Abstract
Although 11% (6.4 million) American children are diagnosed with attention deficit/hyperactivity disorder (ADHD), the role of ADHD severity in shaping the association between ADHD diagnosis and academic achievement is not understood. Using a nationally-representative sample of 7830 U.S. kindergartners from the Early Childhood Longitudinal Study-Kindergarten Cohort, we use regression and propensity score matching to compare diagnosed (N = 350) and undiagnosed children who are cognitively, behaviorally, and demographically similar. Diagnosed children with less severe ADHD-related behaviors on average scored lower in reading (–0.30 SD) and math (–0.22 SD) than their undiagnosed peers – a difference two times larger than that between diagnosed and undiagnosed children with more severe ADHD-related behaviors. Pharmacological treatment did not attenuate most of this “diagnostic labeling effect” among children with less severe ADHD-related behaviors. Negative factors associated with an ADHD diagnosis may outweigh potential benefits for achievement among children with less severe ADHD-related behaviors, even those receiving treatment.
Keywords: Child health, Mental health, Attention-deficit/hyperactivity, disorder (ADHD), Behavioral development, Cognitive development, Academic achievement, Education, Stigma
1. Introduction
Attention deficit/hyperactivity disorder (ADHD) is the most commonly diagnosed neurobehavioral disorder among American children (Currie and Stabile, 2006). Today, 4.9% of children ages 5–11 years and 11% ages 4–17 years (approximately 6.4 million children) are diagnosed with ADHD (Visser et al., 2013, 2014). In recent works, scholars situate ADHD-related behaviors along a spectrum of severity in recognition of the importance of variation in the severity of diagnosed children’s behavioral and cognitive impairments (Asherson and Trzaskowski, 2015; Kiely and Adesman, 2015). However, this heterogeneity in ADHD severity is rarely considered empirically when examining the implications of diagnosing children with ADHD (Hinshaw and Scheffler, 2014; Swanson et al., 2001). The efficacy of diagnosis and treatment for young children with less severe, as compared to more severe, ADHD and co-morbid oppositional defiant disorder (ODD) behaviors remains understudied (Olfson et al., 2003; Visser et al., 2010, 2014).1 This is the first study to use nationally representative longitudinal U.S. data to examine the relationship between early elementary school ADHD diagnosis and adolescent academic achievement (Baughman Jr, 2006; Bokhari and Schneider, 2011; Evans et al., 2010; Rappley et al., 1999; Zito et al., 2000).
An ADHD diagnosis has both positive and negative implications for a child’s academic achievement (Efron et al., 2014; Link and Phelan, 2010; McLeod et al., 2004; Zoega et al., 2012). Positive aspects of early detection may include access to efficacious forms of stimulant and behavioral treatment, as well as Individualized Education Programs (IEPs) and 504 Special Education Plans (Scheffler et al., 2009a). Early diagnosis also provides families and schools with an explanation for the child’s ADHD-related academic and social difficulties and may prevent blame being laid on the child. Negative social aspects may include parents and teachers assuming blame for the child’s difficulties and engaging in less academic and extracurricular “opportunity-pushing” for fear of overburdening the child or placing excessive expectations on them given their condition (Angold et al., 2000; Barry et al., 2002; Eisenberg and Schneider, 2007; McLeod et al., 2004; Rennie et al., 2014; Singh, 2003, 2007; Wolraich, 2000). As a result, the child diagnosed with ADHD may be less academically and socially prepared. Aware of being differentially treated, the diagnosed child may experience lowered self-concept, self-confidence, and academic expectations (Angold et al., 2000; Barry et al., 2002; Eisenberg and Schneider, 2007; Link and Phelan, 2010; Rennie et al., 2014; Singh, 2003, 2007). How these pros and cons associated with an early childhood ADHD diagnosis balance out to shape the “net association” (henceforth referred to simply as association), between an early elementary school ADHD diagnosis and later academic achievement has not been examined in a nationally representative longitudinal sample (Hinshaw and Scheffler, 2014; Molina et al., 2009).
In light of substantial heterogeneity in the severity of children’s underlying ADHD-related behaviors and academic and social impairment (Rennie et al., 2014; Asherson and Trzaskowski, 2015), some children with less severe ADHD-related behaviors and impairment fall into a gray area with regard to meeting clinical standards for an ADHD diagnosis (Kiely and Adesman, 2015; Pescosolido et al., 2000; Verbrugge and Jette, 1994). For these children, parents’, teachers’, and clinicians’ perceptions of the severity and duration of a child’s impairments may be especially important in tipping the balance in making a diagnosis (Charach et al., 2013; Evans et al., 2010; Hinshaw and Scheffler, 2014; Pescosolido et al., 2000). Reports of the severity of ADHD-related behaviors also may moderate the association between an ADHD diagnosis and later achievement. But, to our knowledge, no studies have examined this possibility.
Overall, due to the countervailing positive and negative implications of an ADHD diagnosis and differences in the severity of ADHD-related behaviors, it is unclear a priori whether an ADHD diagnosis has, on balance, a negative, neutral, or positive association with children’s academic achievement and whether the association varies by the level of ADHD severity. Uncertainty arises because existing studies: 1) rarely examine how the positive and negative implications of diagnosis balance out, controlling for the baseline achievement or impairment and underlying ADHD-related behaviors that also affect later achievement (Currie and Stabile, 2006; Efron et al., 2014), 2) often over-represent children with more severe ADHD, making it difficult to generate nationally representative U.S. estimates of how diagnosis and treatment affect the achievement of children with less severe, as compared to more severe, ADHD (Bussing et al., 2010; Mueller et al., 2012; Travell and Visser, 2006; Zoega et al., 2012), and; 3) often compare children diagnosed with ADHD to case controls with different levels of baseline academic ability and severity of ADHD, making it difficult to accurately isolate the association between an ADHD diagnosis and later achievement at differing levels of ADHD severity (Efron et al., 2014; Podolski and Nigg, 2001).
To help address these gaps in extant research, we address the following research questions: 1) How does severity of ADHD-related behaviors shape the estimated association between an early childhood ADHD diagnosis and later academic achievement? 2) How much of the estimated association between an early childhood ADHD diagnosis and later academic achievement is offset by pharmacological treatment, behavioral counseling, or special education services among children with less severe compared to more severe ADHD-related behaviors?
1.1. Severity of ADHD-related behaviors, treatment, and the relationship between an ADHD diagnosis and achievement
Children who receive a diagnosis of ADHD but display less severe ADHD-related behaviors and impairments may face a double jeopardy, or double disadvantage. First, children with less severe ADHD-related behaviors may be less likely to receive medication and behavioral and educational services due to factors like lower acceptance of medication and service use among people with less severe mental illness (McLeod et al., 2004). Among children diagnosed with ADHD who do receive medication or behavioral/educational services, the efficacy of medication or services may not be uniform by ADHD severity. Research on the efficacy of pharmacological interventions to treat children with ADHD suggests that ADHD severity may moderate the effect of treatments on later academic achievement (Brassett-Harknett and Butler, 2007; Charach et al., 2013; Swanson et al., 2001). On one hand, children with less severe ADHD may benefit more from treatment because they are less likely to have other co-morbid conditions and are more likely to receive low dose medication, which is associated with fewer adverse side-effects (Ghuman et al., 2009). On the other hand, children with more severe ADHD may benefit more from medication because of higher rates of adherence, lower rates of misdiagnosis, and greater room for noticeable behavioral improvement (Charach et al., 2013; Evans et al., 2010; Ghuman et al., 2009; Pescosolido et al., 2000).
Second, school and learning context factors associated with treatment also may influence the diagnosis-achievement relationship differently for children with less severe compared to more severe ADHD-related behaviors. To the extent medication use is visible in schools and communities and occurs in contexts in which such use is uncommon, receiving medication for a behavioral condition like ADHD also may trigger in the child and others a belief that the child’s academic, social, or developmental abilities are lacking – a process known as negative-ability labeling (Link and Phelan, 2010). For example, in the late 1980s through late 2000s, the modal prescription for young children diagnosed with ADHD required two to three doses per day, making the child’s receipt of medication visible during the school day (Charach et al., 2013). Even without external activation of a negative ability label, the child may him or herself internalize receipt of medication as an indicator of negative ability, which may in turn be associated with lower academic performance.
In particular, labeling may be associated with lower performance among children with less severe ADHD because they are more likely to remain in regular instruction classrooms (Bussing et al., 2012b). In regular instruction classrooms, children diagnosed and/or treated for ADHD or another condition are more likely to be compared, and compare themselves, to children without a diagnosed mental health condition (Eisenberg and Schneider, 2007). As such, children with less severe ADHD-related behaviors may be more likely than children with more severe ADHD-related behaviors to experience negativeability labeling when diagnosed with ADHD and/or treated with medication. By contrast, to the extent medication helps control behaviors and the behaviors themselves trigger the experience of negative-ability social labeling, treatment may attenuate the association between an ADHD diagnosis and achievement (Pescosolido et al., 2008).
Finally, the extent to which an ADHD diagnosis triggers the negative ability beliefs that are associated with lower academic achievement may also vary by learning activity (Hinshaw and Scheffler, 2014; Rucklidge and Tannock, 2001). Activities like reading are more likely to be typed as difficult for children with ADHD because they tend to require extended concentration (Rucklidge and Tannock, 2001). By contrast, elementary school math is less likely to be typed as difficult for children with ADHD because, unlike for reading long passages, solving elementary and middle school level math problems does not necessarily require extended periods of concentration. Therefore, the magnitude of the ADHD diagnosis-reading achievement relationship may be larger (i.e., more negative) than the diagnosis-math relationship even among children with less severe inattentive and hyperactivity/impulsivity behaviors. The diagnosis-reading relationship may be even larger still if medication treatment is less efficacious due to misdiagnosis or marginal qualification for an ADHD diagnosis among some children with less severe ADHD, as discussed previously.
