Abstract
Purpose
To characterize the prevalence of and contributing factors to adult obesity in the most common recurrent copy number variation (CNV), 22q11.2 deletion, given that other rare CNVs are known to have obesity phenotypes.
Methods
For 207 adults with 22q11.2 deletion syndrome (22q11.2DS), we used available height and weight measurements to calculate body mass index (BMI) and recorded associated factors that could play a role in obesity. We used maximum BMI per subject and logistic regression to test a model predicting obesity class.
Results
The prevalence of obesity (BMI≥30) in 22q11.2DS (n=90, 43.5%; at median age 26.7 years) was significantly greater than for Canadian norms (OR 2.30, 95%CI=1.74–3.02, p<0.0001), even after excluding individuals with a history of antipsychotic use. The regression model was significant (P<0.0001). Psychotropic medication use and age, but not sex or presence of intellectual disability, were associated with higher obesity level. Ten (4.8%) individuals were diagnosed with type 2 diabetes at median age 39.5 years; prevalence was higher in those with obesity (P<0.01).
Conclusion
The results suggest that adult obesity is related to the 22q11.2 deletion. The findings expand the potential genetic causes of obesity and have important implications for management of 22q11.2DS.
Keywords: DiGeorge syndrome, hypothyroidism, congenital heart disease, energy metabolism, copy number variation
INTRODUCTION
Rare copy number variations (CNVs) are known to contribute to obesity.1–3 There are limited data, however, on obesity for the recurrent pathogenic 22q11.2 deletion. Studies examining body mass index (BMI) in 22q11.2 deletion syndrome (22q11.2DS) (OMIM 188400/192430) have focused primarily on children.4–7 Early growth faltering,4–7 possibly associated with congenital heart disease (CHD),6 does not appear to persist over time.4–7 Some studies have suggested a trend toward increased weight and obesity in adolescence and adulthood4,7 but numbers of adults studied are small.5–7 An early report on 78 adults with 22q11.2DS suggested that obesity may be an associated feature8 but contributors to obesity were not examined. These are important considerations, given that some of the common features of 22q11.2DS,8,9 such as intellectual disability, hypothyroidism and psychotic illness, including schizophrenia in ~25% of adults, are also independently associated with obesity. Antipsychotic medications are known to be associated with weight gain and risk for type 2 diabetes in the general population.10,11
We sought to characterize the adult prevalence of and contributors to obesity in 22q11.2DS, and to determine the prevalence of type 2 diabetes. We hypothesized that the prevalence of obesity would be greater in 22q11.2DS than in the general population, and that variables that are predictive of obesity in the general population would similarly be contributors to obesity in 22q11.2DS.
MATERIALS AND METHODS
Subjects
The sample comprised 207 adults (96 males) with 22q11.2DS from a well-characterized Canadian cohort,8,12,13 where adult BMI data were available (measured at ≥18 years of age). 22q11.2 deletions were confirmed by standard molecular methods.8,12 The study was approved by local research ethics boards and written informed consent was obtained for each subject. As previously described,8,12 most subjects were ascertained through adult congenital cardiac, psychiatric, and/or genetics services.
Obesity prevalence
We used available lifetime medical records for all subjects to record objective measurements of height and weight, converting inches to centimeters and pounds to kilograms where necessary. Using the date of assessment and the subject’s date of birth, we calculated age at assessment. For BMI we used the standard formula . We excluded any BMI measurements calculated when the subject was >3 months pregnant and up to 6 months following either delivery or late miscarriage/termination. We calculated a total of 1168 adult BMI measurements (median 4, range 1–28, per subject) for the 207 subjects; 186 (90%) had more than one BMI measurement available. To evaluate lifetime obesity, we used the maximum available adult BMI for each subject to assign the level of obesity according to the four standard categories: not obese (BMI<30), obese class I (35>BMI≥30), obese class II (40>BMI≥35), and obese class III (BMI≥40).14
We calculated 95% confidence intervals for the prevalence estimates of obesity in our population using the formula in Richardson et al. (2000).15 The median year at maximum BMI measurement was 2011 (range 1986–2015). For comparison, we used the most recently reported population prevalence data for obesity measured in Canadian adults (≥18 years), excluding pregnant females, in 2008.16
Contributing factors to obesity
To avoid model overfitting and to focus on clinically important associations, we only considered variables for which we had a priori suspicion of a relationship to BMI based on general population data and/or if the variable was a major clinical feature of 22q11.2DS.8,9 We included variables that were present in ≥5 subjects. We defined lifetime history to mean presence at or before the time of maximum BMI measurement. These variables were coded as absent if they were only observed or diagnosed after maximum BMI measurement because we were interested in contributing factors to obesity rather than downstream consequences.
