Abstract
Background
Depression is common in low-income pregnant women, and treatments need to be fitted to meet their needs. We conducted a randomized controlled trial comparing brief interpersonal psychotherapy (brief-IPT) to enhanced treatment as usual (ETAU) for perinatal depression in low-income women. The brief-IPT model is designed to better engage low-income women by utilizing an engagement session, providing flexible delivery of sessions, and pragmatic case management.
Methods
Pregnant women, aged ≥ 18, between 12–30 weeks gestation were recruited from an urban prenatal clinic. Women scoring ≥ 10 on the Edinburgh Depression Scale and meeting depressive disorder criteria were randomized to either brief-IPT (n=21) or ETAU (n=21). We assessed treatment outcomes, acceptability, and feasibility of the intervention (measured by session attendance).
Results
Depression scores significantly decreased in both brief-IPT and ETAU. Brief-IPT participants reported significant improvements in social support satisfaction as compared to ETAU participants, even after controlling for concurrent depressive symptoms. Brief-IPT participants reported high satisfaction with the program. However, many participants did not participate in the full 9-session course of treatment (average sessions attended = 6, range 0–17).
Limitations
Small sample size, use of self-report measures, and lack of an active psychotherapy control group limits interpretation of study results.
Conclusions
Brief-IPT for perinatal depression is acceptable to low-income women and is helpful for improving depressive symptoms and social support. However, feasibility of the treatment was limited by relatively low session attendance in spite of efforts to maximize treatment engagement. Additional modifications to meet the needs of low-income women are discussed.
Keywords: psychotherapy, poverty, patient engagement, depressive symptoms, perinatal
Introduction
Perinatal depression (depression occurring during pregnancy or postpartum time period) is a major public health problem. Depression during pregnancy has particularly deleterious effects on both the mother’s pregnancy and her infant’s social and emotional development (Moore, Cohn, & Campbell, 2001; Murray & Cooper, 1997). A significant proportion of women who are depressed antenatally remain depressed postpartum (O’Hara and Swain, 1996); thus, early intervention is imperative for the health and well-being of mothers and their babies.
Low income and minority women report high levels of depressive symptoms during pregnancy and postpartum; ranging from 25% meeting psychiatric diagnostic criteria to 47% reporting clinically elevated symptoms on self-report screening measures (for review see Bennett et al., 2004). Yet many pregnant women experiencing significant depressive symptoms go unrecognized and undiagnosed (Cox et al., 2016; Ko et al., 2012). Even when symptoms are recognized, community rates of treatment for perinatal depression are very low: it is estimated that fewer than 20% who receive a referral for depression treatment follow through with an appointment (Flynn et al., 2006; Ko et al., 2012; Munk-Olsen et al., 2016; Vesga-López O et al., 2008).
Recent studies have attempted to identify potential reasons for low-uptake of mental health treatment among women with low-incomes. Sleath and colleagues (2005), found an overwhelming preference among African American pregnant women as compared to Whites to “wait to get over it naturally”. Similarly, another study interviewing African American women in OBGyn clinics identified a perceived threat of a therapeutic relationship including worry that the therapist will not understand or will judge, as well as worry about abandonment from the therapist (Poleshuck et al., 2013). Women also reported doubt that therapy could help them, difficulty with trusting others, decreased motivation to engage in activity, a strong urge to be left alone, and an overall ambivalence towards depression treatment (Poleshuck et al., 2013). In addition to practical barriers such as child care, transportation, and inflexible scheduling; a review by Levy and O’Hara (2010) highlighted additional challenges common to both poverty and perinatal depression. For example, domestic violence, childhood abuse history, and single parenthood may all contribute to low uptake of depression treatment(Levy and O’Hara, 2010). Effective interventions that are acceptable and accessible for low-income pregnant women are needed. Potential modifications that may improve treatment uptake include: constant outreach, pre-treatment education and engagement, simultaneously addressing barriers in multiple domains (practical, psychological, and cultural), and closer collaboration with trusted health providers(Levy and O’Hara, 2010; Miranda J et al., 2003; Poleshuck et al., 2013).