In sum, children who receive a diagnosis of ADHD but display less severe ADHD-related behaviors and impairments nevertheless may experience the negative social implications of carrying the diagnostic label. This may be partly because children with less severe ADHD-related behaviors are more likely to remain in regular instruction classrooms and therefore to be compared to neurotypical children more often and thereby assessed as having lower social and academic skills and trajectories relative to neurotypical children (Carpenter and Austin, 2008; Eisenberg and Schneider, 2007; Pescosolido et al., 2008). Even if they receive medication or other treatments, these negative assessments may result in dampened self-esteem and academic expectations, which are negatively associated with academic achievement. Medication may not help a child overcome the burden of a negative-ability label because medications are designed to control behaviors and improve concentration rather than address the social and psychological processes that lead to lowered achievement. By contrast, medication and other treatments may be more efficacious in improving reading achievement among children with more severe ADHD-related behaviors. The greater efficacy of treatments among children with more severe ADHD-related behaviors may be both because these children are less likely to be misdiagnosed and because their more severe condition(s) may be associated with even lower reading impairments, creating greater room for reading improvement.
But, due in part to a lack of studies including children with less severe ADHD-related behaviors, differences in the efficacy of treatments are under examined. In this study, we examine whether an ADHD diagnosis is associated with lower performance due to the ADHD diagnosis, and how treatment may modify the diagnosis-achievement relationship. We hypothesize:
Severity of ADHD-related behaviors moderates the estimated association between an early childhood ADHD diagnosis and later academic achievement. Children with less severe ADHD-related behaviors experience a large, negative association between an ADHD diagnosis and reading achievement;
Pharmacological treatment, behavioral counseling, and special education services will offset only a small share of the large anticipated negative association between an ADHD diagnosis and reading achievement among children with less severe ADHD-related behaviors diagnosed with ADHD, and;
The experience of receiving medication treatment due to diagnosis with another mental health condition or later diagnosis with ADHD may also trigger negative ability labeling. Because we do not know the etiology of any co-morbid conditions for which medication is used in our sample, labeling due to medication use without an early ADHD diagnosis may be associated with lower achievement among both children with less severe and more sever ADHD-related behaviors.
Taken together, this study helps fill gaps in existing work on the links between ADHD diagnosis and academic achievement by producing nationally representative population estimates of the association between an early childhood ADHD diagnosis and eighth grade reading and math test scores for children with less severe as well as more severe ADHD-related behaviors. The study also examines how much of the estimated association between a diagnosis and achievement is offset by pharmacological treatment, behavioral counseling, or special education services.
2. Methods
2.1. Data and sample
This study was approved by the relevant Institutional Review Board. This study draws on the restricted-use Early Childhood Longitudinal Study-Kindergarten Cohort of 1998 (ECLS-K) collected by the U.S. Department of Education’s National Center for Education Statistics. The ECLS-K, spanning 1998 to 2008, is the most recent longitudinal study to follow a nationally representative cohort of children from kindergarten through eighth grade. The ECLS-K is a school-based sample that initially included 21,410 kindergartners from 1280 public (72%) and private (28%) schools (cell sizes rounded to the nearest 10 in compliance with our restricted data agreement). To remain in the longitudinal sample, children must have been present in all six rounds of data collection between the fall of kindergarten and the spring of eighth grade. Therefore the 170 children who were added to the first grade sample to restore national representativeness are excluded from this analysis. In addition, the ECLS-K follow-up sampling frame included a number of eligibility changes and exclusions due to school transfers or deaths. Only a 50% subsample of the fall kindergarten baseline sample who transferred schools prior to each of the spring first grade, spring third grade, and spring fifth grade follow-ups were eligible for inclusion, reducing the eligible sample to 18,080 in first grade, 16,670 in third grade, 12,030 in fifth grade, and 11,930 in eighth grade. We also exclude 420 twins and higher-order births because they are at higher risk of low birth weight and other health outcomes and because the presence of twins may influence reports of children’s behaviors differently than if there were no twin in the household (Royer, 2009). Of the 11,930 kindergartners eligible for sampling in the eighth grade survey, 22% (n = 2670) of eligible children attrite from the sample entirely or otherwise were not present at one or more waves between the fall of kindergarten and eighth grade, resulting in an eighth grade sample of 9260.
As with longitudinal surveys more generally, this represents substantial sample attrition. Due to this notable sample attrition and to population composition changes in the U.S. since 1998–99, the eighth grade sample is therefore not nationally representative of all eighth graders in the U.S. in 2007–08. Instead, the eighth grade sample should be viewed as a nationally representative sample of kindergartners in 1998–99. Children who are retained in the sample through all six waves and are included in the eighth grade wave are more likely to be white, have mothers with slightly higher educational levels, and have slightly lower inattentive behavior scores at baseline. They are neither significantly different from the baseline sample in their baseline achievement scores in kindergarten nor in their kindergarten hyperactive/impulsive behaviors scores.
2.2. Measures
2.2.1. Math and reading achievement scores
Our dependent variables consisted of eighth grade math and reading standardized assessment scores measured in eighth grade (as outcome variables). Because problems in school achievement are often considered in ADHD evaluations, we additionally controlled for math and reading scores in kindergarten (Hinshaw and Scheffler, 2014; Spencer et al., 2007). Kindergarten scores were measured prior to or concurrent with diagnosis for children in our sample. These psychometrically validated tests were untimed and contained 50–70 items (Baker, 1993; Tourangeau et al., 2009). Reading assessments emphasized grade-appropriate reading skills/comprehension (Tourangeau et al., 2009). Math assessments measured grade-appropriate conceptual number sense, properties, and operations skills (Tourangeau et al., 2009).
2.2.2. Ascertainment of ADHD diagnosis
ADHD diagnosis was ascertained based on parent report of diagnoses received by the child between kindergarten and third grade. To limit misreporting, parents answered three questions: (1) “Has the child been evaluated by a professional in response to a problem in paying attention, learning, behaving, or in activity level?” (2) “Has the child received a diagnosis by this professional?” and; (3) “Was the diagnosis for ADHD, ADD, or hyperactivity?” Following prior research, we identified an ADHD diagnosis if the parent answered “yes”’ to all three survey questions (Biederman et al., 1993, 2004, 2006; Bussing et al., 2003; Faraone et al., 1995; Tourangeau et al., 2009).
2.2.3. Ascertainment of ADHD-related and comorbid oppositional defiant disorder (ODD) and conduct disorder (CD) behaviors
We measured ADHD severity at school and home using separate teacher and parent reports of the core behaviors of ADHD, drawing on items from the psychometrically validated Social Rating Scale (Morgan et al., 2013; Tourangeau et al., 2009). Behavior ratings from multiple reporters provide a more comprehensive profile of child behavior given that behaviors may vary across context (school versus home) and as a function of relationship to child/reference group for comparison (Johnston et al. 2013). The results in the main text average the subset of items broadly measuring the core symptoms of ADHD on a four-point scale (1 = “rarely” – 4 = “always”). Hyperactivity/impulsivity psychopathology averages two global items for the frequency with which the child is: (1) impulsive (acts without thinking) and (2) restless (overly active, cannot sit still). The inattention score averages two reverse-coded items measuring: (1) attention and (2) concentration skills. Results using the complete externalizing behaviors and approaches to learning scales available in the ECLS-K to approximate ADHD-related behaviors are reported in Online Appendix Table A.1.
The index of comorbid oppositional defiant disorder (ODD) and conduct disorder (CD) behaviors consists of the average frequency of: (1) fighting, (2) arguing, (3) throwing tantrums, (4) getting angry, (5) ease in joining in play (reverse-coded), (6) ability to make and keep friends (reverse-coded), and (7) positive interactions with peers (reverse-coded). We included separate parent- and teacher-reported ODD/CD behaviors scales, both measured on the same four-point scale and at the same time as the hyperactivity/impulsivity and inattention items described above (Efron et al., 2014; Swanson et al., 2001).
To ensure that behavior scores were not confounded by the influence of treatment and behavioral or special education services, assessments from the wave prior to ADHD diagnosis (46% from kindergarten, 54% from first grade) were used for children diagnosed with ADHD. First grade behavior assessments were used for children without an ADHD diagnosis. Additionally, sensitivity analyses showed that findings are robust to the choice of kindergarten or first grade behavior assessment (Elder, 2010; Evans et al., 2010). Because 14% of ADHD diagnoses were reported at the first kindergarten survey, we were unable to measure ADHD-related behaviors prior to diagnosis for this subset of diagnosed cases. However, sensitivity analyses displayed in Online Appendix Table A.2 indicated that exclusion of these cases left substantive conclusions unchanged.
2.2.4. Pharmacological treatment, behavioral counseling, and special education services
Items measuring receipt of treatment and services were fielded in first, third, fifth, and eighth grades. Parents indicated whether the child was “taking medication to control his/her behavior,” “receiving an individualized education program (IEP) or special education services” or “receiving behavioral counseling or therapy.” Few children received medication/treatment prior to or without an ADHD diagnosis. Children who did were likely treated due to diagnosis with a co-morbid condition.
2.2.5. Additional covariates/controls
We additionally controlled for many potential confounding behavioral, early achievement/cognitive development (discussed above), health, socioeconomic, and demographic factors shown in Table 1. In particular, the additional behavioral controls tapped into child and maternal depressive behaviors. This included a child internalizing behaviors score measured in the same waves as the ADHD-related behaviors scores described above. We also included a binary indicator for mother’s Center for Epidemiologic Studies-Depression (CES-D) symptoms score greater than a score of 10, the threshold for clinically significant depressive symptoms on the scale from 0 to 36 (Nord et al., 2004). In sensitivity analyses, we used the continuous measure for maternal depression score. Substantive findings did not change.
