Abstract
Bacillus anthracis is reported to be naturally resistant to trimethoprim (TMP), a drug that inhibits dihydrofolate reductase (DHFR), a key enzyme in the folate pathway. A microdilution broth assay established that the MIC of TMP for B. anthracis Sterne is >2,048 but ≤4,096 μg/ml. A putative DHFR sequence was amplified from B. anthracis Sterne genomic DNA. The PCR product was cloned into the Invitrogen pCRT7/CT-TOPO vector, followed by transformation into Escherichia coli TOP10F′ chemically competent cells. Plasmid DNA from a clone showing the correct construct with a thrombin cleavage site attached downstream from the terminus of the cloned PCR product was transformed into E. coli BL21 Star (DE3)pLysS competent cells for expression of the six-histidine-tagged fusion protein and purification on a His-Bind resin column. Functionality of the purified Sterne recombinant DHFR (Sterne rDHFR) was confirmed in an established enzyme assay. The 50% inhibitory concentrations of TMP and methotrexate for the Sterne rDHFR were found to be 77,233 and 12.2 nM, respectively. TMP resistance was observed with E. coli BL21 Star (DE3)pLysS competent cells transformed with the Sterne DHFR gene. Alignment of the amino acid sequence of the Sterne DHFR gene revealed 100% homology with various virulent strains of B. anthracis. These results confirm the natural resistance of B. anthracis to TMP and clarify that the resistance is correlated to a lack of selectivity for the chromosomally encoded gene product. These findings will assist in the development of narrow-spectrum antimicrobial agents for treatment of anthrax.
With the increased threat of bioterrorism, it is apparent that the development of new and/or improved antimicrobial agents is a critical and logical response to the hazards that could result from an attack with biological agents. It is important to develop new therapeutics in such a way as to expedite clinical trials and subsequent availability for biodefense. One biological weapon that poses a major threat is the spore-forming gram-positive bacterium Bacillus anthracis, the etiological agent of anthrax.
One of the priorities of the National Institute of Allergy and Infectious Diseases division of the National Institutes of Health (NIH) is the design, development, and testing of products specific to category A to C priority pathogens. Bacillus anthracis is on the list of category A priority pathogens. One of the objectives of NIH is to develop narrow-spectrum antimicrobial agents for use in the treatment of anthrax.
At this time, three types of antibiotics are approved for treatment of anthrax, ciprofloxacin (a quinolone), tetracyclines (including doxycycline), and penicillins (14). Increasing resistance to quinolones and macrolides can develop in B. anthracis (3), and doxycycline-resistant strains of B. anthacis have been genetically engineered (25). Penicillin-resistant strains have also been identified (4, 6, 18). Some of these strains were negative for beta-lactamase production (6), whereas some were not (18). Two antimicrobial agents generally used in combination that are not recommended at this time are trimethoprim (TMP) and sulfamethoxazole (14). The justification for this appears to have resulted from findings reported in a 1991 article that described the antibiotic sensitivity patterns of B. anthracis strains that were isolated from the Kruger National Park in South Africa (20). In that report, 44 B. anthracis isolates from animal carcasses and soil in various locations of an area where anthrax is endemic were tested for susceptibility to 18 different antibiotics (20). Using a standard disk diffusion method, the team observed resistance to TMP and sulfamethoxazole in 100% of the isolates (20). Resistance to TMP-sulfamethoxazole has been reported in at least one other study involving B. anthracis isolated from cutaneous anthrax cases in an area of Turkey where anthrax is endemic (2). Trimethoprim and sulfamethoxazole are antimicrobial agents that inhibit dihydrofolate reductase (DHFR) and dihydropteroate synthase, respectively, two key enzymes in the folate biosynthetic pathway that generates cofactors necessary for continued DNA and RNA synthesis.
The objectives of this study were to (i) verify the TMP resistance identified in the previous study for B. anthracis, (ii) clone and express the chromosomally encoded DHFR gene from the B. anthracis Sterne strain, (iii) confirm its functionality in an appropriate enzyme assay, and (iv) verify its resistance to TMP. With that information and the recombinant enzyme, it would then be possible to establish effective drug screening that could be used to search for effective DHFR inhibitors. The ultimate aim of this work is to exploit the natural resistance pattern in B. anthracis and use it to develop narrow-spectrum antibiotics for treatment of anthrax.
(Part of this research was presented at the American Society for Microbiology Biodefense Research Meeting in March 2004 [abstract 165].)
MATERIALS AND METHODS
In vitro drug susceptibility.
Using commercially available disks (Sensi-Disk; Becton Dickinson), B. anthracis Sterne, and Escherichia coli (ATCC 25922; positive control) were screened against trimethoprim (TMP) (5 μg), sulfamethoxazole-trimethoprim (SXT) (23.75 μg of sulfamethoxazole and 1.25 μg of trimethoprim), and sulfisoxazole (250 μg). The screening results indicated that B. anthracis Sterne strain was resistant to TMP (5 μg), resistant to SXT, and sensitive to sulfisoxazole. E. coli zones were the appropriate size and fell within NCCLS guidelines (data not shown).
Subsequently, the MIC of TMP for B. anthracis Sterne was determined by an AlamarBlue microdilution broth assay modified from a previously described method (26). Ninety-six-well microtiter panels of test compounds and control antimicrobial agents were prepared according to the NCCLS broth microdilution reference method in cation-adjusted Mueller-Hinton broth (CAMHB) (Becton Dickinson) containing 10% AlamarBlue dye reagent (TREK Diagnostic Systems) (19).
