 µm in males and 121 ± 3 µm in females with no statistically significant difference seen between the sexes (P = 0.12). After a second removal of the loosely adherent mucus layer the thickness of the firmly adherent layer was 80 ± 1 µm in males and 78 ± 4 µm in females indicating that the increase in mucus thickness was due to accumulation of loosely adherent mucus (Figure 3).
Figure 3.
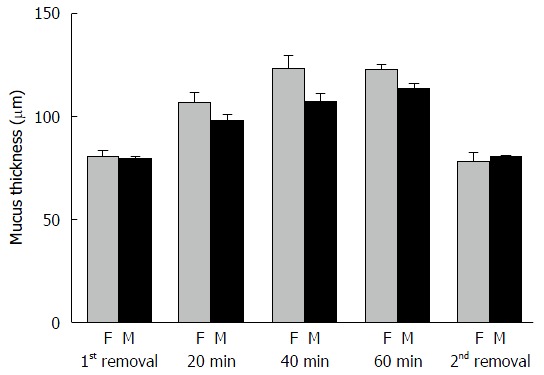
Mucus thickness and accumulation rate. Mucus thickness and accumulation rate (means ± SE) in male (M) (n = 8) and female (F) (n = 11) animals. Time in minutes is given on the X-axis. 1st removal marks the mucus thickness of the firmly adherent mucus layer after removal of the loosely adherent mucus layer at the start of the experiment. Subsequent time periods show the accumulation rate of the loosely adherent mucus layer which is again removed at the second removal.
Gastric mucosal blood flow before and after oestrogen administration
Following oestrogen administration (0.1 followed by 1 µg/kg•min), mean blood flow in the gastric mucosa decreased by 31% (68 ± 13 PFU) in males (n = 7) which was significantly different compared to baseline (P = 0.02). In females (n = 5) however, blood flow remained largely unchanged with a 4% (5 ± 33 PFU) decrease. MAP remained unchanged during the experimental protocol with no significant changes either within each group or between the sexes (Figure 4).
Figure 4.
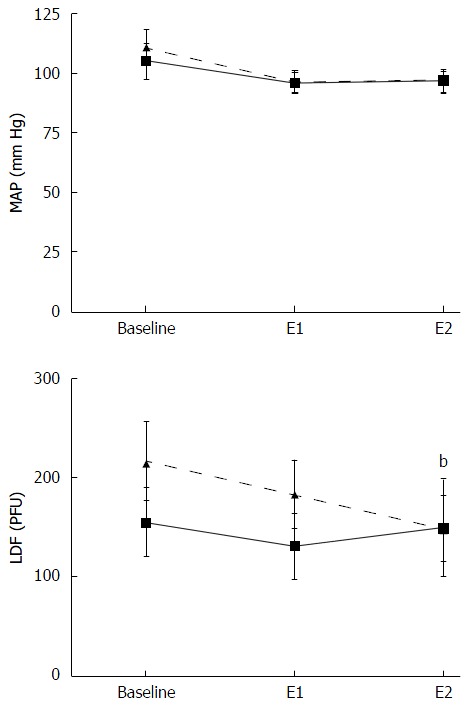
Gastric mucosal blood flow before and after oestrogen administration. Gastric mucosal blood flow [laser doppler flow (LDF)] presented as perfusion units (PFU) and mean arterial pressure (MAP) in male (dashed line) and female (solid line) animals. The X-axis shows values at baseline and following oestrogen administration at 0.1 µg/kg•min (E1) as well as 1 µg/kg•min (E2) respectively. Mean blood flow in the gastric mucosa decreased by 31% (68 ± 13 PFU) in males (n = 7) which was significantly different compared to baseline (b).
Gastric mucosal permeability
No effect on clearance was seen after an intravenous bolus dose of diclofenac (data not shown). The calculated mean clearance increased from 0.1 ± 0.04 to 1.1 ± 0.1 mL/min•100 g (P = 0.01) in males (n = 6) and from 0.4 ± 0.3 to 2.1 ± 0.3 mL/min•100 g (P = 0.001) in females (n = 6). There was no statistical significance between the sexes at baseline (P = 0.2). The absolute permeability of the gastric mucosa was greater after taurocholate challenge in females compared to males (P = 0.01). However, the difference in mean clearance increase between the sexes did not reach significance (P = 0.065) (Figure 5A and B). This increase in permeability was completely reversible to 0.1 ± 0.07 mL/min•100 g in males and 0.6 ± 0.2 mL/min•100 g in females within 60 min of removal of taurocholate.