We considered age at assessment, sex, lifetime history of smoking (defined here as at least weekly use), presence of CHD of any severity from simple (e.g. septal defect) to complex (e.g. tetralogy of fallot with pulmonary atresia),17 presence of intellectual disability18 (mild to severe), lifetime history of diagnosed hypothyroidism,19 and lifetime use of psychotropic medications associated with weight gain (antipsychotics, selective serotonin reuptake inhibitors, valproic acid, venlafaxine, lithium).10,11,20,21 There was substantial overlap in use of psychotropic medications within patients. We considered psychotropic medication use as a single factor in order to avoid multicolinearity while accounting for the maximal potential effect of any of these medications in the model. Given that smoking in conjunction with antipsychotic use has been previously associated with less weight gain,22 we also considered psychotropic medications and smoking together as an interaction term in the model. There were 202 subjects with sufficient data available to assess all contributing factors considered. The remaining five subjects were in the non-obese category.
Obesity and type 2 diabetes
With respect to potential consequences of obesity, we recorded the presence of type 2 diabetes, the age at diagnosis, and whether the subject had a history of a psychotic disorder and/or psychotropic medication use before diagnosis of diabetes.
Statistical analyses
We used an ordinal logistic regression model to identify clinical and demographic variables that were contributory factors to maximum BMI obesity class. We selected this analytic method based on consistency with existing literature, a greater level of detail than binomial logistic regression and fewer assumptions than multiple linear regression. We reported odds ratios and 95% confidence intervals (95% CI). All psychotropic medications showed the same direction of effect when examined individually. The variance inflation factor for each predictor included in the analysis was examined to ensure there were no problems with multicollinearity. Pairwise interactions between predictor variables were investigated one at a time by running smaller models consisting of the two predictor terms and the corresponding interaction term. Significant interaction terms were then verified as important after accounting for the other variables of interest. Post hoc X2 or Fisher’s exact tests were used to further characterize significant effects, and the prevalence of obesity in relation to type 2 diabetes. All statistical analyses were carried out in SAS 9.4 (SAS institute, Cary, NC). Statistical significance was defined by a P value <0.05.
RESULTS
Prevalence of obesity in 22q11.2DS
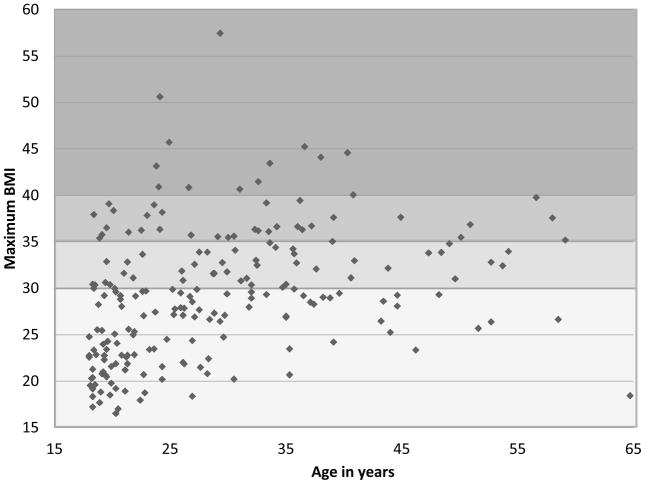