B. anthracis Sterne was subcultured twice on Trypticase soy agar (TSA) plates containing 5% sheep blood (Hardy Diagnostics). Cultures were incubated at 35°C overnight. Bacteria were transferred to 5 ml of sterile saline and suspended to a turbidity of a 0.5 McFarland standard. From the suspension, a 1:20 dilution was made in CAMHB, and 10 μl was inoculated into each test well in a 96-well plate (19). Microdilution panels were then placed into a gas-diffusible polypropylene bag in ambient air at 35°C for 16 to 20 h. The number of CFU in the final inoculum was verified by inoculating appropriate dilutions onto TSA blood agar plates and counting the colonies. The final inoculum was approximately 7.5 × 105 CFU/ml or 7.5 × 104 CFU/100-μl well, as suggested by NCCLS (19). Quality control bacterial strains were tested against antimicrobial agents for which acceptable ranges have been published (19).
Quality control drugs were prepared at appropriate concentrations in CAMHB and then aliquoted into 96-well plates at 100 μl/well (plate 1). For B. anthracis Sterne, the following group of drugs, at twofold dilutions, were used: (i) TMP at 0.25, 0.50, 1.0, 2.0, 4.0, 8.0, 16.0, and 32.0 μg/ml, (ii) doxycycline at 0.25, 0.5, 1.0, 2.0, 4.0, and 8.0 μg/ml, and (iii) ciprofloxacin at 0.125, 0.25, 0.5, 1.0, 2.0, and 4.0 μg/ml. These drugs and concentrations are based upon NCCLS interpretive standards for B. anthracis (Table 2K in reference 19): ≤1.0 μg/ml for doxycycline and ≤ 0.5 μg/ml for ciprofloxacin. These three drugs and the complete range of twofold dilutions were set up in duplicate in a 96-well plate, in addition to growth and sterility controls. A standardized inoculum of B. anthracis Sterne was prepared as described above, and 10 μl was used to inoculate each well, except the wells reserved for sterility control. Plates were incubated at 35°C for 16 to 20 h. Controls were set up on all 96-well panels used in this study.
To validate antibiotic performance on each plate, wells were set up with the following quality control strains: E. coli ATCC 25922 for doxycycline (twofold dilution range, 0.25 to 8.0 μg/ml) and for TMP from 0.25 to 32 μg/ml; Staphylococcus aureus ATCC 29213 for TMP (twofold dilution range, 0.25 to 32.0 μg/ml) and ciprofloxacin (twofold dilution range, 0.125 to 4.0 μg/ml); and Enterococcus faecalis ATCC 29212 for ciprofloxacin from 0.125 to 4.0 μg/ml and for TMP from 0.25 to 32.0 μg/ml. A standardized inoculum was prepared for each organism in the same manner as inoculum for test strains and used to inoculate appropriate wells. Plates were incubated at 35°C for 16 to 20 h.
After incubation, the MIC was read visually and in an optical microtiter plate reader programmed to subtract the absorbance at 600 nm (A600) from that at 570 nm (A570). The MIC is reported as the lowest drug concentration yielding a differential absorbance of zero or less (i.e., color remains blue). MICs were compared to acceptable limits for quality control strains (Table 3 in reference 19) to validate drug performance.
All quality control tests were within expected ranges, but B. anthracis Sterne was not inhibited by TMP at 32.0 μg/ml. As a result, the 96-well format was redesigned to encompass higher concentrations of TMP; twofold dilutions were used from 48 to 2,048 μg/ml. After 16 h, the growth of B. anthracis Sterne was reduced by 2,048 μg of TMP per ml, but by 20 h, these wells showed growth using the microtiter plate reader. The 96-well plate format was again designed to include higher levels of TMP for testing against B. anthracis Sterne; twofold dilutions up to 8,192 μg of TMP per ml were included in addition to the lower dilutions previously used. Drugs at these higher concentrations precipitated out of solution during incubation. In order to achieve these drug concentrations, the amount of dimethyl sulfoxide was increased to a level that showed growth inhibition with the solvent control. After 20 h of incubation at 4,096 μg of TMP per ml, there was a differential absorbance reading (A570 − A600) of 0.116, while the solvent control differential was 0.943.
Transfer of resistance to E. coli.
In vitro susceptibility was also determined for E. coli BL21 Star (DE3)pLysS chemically competent cells. E. coli BL21 Star (DE3)pLysS chemically competent cells were transformed with the Invitrogen pCRT7/CT-TOPO vector (Invitrogen Life Technologies) or the Invitrogen pCRT7/CT-TOPO vector with the B. anthracis Sterne DHFR insert (pCRT7/CT-TOPO-Sterne DHFR). E. coli BL21 Star (DE3)pLysS was grown on Luria-Bertani (LB) agar containing 34 μg of chloramphenicol per ml. E. coli BL21 Star (DE3)pLysS, carrying either pCRT7/CT-TOPO or pCRT7/CT-TOPO-Sterne DHFR, was grown on LB agar medium containing 34 μg of chloramphenicol per ml and 100 μg of carbenicillin per ml. The same protocol used to set up the MIC plate for B. anthracis Sterne was used with the E. coli strains with the following modifications. All saline and CAMHB used for E. coli BL21 Star (DE3)pLysS had 34 μg of chloramphenicol per ml added. All saline and CAMHB used for E. coli BL21 Star (DE3) carrying pLysS and pCRT7/CT-TOPO-Sterne DHFR had 34 μg of chloramphenicol per ml and 100 μg of carbenicillin per ml added. TMP was used in twofold serial dilutions from 1 to 4,096 μg/ml. E. coli (ATCC 29522) and Enterococcus faecalis (ATCC 29212), control organisms, were tested against TMP, doxycycline, and SXT. Inoculum preparation and incubation conditions were as stated above.
Primers and PCR amplification.
Forward and reverse primers for PCR amplification of the DHFR genes were designed with the Primer 3 program provided by the National Center for Biotechnology Information (NCBI) (http://www.basic.nwu.edu/biotools/Primer3.html) based on information provided by the ongoing The Institute for Genomic Research (TIGR) sequence program for B. anthracis (Ames strain) (http://tigrblast.tigr.org/ufmg). These primers were designed so that they would be positioned several bases upstream and downstream from the putative gene sequence for DHFR (Fig. 1). Forward and reverse primers designed for B. anthracis DHFR were 5′-CGTCCATTCCCGAAACTTAC-3′ and 5′-GCATTTTCACATGCTACCTTTC-3′, respectively. PCR amplification was conducted with genomic DNA extracted from B. anthracis Sterne, using the DNeasy tissue kit, following the protocol for gram-positive bacteria (QIAGEN), with necessary modifications. PCR products were confirmed by separation on agarose gels, and sequence analysis of products was performed by the Oklahoma State University DNA/Protein Resource Facility. The primers used for sequencing were the same as those used for PCR amplification.