Figure 5.
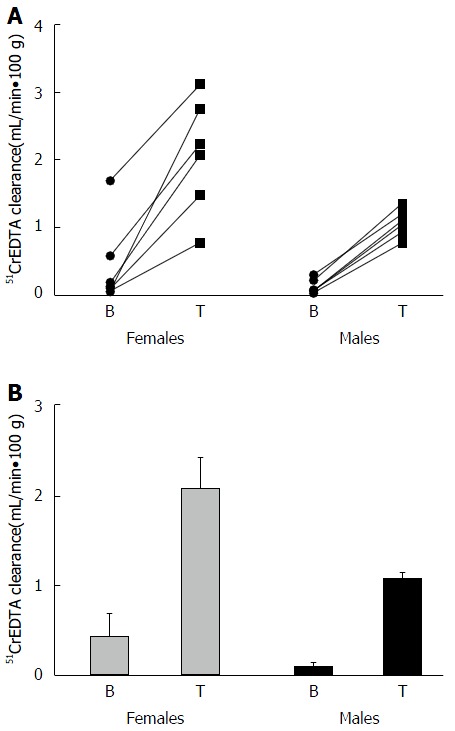
Difference in mean clearance increase between the sexes did not reach significance. A: Absolute clearance increase. Absolute 51CrEDTA clearance increase (mL/min•100 g) in female (n = 6) and male (n = 6) animals from baseline (B) to after exposure to an NSAID and Taurocholate (T) challenge. B: Calculated mean clearance increase. Calculated mean ± SE 51CrEDTA clearance increase (mL/min•100 g) in female (n = 6) and male (n = 6) animals from baseline (B) to after exposure to an NSAID and Taurocholate (T) challenge. NSAID: Nonsteroidal anti-inflammatory drug.
ERα, ERβ and CGRP in the gastric mucosa
The ratio of positive staining was calculated in every sample and applied to the statistical analysis. Table 1 shows immunostaining of ERα, ERβ and CGRP in endothelial cells of the stomach wall. Values are calculated as mean ratios of positive staining ± SE.
Table 1.
Immunostaining of oestrogen receptors and calcitonin gene related peptide
| Male (n = 16) | Female (n = 6) | P value | |
| ERα | 0.06 ± 0.07 | 0.11 ± 0.11 | 0.24 |
| ERβ | 0.18 ± 0.21 | 0.06 ± 0.12 | 0.11 |
| CGRP | 0.04 ± 0.05 | 0.11 ± 0.10 | 0.14 |
Immunostaining of ERα, ERβ and CGRP in endothelial cells of the stomach wall expressed as mean ratios ± SE of positive staining. CGRP: Calcitonin gene related peptide; ERs: Oestrogen receptors.
Staining for ERα after exposure to oestrogen could be observed in gastric epithelial cells, glandular cells (both chief cells and parietal cells), infiltrating cells, myenteric neurons near the serosa in the outer longitudinal muscle of the muscularis and in endothelial cells of blood vessels. The staining (proportion of stained cells in relation to the total number of observable cells) of ERα in endothelial cells was low and the intensity was weak. There were no significant differences between 17β-Estradiol treated males and females in the staining of ERα (P = 0.24).
Staining for ERβ was seen in chief cells, at the base of the gastric glands, infiltrating cells, adipocytes and in endothelial cells of blood vessels. The staining of ERβ was seen in a larger number of endothelial cells and of a greater intensity than for ERα. There were no significant differences between 17β-Estradiol treated males and females in the staining of ERβ (P = 0.11).
CGRP staining was present in gastric glands, infiltrating cells, myenteric neurons of the muscularis and in endothelial cells of blood vessels. CGRP staining in endothelial cells was less than for ERα and ERβ. There were no significant differences between 17β-Estradiol treated males and females in the staining of CGRP (P =0.14) (Figure 6).