Table 1.
Sample characteristics, by severity of ADHD-related behaviors and ADHD diagnostic status.
| Variable | Less severe ADHD-related behaviors
|
More severe ADHD-related behaviors
|
Overall min | Overall max. | ||
|---|---|---|---|---|---|---|
| Diagnosed with ADHD (N = 90)
|
Undiagnosed with ADHD (N = 5810)
|
Diagnosed with ADHD (N = 260)
|
Undiagnosed with ADHD (N = 1670)
|
|||
| Displaying means or proportions (SD of means in parentheses) | ||||||
| Primary Outcome Variable | ||||||
| Average Reading Achievement Scores in 8th Grade (std.) | –0.41 (0.92) | 0.16 (0.94) | –0.54 (1.01) | –0.46 (1.00) | –3 | 3 |
| Average Math Achievement Scores in 8th Grade (std.) | –0.34 (0.94) | 0.15 (0.93) | –0.53 (0.98) | –0.44 (1.00) | –3 | 3 |
| Key Predictor Variables for ADHD-Related Behaviors | ||||||
| Hyperactivity Behaviors Score in First Grade/Wave Prior to Diagnosis (Parent) | 1.88 (0.63) | 1.66 (0.51) | 2.63 (0.77) | 2.27 (0.66) | 1 | 4 |
| Inattentive Behaviors Score in First Grade/Wave Prior to Diagnosis (Parent) | 2.35 (0.64) | 1.96 (0.63) | 2.76 (0.60) | 2.57 (0.59) | 1 | 4 |
| ODD or CD Score in First Grade/Wave Prior to Diagnosis (Parent) | 2.01 (0.39) | 2.00(0.40) | 2.55 (0.49) | 2.46 (0.49) | 1 | 4 |
| Hyperactivity Behaviors Score in First Grade/Wave Prior to Diagnosis (Teacher) | 1.57 (0.42) | 1.40 (0.40) | 2.42 (0.73) | 2.22 (0.65) | 1 | 4 |
| Inattentive Behaviors Score in First Grade/Wave Prior to Diagnosis (Teacher) | 2.14 (0.65) | 1.64 (0.66) | 2.86 (0.66) | 2.68 (0.67) | 1 | 4 |
| ODD or CD Score in First Grade/Wave Prior to Diagnosis (Teacher) | 1.94 (0.45) | 1.77 (0.51) | 2.70 (0.51) | 2.61 (0.46) | 1 | 4 |
| Key Predictor Variables-Other Measures of Child Behavior | ||||||
| Internalizing Behavior Problems Score (Teacher) | 1.64 (0.58) | 1.49 (0.49) | 1.79 (0.60) | 1.78 (0.62) | 1 | 4 |
| Control Variables | ||||||
| Average Reading Achievement Scores in Kindergarten (std.) | –0.28 (0.79) | 0.09 (0.98) | –0.45 (0.86) | –0.43 (0.97) | –4 | 4 |
| Average Math Achievement Scores in Kindergarten (std.) | –0.34 (0.78) | 0.17 (0.95) | –0.45 (0.92) | –0.40 (0.98) | –3 | 4 |
| Male | 0.66 | 0.45 | 0.76 | 0.63 | 0 | 1 |
| Black | 0.07 | 0.09 | 0.10 | 0.20 | 0 | 1 |
| Hispanic | 0.07 | 0.19 | 0.08 | 0.24 | 0 | 1 |
| White | 0.86 | 0.72 | 0.82 | 0.56 | 0 | 1 |
| Mother Has CES-D Score >9 (Clinically Depressive Symptoms) | 0.21 | 0.13 | 0.27 | 0.27 | 0 | 1 |
| Mother Has Less than a HS Education | 0.03 | 0.07 | 0.07 | 0.16 | 0 | 1 |
| Mother Has High School Education | 0.37 | 0.28 | 0.37 | 0.35 | 0 | 1 |
| Mother Has Completed Some College | 0.24 | 0.31 | 0.30 | 0.29 | 0 | 1 |
| Mother Has Completed Four Year College Degree or Higher | 0.36 | 0.34 | 0.27 | 0.21 | 0 | 1 |
| Current Age of Social Mother in Kindergarten | 34.17 (5.96) | 34.31 (6.02) | 33.30 (6.68) | 33.24 (6.97) | 18 | 80 |
| Household Income Below Federal Poverty Line in Kindergarten | 0.06 | 0.13 | 0.16 | 0.26 | 0 | 1 |
| Child Not Covered by Insurance in Kindergarten/First Wave Available | 0.10 | 0.17 | 0.10 | 0.17 | 0 | 1 |
| Lives in Midwest in Kindergarten/First Wave Available | 0.29 | 0.28 | 0.34 | 0.25 | 0 | 1 |
| Lives in West Near in Kindergarten/First Wave Available | 0.07 | 0.18 | 0.08 | 0.19 | 0 | 1 |
| Lives in Northeast in Kindergarten/First Wave Available | 0.22 | 0.21 | 0.14 | 0.17 | 0 | 1 |
| Lives in South in Kindergarten/First Wave Available | 0.43 | 0.32 | 0.42 | 0.37 | 0 | 1 |
| Child Born Weighing Less than 5.5 lbs (Low Birthweight) | 0.07 | 0.07 | 0.09 | 0.08 | 0 | 1 |
| Number of Other Children in Household in Kindergarten | 1.44 (1.14) | 1.53 (1.07) | 1.37 (1.00) | 1.50 (1.10) | 0 | 11 |
| Child Been in Childcare Outside Home in Kindergarten | 0.57 | 0.48 | 0.59 | 0.54 | ||
| Behavioral Treatments and Services | 0 | 1 | ||||
| Child Taking Medication for Health Problem at 5th or 8th Grade | 0.69 | 0.01 | 0.77 | 0.08 | 0 | 1 |
| Child in Counseling at 5th or 8th Grade | 0.10 | 0.01 | 0.19 | 0.03 | 0 | 1 |
| Child in Special Education at 5th or 8th Grade | 0.29 | 0.05 | 0.38 | 0.13 | 0 | 1 |
Data Source: Early Childhood Longitudinal Study, Kindergarten Cohort of 1998–1999 (ECLS-K).
Notes: Our working sample consists of the children eligible for the kindergarten, first, third, fifth, and eighth grade survey rounds with non-missing information on ADHD diagnosis between kindergarten and third grade and 8th grade reading and math scores. Sample sizes are rounded to the nearest 10 in accordance with NCES restricted data requirements. Multiple imputation was used to handle item-missingness on all other predictors.
2.3. Missing data
Of the 9260 kindergartners included in the eighth grade sample, 15.4% lacked complete information on key variables: eighth grade reading, eighth grade math, or ADHD diagnosis. Item-missingness on these covariates was more common among boys, African-Americans, and children with mothers with less than a college degree. We used multiple imputation of 20 datasets to address item-missingness on all covariates except ADHD diagnosis and eighth grade reading and math test scores, although these covariates are included in the imputation equation and then dropped before conducting analyses, following Von Hippel (2007). Our final analytic sample consisted of the 7830 children. Note that results using listwise deletion (or complete case analysis) are shown in Online Appendix Table A.3. Substantive conclusions are unchanged.
2.4. Data analysis
Viewing severity of ADHD-related behaviors along a spectrum of severity, all children were divided into two groups representing those with “less severe” and “more severe” ADHD-related behaviors based on whether the average of their standardized hyperactive/impulsive, inattentive, and ODD/CD behaviors scores fell above or below the 25th percentile of scores among diagnosed children.2 We then applied the same cut-point to children without an ADHD diagnosis in order to enable comparison of diagnosed and undiagnosed children with ADHD-related behaviors in the same severity group.3 In sensitivity analyses we additionally used several different measures to ensure choice of included measures did not drive results. These included: a) only the averaged standardized hyperactive/impulsive and inattentive behaviors scores, b) the averaged standardized hyperactive/impulsive and inattentive behaviors scores and the standardized early reading and math achievement scores, c) the averaged standardized hyperactive/impulsive, inattentive, and ODD/CD behaviors scores, and d) the complete externalizing behaviors and approaches to learning scores available in the ECLS-K. Results were similar across specifications.
Because we were agnostic as to the specific cut-points used to differentiate children by severity of ADHD-related behaviors, we varied our criteria for classification into “less severe” and “more severe” groups. Cut-points ranged from the 10th percentile to the 50th percentile of the averaged score of ADHD- and ODD-related behaviors among children diagnosed with ADHD. The magnitude of the diagnosis-achievement relationship decreased as the cut-point shifted rightward (e.g., the difference in the average diagnosis-achievement relationship by severity was largest using the 10th percentile as a cut-point and smallest using higher percentiles cut-points). For readability, we focused our reporting of results on those from the 25th percentile cut-point as this was in the middle of the range of cut-points we used (results using other cut-points are available upon request). Therefore, in the main text, children who are reported as diagnosed with ADHD were categorized as having less severe ADHD if their standardized ADHD-related behaviors score was in the bottom 25% of scores among diagnosed cases and as having more severe ADHD if their score was in the top 75% of diagnosed cases. In sensitivity analyses, we also explored classifying children into three or more severity groupings based on their ADHD-related behaviors score, but findings from these analyses suggested a two-group model accurately captures significant differences in the estimated relationships between an early ADHD diagnosis and academic achievement.