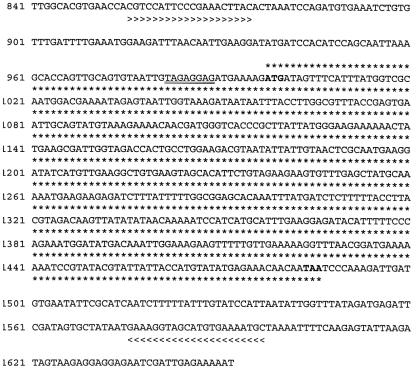
FIG. 1.
Part of the contig obtained from the TIGR database (http://www.tigr.org) by BLAST search (BLAST hit start of 2088847 and BLAST hit end of 2089326 >contig:6611:b_anthracis). The B. anthracis DHFR gene sequence (asterisks), start and stop codons (boldface type), and the putative Shine-Dalgarno sequence (double underline) are indicated. The locations of the left primer (>>>>) and right primer (<<<<) are indicated.
Construction of expression plasmid.
The Invitrogen pCRT7/CT-TOPO TA expression kit was used to construct the expression plasmid. The forward primer for cloning into the Invitrogen pCRT7/CT-TOPO vector was designed following the manufacturer's specifications (Invitrogen Life Technologies). The reverse primer was designed by removing the gene's stop codon and adding a thrombin cleavage site. The sequence of the forward primer was 5′-AAGATGATAGTTTCATTTATGGTCGC-3′. The sequence of the reverse primer was 5′-GCTGCCGCGAGGTACTAGTTGTTGTTTCTCATATAC-3′. PCR was used to amplify B. anthracis Sterne genomic DNA using these primers (Fig. 1). The PCR product was then cloned into the Invitrogen pCRT7/CT-TOPO vector and transformed into E. coli TOP10F′ chemically competent cells. Of the 10 clones picked, restriction enzyme analysis of purified plasmid DNA showed that 8 had the insert in the proper orientation in the vector. Plasmid DNA from these clones was sequenced by the Oklahoma State University DNA/Protein Resource Facility using primers included in the Invitrogen TA cloning kit. The primers were T7 forward (5′-TAATACGACTCACTATAGGG-3′) and V5 C-terminal reverse (5′-ACCGAGGAGAGGGTTAGGGAT-3′). Plasmid DNA from a clone showing the correct construct with a thrombin cleavage site was transformed into E. coli BL21 Star (DE3)pLysS chemically competent cells for expression of the six-histidine-tagged fusion protein.
Expression and initial purification of B. anthracis Sterne recombinant DHFR (rDHFR).
As stated above, plasmid DNA with the correct construct was transformed into E. coli BL21 Star (DE3)pLysS chemically competent cells for expression of the six-histidine-tagged fusion protein, followed by purification on a His-Bind resin column (Novagen, Inc., Madison, Wis.). The expression strain was grown in MM/CA (21a) containing 34 μg of chloramphenicol per ml and 100 μg of carbenicillin per ml at 37°C to an optical density at 600 nm of 0.6, induced with 1 mM isopropyl-β-d-thiogalactopyranoside (IPTG), and cultivated for 24 h at 28°C. Cells were harvested and lysed using Novagen Bug Buster protein extraction reagent with benzonase nuclease and protease inhibitory cocktail set III (Calbiochem). Insoluble proteins were removed by centrifugation, and the soluble proteins were purified by binding the His tag portion of the fusion protein to a His-Bind (Novagen) resin column and eluted with a 5 to 500 mM imidazole gradient in a solution of 20 mM Tris-HCl (pH 7.9) and 500 mM NaCl.
Fast-performance liquid chromatography (FPLC) purification of Sterne rDHFR.
Fractions containing B. anthracis Sterne rDHFR from the His-Bind column were pooled and concentrated using Amicon Ultra-15 Centrifugal Filter Devices with a 10,000-molecular-weight cutoff (Millipore Corp., Bedford, Mass.) at 4,000 × g and 4°C in a Beckman Avanti J-25 centrifuge with a JS-7.5 rotor. The concentrated sample was desalted, and buffer was exchanged using PD 10 columns (Sephadex R G-25 M) (Amersham Biosciences). Fractions were loaded onto a high-resolution Mono-Q 5/50 GL anion exchange column (Amersham Biosciences) and eluted in a buffer containing 20 mM Tris (pH 8.5), 1 M NaCl, 5% glycerol, and 1 mM NaN3 (elution buffer), using a gradient of 0 to 100% elution buffer. Two-milliliter fractions were collected. The Sterne rDHFR eluted between ∼20 and 25% (i.e., 0.2 to 0.25 M NaCl).
IEF.
The isoelectric point of the Sterne rDHFR was determined using Bio-Rad Isoelectric Focusing (IEF) Ready Gels pH 3 to 10 and pH 5 to 8 under native conditions. The gels were run with Bio-Rad IEF standards, and samples were diluted 1:1 in IEF sample buffer (50% glycerol). Focusing was performed in a Mini Protean 3 Cell with anode buffer (7 mM phosphoric acid) in the lower chamber and cathode buffer (20 mM lysine and 20 mM arginine) in the upper chamber. Gels were run under the following conditions in steps: 100 V constant for 60 min, 250 V constant for 60 min, and 500 V constant for 30 min. Gels were stained with Bio-Rad Crocein scarlet and Coomassie blue IEF stain for exactly 45 min followed by destaining in multiple changes of destaining solution (40% methanol, 10% acetic acid) over a period of 2 to 3 h. Samples had been desalted and concentrated in Amicon Ultra-4 units (Millipore) with a 10,000-molecular-weight cutoff.