Figure 6.
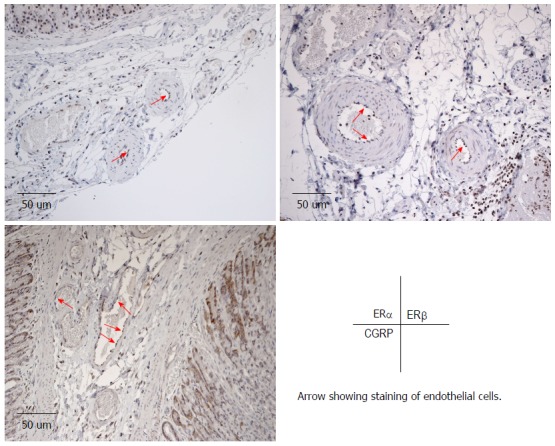
Immunostaining of ERα, ERβ and calcitonin gene related peptide in the male rat stomach. Haematoxylin-stained slides depicting arteries in the male rat stomach. Arrows indicate immunostaining of ERα (top left), ERβ (top right) and CGRP (bottom left) in the endothelium after exposure to oestrogen. Immunostaining is also visible in many other cell-types surrounding the blood vessels. CGRP: Calcitonin gene related peptide.
DISCUSSION
The main finding in this experimental study of the rat is that there was a difference in the gastric mucosal blood flow between the sexes. The absolute blood flow in the corpus of the stomach was substantially lower in female than in male rats and during oestrogen administration the gastric mucosal blood flow decreased in males but not in females. Moreover, the permeability of the mucosal epithelial barrier was significantly higher in females than in males after exposure to a combination of an NSAID and bile acid. There were no sex differences regarding mucus thickness and accumulation rate. Also, there were no sex differences in the expression of endothelial ERα, ERβ or CGRP in the stomach.
To our knowledge a sex difference in absolute gastric mucosal blood flow has not been previously reported. Since a higher blood flow has been suggested to protect the gastric mucosa[26,27] and females have a lower incidence of several gastric diseases such as adenocarcinoma, our hypothesis was that gastric mucosal blood flow would be higher in females than in males. However, there are several other studies in both humans and animals, which demonstrate similar sex differences in blood flow albeit not in the gastric mucosa. In a clinical study by Cooke et al[28] it was shown that skin blood flow as well as blood flow in the hands and fingers of females were significantly lower than in males. In another study in dogs, Pontari et al[29] demonstrated that mucosal blood flow in the bladder was significantly lower in females than in males.
Oestrogen has been shown to cause activation of endothelial nitric oxide synthase (eNOS) leading to production of NO, local vasodilation and an increase in blood flow through non-genomic (within seconds to minutes) stimulation of primarily membrane-bound ERα - but also ERβ receptors as well as through direct effects that are independent of the endothelium and ERs[30]. Therefore, the finding that oestrogen decreased relative gastric mucosal blood flow in males was unexpected. However, in light of our own results that absolute gastric mucosal blood flow is lower in female than in male rats, it is not at all that surprising. In humans oestrogen was seen to induce vasodilation in a major artery in females but not in males, concluding that there may be gender differences in the effects of oestrogen therapy on endothelial functions and NO production/release[31]. Oestrogen has been shown to increase levels of CGRP in sensory nerve-endings leading to increased blood flow through endothelial production of NO, COX-1 and prostacyclin which in turn inhibits neutrophil activation reducing inflammatory response[32]. Although these factors explain in part why females are more resistant to gastric mucosal injury they do not explain the mechanisms behind lower gastric mucosal blood flow in females at baseline or the decrease in blood flow in males during oestrogen administration. Further research to elucidate these mechanisms is warranted.
We did not observe any changes in gastric mucosal blood flow during 17β-Estradiol administration in females. This response agrees with a previous study by Zhang et al[33] in which blood flow was measured using the H2-gas clearance technique and a much lower dose of oestrogen was used. Of interest from that study is also that the gastric mucosal blood flow level recorded in the corpus part of the stomach is virtually identical to our absolute values in females recorded using the microsphere method.