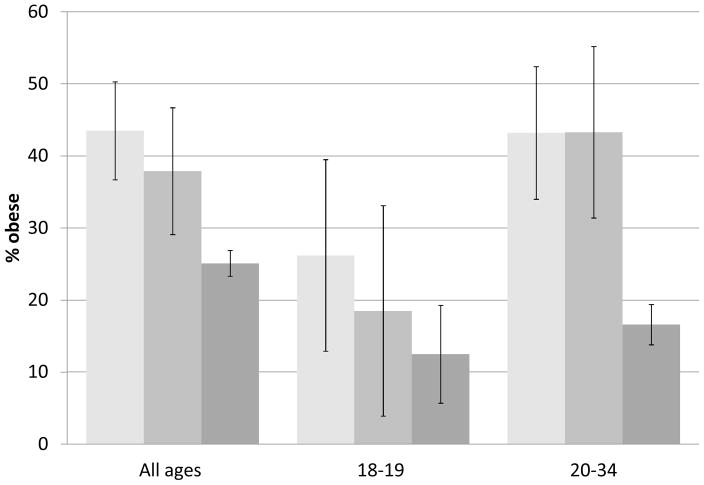
For the 207 adults with 22q11.2DS studied, the median BMI was 29.2 (range 16.5–57.5), assessed at median age 26.7 (range 18.0–64.7) years (Figure 1). The prevalence of obesity was 43.5% (n=90), with 21.3% (n=44) having class I, 15.9% (n=33) class II and 6.3% (n=13) class III obesity. The prevalence of obesity across all classes was significantly greater than that reported for the Canadian adult population (OR 2.30, 95% CI 1.74–3.02, P<0.0001), even after excluding those with antipsychotic medication use (OR 1.82, 95% CI 1.25–2.65, P=0.002) (Figure 2). Using the age sub-groupings provided for Canadian population norms, and where data were sufficient (>20 subjects) in the 22q11.2DS sample, we found that for the 20–34 year group obesity prevalence was significantly greater in 22q11.2DS (OR 3.82, 95% CI 2.57–5.66, P=0.0009); results were non-significant for the 18–19 year group when restricted to those with no antipsychotic medication exposure (Figure 2).
Figure 1. Maximum BMI in 207 adults with 22q11.2DS, by age.
Scatterplot of maximum BMI and age at assessment for 207 adults with 22q11.2DS. Colored panels from bottom to top indicate four BMI classes:14 not obese (green), class I (yellow), class II (yellow-orange) and class III obesity (orange). The “not obese” category includes eight subjects with maximum BMI <18.5 who would be considered underweight.
Figure 2. Obesity prevalence in 22q11.2DS compared to Canadian norms.
Bar graph illustrating the obesity prevalence in 22q11.2DS, with (dark yellow) and without (pale yellow bar) history of antipsychotic use, compared to the reported obesity prevalence in the general Canadian population (mauve bar).16 Error bars represent 95% confidence intervals calculated based on Richardson et al. (2000),15 or as provided for Canadian norms.16 Also displayed are data for the age groups reported by Statistics Canada16 where the number of subjects was >20 for 22q11.2DS, including the subgroup with no antipsychotic use, i.e. 18–19 years and 20–34 years of age.
Contributing factors to obesity
The logistic regression model predicting BMI class (Table 1) in adults with 22q11.2DS was significant (likelihood ratio test: X2=49.71, df=8; P<0.0001). Lifetime use of psychotropic medications and older age were associated with higher BMI class. Results for psychotropic medication use remained significant if medications were restricted to antipsychotics (OR=2.60, 95% CI=1.31–5.13, P=0.006). The interaction variable of psychotropic medication use and smoking was associated with a lower BMI class. Neither sex nor presence of intellectual disability were significant predictors, even when considered in single variable models (data not shown) (Figure S1).
Table 1.