Our first set of analyses examined differential selection into ADHD diagnosis by severity of ADHD-related behaviors. We examined descriptive statistics stratified by severity group to see how observed factors like early cognitive development/ achievement, race/ethnicity, socioeconomic status, and maternal and child health shaped the probability of diagnosis differently for children with less severe compared to more severe ADHD-related behaviors. In supplementary analyses we estimated linear probability models (LPMs) predicting diagnosis by severity group (results are available from the authors upon request).
After examining the differential selection processes underlying diagnosis by ADHD severity, we then carried out a series of ordinary least squares (OLS) regressions within both ADHD severity group (i.e., sub-classification or stratification analysis) (Stuart et al., 2009). Regressions examined how the estimated ADHD diagnosis-achievement relationship varied based on the severity of ADHD and comorbid ODD/CD behaviors. Model estimates were clustered at the school level.
Sensitivity analyses excluded undiagnosed cases with behavior scores below the minimum observed for diagnosed cases in order to ensure a similar range of ADHD-related behaviors between diagnosed and undiagnosed children. Findings were robust to this trimming. Importantly, all analyses controlled for kindergarten academic achievement, as a measure of early cognitive development, as well as teacher- and parent-reported inattentive, impulsive/hyperactive, ODD/CD, and internalizing behaviors plus demographic controls (Stuart et al., 2009). These controls helped to isolate the effect of diagnosis from ADHD severity. Robustness checks using propensity score matching (using nearest neighbor matching) yielded similar results and are displayed in Online Appendix Figure A.1.
Finally, we examined whether receipt of medication, behavioral counseling, or special education services further moderated the magnitude of the diagnosis-achievement relationship among children in both severity groups. We did so by interacting the indicator for ADHD diagnosis with that for each form of treatment/service receipt reported in fifth or eighth grade (after diagnosis). This produced three categories: ‘diagnosed without treatment,’ ‘diagnosed with treatment,’ and ‘treatment without ADHD diagnosis’ (indicating the presence of another diagnosis besides ADHD or an ADHD diagnosis between third and eighth grade). Each of these was relative to the reference category of ‘undiagnosed with ADHD and untreated for ADHD’. Because medication treatment was the largest moderator of the diagnosis-achievement relationship, we report these interactions and show only main effects for behavioral counseling and special education services.
3. Results
3.1. Sample characteristics and factors driving selection into diagnosis by behavioral severity
Our first set of results describes the factors driving selection into diagnosis. Among the 350 children (4.5% of the total sample) diagnosed with ADHD between kindergarten and third grade (Table 1), we find notable compositional differences by ADHD severity. Reading and math achievement scores each averaged roughly 0.10–0.20 standard deviations higher among diagnosed children with less severe ADHD-related behaviors compared to diagnosed children with more severe ADHD-related behaviors in both kindergarten and eighth grade. Across both ADHD severity groups, children from more disadvantaged backgrounds were also less likely to be diagnosed: the majority of diagnosed children were male, white, had mothers with at least a high school degree, had household incomes above the Federal Poverty Level, and were covered by health insurance. Minority children and children from socioeconomically disadvantaged families had lower overall probabilities of diagnosis but were relatively more represented among children with more severe ADHD diagnoses.
Only 6% of diagnosed children with less severe ADHD-related behaviors lived in households with incomes below the Federal Poverty Level compared to 13% of their undiagnosed peers and 16% of diagnosed children with more severe ADHD-related behaviors. Overall, diagnosed children with both less severe and more severe ADHD-related behaviors were also more likely to be covered by health insurance. Only 10% of diagnosed children in both behavioral severity groups were without health insurance compared to 17% of undiagnosed children in each severity group.
3.2. Stratification analysis estimates of the diagnosis-achievement relationship
Estimates from stratified OLS regression analyses adjusting for early cognitive development/early achievement, severity of ADHD-related behaviors, and demographic controls are shown in Table 2. Consistent with hypothesis 1, both diagnosis-reading and diagnosis-math achievement relationships were large and negative among children with less severe ADHD-related behaviors. However, these magnitudes of association were at least 50% smaller among children with more severe ADHD-related behaviors. On average among children with less severe ADHD-related behaviors, an ADHD diagnosis was associated with a statistically significant –0.30 SD lower eighth grade reading score and a statistically significant –0.22 SD lower math achievement score, net of controls.4 Among children with more severe ADHD-related behaviors, those with an ADHD diagnosis scored on average –0.12 SD lower on reading than those without a diagnosis and –0.11 SD on math, and only the coefficient on reading is statistically significant. As shown in Online Appendix Figure A.1, nearest neighbor propensity score matching estimates followed a similar pattern of results compared to the OLS regression estimates (the main differences were a slightly substantively larger –0.37 SD estimated average treatment effect of an ADHD diagnosis on eighth grade reading and a larger but statistically non-significant –0.34 SD estimated effect on math among children with less severe ADHD-related behaviors).5
Table 2.
OLS estimates of the relationship between an early elementary school ADHD diagnosis and eighth grade reading or math achievement, by severity of ADHD-Related Behaviors.
| Less severe ADHD-related behaviors
|
More severe ADHD-related behaviors
|
|||||||
|---|---|---|---|---|---|---|---|---|
| (1)
|
(2)
|
(3)
|
(4)
|
|||||
| Reading
|
Math
|
Reading
|
Math
|
|||||
| Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | |
| ADD/ADHD Diagnosis | –0.30*** | (0.08) | –0.22** | (0.08) | –0.12* | (0.06) | –0.11 | (0.06) |
| ADHD-Related Behaviors | ||||||||
| Inattentive Behaviors Score (Parent) | –0.05** | (0.02) | –0.08*** | (0.02) | –0.07* | (0.03) | –0.12*** | (0.03) |
| Hyperactivity Behaviors Score (Parent) | –0.02 | (0.02) | 0.00 | (0.02) | –0.07* | (0.03) | –0.06* | (0.03) |
| ODD/CD Behaviors Score (Parent) | 0.02 | (0.03) | 0.02 | (0.02) | –0.03 | (0.04) | –0.02 | (0.04) |
| Inattentive Behaviors Score (Teacher) | –0.17*** | (0.02) | –0.18*** | (0.02) | –0.13*** | (0.03) | –0.20*** | (0.03) |
| Hyperactivity Behaviors Score (Teacher) | 0.02 | (0.03) | –0.01 | (0.03) | 0.01 | (0.03) | 0.02 | (0.03) |
| ODD/CD Behaviors Score (Teacher) | –0.02 | (0.02) | 0.02 | (0.03) | 0.01 | (0.05) | –0.06 | (0.05) |
| Internalizing Behaviors Score | –0.01 | (0.02) | –0.03 | (0.02) | –0.04 | (0.04) | –0.02 | (0.03) |
| Baseline Achievement/Early Cognitive Development | ||||||||
| Kindergarten Reading Achievement Score (std.) | 0.11*** | (0.02) | 0.06*** | (0.02) | 0.13*** | (0.03) | 0.05 | (0.03) |
| Kindergarten Math Achievement Score in (std.) | 0.26*** | (0.02) | 0.35*** | (0.02) | 0.25*** | (0.03) | 0.39*** | (0.03) |
| Child Controls | ||||||||
| Male | –0.09*** | (0.02) | 0.22*** | (0.02) | –0.04 | (0.04) | 0.19*** | (0.04) |
| Black | –0.38*** | (0.04) | 30.41*** | (0.04) | –0.50*** | (0.05) | –0.45*** | (0.05) |
| Hispanic | –0.10*** | (0.03) | –0.03 | (0.03) | –0.15** | (0.05) | 0.01 | (0.06) |
| Lives in Midwest in Kindergarten/First Wave Available | 0.05 | (0.03) | 0.01 | (0.04) | 0.07 | (0.05) | 0.03 | (0.05) |
| Lives in West Near in Kindergarten/First Wave Available | 0.01 | (0.04) | 30.01 | (0.04) | 0.05 | (0.06) | 30.05 | (0.07) |
| Lives in Northeast in Kindergarten/First Wave Available | 0.07* | (0.03) | 0.01 | (0.04) | 0.14** | (0.05) | 0.09 | (0.05) |
| Child Born Weighing Less than 5.5 lbs (LBW) | –0.01 | (0.04) | –0.05 | (0.04) | 0.13 | (0.07) | 0.05 | (0.06) |
| Child Not Covered by Insurance | 0.01 | (0.03) | 0.01 | (0.03) | 0.00 | (0.05) | 0.02 | (0.05) |
| HH Income Below Federal Poverty Line | –0.16*** | (0.04) | –0.07* | (0.03) | –0.14** | (0.05) | –0.11* | (0.05) |
| Number of Other Children in HH | –0.02 | (0.01) | 0.02 | (0.01) | –0.01 | (0.02) | 0.01 | (0.02) |
| Child Been in Childcare Outside Home | –0.05* | (0.02) | –0.04* | (0.02) | –0.04 | (0.04) | –0.02 | (0.04) |
| Mother Controls | ||||||||
| Mother Has HS Education | 0.22*** | (0.05) | 0.16** | (0.05) | 0.12* | (0.06) | 0.10 | (0.06) |
| Mother Has Completed Some College | 0.30*** | (0.05) | 0.27*** | (0.05) | 0.25*** | (0.06) | 0.23*** | (0.07) |
| Mother Has Completed Four Year College Degree | 0.56*** | (0.05) | 0.47*** | (0.05) | 0.52*** | (0.07) | 0.43*** | (0.07) |
| Current Mother Age at Kindergarten Round | 0.01** | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | –0.00 | (0.00) |
| Mother Has Clinically Depressive Symptoms at Kindergarten | –0.11*** | (0.03) | –0.08** | (0.03) | 0.00 | (0.04) | 0.04 | (0.04) |
| Constant | 0.10 | (0.11) | 0.08 | (0.11) | 0.25 | (0.25) | 0.67** | (0.24) |
|
| ||||||||
| N | 5890 | 5890 | 1930 | 1930 | ||||
| R Squared | 0.37 | 0.39 | 0.38 | 0.42 | ||||
p < 0.05,
p < 0.01,
p < 0.001.