The differences found here between males and females in absolute values of gastric mucosal blood flow, as well as the influence of oestrogen cannot be explained by differences in the conductions of the experiments. The male and female animals were subject to the exact same protocols and experiments were carried out interchangeably between the sexes overall during the same period of calendar time minimising the influence of different batches of animals or seasonal variations. The reason to why we chose not to perform bilateral ovariectomy, which is conducted in most other studies of this nature, was that our aim was to study the response in the intact animal with a normal and preserved oestrogen cycle. One limitation is that we did not measure in which phase of the oestrous cycle the female animal was before the start of the experiment. This could potentially affect the response to exogenous oestrogen administration. However, since the dose of oestrogen administered should result in between 30 and 300 times the normal physiological serum concentration the impact of the oestrous phase in these animals should be minimal.
After exposure to a combination of NSAID and bile acid, not resulting in permanent damage, the permeability of the gastric mucosa was significantly higher in females than in males. Moreover, the basal clearance levels agree with earlier results in male rats presented by our laboratory[22]. The finding of a difference in gastric permeability between the sexes during challenge of the mucosa point to a greater ability in females to increase removal of potentially toxic substances from the gastric mucosa. However, since this method can only evaluate clearance from blood to lumen and not from the lumen to the cell surface we cannot draw any conclusions about sex differences in the function of the mucosal epithelial barrier.
Our measurements of mucus thickness and accumulation rate are in accordance with previous work by Atuma et al[12] in which, however, only male rats were investigated. To our knowledge sex differences in mucus thickness and accumulation rate as well as the integrity of the mucosal epithelial barrier after exposure to NSAID and bile acid have not been previously evaluated. Even though we did not observe any basal physiological sex differences in mucus thickness and accumulation rate the effects of sex hormones on gastric mucosal pathology and especially drug-induced damage and ulcer healing have been extensively studied with a tendency to sex dependent results. A study in female rats demonstrated that 17β-Estradiol aggravated ulcer healing[34] whereas another study in male rats presented conflicting results showing an attenuating effect of both progesterone and oestrogen on drug-induced gastric damage[35].
Oestrogen acts on intracellular ERs that regulate gene expression and are found in both cancerous and non-cancerous gastric tissue, although their purpose is not fully understood[36]. We did not find any differences in ER or CGRP receptor expression between the sexes. However, oestrogen effects could still be dissimilar without any differences in receptor expression why further analysis on this matter is warranted.
We found a sex difference in absolute gastric mucosal blood flow not previously reported. Male rats had approximately twice as high blood flow in the gastric corpus mucosa compared to females and the blood flow decreased during oestrogen administration in males but not in females. The significance and mechanisms of these findings need to be further elucidated. The observed lack of sex differences regarding the properties and integrity of the mucosal epithelial barrier and the distribution of ERα, ERβ or CGRP in this study are tentative and warrant further investigation. Thus, our results do not explain why human females seem to be protected against gastric diseases such as peptic ulcer disease and adenocarcinoma, but increase our knowledge of sex differences in basic gastric mucosal physiology in the rat.
ACKNOWLEDGMENTS
The authors sincerely express their gratitude to Annika Jägare for her expertise and technical assistance.
COMMENTS
Background
There is a male predominance in the incidence of gastric diseases such as adenocarcinoma (2-3:1) unexplained by sex differences in the prevalence of known risk factors. This implies a basic physiological difference between the sexes and supports the hypothesis that sex differences in the incidence of several gastric diseases could be due to a protective effect of female sex hormones, mainly oestrogens. The authors therefore hypothesised that a potentially protective effect of oestrogen would be exerted by influencing the mechanisms of gastric mucosal defence.
Research frontiers
The relationship between gastric disease, oestrogen and gastric mucosal defence has been suggested in a number of epidemiological and experimental studies. However, the mechanisms of these interactions need to be further elucidated.
Innovations and breakthroughs
The authors found a sex difference in absolute gastric mucosal blood flow of the rat not previously reported. Male rats had approximately twice as high blood flow in the gastric corpus mucosa compared to females and the blood flow decreased during oestrogen administration in males but not in females.