Although depression during pregnancy is common, few randomized trials have investigated the efficacy of psychotherapeutic treatment of depression during pregnancy (Dennis et al., 2007). Early studies reported significant difficulties enrolling and retaining pregnant or postpartum women in Cognitive Behavioral Therapy (CBT) (Carter et al., 2005; McKee et al., 2006). As a result, recent studies have modified CBT to improve feasibility and acceptability among pregnant women (McGregor et al., 2014; Milgrom et al., 2015; O’Mahen et al., 2013). For example, O’Mahen and colleagues (2013) utilized an engagement interview followed by modular sessions delivered in a flexible format (home or clinic) with an “active outreach strategy” to retain participants. Milgrom and colleagues (2015) modified their CBT based intervention for pregnancy by changing from 12 group sessions to 8 individual sessions. Both studies showed promise in increasing engagement and retention into psychotherapy and in effectively reducing depressive symptoms.
Interpersonal Psychotherapy (IPT), another evidence-based intervention for depression, focuses on issues commonly associated with perinatal depression like lack of social support and stressful life events. Spinelli and colleagues examined the efficacy of 12-session IPT with pregnant women with diverse racial and socioeconomic backgrounds and found significant improvement in depressive symptoms especially in women with moderate to severe depression (Spinelli et al., 2016; Spinelli and Endicott, 2003). However, 30% of women randomized to IPT dropped out of the study despite reimbursement for child care and transportation costs. Reasons for attrition included childcare and employment demands, unstable housing and support systems, pregnancy complications such a physical ailments and bed rest, and disconnected phone numbers (Spineli and Edicott, 2003). Noting the substantial barriers to care faced by low-income populations as described by Spinelli and Endicott 2003 and others, Grote and colleagues subsequently modified a brief version of IPT designed to improve feasibility in low-income women by including an engagement interview (addressing psychological and cultural barriers to care), 8 prenatal IPT sessions, and case management (i.e., bus passes, child care, baby supplies) (Grote et al., 2004). Brief-IPT participants were more likely to show improvements in depressive symptoms and social functioning than women in usual care (Grote et al., 2009). Fewer than 10% dropped out of the study and 68% attended greater than 7 IPT sessions (considered a full dose). These findings suggest that IPT is an effective intervention for depression during pregnancy and with modification, feasible in low-income populations.
Though some progress has been made, engaging and retaining low-income and minority women in psychotherapy remains a significant challenge. Designed as a pilot study to test feasibility of conducting larger clinical trial, we aimed to replicate Grote and colleagues 2009) brief-IPT model using similar modifications to engage low-income women into treatment. The current report presents acceptability, feasibility, and clinical outcomes data from a randomized controlled trial comparing brief-IPT to Enhanced Treatment as Usual (ETAU) during pregnancy. This study, to our knowledge, is the first independent replication of the brief-IPT model (as reported by Grote et al., 2004; 2009) with a low-income perinatal population.
Methods
Procedures
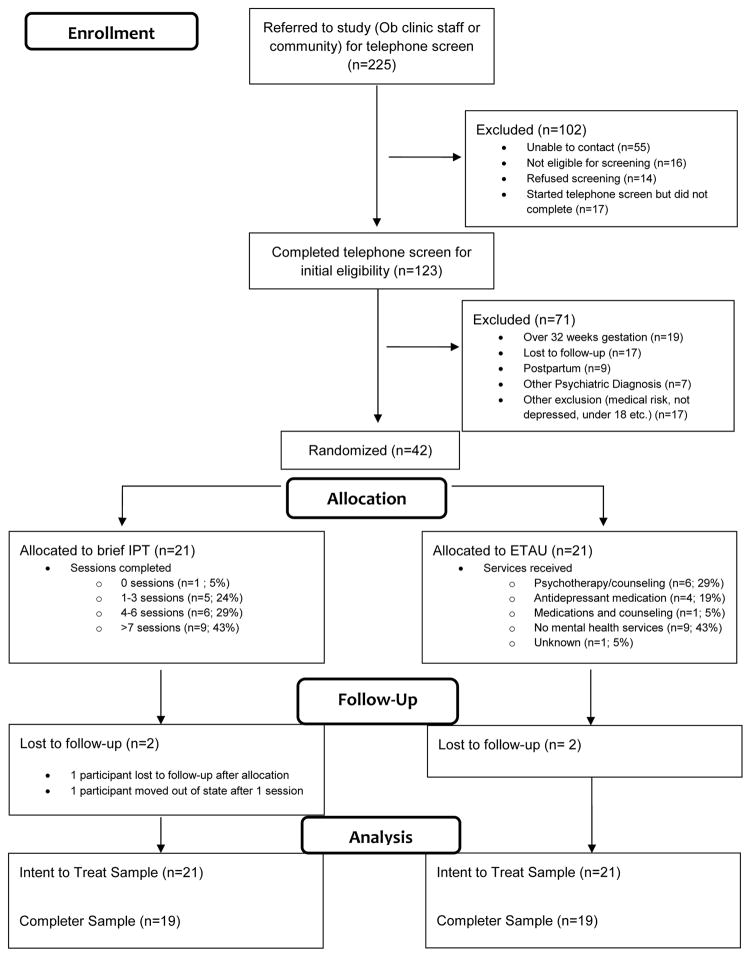
Study procedures were in compliance with the Declaration of Helsinki and were approved by the Washington University Institutional Review Board. Participants provided written informed consent prior to participation. Pregnant women, ages 18 and older, between 12–30 weeks gestation with singleton pregnancies were recruited from an urban prenatal clinic by flyers posted in the OB-Gyn clinic, OB-Gyn clinic staff referral, and referrals from community social service agencies. Research staff administered the Edinburgh Depression Scale (EDS; Cox et al., 1987) in person or by phone to determine initial eligibility. The Structured Clinical Interview for DSM-IV (SCID; First et al., 1995) was used to establish diagnostic