Standard errors in parentheses.
Data Source: Early Childhood Longitudinal Study, Kindergarten Cohort of 1998–1999 (ECLS-K).
Notes: Our working sample consists of the children eligible for the kindergarten, first, third, fifth, and eighth grade survey rounds with non-missing information on ADHD diagnosis between kindergarten and third grade and 8th grade reading and math scores. Sample sizes are rounded to the nearest 10 in accordance with NCES restricted data requirements. Multiple imputation was used to handle item-missingness on all other predictors.
3.3. The ADHD diagnostic label and treatments or services: the roles of medication use, behavioral counseling, and special education services
Table 3 and Figs. 1-2 display OLS regression estimates of the diagnosis-achievement relationship and receipt of pharmacological treatment and behavioral/educational services following diagnosis. Consistent with hypothesis 2, neither pharmacological medication nor behavioral counseling offset most of the negative diagnosis-achievement relationships among children with less severe ADHD-related behaviors. Model (1) of Table 3 shows that, among children with less severe ADHD-related behaviors, both diagnosed and unmedicated and diagnosed and medicated children experienced on average –0.32 and –0.31 SD lower reading achievement than their undiagnosed, unmedicated counterparts with the same ADHD-related behaviors, early cognitive development/achievement, and demographic characteristics. Model (2) shows that, also as predicted, an ADHD diagnosis was not associated with lower math achievement among children with less severe ADHD-related behaviors who were unmedicated. By contrast, children with less severe ADHD-related behaviors who were diagnosed and medicated exhibited −0.29 SD lower math achievement, on par with that for reading.
Table 3.
OLS estimates of relationship between an early elementary school ADHD diagnosis and eighth grade reading or math achievement, controlling for treatments to help control behaviors, by severity of ADHD-Related behaviors (complete model results in Appendix Table A.6).
| Less severe ADHD-related behaviors
|
More severe ADHD-related behaviors
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1)
|
(2)
|
(3)
|
(4)
|
(5)
|
(6)
|
(7)
|
(8)
|
|||||||||
| Reading
|
Math
|
Reading
|
Math
|
Reading
|
Math
|
Reading
|
Math
|
|||||||||
| Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | Coef. | SE | |
| Diagnosed with ADHD, Medication (5th or 8th Grade) | –0.31** | (0.11) | –0.29** | (0.10) | –0.23* | (0.11) | –0.22* | (0.10) | –0.13 | (0.07) | –0.09 | (0.07) | –0.05 | (0.07) | –0.03 | (0.07) |
| Diagnosed with ADHD, No Medication | –0.32* | (0.13) | –0.08 | (0.16) | –0.27* | (0.13) | –0.04 | (0.16) | –0.26* | (0.11) | –0.26** | (0.10) | –0.20 | (0.11) | –0.20* | (0.10) |
| Not Diagnosed with ADHD, Medication (5th or 8th Grade) | –0.26** | (0.08) | –0.29** | (0.09) | –0.17 | (0.09) | –0.20* | (0.09) | –0.26** | (0.08) | –0.18* | (0.07) | –0.19* | (0.08) | –0.13 | (0.07) |
| Not Diagnosed with ADHD, No Medication | ||||||||||||||||
| Other Behavioral Treatments and Services (Main Effects) | ||||||||||||||||
| Counseling (5th or 8th Grade) | –0.20 | (0.11) | –0.17 | (0.13) | –0.01 | (0.09) | –0.00 | (0.10) | ||||||||
| Special Education (5th or 8th Grade) | –0.25*** | (0.05) | –0.24*** | (0.05) | –0.33*** | (0.05) | –0.28*** | (0.06) | ||||||||
| ADHD-Related Behaviors | ||||||||||||||||
| Inattentive Behaviors Score (Parent) | –0.05** | (0.02) | –0.08*** | (0.02) | –0.05** | (0.02) | –0.08*** | (0.02) | –0.06 | (0.03) | –0.11*** | (0.03) | –0.05 | (0.03) | –0.11*** | (0.03) |
| Hyperactivity Behaviors Score (Parent) | –0.02 | (0.02) | 0.00 | (0.02) | –0.02 | (0.02) | 0.01 | (0.02) | –0.06 | (0.03) | –0.05 | (0.03) | –0.04 | (0.03) | –0.04 | (0.03) |
| ODD/CD Behaviors Score (Parent) | 0.02 | (0.03) | 0.02 | (0.02) | 0.03 | (0.03) | 0.02 | (0.02) | –0.02 | (0.04) | –0.01 | (0.04) | –0.01 | (0.04) | –0.00 | (0.04) |
| Inattentive Behaviors Score (Teacher) | –0.16*** | (0.02) | –0.18*** | (0.02) | –0.15*** | (0.02) | –0.17*** | (0.02) | –0.12*** | (0.03) | –0.19*** | (0.03) | –0.11*** | (0.03) | –0.18*** | (0.03) |
| Hyperactivity Behaviors Score (Teacher) | 0.03 | (0.03) | –0.01 | (0.03) | 0.02 | (0.03) | –0.01 | (0.03) | 0.01 | (0.03) | 0.02 | (0.03) | 0.01 | (0.03) | 0.02 | (0.03) |
| ODD/CD Behaviors Score (Teacher) | –0.02 | (0.02) | 0.02 | (0.03) | –0.02 | (0.02) | 0.02 | (0.03) | 0.01 | (0.05) | –0.06 | (0.05) | 0.01 | (0.05) | –0.06 | (0.05) |
| Internalizing Behaviors Score | –0.01 | (0.02) | –0.03 | (0.02) | 0.00 | (0.02) | –0.02 | (0.02) | –0.03 | (0.04) | –0.02 | (0.03) | –0.01 | (0.03) | –0.00 | (0.03) |
| Baseline Achievement | ||||||||||||||||
| Kindergarten Reading Achievement Score (std.) | 0.12*** | (0.02) | 0.06*** | (0.02) | 0.11*** | (0.02) | 0.06*** | (0.02) | 0.13*** | (0.03) | 0.04 | (0.03) | 0.13*** | (0.03) | 0.05 | (0.03) |
| Kindergarten Math Achievement Score in (std.) | 0.26*** | (0.02) | 0.35*** | (0.02) | 0.25*** | (0.02) | 0.34*** | (0.02) | 0.25*** | (0.03) | 0.39*** | (0.03) | 0.23*** | (0.03) | 0.38*** | (0.03) |
|
| ||||||||||||||||
| N | 5890 | 5890 | 5890 | 5890 | 1930 | 1930 | 1930 | 1930 | ||||||||
| R Squared | 0.37 | 0.39 | 0.0.37 | 0.39 | 0.38 | 0.42 | 0.39 | 0.43 | ||||||||
p< 0.05,
p < 0.01
p < 0.001.
Standard errors in parentheses. All maternal and child controls shown in Table 2 are included in these models but not shown (see Appendix Table A.6 for complete model results).
Data Source: Early Childhood Longitudinal Study, Kindergarten Cohort of 1998–1999 (ECLS-K).
Notes: Our working sample consists of the children eligible for the kindergarten, first, third, fifth, and eighth grade survey rounds with non-missing information on ADHD diagnosis between kindergarten and third grade and 8th grade reading and math scores. Sample sizes are rounded to the nearest 10 in accordance with NCES restricted data requirements. Multiple imputation was used to handle item-missingness on all other predictors. All child and mother controls shown in Table 2 are included in these models but not shown (see Appendix for complete model results).
Fig. 1.
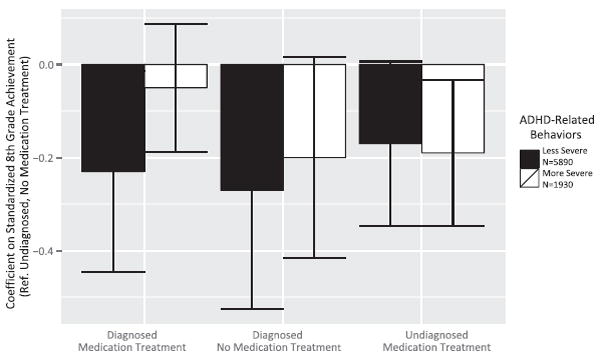
OLS estimates of the association between an early elementary school ADHD diagnosis, medication treatment, and eighth grade reading achievement, by severity of ADHD-related behaviors.
Data Source: Early Childhood Longitudinal Study, Kindergarten Cohort of 1998-1999 (ECLS-K).
Notes: Our working sample consists of the children eligible for the kindergarten, first, third, fifth, and eighth grade survey rounds with non-missing information on ADHD diagnosis between kindergarten and third grade and 8th grade reading and math scores. Sample sizes are rounded to the nearest 10 in accordance with NCES restricted data requirements. Multiple imputation was used to handle item-missingness on all other predictors.
Fig. 2.