Contributing factors to obesity in 202 adults with 22q11.2DS
| Distribution of features by level of obesitya | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not obese | Obesity class | ||||||||||||
| n=202 | n=112 | I n=44 |
II n=33 |
III n=13 |
Logistic regression analysis | ||||||||
| Contributing factors | n | n | % | n | % | n | % | n | % | OR | 95% CI | P | |
| Male sex | 94 | 54 | 48.2 | 20 | 45.5 | 15 | 45.5 | 5 | 38.5 | 1.06 | 0.60 | 1.88 | 0.836 |
| Intellectual disabilityb | 117 | 71 | 63.4 | 19 | 43.2 | 21 | 63.6 | 6 | 46.2 | 0.83 | 0.46 | 1.48 | 0.524 |
| Hypothyroidism | 39 | 16 | 14.3 | 9 | 20.5 | 9 | 27.3 | 5 | 38.5 | 1.88 | 0.94 | 3.77 | 0.076 |
| CHDb | 114 | 64 | 57.1 | 21 | 47.7 | 19 | 57.6 | 10 | 76.9 | 1.82 | 0.99 | 3.34 | 0.053 |
| Psychotropic medicationsc | 119 | 54 | 48.2 | 29 | 65.9 | 27 | 81.8 | 9 | 69.2 | 3.88 | 1.93 | 7.82 | <0.001 |
| Smoking | 42 | 30 | 26.8 | 6 | 13.6 | 4 | 12.1 | 2 | 15.4 | 1.08 | 0.32 | 3.62 | 0.901 |
| Psychotropic medications x Smoking | 28 | 21 | 18.8 | 3 | 6.8 | 3 | 9.1 | 1 | 7.7 | 0.13 | 0.03 | 0.60 | 0.009 |
| Med | IQR | Med | IQR | Med | IQR | Med | IQR | ||||||
| Age at assessment (y) | 23.1 | 9.8 | 31.4 | 12.5 | 32.3 | 14.2 | 31.0 | 11.7 | 1.06 | 1.03 | 1.10 | <0.0001 | |
Not obese (BMI<30), class I (35>BMI≥30), class II (40>BMI≥35), and class III (BMI≥40) obesity
For details, see text
Lifetime use of antipsychotics, selective serotonin reuptake inhibitors, valproic acid, venlafaxine, or lithium. Of 119 subjects with a history of psychotropic medication use, 87 (73.1%) had a history of antipsychotic, with (n=70) or without (n=17), other medication use. 32 (26.9%) subjects had a history of one or more of the other psychotropic medications listed. Overall, 82 had a history of SSRI, 35 valproic acid, 12 venlafaxine and 9 lithium use.
Med: median, IQR: interquartile range, OR: odds ratio, CI: confidence interval, P: p-value, y: years.
Although neither CHD nor hypothyroidism alone were significant variables (Table 1), when present together (n=17) the interaction variable was significantly associated with higher BMI class (OR=7.07, 95% CI=1.83–27.22, P<0.01), even after accounting for the other factors (data not shown). Post hoc analyses revealed that the association was only present at more severe levels of obesity: class II (FET, P=0.001) and class III (FET, P=0.015). There were no other significant pairwise interaction terms among the seven predictors.
Prevalence of type 2 diabetes
Ten subjects (4.8%) had a diagnosis of type 2 diabetes, diagnosed at a median age of 39.5 (range 27–59) years; the three individuals with class III obesity were all diagnosed before age 35 years. The prevalence of type 2 diabetes was significantly higher in obese (9/90, 10.0%) than in non-obese subjects (1/117, 0.9%: FET P=0.003). Nine (90.0%) of the 10 individuals with type 2 diabetes had a psychotic illness, and the prevalence of type 2 diabetes among those with a psychotic disorder was 10.1% (9/89).