Applications
These results do not explain why human females seem to be protected against gastric diseases such as adenocarcinoma, but increase our knowledge of sex differences in basic gastric mucosal physiology in the rat. The significance and mechanisms of our findings need to be further elucidated.
Terminology
Gastric mucosal defence refers to pre-epithelial (the mucus-bicarbonate barrier), epithelial and sub-epithelial (mucosal blood flow) mechanisms, which protect the stomach against hydrochloric acid and potentially noxious agents.
Peer-review
The paper is interesting but has a major problem. In the introduction and conclusions the authors made extensive references to gastric cancer and hypothesized that a potentially protective effect of estrogen could be exerted by influencing the mechanisms of gastric mucosal defense including blood flow. Since they did not study gastric cancer model in rat (e.g., nitrosoguanidine-induced gastric cancer in rats) nor the effect of estrogens in this model they could not test their hypothesis.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Sweden
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: This study was reviewed and approved by the Regional Ethical Committee for Laboratory Animal Experiments in Uppsala.
Institutional animal care and use committee statement: All procedures involving animals were reviewed and approved by the Regional Ethical Committee for Laboratory Animal Experiments in Uppsala (IACUC protocol number: C288/9).
Conflict-of-interest statement: There are no conflicts of interest.
Data sharing statement: No additional data are available.
Peer-review started: July 1, 2016
First decision: August 8, 2016
Article in press: October 19, 2016
P- Reviewer: Ahluwalia A, Garcia-Olmo D S- Editor: Qi Y L- Editor: A E- Editor: Liu WX
References
- 1.Rutegård M, Shore R, Lu Y, Lagergren P, Lindblad M. Sex differences in the incidence of gastrointestinal adenocarcinoma in Sweden 1970-2006. Eur J Cancer. 2010;46:1093–1100. doi: 10.1016/j.ejca.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Sipponen P, Correa P. Delayed rise in incidence of gastric cancer in females results in unique sex ratio (M/F) pattern: etiologic hypothesis. Gastric Cancer. 2002;5:213–219. doi: 10.1007/s101200200037. [DOI] [PubMed] [Google Scholar]
- 3.Lin KJ, García Rodríguez LA, Hernández-Díaz S. Systematic review of peptic ulcer disease incidence rates: do studies without validation provide reliable estimates? Pharmacoepidemiol Drug Saf. 2011;20:718–728. doi: 10.1002/pds.2153. [DOI] [PubMed] [Google Scholar]
- 4.Shimozawa N, Okajima K, Harada N. Estrogen and isoflavone attenuate stress-induced gastric mucosal injury by inhibiting decreases in gastric tissue levels of CGRP in ovariectomized rats. Am J Physiol Gastrointest Liver Physiol. 2007;292:G615–G619. doi: 10.1152/ajpgi.00117.2006. [DOI] [PubMed] [Google Scholar]
- 5.Smith A, Contreras C, Ko KH, Chow J, Dong X, Tuo B, Zhang HH, Chen DB, Dong H. Gender-specific protection of estrogen against gastric acid-induced duodenal injury: stimulation of duodenal mucosal bicarbonate secretion. Endocrinology. 2008;149:4554–4566. doi: 10.1210/en.2007-1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granger DN, Holm L, Kvietys P. The Gastrointestinal Circulation: Physiology and Pathophysiology. Compr Physiol. 2015;5:1541–1583. doi: 10.1002/cphy.c150007. [DOI] [PubMed] [Google Scholar]