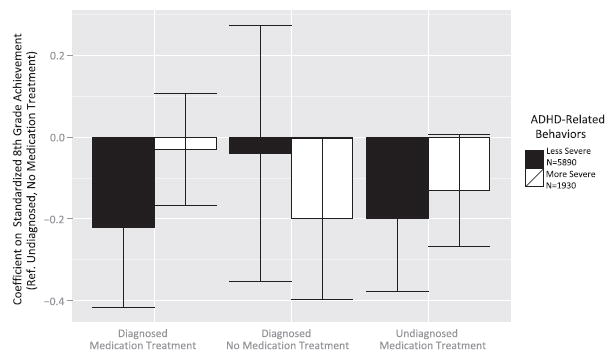
OLS estimates of the association between an early elementary school ADHD diagnosis, medication treatment, and eighth grade math achievement, by severity of ADHD-Related behaviors.
Data Source: Early Childhood Longitudinal Study, Kindergarten Cohort of 1998-1999 (ECLS-K).
Notes: Our working sample consists of the children eligible for the kindergarten, first, third, fifth, and eighth grade survey rounds with non-missing information on ADHD diagnosis between kindergarten and third grade and 8th grade reading and math scores. Sample sizes are rounded to the nearest 10 in accordance with NCES restricted data requirements. Multiple imputation was used to handle item-missingness on all other predictors.
This suggests that the process of receiving medication may serve an important role in the labeling process that triggers lowered achievement among diagnosed children with less severe ADHD-related behaviors, at least in terms of math achievement. In light of this finding, we conducted supplementary analysis to investigate selection into medication receipt among children with less severe ADHD-related behaviors. Results shown in Online Appendix Table A.5 indicate that medication treatment is quite evenly distributed across behavioral and cognitive achievement scores among children with less severe ADHD-related behaviors. Additionally, models interacting diagnosis * behavior/achievement scores (not shown) reveal that this pattern appears both among children diagnosed with ADHD between kindergarten and third grade and among those otherwise receiving medication (likely due to diagnosis with a co-morbid condition other than ADHD or with an ADHD diagnosis between third and eighth grades). These supplementary findings are consistent with the interpretation that the process of receiving medication may play an important role in triggering labeling. That is, they suggest there does not appear to be selection into treatment as a function of factors like behaviors and baseline achievement. At the same time, it is also possible that medication receipt itself is associated with lowered achievement due to factors like adverse side-effects of treatments. However, we are unable to identify the specific mechanism in effect.
Among children with more severe ADHD-related behaviors, an ADHD diagnosis without receipt of medication treatment was associated with –0.26 SD lower reading and math achievement (Models (5)–(6)). However, children with more severe ADHD-related behaviors who received both an ADHD diagnosis and medication treatment had reading and math scores statistically indistinguishable from undiagnosed, un-medicated peers. This suggests medication treatment is efficacious for children diagnosed with more severe ADHD-related behaviors.
Results lend support to the idea that the context of special education shapes the experience of the ADHD diagnostic label. Children in regular instruction classrooms who are diagnosed with ADHD and receiving medication on average score –0.23 SD lower in reading compared to children neither diagnosed nor medicated, net of the severity of their specific ADHD-related behaviors, cognitive impairments, and demographic traits (Model (3) of Table 3; full controls shown in Online Appendix Table A.6). Above and beyond their diagnostic and medication status, children in special education classrooms on average score –0.25 SD lower than children not in special education.6 This lower average reading achievement of children in special education may partly reflect the correlation between ADHD diagnosis with medication and receipt of special education (Model (1) versus Model (3)). However, only roughly 30% of diagnosed children with less severe ADHD-related behaviors are in special education while roughly 70% receive medication. In supplementary analyses we show these same results when excluding the indicator for receipt of behavioral counseling, which is not a statistically significant predictor of achievement.
Finally, results are consistent with hypothesis 3, that receipt of medication plays an important role in triggering negative labeling even among children diagnosed with another mental health condition other than ADHD (or among those diagnosed with ADHD between third and eighth grades). For example, Model (1) of Table 3 reveals that children with less severe ADHD-related behaviors who received medication treatment but were not diagnosed with ADHD by third grade nonetheless also scored on average –0.26 SD lower in reading than their undiagnosed, unmedicated counterparts with the same behaviors, early achievement, and demographic traits. A similar pattern is visible for math achievement (Model (2)). Although we lack specific information about the other conditions with which children were diagnosed, we find that even children with more severe ADHD-related behaviors who receive medication treatment for some other condition also experience significantly lower reading and math achievement (–0.26 SD and –0.18 SD), as shown in Models (5)–(6) of Table 3. We consider several possible explanations for this negative labeling in the discussion.
4. Discussion
Drawing on a nationally representative, longitudinal sample of U.S. kindergartners followed through eighth grade, this study finds results consistent with prior work: children with more severe ADHD-related behaviors fare worse academically than children with relatively less severe ADHD-related behaviors (Efron et al., 2014; Shaw et al., 2012; Stuart et al., 2009). However, this study also shows that, distinct from the effect of the severity of the ADHD-related behaviors themselves, there is a large negative estimated effect of the ADHD diagnosis for children with less severe ADHD-related behaviors. This finding is consistent with the possibility that, for children with relatively less severe ADHD-related behaviors, the negative social implications of an early childhood ADHD diagnosis may outweigh positive social implications (e.g., avoiding blaming the child for their academic difficulties) and the benefits of medication treatment or behavioral and educational services.
Our main innovation in this study is that we estimate the association between early elementary school ADHD diagnoses, as opposed to observed ADHD-related behaviors, and long-term academic achievement. This study’s use of a nationally representative, longitudinal kindergarten sample helps overcome selection bias due to sampling within a clinical setting, where children with severe ADHD-related behaviors tend to be overrepresented. The first key finding is that the estimated associations between an early ADHD diagnosis and math and reading achievement are substantially larger and negative for children with less severe ADHD-related behaviors relative to comparable children without an ADHD diagnosis. This finding holds across OLS and propensity score estimates of the diagnosis-achievement relationship for reading and is also robust across choice of ADHD-related behavioral controls. This finding is consistent with the hypothesis that the social label associated with the ADHD diagnosis has a large negative effect on later academic achievement, especially reading, for children with relatively less severe levels of ADHD-related behaviors. By contrast, the estimated effect of diagnosis is at least 50% smaller in magnitude and only statistically significant for reading scores among children with more severe ADHD-related behaviors. This finding also is consistent across estimation strategies and choice of behavioral controls.
The second part of the study turns to the role of treatments in offsetting the negative estimated association between an ADHD diagnosis and academic achievement among children with less severe ADHD-related behaviors. This study’s second key finding is that pharmacological treatment only offsets the majority of the negative diagnosis-achievement relationship among children diagnosed with more severe ADHD-related behaviors who receive medication treatment. By contrast, medication use does not offset the large, negative association between diagnosis and reading achievement. Among children with less severe ADHD-related behaviors, diagnosed children exhibit similarly low average levels of reading achievement as diagnosed, unmedicated children. In terms of math achievement, an ADHD diagnosis accompanied by medication use among children with less severe ADHD-related behaviors is associated with an even lower average math score compared to diagnosed but unmedicated children.
One possible explanation for these results is that medication use activates the negative ability label associated with an ADHD diagnosis. The negative ability label may be especially detrimental for the development of strong reading skills in elementary school, where extended concentration is particularly necessary. Necessary concentration may be interrupted due to the need to leave class in order to receive medication (Charach et al., 2013), or due to the psychological burden associated with the negative ability label. Another possible explanation, however, is that medication use lowers both reading and math achievement because of its direct effect on cognitive development. Some research shows that pharmacological treatments for mood disorders may have adverse effects such as lowered levels of cognitive development, which may manifest as lowered math and reading achievement (Barker et al., 2004; Wingo et al., 2009). Epilepsy medication is one concrete example of such a drug, however, prevalence of epilepsy is likely very low in this nationally representative sample, especially among children with less severe ADHD.
That medication treatment does not attenuate the diagnosis achievement association among children with less severe ADHD-related behaviors is consistent with prior work showing that the long-term efficacy of treatments on behavioral, social, and academic outcomes is unclear. For example, Scheffler et al. (2009b), Shaw et al. (2012), Molina et al. (2009), and Zoega et al. (2012) found that pharmacological treatment for ADHD was typically associated with some improvement in long-term academic outcomes, but not to the level of comparable neurotypical children. Bussing et al. (2012a) found a similar pattern for children receiving special education services.
The primary implication of this study’s findings is that, when deciding whether to make a positive ADHD diagnosis for children on the border of clinical and subclinical levels of ADHD-related behaviors and impairment, clinicians should consider the social aspects of an early childhood ADHD diagnosis. In particular, the social labeling that accompanies the diagnosis may outweigh the positive implications among children with less severe ADHD-related behaviors and impairment. However, a child’s specific social contexts need to be carefully considered in weighing the pros and cons of diagnosis.
This study has a number of important limitations. First, analyses rely on four broad items measuring ADHD-related behaviors and seven items measuring comorbid ODD/CD behaviors, far fewer than numbers used to diagnose ADHD and ODD or CD in the Diagnostic and Statistical Manual-Fourth Edition (American Psychiatric Association, 2000). We also lack information on ADHD sub-type and verification of diagnosis based on medical records. Estimates of the diagnosis-achievement relationship therefore assume no systematic differences in reporting on these global measures of inattention, hyperactivity, and oppositional-defiance than would be observed using validated ADHD and ODD/CD screeners (though Efron et al. (2014) do not detect differences in academic performance by ADHD subtype). To estimate the magnitude of potential bias, all five observed externalizing problems and all six approaches to learning (reverse-coded) items correlated with ADHD and ODD behaviors were used to test sensitivity of findings to the number and pattern of correlations across ADHD and ODD behaviors (Eisenberg and Schneider, 2007; Morgan et al., 2013; Tourangeau et al., 2009). Substantive conclusions did not change. Nevertheless, findings only generalize to children who display the broad inattentive, hyperactive/impulsive, and ODD/CD behaviors measured. Parental reports of ADHD diagnosis also do not specify precise timing of diagnosis. For the few children diagnosed in kindergarten, ADHD-related behaviors may have been reported after diagnosis and receipt of treatment/services. However, sensitivity analyses excluding these children did not alter substantive findings.