Thrombin cleavage and purification of Sterne rDHFR.
The His tag was removed by cleavage with 1.0 U of biotinylated thrombin (Novagen) per mg of recombinant protein for 1 h at room temperature, followed by purification with streptavidin agarose. B. anthracis Sterne rDHFR was stabilized throughout the purification with 5 to 10% glycerol and stored at −80°C. Protein concentration was determined using the Bio-Rad microassay in a 96-well format.
Molecular mass determination.
Molecular mass was estimated for B. anthracis Sterne rDHFR before and after removal of the six-histidine tag by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) (12.5% polyacrylamide) with Novagen Perfect Protein markers. Samples and 2× Novagen sample buffer (1:1) were heated at 95°C for 5 min prior to loading on SDS-12.5% polyacrylamide gels. Gels were run with 200 V constant for 45 min. Gels were stained with Coomassie brilliant blue R-250 stain and destained with 40% methanol-10% acetic acid. Calculated molecular masses were determined with a calculator program provided by the National Biomedical Research Foundation of Georgetown University Medical Center (http://pir.georgetown.edu/pirwww/search/comp_mw.shtml). The amino acid sequences for the gene with the His tag cleaved and for the gene with the vector components and the His-tagged fusion protein were entered into the calculator program, and the molecular masses were determined.
DHFR assay.
The activity for B. anthracis Sterne rDHFR was measured at 30°C as the decrease in A340 over 3 min (28). The reaction mixture (1 ml) contained 10 mM 2-mercaptoethanol, 0.1 mM NADPH, 0.1 mM dihydrofolate, 1 mM EDTA, 50 mM potassium phosphate (pH 7), and enzyme. The reaction was initiated by the addition of dihydrofolate after preincubation of the other components for 3 min. For inhibition assays, various amounts of inhibitor were added to the mixture before the 3-min preincubation period. The 50% inhibitory concentrations (IC50s) for TMP and methotrexate were determined from a plot of the log10 of the drug concentration versus percent inhibition using KC Junior software. The average of two or more determinations was used. One unit of enzyme is defined as the amount that reduces 1 μmol of dihydrofolate per min using a molar extinction coefficient of 12,300 M−1 (12).
For some enzyme assays, a cell extract of E. coli BL21 Star (DE3)pLysS was used to demonstrate the IC50 of TMP for E. coli BL21 Star (DE3)pLysS DHFR, a bacterial strain that is sensitive to TMP (MIC of ≤1 μg/ml), as described below in Results. The cell extract was obtained as follows. A cell pellet from a 0.5-liter culture of E. coli BL21 Star (DE3)pLysS was treated with Bug Buster, benzonase (Novagen), and protease inhibitor cocktail set III (Calbiochem) following the manufacturer's instructions. The lysate was centrifuged at 48,000 × g and 4°C for 20 min and filtered through a 0.2-μm-pore-size filter. The enzyme lysate was concentrated using Amicon Ultra-15 Centrifugal Devices (Millipore) with a 10,000-molecular-weight cutoff, and buffer was exchanged to 5 mM imidazole-0.5 M NaCl-20 mM Tris-HCl (pH 7.9). The cell extract was used in the DHFR assay described above to determine the IC50 for TMP.
RESULTS
In vitro drug susceptibility.
After the plates were incubated, the MIC was read visually and evaluated with an optical microtiter plate reader (at 570 and 600 nm). The MICs were compared to acceptable limits for quality control strains to validate drug performance (19). The MIC was the lowest concentration of antimicrobial agent at which no color change occurred (i.e., color remains blue). The MICs of ciprofloxacin and doxycycline for B. anthracis Sterne were 0.25 and ≤0.25 μg/ml, respectively. The MIC of TMP for B. anthracis Sterne was determined to be >2,048 but ≤4,096 μg/ml.
Transfer of resistance.
Transformation of the B. anthracis Sterne DHFR gene into E. coli BL21 Star (DE3)pLysS and subsequent MIC evaluation using the AlamarBlue broth dilution assay demonstrated a change in the MIC of TMP from ≤1 μg/ml for the wild-type E. coli BL21 Star (DE3)pLysS to >2,048 but ≤4,096 μg/ml for the E. coli BL21 Star (DE3)pLysS containing the Sterne DHFR construct. The MIC of TMP for E. coli BL21 Star (DE3)pLysS, transformed with the vector only, was ≤1.0 μg/ml. This was equivalent to the TMP MIC obtained with the AlamarBlue broth dilution assay using B. anthracis Sterne as the test organism. A protein-protein BLAST search with the B. anthracis Sterne DHFR demonstrated that the B. anthracis virulence plasmids pX01 (NC003980) and pX02 (NC4003981), sequenced by NCBI, do not contain DHFR genes. Therefore, these results suggest that the basis for TMP resistance is located on the chromosome.
Deduced sequence of DHFR gene from B. anthracis Sterne.
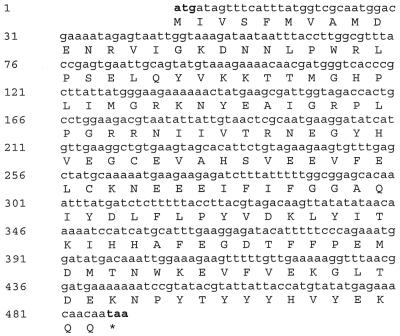
A BLAST search of the TIGR Genome Sequencing project (http://www.tigr.org), using NCBI accession number NP656101 resulted in the contig sequence presented in Fig. 1. Primers (described above) were designed using the Primer3 program provided by the Whitehead Institute for Biomedical Research (http://frodo.wi.mit.edu/cgi-bin/primer3/primer3.cgi) (Fig. 1). The NCBI ORF Finder was then used to determine the open reading frame (ORF) of the putative DHFR (Fig. 2) (http://www.ncbi.nlm.nih.gov/gorf/gorf.html) (Fig. 1). A BLAST search of NCBI with the ORF information was used to confirm the putative sequences, and the Shine-Dalgarno sequence was deduced (24).