DISCUSSION
The results of this study suggest that obesity is a common adult manifestation of 22q11.2DS. Consistent with our hypothesis, the prevalence of obesity was significantly greater in 22q11.2DS than in the general Canadian population. Although the presence and severity of obesity appeared to be influenced by some of the same factors as for general population studies of obesity, the effects of the 22q11.2 deletion were evident as significantly elevated levels of obesity by early adulthood in the absence of these factors.16,23
Pediatric data available for 22q11.2DS has indicated a trend to increasing weight in late adolescence.4–7 Divergence from normal curves begins around 10–12 years of age with an ever-widening gap through adolescence.6 Consistent with a later onset of obesity than that found associated with some other rare CNVs,2 we found that obesity prevalence was not significantly elevated in the 18–19 year old age group in the absence of antipsychotic medication exposure compared to population norms,16 but significant differences were apparent for the 20–34 year old group (Figure 2). Obesity in 22q11.2DS appears in the context of evidence of early growth abnormalities in terms of undergrowth, including elevated prevalence of being small for gestational age5,13 and early growth faltering.4–7 This is consistent with reported patterns in other genomic disorders, including other recurrent deletions such as 16p11.2 deletions3 and Prader-Willi syndrome.24 Later onset of obesity in 22q11.2DS may be why 22q11.2 deletions have not been identified in studies of early onset obesity.25 Interestingly, the findings for type 2 diabetes, while lower in prevalence, appeared similar in age at onset to those for adults with Prader-Willi syndrome.1 The median age of diagnosis for type 2 diabetes in 22q11.2DS was 39.5 years, younger by over 14 years than that for all types of diabetes reported for adults in the general US population (54.2 years).26
The results suggest that psychotic illness associated with 22q11.2DS may contribute to the obesity observed. With respect to antipsychotic medication, the results for 22q11.2DS (OR=2.60) appear comparable to those observed in idiopathic schizophrenia, where 2 to 2.8-fold increases in obesity prevalence have been reported.27,28 This is consistent with previous findings for the antipsychotic clozapine that indicated similar weight gain findings for 22q11.2DS and others with schizophrenia.29 The prevalence of type 2 diabetes among adults with 22q11.2DS and a history of psychotic illness (10.1%) was also similar to that reported for idiopathic schizophrenia (10.9%).30 The stronger result (OR=3.89) when all psychotropic medications were considered, and the fact that the prevalence of obesity remained significantly higher for adults with 22q11.2DS than Canadian norms in the absence of any antipsychotic exposure, indicate that other factors are important in the relationship of obesity to 22q11.2DS. As reported for recurrent 16p11.2 deletions,3 presence of intellectual disability was not associated with obesity in 22q11.2DS.
Advantages and limitations
To our knowledge, this sample represents the largest cohort of adults for a study of obesity for any recurrent CNV, including 16p11.2 deletions and Prader-Willi syndrome.1,3 Nonetheless, data points are still fairly scarce over age 40 years. This may explain why we did not detect an effect of sex on obesity, as this emerges at ~age 35 years in the general population.31 As for all cross-sectional, retrospective studies, it is difficult to draw causal inferences and to eliminate bias. We attempted to account for the maximal effect of each contributing factor on obesity through using maximum BMI and only examining the presence of factors prior to the maximum BMI. We cannot rule out, however, that for some factors variability in the onset and duration of exposures could have affected results. We were unable to evaluate pediatric factors such as undergrowth and feeding difficulties due to limitations in retrospective data. We also did not include palatal anomalies in this study, most of which were repaired,8 and in a previous study reported to be unrelated to pediatric growth abnormalities.6 Most subjects were assessed using FISH and typical probes that would not allow analyses targeted to specific deletion extent. Excluding the four subjects assessed by microarray to have shorter nested 22q11.2 deletions from the regression analysis and population comparisons made no material difference to the main results. Future studies using larger samples with detailed molecular characterization may enable stratification based on the 22q11.2 deletion extent to determine whether the prevalence of obesity differs between those with proximal or nested deletions, compared to those with the typical A–D deletion present in 85–90% of individuals with 22q11.2DS.
Implications and future directions
The results of the current study, together with available pediatric growth curve data,5–7 support early (e.g., from age 12 years) and ongoing attempts to encourage healthy diet and exercise behaviors in 22q11.2DS. The involvement of a dietitian may be helpful, particularly in the context of other factors such as treatment with antipsychotic and other psychotropic medications. General clinical practice guidelines for schizophrenia would include active monitoring for weight gain and metabolic side effects. Medication choice should include balancing efficacy and side effects.29 Metabolic and motor considerations may both be of concern in 22q11.2DS given the predisposition to obesity and to movement disorders.32,33 The results also suggest that extra attention to metabolic control may be needed for adults with hypothyroidism, especially in the presence of congenital cardiac disease. Obesity is common amongst individuals with intellectual disability in the general population.34 Although intellectual disability was not a contributing factor in the regression analysis, most individuals with a recurrent 22q11.2 deletion have intellectual functioning that is below the average and thus issues related to intellectual functioning may not be readily separable from the effect of the 22q11.2 deletion itself. Nonetheless, intellectual level may pose a challenge to management of obesity (Figure S1).