- 7.Henriksnäs J, Phillipson M, Storm M, Engstrand L, Soleimani M, Holm L. Impaired mucus-bicarbonate barrier in Helicobacter pylori-infected mice. Am J Physiol Gastrointest Liver Physiol. 2006;291:G396–G403. doi: 10.1152/ajpgi.00017.2006. [DOI] [PubMed] [Google Scholar]
- 8.Henriksnäs J, Atuma C, Phillipson M, Sandler S, Engstrand L, Holm L. Acute effects of Helicobacter pylori extracts on gastric mucosal blood flow in the mouse. World J Gastroenterol. 2009;15:219–225. doi: 10.3748/wjg.15.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laine L, Takeuchi K, Tarnawski A. Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology. 2008;135:41–60. doi: 10.1053/j.gastro.2008.05.030. [DOI] [PubMed] [Google Scholar]
- 10.Tarnawski AS, Ahluwalia A, Jones MK. Increased susceptibility of aging gastric mucosa to injury: the mechanisms and clinical implications. World J Gastroenterol. 2014;20:4467–4482. doi: 10.3748/wjg.v20.i16.4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holm-Rutili L, Obrink KJ. Rat gastric mucosal microcirculation in vivo. Am J Physiol. 1985;248:G741–G746. doi: 10.1152/ajpgi.1985.248.6.G741. [DOI] [PubMed] [Google Scholar]
- 12.Atuma C, Strugala V, Allen A, Holm L. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 2001;280:G922–G929. doi: 10.1152/ajpgi.2001.280.5.G922. [DOI] [PubMed] [Google Scholar]
- 13.Gangula PR, Lanlua P, Wimalawansa S, Supowit S, DiPette D, Yallampalli C. Regulation of calcitonin gene-related peptide expression in dorsal root ganglia of rats by female sex steroid hormones. Biol Reprod. 2000;62:1033–1039. doi: 10.1095/biolreprod62.4.1033. [DOI] [PubMed] [Google Scholar]
- 14.Holm L, Phillipson M. Assessment of mucus thickness and production in situ. Methods Mol Biol. 2012;842:217–227. doi: 10.1007/978-1-61779-513-8_12. [DOI] [PubMed] [Google Scholar]
- 15.Phillipson M, Johansson ME, Henriksnäs J, Petersson J, Gendler SJ, Sandler S, Persson AE, Hansson GC, Holm L. The gastric mucus layers: constituents and regulation of accumulation. Am J Physiol Gastrointest Liver Physiol. 2008;295:G806–G812. doi: 10.1152/ajpgi.90252.2008. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson GE, Tenland T, Oberg PA. Evaluation of a laser Doppler flowmeter for measurement of tissue blood flow. IEEE Trans Biomed Eng. 1980;27:597–604. doi: 10.1109/TBME.1980.326582. [DOI] [PubMed] [Google Scholar]
- 17.Holm-Rutili L, Berglindh T. Pentagastrin and gastric mucosal blood flow. Am J Physiol. 1986;250:G575–G580. doi: 10.1152/ajpgi.1986.250.5.G575. [DOI] [PubMed] [Google Scholar]
- 18.Kvietys PR, Shepherd AP, Granger DN. Laser-Doppler, H2 clearance, and microsphere estimates of mucosal blood flow. Am J Physiol. 1985;249:G221–G227. doi: 10.1152/ajpgi.1985.249.2.G221. [DOI] [PubMed] [Google Scholar]
- 19.Binko J, Majewski H. 17 beta-Estradiol reduces vasoconstriction in endothelium-denuded rat aortas through inducible NOS. Am J Physiol. 1998;274:H853–H859. doi: 10.1152/ajpheart.1998.274.3.H853. [DOI] [PubMed] [Google Scholar]
- 20.Warner M, Gustafsson JA. Nongenomic effects of estrogen: why all the uncertainty? Steroids. 2006;71:91–95. doi: 10.1016/j.steroids.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Philp KL, Hussain M, Byrne NF, Diver MJ, Hart G, Coker SJ. Greater antiarrhythmic activity of acute 17beta-estradiol in female than male anaesthetized rats: correlation with Ca2+ channel blockade. Br J Pharmacol. 2006;149:233–242. doi: 10.1038/sj.bjp.0706850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petersson J, Phillipson M, Jansson EA, Patzak A, Lundberg JO, Holm L. Dietary nitrate increases gastric mucosal blood flow and mucosal defense. Am J Physiol Gastrointest Liver Physiol. 2007;292:G718–G724. doi: 10.1152/ajpgi.00435.2006. [DOI] [PubMed] [Google Scholar]