FIG. 2.
ORF obtained with ORF Finder (NCBI) using the contig presented in Fig. 1. Start and stop codons are shown in boldface type.
Transformation, expression, and purification.
Sequence analysis of plasmid DNA from two clones of E. coli TOP10F′ transformed with pCRT7/CT-TOPO-Sterne DHFR showed the correct construct including the thrombin cleavage site. A pilot expression experiment was performed by transforming E. coli BL21 Star (DE3)pLysS competent cells with plasmid DNA from one of the clones and growing the organism in MM/CA with 34 μg of chloramphenicol per ml and 100 μg of carbenicillin per ml. E. coli BL21 Star (DE3)pLysS competent cells was transformed with plasmid DNA containing only the pCRT7/CT-TOPO vector to compare B. anthracis Sterne DHFR expression and enzyme activity to that of endogenous E. coli BL21 Star (DE3)pLysS enzyme. Cultures were grown at 37°C with shaking at 200 rpm until the bacteria were induced with 1 mM IPTG. When the bacteria were induced with IPTG, incubation conditions were changed to 28°C and 200 rpm for 24 h. Samples were taken at the appropriate times for lysis and protein evaluation. After 24 h, cultures were harvested by centrifugation at 10,000 × g and 4°C for 20 min, the supernatants were removed, and the pellets were frozen at −80°C. Pellets were lysed with Bug Buster (Novagen), benzonase nuclease (Novagen), and protease inhibitor cocktail III (Calbiochem). The gel analysis showed good expression of Sterne rDHFR and little expression of endogenous DHFR (Fig. 3).
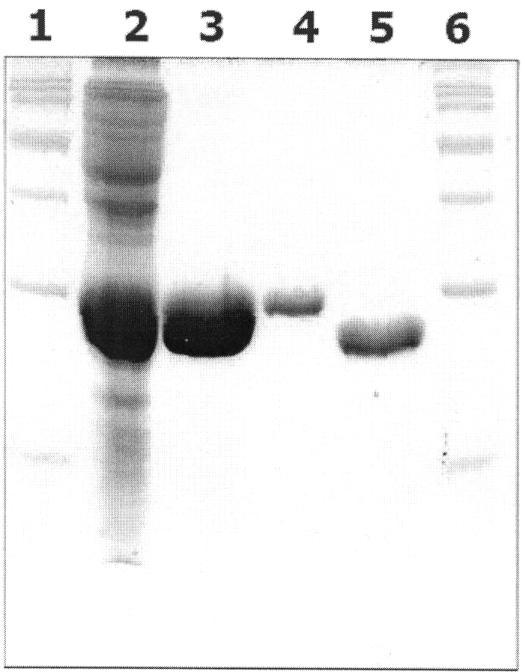
FIG. 3.
SDS-12.5% polyacrylamide gel showing steps involved in purification of B. anthracis Sterne rDHFR. Lanes 1 and 6 contain Novagen Perfect Protein markers (15 to 150 kDa ladder). Lane 2 contains cell lysate from E. coli BL21 Star (DE3) carrying plasmids pLysS and pCRT7/CT-TOPO-Sterne rDHFR with the six-histidine tag (precolumn) (lysate filtered through a 0.22-μm-pore-size filter). Lane 3 contains pooled Sterne rDHFR with the six-His tag (enzyme purified by passage through a nickel column). Lane 4 contains FPLC-purified Sterne rDHFR with the six-His tag, and lane 5 contains FPLC-purified Sterne rDHFR with the six-His tag removed.
B. anthracis Sterne rDHFR expression on a large scale was studied as follows. Cells were grown in 0.5 liter of MM/CA containing 34 μg of chloramphenicol per ml, 100 μg of carbenicillin per ml, and 1 mM IPTG for induction. Cells were grown at 28°C for 24 h. Cells were harvested by centrifugation and lysed with Bug Buster (Novagen) as usual. Soluble His-tagged Sterne rDHFR was initially purified using His-Bind resin (Novagen) with elution using a 5 to 500 mM imidazole gradient. SDS-PAGE analysis of eluted fractions indicated those fractions which contained six-histidine-tagged Sterne rDHFR. Those fractions were pooled, concentrated, and desalted, and buffer was exchanged to 20 mM Tris-HCl (pH 8.5)-5% glycerol. Samples were loaded onto a Mono-Q column and eluted with a 0 to 100% gradient of solution consisting of 1 M NaCl, 20 mM Tris-HCl (pH 8.5), and 5% glycerol.
In order to optimize Mono-Q purification, the isoelectric point of the recombinant fusion protein was determined to be 7.1. Once optimum conditions were determined, a purification protocol for Sterne rDHFR was established. This protocol consisted of prepurification with the His-Bind column, followed by final purification using the Mono-Q column. For some enzyme assays, the histidine tag was cleaved, and the resulting rDHFR was purified as described in Materials and Methods. The isoelectric point of the cleaved protein (Sterne DHFR with the six-histidine tag removed) is 5.5.
Molecular mass determination.
SDS-PAGE with Novagen Perfect Protein markers showed that the molecular masses of Sterne rDHFR with the six-histidine tag and Sterne rDHFR with the histidine tag cleaved were 23.5 and 21.5 kDa, respectively (Fig. 3). The calculated molecular masses were 23 and 19.6 kDa, respectively.
Enzyme functionality.
Enzyme assays demonstrated that the B. anthracis Sterne rDHFR had high enzyme activity, while the lysate from the construct with only the vector had very little activity (Table 1).
TABLE 1.