Our results expand the potential genetic causes of obesity to include recurrent 22q11.2 deletions. The similarities and differences to other obesity associated recurrent CNVs may be fruitful avenues for future research efforts. These would include satiety responsiveness,35 the trajectory of weight gain for individuals, and the development of obesity-related complications, including mortality.33,36 In addition to dosage decreases in the respective microdeletion regions, there may be contributing genetic factors and pathways to obesity expression that converge for CNVs with obesity phenotypes.25,37 Animal models of deletions and reciprocal duplications may assist in understanding the molecular pathways involved.37 To our knowledge, however, obesity has not been reported for animal models of the 22q11.2 deletion,38 perhaps because of the emphasis on embryonic and early development. A recent biochemical study of 11 non-obese children with 22q11.2DS implicated dysregulated energy homeostasis.39 Studies of such state biomarker profiles, and of genome-wide genetic variants, in obese and non-obese adults with 22q11.2DS may shed light on factors that are important in both metabolic and neuronal functions.
Supplementary Material
Bar graph illustrating the relationship between intellectual level and BMI class for the 206 adults with 22q11.2DS with data available. 1=normal intellectual functioning, 2=borderline intellectual functioning, 3,4,5=mild, moderate, and severe intellectual disability, respectively. Colors indicate the four BMI classes:14 not obese (green), class I (yellow), class II (orange) and class III obesity (red).
Acknowledgments
The authors thank the adults with 22q11.2DS and their families, as well as the many referring clinicians, for their generous contributions to this and related research studies. This work was supported by Canadian Institutes of Health Research (CIHR) grants (MOP-97800 and MOP-89066), the University of Toronto McLaughlin Centre, and National Institute of Mental Health U01 MH101723-01. ASB holds the Canada Research Chair in Schizophrenia Genetics and Genomic Disorders, and the Dalglish Chair in 22q11.2 Deletion Syndrome.
Footnotes
Supplementary information is available at the Genetics in Medicine website.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Sinnema M, Maaskant MA, van Schrojenstein Lantman-de Valk HM, et al. Physical health problems in adults with Prader-Willi syndrome. Am J Med Genet A. 2011;155A:2112–2124. doi: 10.1002/ajmg.a.34171. [DOI] [PubMed] [Google Scholar]
- 2.Butler MG, Lee J, Manzardo AM, et al. Growth charts for non-growth hormone treated Prader-Willi syndrome. Pediatrics. 2015;135:e126–135. doi: 10.1542/peds.2014-1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zufferey F, Sherr EH, Beckmann ND, et al. A 600 kb deletion syndrome at 16p11. 2 leads to energy imbalance and neuropsychiatric disorders. J Med Genet. 2012;49:660–668. doi: 10.1136/jmedgenet-2012-101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Digilio MC, Marino B, Cappa M, Cambiaso P, Giannotti A, Dallapiccola B. Auxological evaluation in patients with DiGeorge/velocardiofacial syndrome (deletion 22q11.2 syndrome) Genet Med. 2001:30–33. doi: 10.1097/00125817-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Tarquinio DC, Jones MC, Jones KL, Bird LM. Growth charts for 22q11 deletion syndrome. Am J Med Genet A. 2012;158A:2672–2681. doi: 10.1002/ajmg.a.35485. [DOI] [PubMed] [Google Scholar]
- 6.Habel A, McGinn M-J, 2nd, Zackai EH, Unanue N, McDonald-McGinn DM. Syndrome-specific growth charts for 22q11. 2 deletion syndrome in Caucasian children. Am J Med Genet A. 2012;158A:2665–2671. doi: 10.1002/ajmg.a.35426. [DOI] [PubMed] [Google Scholar]
- 7.Guzman ML, Delgado I, Lay-Son G, Willans E, Puga A, Repetto GM. Growth in Chilean infants with chromosome 22q11 microdeletion syndrome. Am J Med Genet A. 2012;158A:2682–2686. doi: 10.1002/ajmg.a.35525. [DOI] [PubMed] [Google Scholar]