- 23.Davies NM. Review article: non-steroidal anti-inflammatory drug-induced gastrointestinal permeability. Aliment Pharmacol Ther. 1998;12:303–320. doi: 10.1046/j.1365-2036.1998.00300.x. [DOI] [PubMed] [Google Scholar]
- 24.Saji S, Jensen EV, Nilsson S, Rylander T, Warner M, Gustafsson JA. Estrogen receptors alpha and beta in the rodent mammary gland. Proc Natl Acad Sci USA. 2000;97:337–342. doi: 10.1073/pnas.97.1.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allred DC, Clark GM, Elledge R, Fuqua SA, Brown RW, Chamness GC, Osborne CK, McGuire WL. Association of p53 protein expression with tumor cell proliferation rate and clinical outcome in node-negative breast cancer. J Natl Cancer Inst. 1993;85:200–206. doi: 10.1093/jnci/85.3.200. [DOI] [PubMed] [Google Scholar]
- 26.Leung FW, Itoh M, Hirabayashi K, Guth PH. Role of blood flow in gastric and duodenal mucosal injury in the rat. Gastroenterology. 1985;88:281–289. doi: 10.1016/s0016-5085(85)80181-5. [DOI] [PubMed] [Google Scholar]
- 27.Sørbye H, Svanes K. The role of blood flow in gastric mucosal defence, damage and healing. Dig Dis. 1994;12:305–317. doi: 10.1159/000171465. [DOI] [PubMed] [Google Scholar]
- 28.Cooke JP, Creager MA, Osmundson PJ, Shepherd JT. Sex differences in control of cutaneous blood flow. Circulation. 1990;82:1607–1615. doi: 10.1161/01.cir.82.5.1607. [DOI] [PubMed] [Google Scholar]
- 29.Pontari MA, Ruggieri MR. Sex differences and role of nitric oxide in blood flow of canine urinary bladder. Am J Physiol. 1999;276:R407–R413. doi: 10.1152/ajpregu.1999.276.2.R407. [DOI] [PubMed] [Google Scholar]
- 30.Huang A, Kaley G. Gender-specific regulation of cardiovascular function: estrogen as key player. Microcirculation. 2004;11:9–38. doi: 10.1080/10739680490266162. [DOI] [PubMed] [Google Scholar]
- 31.Kawano H, Motoyama T, Kugiyama K, Hirashima O, Ohgushi M, Fujii H, Ogawa H, Yasue H. Gender difference in improvement of endothelium-dependent vasodilation after estrogen supplementation. J Am Coll Cardiol. 1997;30:914–919. doi: 10.1016/s0735-1097(97)00234-9. [DOI] [PubMed] [Google Scholar]
- 32.Ham M, Kaunitz JD. Gastroduodenal defense. Curr Opin Gastroenterol. 2007;23:607–616. doi: 10.1097/MOG.0b013e3282f02607. [DOI] [PubMed] [Google Scholar]
- 33.Zhang RS, Guth PH, Scremin OU, Chaudhuri G. H2 gas clearance technique for separating rat uterine blood flow into endometrial and myometrial components. Am J Physiol. 1995;268:R569–R575. doi: 10.1152/ajpregu.1995.268.2.R569. [DOI] [PubMed] [Google Scholar]
- 34.Drago F, Montoneri C, Varga C, Làszlò F. Dual effect of female sex steroids on drug-induced gastroduodenal ulcers in the rat. Life Sci. 1999;64:2341–2350. doi: 10.1016/s0024-3205(99)00187-3. [DOI] [PubMed] [Google Scholar]
- 35.Aguwa CN. Effects of exogenous administration of female sex hormones on gastric secretion and ulcer formation in the rat. Eur J Pharmacol. 1984;104:79–84. doi: 10.1016/0014-2999(84)90371-6. [DOI] [PubMed] [Google Scholar]
- 36.Zhao XH, Gu SZ, Liu SX, Pan BR. Expression of estrogen receptor and estrogen receptor messenger RNA in gastric carcinoma tissues. World J Gastroenterol. 2003;9:665–669. doi: 10.3748/wjg.v9.i4.665. [DOI] [PMC free article] [PubMed] [Google Scholar]