Second, this study’s findings are subject to omitted-variables bias due to the possibility of unobserved factors correlated with both an ADHD diagnosis and later academic outcomes. Although we control for baseline reading and math achievement, which is correlated with early IQ, maternal depression, and a host of other characteristics, possible omitted factors may remain. These may include poor executive functioning, child-teacher relationships, school tracking and curriculum, and school climate toward the treatment of child behavior problems. Estimates from this study may also be subject to bias due to measurement error. Our models do not control for all comorbid conditions (e.g., symptoms and/or diagnoses) of ADHD, including depression, learning disability, or autism spectrum disorders, which would ideally draw from medical records rather than parent report. Our estimates may overstate the diagnosis-achievement relationship if omitted comorbidities are highly correlated with both diagnosis and achievement.
Third, sub-classification analysis assumes that similar diagnosed and undiagnosed cases are being compared in the less severe and more severe categories and findings are not sensitive to the precise cut-points for the ADHD severity groups. Sensitivity analyses show that the diagnosis-achievement relationship is large and negative if the cut-point for less severe ADHD/ODD is set to the bottom fifth, fourth, or third of the sample, if baseline achievement is included in the stratification criteria, and if dissimilar undiagnosed cases are excluded.
Finally, roughly 20% of the baseline sample attrite from this study before eighth grade. To the extent attrition was non-random, estimates may over-represent groups with lower attrition rates, including females, whites, and children of mothers who are college graduates, covered by insurance, or above the federal poverty line. Although 20–40% attrition is typical for longitudinal studies of this size and time frame of follow-up (Scanlan et al., 1998), results based on multiple imputation of 20 datasets to address item-missingness and inverse-probability weights correcting for sampling design and attrition were substantively unchanged.
In light of these limitations, future work should consider how the ADHD diagnosis-achievement relationship varies by ADHD severity, subtype, family socioeconomic status, gender, and race/ethnicity. Future research should identify whether these and other possibly omitted factors bias results. It should also explicitly test the social mechanisms underlying the estimated negative effect of diagnosis for children with less severe ADHD-related behaviors. We suspect that the negative ADHD diagnosis-achievement relationship may be attributed to lower school attachment and lower self-esteem among children diagnosed with ADHD, or lower perceptions of their academic ability by teachers, parents, and the children themselves (Efron et al., 2014; Eisenberg and Schneider, 2007). Further research is necessary to investigate these possibilities.
Supplementary Material
Acknowledgments
Dr. Owens gratefully acknowledges support from Brown University and the Robert Wood Johnson Foundation Health and Society Scholars Program. Dr. Jackson acknowledges support from NIA Training Grants (University of Wisconsin: #T32 AG00129, Johns Hopkins: #T32 AG000247). The authors thank Dr. Paul Rathouz (University of Wisconsin) for statistical expertise and Jienian Zhang for research assistance.
Funding source
Funding for this study was obtained through the Robert Wood Johnson Foundation Health & Society Scholars Program and an NIH Training Grant through the Center for Demography and Ecology at the University of Wisconsin.
Footnotes
Abbreviations include: ADHD (attention deficit/hyperactivity disorder), ODD (oppositional defiant disorder), and CD (conduct disorder).
Henceforth, we refer to the combination of hyperactive/impulsive, inattentive, and ODD/CD behaviors as “ADHD-related behaviors” for short.
Because the majority of undiagnosed children fall into the less severe ADHD-related behaviors category, the less severe ADHD-related behaviors group is much larger in total size than the more severe ADHD-related behaviors group.
In supplementary OLS regressions predicting achievement among children in the less severe ADHD-related behaviors group, shown in Online Appendix Table A.4, we interact the indicator for ADHD diagnosis with each of the ADHD-related behavior scores, net of other controls. This helps us identify whether there is a gradient in the diagnosis-achievement relationship even among children with less severe ADHD. We find that the association between an ADHD diagnosis and both reading and math achievement do not vary statistically significantly by severity of ADHD-related behaviors among children with less severe ADHD. The exception is for teacher reported inattentive symptoms, for which higher levels of inattention are associated with a less pronounced negative labeling effect, holding all other factors constant.
All referenced appendix material is available via the online supplement.
We note, however, that supplementary models of achievement additionally including interactions between diagnosis and receipt of special education (and, separately, behavioral counseling) services, yield non-significant interactions. This indicates that achievement levels of diagnosed children with less severe ADHD-related behaviors do not differ significantly between those receiving versus not receiving special education/counseling. Nonetheless, the large, negative relationship between special education and achievement is consistent with the notion that children with less severe ADHD who are in special education do experience substantial negative labeling, though it is unclear whether this labeling is triggered by diagnosis, special education, or some combination.
Financial disclosure
Authors have no financial relationships relevant to this article to disclose.
Conflict of interest
Authors have no Conflicts of interest to disclose.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.ssresearch.2016.06.018.
References
- Angold A, Erkanli A, Egger HL, Costello E. Stimulant treatment for children: a community perspective. J Am Acad Child Adolesc Psychiatry. 2000;39(8):975–984. doi: 10.1097/00004583-200008000-00009. [DOI] [PubMed] [Google Scholar]
- Asherson P, Trzaskowski M. Attention-deficit/hyperactivity disorder is the extreme and impairing tail of a continuum. J Am Acad Child Adolesc Psychiatry. 2015;54(4):249–250. doi: 10.1016/j.jaac.2015.01.014. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision (Dsm-Iv-Tr) American Psychiatric Association; 2000. [Google Scholar]
- Baker PC. Nlsy Child Handbook: a Guide to the 1986-1990 National Longitudinal Survey of Youth Child Data 1993 [Google Scholar]
- Barker MJ, Greenwood KM, Jackson M, Crowe SF. Cognitive effects of long-term benzodiazepine use. CNS drugs. 2004;18(1):37–48. doi: 10.2165/00023210-200418010-00004. [DOI] [PubMed] [Google Scholar]
- Barry TD, Lyman RD, Klinger LG. Academic underachievement and attention-deficit/hyperactivity disorder: the negative impact of symptom severity on school performance. J Sch Psychol. 2002;40(3):259–283. [Google Scholar]
- Baughman FA., Jr . The ADHD Fraud: How Psychiatry Makes” Patients” of Normal Children. Trafford Publishing; 2006. [Google Scholar]
- Biederman J, Faraone SV, Milberger S, Doyle A. Diagnoses of attention-deficit hyperactivity disorder from parent reports predict diagnoses based on teacher reports. J Am Acad Child Adolesc Psychiatry. 1993;32(2):315–317. doi: 10.1097/00004583-199303000-00011. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Monuteaux MC, Grossbard JR. How informative are parent reports of attention-deficit/hyperactivity disorder symptoms for assessing outcome in clinical trials of long-acting treatments? a pooled analysis of parents’ and teachers’ reports. Pediatrics. 2004;113(6):1667–1671. doi: 10.1542/peds.113.6.1667. [DOI] [PubMed] [Google Scholar]
- Biederman J, Gao H, Rogers AK, Spencer TJ. Comparison of parent and teacher reports of attention-deficit/hyperactivity disorder symptoms from two placebo-controlled studies of atomoxetine in children. Biol Psychiatry. 2006;60(10):1106–1110. doi: 10.1016/j.biopsych.2006.03.036. http://dx.doi.org/10.1016/j.biopsych.2006.03.036. [DOI] [PubMed] [Google Scholar]
- Bokhari FAS, Schneider H. School accountability laws and the consumption of psychostimulants. J Health Econ. 2011;30(2):355–372. doi: 10.1016/j.jhealeco.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Brassett-Harknett A, Butler N. Attention-deficit/hyperactivity disorder: an overview of the etiology and a review of the literature relating to the correlates and lifecourse outcomes for men and women. Clin Psychol Rev. 2007;27(2):188–210. doi: 10.1016/j.cpr.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Bussing R, Mason DM, Leon CE, Sinha K. Agreement between CASA parent reports and provider records of children’s ADHD Services. J Behav Health Serv Res. 2003;30(4):462–469. doi: 10.1007/BF02287433. [DOI] [PubMed] [Google Scholar]
- Bussing R, Mason DM, Bell L, Porter P, Garvan C. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J Am Acad Child Adolesc Psychiatry. 2010;49(6):595–605. doi: 10.1016/j.jaac.2010.03.006. http://dx.doi.org/10.1016/j.jaac.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Koro-Ljungberg M, Noguchi K, Mason D, Mayerson G, Garvan CW. Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Soc Sci Med. 2012a;74(1):92–100. doi: 10.1016/j.socscimed.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Porter P, Zima BT, Mason D, Garvan C, Reid R. Academic outcome trajectories of students with ADHD does exceptional education status matter? J Emot Behav Disord. 2012b;20(3):131–143. [Google Scholar]
- Carpenter L, Austin H. How to be recognized enough to be included? Int J Incl Educ. 2008;12(1):35–48. [Google Scholar]