- 8.Bassett AS, Chow EW, Husted J, et al. Clinical features of 78 adults with 22q11 Deletion Syndrome. Am J Med Genet A. 2005;138:307–313. doi: 10.1002/ajmg.a.30984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oskarsdottir S, Persson C, Eriksson BO, Fasth A. Presenting phenotype in 100 children with the 22q11 deletion syndrome. Eur J Pediatr. 2005;164:146–153. doi: 10.1007/s00431-004-1577-8. [DOI] [PubMed] [Google Scholar]
- 10.Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiat. 2015;14:119–136. doi: 10.1002/wps.20204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PloS one. 2014;9:e94112. doi: 10.1371/journal.pone.0094112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bassett AS, Marshall CR, Lionel AC, Chow EW, Scherer SW. Copy number variations and risk for schizophrenia in 22q11.2 deletion syndrome. Hum Mol Genet. 2008;17:4045–4053. doi: 10.1093/hmg/ddn307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van L, Butcher NJ, Costain G, Ogura L, Chow EW, Bassett AS. Fetal growth and gestational factors as predictors of schizophrenia in 22q11.2 deletion syndrome. Genet Med. 2015 doi: 10.1038/gim.2015.84. Epub: Jun 18 2015. [DOI] [PubMed] [Google Scholar]
- 14.Health Canada. [Accessed May 17 2016];Canadian Guidelines for Body Weight Classification in Adults. 2004 doi: 10.1503/cmaj.1032012. Available at: http://www.hc-sc.gc.ca/fn-an/nutrition/weights-poids/guide-ld-adult/index-eng.php. [DOI] [PMC free article] [PubMed]
- 15.Richardson WS, Wilson MC, Williams JW, Jr, Moyer VA, Naylor CD. Users’ guides to the medical literature: XXIV. How to use an article on the clinical manifestations of disease. Evidence-Based Medicine Working Group. JAMA. 2000;284:869–875. doi: 10.1001/jama.284.7.869. [DOI] [PubMed] [Google Scholar]
- 16.Statistics Canada. [Accessed May 17 2016];Measured adult body mass index (BMI), by age group and sex, household population aged 18 and over excluding pregnant females, Canada (excluding territories) 2009 Available at: http://www5.statcan.gc.ca/cansim/a26?id=1050507&retrLang=eng&lang=eng.
- 17.Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;52:e143–263. doi: 10.1016/j.jacc.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Hsieh K, Rimmer JH, Heller T. Obesity and associated factors in adults with intellectual disability. J Intellect Disability Res. 2014;58:851–863. doi: 10.1111/jir.12100. [DOI] [PubMed] [Google Scholar]
- 19.Baron DN. Hypothyroidism; its aetiology and relation to hypometabolism, hypercholesterolaemia, and increase in body-weight. Lancet. 1956;271:277–281. doi: 10.1016/s0140-6736(56)92080-3. [DOI] [PubMed] [Google Scholar]
- 20.Gracious BL, Meyer AE. Psychotropic-induced weight gain and potential pharmacologic treatment strategies. Psychiatry (Edgmont) 2005;2:36–42. [PMC free article] [PubMed] [Google Scholar]
- 21.Blumenthal SR, Castro VM, Clements CC, et al. An electronic health records study of long-term weight gain following antidepressant use. JAMA psychiatry. 2014;71:889–896. doi: 10.1001/jamapsychiatry.2014.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gebhardt S, Haberhausen M, Heinzel-Gutenbrunner M, et al. Antipsychotic-induced body weight gain: predictors and a systematic categorization of the long-term weight course. J Psychiatr Res. 2009;43:620–626. doi: 10.1016/j.jpsychires.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Villareal DT, Apovian CM, Kushner RF, Klein S American Society for N, Naaso TOS. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am J Clin Nutr. 2005;82:923–934. doi: 10.1093/ajcn/82.5.923. [DOI] [PubMed] [Google Scholar]
- 24.Butler MG. Prader-Willi Syndrome: Obesity due to Genomic Imprinting. Curr Genomics. 2011;12:204–215. doi: 10.2174/138920211795677877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wheeler E, Huang N, Bochukova EG, et al. Genome-wide SNP and CNV analysis identifies common and low-frequency variants associated with severe early-onset obesity. Nat Genet. 2013;45:513–517. doi: 10.1038/ng.2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. [Accessed May 17, 2016];Mean and median age at diagnosis of diabetes among adult incident cases aged 18–79 years, United States, 1997–2011. 2015 Available at: http://www.cdc.gov/diabetes/statistics/age/fig2.htm.