IC50 data for four rDHFRs
| Enzyme | IC50 (nM)a
|
|
|---|---|---|
| TMP | MTXb | |
| Human rDHFR | 1.62 × 106 ± 5.77 × 103 (2) | 24.3 ± 6.99 (3) |
| B. anthracis Sterne rDHFR | ||
| With His tag | 7.73 × 104 ± 8.24 × 103 (4) | 15.1 ± 2.82 (3) |
| Without His tag | 7.72 × 104 ± 2.04 × 103 (4) | 12.2 ± 3.1 (3) |
| M. avium rDHFR | 5.75 × 103 ± 7.70 × 102 (3) | 5.1 ± 0.83 (5) |
Each value is the mean ± standard error of the mean. The number of samples is given in parentheses.
MTX, methotrexate.
IC50.
The mean IC50s of TMP and methotrexate for Sterne rDHFR with the histidine tag were determined to be 77,324 and 15.06 nM, respectively. With the His tag removed, the IC50s were determined to be 77,233 and 12.21 nM, respectively. Purified Mycobacterium avium rDHFR was used as a reference, since that organism is also naturally resistant to TMP (Table 1) (28). The IC50s of TMP and methotrexate for M. avium rDHFR were 5,752 and 5.10 nM, respectively (Table 1). Methotrexate, a potent inhibitor of DHFR, including human DHFR (27), was used as a positive control. The mean IC50 of TMP for the E. coli BL21 Star (DE3)pLysS DHFR was determined to be 0.63 nM (standard error of the mean = 0.078; n = 3).
Homology.
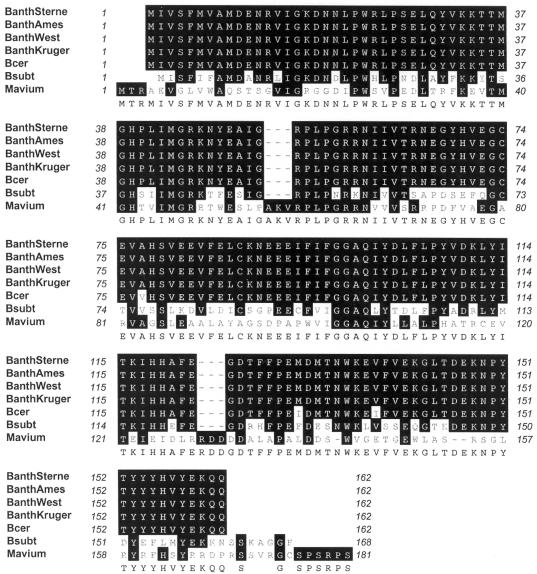
Alignment of the B. anthracis Sterne DHFR (GenBank accession number AY569129) amino acid sequence revealed 100% homology with various virulent strains that are being sequenced by TIGR (http://www.tigr.org/tdb/mdb/mdbinprogress.html), including Ames, Western N. America (GT3 Group A1a), and Kruger B (GT87 Group B1) (Fig. 4). B. anthracis Sterne DHFR showed 98% identity with Bacillus cereus ATCC 14579 DHFR (NCBI accession number NP_831957) (15). B. anthracis Sterne DHFR showed 55% identity with Bacillus subtilis DHFR (NCBI accession number AAA22853) (16) (Fig. 4). B. anthracis Sterne DHFR showed 33% identity with M. avium DHFR (NCBI accession number AF006616) (28) (Fig. 4), which is also naturally resistant to TMP.
FIG. 4.
Alignment of the B. anthracis Sterne DHFR sequence (GenBank accession number AY569129) (BanthSterne) with the DHFR sequences from B. anthracis Ames, Western N. America GT3 Group A1a (West), and Kruger B GT87 Group B1 (Kruger) and from B. cereus (Bcer), B. subtilis (Bsubt), and M. avium (Mavium). Identical residues are shown as white letters on black background. Alignment was accomplished with MacVector 7 (Accelrys, San Diego, Calif.). Gaps introduced to maximize alignment are shown as dashes.
DISCUSSION
Logical drug design requires an appropriate target (e.g., enzyme) and a means by which that target can be evaluated for optimum development of an effective antimicrobial agent. In that regard, for enzyme targets, recombinant enzyme is essential, not only for in vitro assessment of test compounds but also for eventual molecular modeling involving crystallography. Evaluation of the literature revealed that B. anthracis is naturally resistant to an antimicrobial agent that has been shown to be effective against various other bacterial pathogens (20). That antimicrobial is TMP (20), a synthetic drug that targets an enzyme in the folate biosynthetic pathway, DHFR.
Since TMP was introduced for clinical use in 1969, a variety of TMP-resistant bacteria have been isolated (7). The inhibitory effects of TMP are associated with its ability to inhibit DHFR, a key enzyme in the folate biosynthetic pathway (11). As a result of TMP's inhibitory abilities, intracellular reduced folates are depleted and one-carbon transfer reactions are limited (11). This eventually affects RNA, DNA, and protein synthesis (11). Resistance to TMP is generally seen as the production of an extra DHFR found on plasmids or other genetic elements (5, 9, 13). In addition, TMP resistance can result from mutations in the chromosomal gene that result in a higher Ki for the drug (1, 8, 13, 17, 21), as well as the production of an additional DHFR (7). Development of high MICs has been associated with a combination of a structurally modified enzyme and overproduction (10).
If natural resistance to TMP is due to the lack of selectivity for the B. anthracis DHFR, then that enzyme target might prove useful as a candidate for the development of antimicrobial agents that would presumably not be in the standard antimicrobial armamentarium. However, potentially useful drugs might be available in existing chemical libraries and prove to be advantageous for the development of more effective inhibitors for B. anthracis.
One purpose of this study was to confirm the in vitro resistance of B. anthracis to TMP. Another objective was to clone and express recombinant B. anthracis Sterne DHFR and use it to demonstrate that resistance to TMP is due to the lack of selectivity for the enzyme. With this information, it should be possible to screen stockpiled antifolates to identify potential narrow-spectrum drugs that would selectively affect B. anthracis DHFR. rDHFR would also be important for screening purposes and for design and synthesis of new narrow-spectrum inhibitors of B. anthracis.