- Charach A, Carson P, Fox S, Usman Ali M, Beckett J, Lim CG. Interventions for preschool children at high risk for ADHD: a comparative effectiveness review. Pediatrics. 2013;131(5):1–21. doi: 10.1542/peds.2012-0974. [DOI] [PubMed] [Google Scholar]
- Currie J, Stabile M. Child mental health and human capital accumulation: the case of ADHD. J Health Econ. 2006;25(6):1094–1118. doi: 10.1016/j.jhealeco.2006.03.001. http://dx.doi.org/10.1016/j.jhealeco.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Efron D, Sciberras E, Anderson V, Hazell P, Ukoumunne OC, Jongeling B, Schilpzand EJ, Bisset M, Nicholson JM. Functional status in children with ADHD at Age 6-8: a controlled community study. Pediatrics. 2014;134(4):e992–e1000. doi: 10.1542/peds.2014-1027. http://dx.doi.org/10.1542/peds.2014-1027. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Schneider H. Perceptions of academic skills of children diagnosed with ADHD. J Atten Disord. 2007;10(4):390–397. doi: 10.1177/1087054706292105. [DOI] [PubMed] [Google Scholar]
- Elder TE. The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates. J Health Econ. 2010;29(5):641–656. doi: 10.1016/j.jhealeco.2010.06.003. http://dx.doi.org/10.1016/j.jhealeco.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans WN, Morrill MS, Parente ST. Measuring inappropriate medical diagnosis and treatment in survey data: the case of ADHD among school-age children. J Health Econ. 2010;29(5):657–673. doi: 10.1016/j.jhealeco.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Milberger S. How reliable are maternal reports of their children’s psychopathology? one-year recall of psychiatric diagnoses of ADHD Children. J Am Acad Child Adolesc Psychiatry. 1995;34(8):1001–1008. doi: 10.1097/00004583-199508000-00009. http://dx.doi.org/10.1097/00004583-199508000-00009. [DOI] [PubMed] [Google Scholar]
- Ghuman JK, Aman MG, Lecavalier L, Riddle MA, Gelenberg A, Wright R, Rice S, Ghuman HS, Fort C. Randomized, placebo-controlled, crossover study of methylphenidate for attention-deficit/hyperactivity disorder symptoms in preschoolers with developmental disorders. J child Adolesc Psychopharmacol. 2009;19(4):329–339. doi: 10.1089/cap.2008.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Scheffler RM. The ADHD Explosion: Myths, Medication, Money, and Today’s Push for Performance. Oxford University Press; 2014. [Google Scholar]
- Johnston D, Propper C, Pudney S, Shields M. Child mental health and educational attainment: multiple observers and the measurement error problem. J Appl Econ. 2013;29(6):880–900. [Google Scholar]
- Kiely B, Adesman A. What we do not know about ADHD… yet. Curr Opin Pediatr. 2015;27(3):395–404. doi: 10.1097/MOP.0000000000000229. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. In: Labeling and stigma. Scheid T, Brown T, editors. Cambridge University Press; New York: 2010. [Google Scholar]
- McLeod JD, Pescosolido BA, Takeuchi DT, White TF. Public attitudes toward the use of psychiatric medications for children. J Health Soc Behav. 2004;45(1):53–67. doi: 10.1177/002214650404500104. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132(1):85–93. doi: 10.1542/peds.2012-2390. http://dx.doi.org/10.1542/peds.2012-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller AK, Fuermaier ABM, Koerts J, Tucha L. Stigma in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2012;4(3):101–114. doi: 10.1007/s12402-012-0085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nord C, Edwards B, Hilpert R, Branden L, Andreassen C, Elmore A, Sesay D, Fletcher P, Green J, Saunders R. Early Childhood Longitudinal Study, Birth Cohort (Ecls-B): User’s Manual for the Ecls-B Nine-month Restricted-use Data File and Electronic Code Book (Nces 2004-092) National Center for Education Statistics 2004 [Google Scholar]
- Olfson M, Gameroff MJ, Marcus SC, Jensen PS. National trends in the treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160(6):1071–1077. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, McLeod J, Alegria M. Confronting the second social contract: the place of medical sociology in research and policy for the twenty-first century. Handb Med Sociol. 2000:399–426. [Google Scholar]
- Pescosolido BA, Jensen PS, Martin JK, Perry BL, Olafsdottir S, Fettes D. Public knowledge and assessment of child mental health problems: findings from the national stigma study-children. J Am Acad Child Adolesc Psychiatry. 2008;47(3):339–349. doi: 10.1097/CHI.0b013e318160e3a0. [DOI] [PubMed] [Google Scholar]
- Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J Clin Child Psychol. 2001;30(4):503–513. doi: 10.1207/S15374424JCCP3004_07. [DOI] [PubMed] [Google Scholar]
- Rappley MD, Mullan PB, Alvarez FJ, Eneli IU, Wang J, Gardiner JC. Diagnosis of attention-deficit/hyperactivity disorder and use of psychotropic medication in very young children. Arch Pediatr Adolesc Med. 1999;153(10):1039–1045. doi: 10.1001/archpedi.153.10.1039. [DOI] [PubMed] [Google Scholar]
- Rennie B, Beebe-Frankenberger M, Swanson HL. A longitudinal study of neuropsychological functioning and academic achievement in children with and without signs of attention-deficit/hyperactivity disorder. J Clin Exp Neuropsychol. 2014;36(6):621–635. doi: 10.1080/13803395.2014.921284. http://dx.doi.org/10.1080/13803395.2014.921284. [DOI] [PubMed] [Google Scholar]
- Royer H. Separated at girth: US twin estimates of the effects of birth weight. Am Econ J Appl Econ. 2009;1(1):49–85. [Google Scholar]
- Rucklidge JJ, Tannock R. Psychiatric, psychosocial, and cognitive functioning of female adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2001;40(5):530–540. doi: 10.1097/00004583-200105000-00012. [DOI] [PubMed] [Google Scholar]
- Scanlan TM, Hauser RM, West KK. Longitudinal Surveys of Children. National Academies Press; 1998. [Google Scholar]
- Scheffler RM, Brown TT, Fulton BD, Hinshaw SP, Levine P, Stone S. Positive association between attention-deficit/hyperactivity disorder medication use and academic achievement during elementary school. Pediatrics. 2009a;123(5):1273–1279. doi: 10.1542/peds.2008-1597. http://dx.doi.org/10.1542/peds.2008-1597. [DOI] [PubMed] [Google Scholar]
- Scheffler RM, Brown TT, Fulton BD, Hinshaw SP, Levine P, Stone S. Positive association between attention-deficit/hyperactivity disorder medication use and academic achievement during elementary school. Pediatrics. 2009b;123(5):1273–1279. doi: 10.1542/peds.2008-1597. [DOI] [PubMed] [Google Scholar]
- Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, Arnold LE. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med. 2012;10(1):99–114. doi: 10.1186/1741-7015-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh I. Boys will be boys: fathers’ perspectives on ADHD symptoms, diagnosis, and drug treatment. Harv Rev Psychiatry. 2003;11(6):308–316. [PubMed] [Google Scholar]
- Singh I. Clinical implications of ethical concepts: moral self-understandings in children taking methylphenidate for ADHD. Clin Child Psychol Psychiatry. 2007;12(2):167–182. doi: 10.1177/1359104507075920. [DOI] [PubMed] [Google Scholar]
- Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. J Pediatr Psychol. 2007;32(6):631–642. doi: 10.1093/jpepsy/jsm005. [DOI] [PubMed] [Google Scholar]
- Stuart EA, Marcus SM, Horvitz-Lennon MV, Gibbons RD, Normand SLT. Using non-experimental data to estimate treatment effects. Psychiatr Ann. 2009;39(7):41451. doi: 10.3928/00485713-20090625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and odd symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40(2):168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- Tourangeau K, Nord C, Le T, Sorongon AG, Najarian M. Early Childhood Longitudinal Study, Kindergarten Class of 1998-99 Ecls-K Combined User’s Manual for the Ecls-K Eighth-grade and K-8 Full Sample Data Files and Electronic Codebooks. Nces 2009-004. National Center for Education Statistics; 2009. [Google Scholar]
- Travell C, Visser J. ADHD does bad stuff to you’: young people’s and parents’ experiences and perceptions of attention deficit hyperactivity disorder (ADHD) Emot Behav Difficult. 2006;11(3):205–216. [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Perou R, Blumberg SJ. Convergent validity of parent-reported attention-deficit/hyperactivity disorder diagnosis: a cross-study comparison. JAMA Pediatr. 2013;167(7):674–675. doi: 10.1001/jamapediatrics.2013.2364. http://dx.doi.org/10.1001/jamapediatrics.2013.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Bitsko RH, Danielson ML, Perou R, Blumberg SJ. Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among childrend–United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep. 2010;59(44):1439–1443. [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1):34–46. e2. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Hippel PT. Regression with missing Ys: an improved strategy for analyzing multiply imputed data. Sociol Methodol. 2007;37(1):83–117. [Google Scholar]
- Wingo AP, Wingo TS, Harvey PD, Baldessarini RJ. Effects of lithium on cognitive performance: a meta-analysis. J Clin psychiatry. 2009;70(11):1588–1597. doi: 10.4088/JCP.08r04972. [DOI] [PubMed] [Google Scholar]
- Wolraich ML. Primary care providers and childhood mental health conditions. Pediatrics. 2000;105(Suppl. 3):963–963. [PubMed] [Google Scholar]
- Zito JM, Safer DJ, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA. 2000;283(8):1025–1030. doi: 10.1001/jama.283.8.1025. [DOI] [PubMed] [Google Scholar]
- Zoega H, Rothman KJ, Huybrechts KF, Olafsson O, Baldursson G, Almarsdottir AB, Jonsdottir S, Halldorsson M, Hernandez-Diaz S, Valdimarsdottir UA. A population-based study of stimulant drug treatment of ADHD and academic progress in children. Pediatrics. 2012;130(1):e53–62. doi: 10.1542/peds.2011-3493. http://dx.doi.org/10.1542/peds.2011-3493. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