- 27.Wirshing DA. Schizophrenia and obesity: impact of antipsychotic medications. J Clin Psychiatry. 2004;65(Suppl 18):13–26. [PubMed] [Google Scholar]
- 28.Carpiniello B, Corda E, Maccioni R, Pinna F. Schizophrenia, obesity and pharmacotherapy-associated weight gain. Clin Ter. 2008;159:299–306. [PubMed] [Google Scholar]
- 29.Butcher N, Fung W, Fitzpatrick L, et al. Response to clozapine in a clinically identifiable subtype of schizophrenia. Br J Psychiat. 2015;206:484–491. doi: 10.1192/bjp.bp.114.151837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders--a systematic review and meta-analysis. Schizophr Bull. 2013;39:306–318. doi: 10.1093/schbul/sbr148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Statistics Canada Health at a Glance. [Accessed May 17, 2016];Adjusting the scales: Obesity in the Canadian population after correcting for respondent bias. 2014 Available at: http://www.statcan.gc.ca/pub/82-624-x/2014001/article/11922-eng.htm.
- 32.Boot E, Butcher NJ, van Amelsvoort TA, et al. Movement disorders and other motor abnormalities in adults with 22q11. 2 deletion syndrome. Am J Med Genet A. 2015;167A:639–645. doi: 10.1002/ajmg.a.36928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fung WL, Butcher NJ, Costain G, et al. Practical guidelines for managing adults with 22q11.2 deletion syndrome. Genet Med. 2015;17:599–609. doi: 10.1038/gim.2014.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Core Indicators. [Accessed May 17, 2016];2016 Available at: http://www.nationalcoreindicators.org/
- 35.Maillard AM, Hippolyte L, Rodriguez-Herreros B, et al. 16p11.2 Locus modulates response to satiety before the onset of obesity. Int J Obes (Lond) 2015 doi: 10.1038/ijo.2015.247. [DOI] [PubMed] [Google Scholar]
- 36.Bassett AS, Chow EW, Husted J, et al. Premature death in adults with 22q11.2 deletion syndrome. J Med Genet. 2009;46:324–330. doi: 10.1136/jmg.2008.063800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arbogast T, Ouagazzal AM, Chevalier C, et al. Reciprocal Effects on Neurocognitive and Metabolic Phenotypes in Mouse Models of 16p11.2 Deletion and Duplication Syndromes. PLoS Genet. 2016;12:e1005709. doi: 10.1371/journal.pgen.1005709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guna A, Butcher NJ, Bassett AS. Comparative mapping of the 22q11.2 deletion region and the potential of simple model organisms. J Neurodev Disord. 2015;7:18. doi: 10.1186/s11689-015-9113-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Napoli E, Tassone F, Wong S, et al. Mitochondrial Citrate Transporter-dependent Metabolic Signature in the 22q11.2 Deletion Syndrome. J Biol Chem. 2015;290:23240–23253. doi: 10.1074/jbc.M115.672360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Bar graph illustrating the relationship between intellectual level and BMI class for the 206 adults with 22q11.2DS with data available. 1=normal intellectual functioning, 2=borderline intellectual functioning, 3,4,5=mild, moderate, and severe intellectual disability, respectively. Colors indicate the four BMI classes:14 not obese (green), class I (yellow), class II (orange) and class III obesity (red).