Zywno-van Ginkel et al. previously reported the identification and functional cloning of M. avium DHFR (NCBI accession number AF006616) (28), which is also naturally resistant to TMP (26). Suling et al. performed an initial screening with recombinant DHFR, which eventually led to a lead compound that showed selective activity against M. avium rDHFR (26). As discussed in that study, use of the rDHFR was essential in determining a logical progression in the synthesis of improved inhibitors. It is possible that a similar effort is possible with the DHFR from B. anthracis.
Examination of the sequence information for B. anthracis Ames (NCBI accession number NP_844628) (22) and B. anthracis Sterne reveals a 100% homology for the amino acid sequences of the two strains for DHFR [E.C. 1.5.1.3]. In addition, a BLAST search of these amino acid sequences against B. anthracis A2012 (NCBI accession number NP_656101) (23) (data not shown) as well as the Kruger strain (TIGR Microbial Genome project) revealed 100% homology for DHFR. This is important because the Kruger strain originated from the Kruger National Park in South Africa, the area that reported 100% resistance against TMP and 95% resistance for various sulfonamides (20). Thus, the recombinant product produced from the DHFR sequence of the Sterne strain can be used for in vitro drug screening for all the reported virulent strains of B. anthracis.
Using standard procedures, we were able to clone and express the chromosomally encoded gene for DHFR in B. anthracis. In vitro assays with B. anthracis Sterne showed a high level of resistance against TMP (>2,048 but ≤4,096 μg/ml). Previously, others have reported a high level of TMP resistance for a clinical isolate of E. coli; the MIC was >1 g/liter (10). The resistance of that particular isolate was due to overproduction of DHFR as a result of a promoter up-mutation (10). Resistance to TMP due to mutations in the DHFR chromosomal gene has been reported for the gram-positive Streptococcus pneumoniae (1). The MICs reported in that study ranged from 64 to 512 μg/ml and were due to two main groups of mutations both sharing six amino acid changes (1).
In our study, the enzyme assay established an IC50 of 77,233 nM for the Sterne rDHFR when tested with TMP, thus demonstrating a reduced selectivity for the target. By comparison, the IC50 for methotrexate, a potent inhibitor of most DHFRs, including human DHFR (27), was observed to be 12.21 nM. These results help to clarify the reason for TMP resistance in B. anthracis. With this information, it will be possible to conduct appropriate screening of potential inhibitors from chemical stockpiles. Once inhibitors are identified, further drug development can continue, making it possible to obtain narrow-spectrum inhibitors for treatment of anthrax. In that regard, recombinant product will also be important for crystallographic studies that will be essential for designing new inhibitors.
Acknowledgments
This research was funded in part from funds provided by the Sitlington Endowed Chair in Infectious Diseases at Oklahoma State University (William W. Barrow) and a NIH/NIAID grant R21-AI055643 (principal investigator, William W. Barrow).
REFERENCES
- 1.Adrian, P. V., and K. P. Klugman. 1997. Mutations in the dihydrofolate reductase gene of trimethoprim-resistant isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 41:2406-2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakici, M. Z., N. Elaldi, M. Bakir, I. Dodmetas, M. Erandac, and M. Turan. 2002. Antimicrobial susceptibility of Bacillus anthracis in an endemic area. Scand. J. Infect. Dis. 34:564-566. [DOI] [PubMed] [Google Scholar]
- 3.Brook, I., T. B. Elliott, H. I. Pryor, T. E. Sautter, B. T. Gnade, J. H. Thakar, and G. B. Knudson. 2001. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Int. J. Antimicrob. Agents 18:559-562. [DOI] [PubMed] [Google Scholar]
- 4.Cavallo, J. D., F. Ramisse, M. Girardet, J. Vaissaire, M. Mock, and E. Hernandez. 2002. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. Antimicrob. Agents Chemother. 46:2307-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charpentier, E., and P. Courvalin. 1997. Emergence of the trimethoprim resistance gene dfrD in Listeria monocytogenes BM4293. Antimicrob. Agents Chemother. 41:1134-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coker, P. R., K. L. Smith, and M. E. Hugh-Jones. 2002. Antimicrobial susceptibilities of diverse Bacillus anthracis isolates. Antimicrob. Agents Chemother. 46:3843-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coque, T. M., K. V. Singh, G. M. Weinstock, and B. E. Murray. 1999. Characterization of dihydrofolate reductase genes from trimethoprim-susceptible and trimethoprim-resistant strains of Enterococcus faecalis. Antimicrob. Agents Chemother. 43:141-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dale, G. E., D. Broger, A. D'Arcy, P. G. Hartman, R. DeHoogt, S. Jolidon, I. Kompis, A. M. Labhardt, H. Langen, H. Locher, M. G. Page, D. Stüber, R. L. Then, B. Wipf, and C. Oefner. 1997. A single amino acid substitution in Staphylococcus aureus dihydrofolate reductase determines trimethoprim resistance. J. Mol. Biol. 266:23-30. [DOI] [PubMed] [Google Scholar]
- 9.Dale, G. E., H. Langen, M. G. P. Page, R. L. Then, and D. Stüber. 1995. Cloning and characterization of a novel, plasmid-encoded trimethoprim-resistant dihydrofolate reductase from Staphylococcus haemolyticus MUR313. Antimicrob. Agents Chemother. 39:1920-1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flensburg, J., and O. Skold. 1987. Massive overproduction of dihydrofolate reductase in bacteria as a response to the use of trimethoprim. Eur. J. Biochem. 162:473-476. [DOI] [PubMed] [Google Scholar]
- 11.Hartman, P. G. 1993. Molecular aspects and mechanism of action of dihydrofolate reductase inhibitors. J. Chemother. 5:369-376. [PubMed] [Google Scholar]
- 12.Hillcoat, B. L., P. F. Dixon, and R. L. Blakley. 1967. Effect of substrate decomposition on the spectrophotometric assay of dihydrofolate reductase. Anal. Biochem. 21:178-189. [DOI] [PubMed] [Google Scholar]
- 13.Huovinen, P., L. Sundström, G. Swedberg, and O. Sköld. 1995. Trimethoprim and sulfonamide resistance. Antimicrob. Agents Chemother. 39:279-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inglesby, T. V., D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Hauer, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 1999. Anthrax as a biological weapon. JAMA 281:1735-1745. [DOI] [PubMed] [Google Scholar]
- 15.Ivanova, N., A. Sorokin, I. Anderson, N. Galleron, B. Candelon, V. Kapatral, A. Bhattacharyya, G. Reznik, N. Mikhailova, A. Lapidus, L. Chu, M. Mazur, E. Goltsman, N. Larsen, M. D'Souza, T. Walunas, Y. Grechkin, G. Pusch, R. Haselkorn, M. Fonstein, S. D. Ehrlich, R. Overbeek, and N. Kyrpides. 2003. Genome sequence of Bacillus cereus and comparative analysis with Bacillus anthracis. Nature 423:87-91. [DOI] [PubMed] [Google Scholar]
- 16.Iwakura, M., M. Kawata, K. Tsuda, and T. Tanaka. 1988. Nucleotide sequence of the thymidylate synthase B and dihydrofolate reductase genes contained in one Bacillus subtilis operon. Gene 64:9-20. [DOI] [PubMed] [Google Scholar]
- 17.Maskell, J. P., A. M. Sefton, and L. M. C. Hall. 2001. Multiple mutations modulate the function of dihydrofolate reductase in trimethoprim-resistant Streptococcus pneumoniae. Antimicrob. Agents Chemother. 45:1104-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammed, M. J., C. K. Marston, T. Popovic, R. S. Weyant, and F. C. Tenover. 2002. Antimicrobial susceptibility testing of Bacillus anthracis: comparison of results obtained by using the National Committee for Clinical Laboratory Standards broth microdilution reference and Etest agar gradient diffusion methods. J. Clin. Microbiol. 40:1902-1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NCCLS. 2003. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, 6th ed., vol. 23, p. 1-50. NCCLS, Wayne, Pa. [Google Scholar]
- 20.Odendaal, M. S., P. M. Pieterson, V. deMos, and A. D. Botha. 1991. The antibiotic sensitivity patterns of Bacillus anthracis isolated from the Kruger National Park. Onderstepoort J. Vet. Res. 58:17-19. [PubMed] [Google Scholar]
- 21.Pikis, A., J. A. Donkersloot, W. J. Rodriguez, and J. M. Keith. 1998. A conservative amino acid mutation in the chromosome-encoded dihydrofolate reductase confers trimethoprim resistance in Streptococcus pneumoniae. J. Infect. Dis. 178:700-706. [DOI] [PubMed] [Google Scholar]
- 21a.Pryor, K. D., and B. Leiting. 1997. High-level expression of soluble protein in Escherichia coli using a his6- and maltose-binding-protein double-affinity fusion system. Protein Expr. Purif. 10:309-319. [DOI] [PubMed] [Google Scholar]
- 22.Read, T. D., S. N. Peterson, N. Tourasse, L. W. Baillie, I. T. Paulsen, K. E. Nelson, H. Tettelin, D. E. Fouts, J. A. Eisen, S. R. Gill, E. K. Holtzapple, O. A. Okstad, E. Helgason, J. Rilstone, M. Wu, J. F. Kolonay, M. J. Beanan, R. J. Dodson, L. M. Brinkac, M. Gwinn, R. T. DeBoy, R. Madpu, S. C. Daugherty, A. S. Durkin, D. H. Haft, W. C. Nelson, J. D. Peterson, M. Pop, H. M. Khouri, D. Radune, J. L. Benton, Y. Mahamoud, L. Jiang, I. R. Hance, J. F. Weidman, K. J. Berry, R. D. Plaut, A. M. Wolf, K. L. Watkins, W. C. Nierman, A. Hazen, R. Cline, C. Redmond, J. E. Thwaite, O. White, S. L. Salzberg, B. Thomason, A. M. Friedlander, T. M. Koehler, P. C. Hanna, A. B. Kolsto, and C. M. Fraser. 2003. The genome sequence of Bacillus anthracis Ames and comparison to closely related bacteria. Nature 423:81-86. [DOI] [PubMed] [Google Scholar]
- 23.Read, T. D., S. L. Salzberg, M. Pop, M. Shumway, L. Umayam, L. Jiang, E. Holtzapple, J. Busch, K. L. Smith, J. M. Schupp, D. Solomon, P. Keim, and C. M. Fraser. 2002. Comparative genome sequencing for discovery of novel polymorphisms in Bacillus anthracis. Science 296:2028-2033. [DOI] [PubMed] [Google Scholar]
- 24.Shine, J., and L. Dalgarno. 1974. The 3′-terminal sequence of Escherichia coli 16S ribosomal RNA: complementarity to nonsense triplets and ribosome binding sites. Proc. Natl. Acad. Sci. USA 71:1342-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stephenson, J. 2002. Experts focus on infective agents of bioterrorism. JAMA 287:575-576. [PubMed] [Google Scholar]
- 26.Suling, W. J., L. E. Seitz, V. Pathak, L. Westbrook, E. W. Barrow, S. Zywno-van-Ginkel, R. C. Reynolds, J. R. Piper, and W. W. Barrow. 2000. Antimycobacterial activity of 2,4-diamino-5-deazapteridine derivatives and effects on mycobacterial dihydrofolate reductase. Antimicrob. Agents Chemother. 44:2784-2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomson. 2003. Physicians' Desk Reference Electronic Library, version 6.1.252a, 57th ed., vol. 2003.2. Thomson, Montvale, N.J.
- 28.Zywno-van Ginkel, S., T. P. Dooley, W. J. Suling, and W. W. Barrow. 1997. Identification and cloning of the Mycobacterium avium folA gene, required for dihydrofolate reductase activity. FEMS Microbiol. Lett. 156:69-78. [DOI] [PubMed] [Google Scholar]