criteria. Women with EDS scores ≥ 10 and current Major Depression, Dysthymia, or Depression NOS were eligible. Participants with psychotic disorders, current substance abuse, or medically high-risk pregnancies were excluded. Eligible participants were randomized by a statistician using a computer generated block permuted design to either brief-IPT (n=21) or ETAU (n=21). The PI and study staff were blinded to the randomization grid and assignments were stored in opaque, sealed envelopes and opened by the participant once a determination of inclusion and exclusion criteria were met. Figure 1 illustrates screening, enrollment, and retention in the study.
Figure 1.
CONSORT Flow Diagram
Interventions
As previously reported in Lenze, Rodgers, and Luby (2015), participants randomized to brief IPT participated in an ethnographic engagement session followed by 8 individual IPT sessions as described by Grote and colleagues (Grote et al., 2004). Maintenance treatment sessions were conducted with participant who completed all 9 sessions prior to delivery of her baby. Sessions took place in the research clinic, participant homes, or other community locations as desired by the participant. Bus tickets were provided for those who wanted to meet in the clinic and therapy times were flexible to accommodate participant needs. Activities were available for older children who accompanied their mothers to appointments. Reminder calls, follow up to missed appointments, and check in calls when the participant was experiencing increased stress were an important part of the therapeutic relationship and allowed the therapist to remain in contact between therapy sessions. Participants were given diapers for their baby at each therapy session. Therapists included the PI (a clinical psychologist with 15 years of experience conducting and supervising IPT) and two master’s level clinicians. The clinicians participated in structured didactics and readings directed by the PI and received individual supervision using video recordings on a complete brief-IPT case prior to the study. All brief-IPT sessions were video recorded for use in supervision. Throughout the study, both individual and weekly small group supervision (consisting of the PI, the clinician, and a child psychiatrist consulting on the study) meetings were held to discuss cases and ensure fidelity to the model. The PI utilized the Interpersonal Psychotherapy Adherence and Quality Scale (Stuart, 2011) to assess fidelity to the IPT model and to guide individual and group supervision discussions..
Participants assigned to ETAU were referred to community resources (including specialty mental health). Additionally, brief case management, diapers and other baby supplies were provided. Telephone assessments were conducted every 2 weeks to assess depressive and anxiety symptoms and encourage or facilitate depression treatment. Based on participant responses to the scales, the caller would ask follow up questions and encourage the participant to either continue treatment or make contact with referrals for mental health services. As participant needs changed over time, additional referrals were also offered. Figure 1 shows the various types of treatment women in ETAU received.
Measures
Treatment feasibility, acceptability, and clinical outcomes were measured at baseline and between 37–39 weeks gestation in both the brief-IPT and ETAU groups. In addition to a demographics questionnaire, we utilized the Difficult Life Circumstances (DLC; Barnard, 2010), a 28-item self-report checklist, to characterize participants’ experiences of life stressors. Scores of six and higher indicate high risk for adverse parenting. At baseline, participants reported events occurring in the previous 12 months and at the 37–39 weeks gestation assessment, participants reported events occurring since the baseline visit. The income-to-needs ratio was calculated using the U.S. Census Bureau 2014 Poverty Thresholds (reported family income divided by poverty threshold). Adult attachment is associated with emotional regulation and interpersonal relationships (Fraley et al., 2000), persistence of postpartum depressive symptoms (McMahon et al., 2005), and may be predictive of postnatal mother-infant attachment (Fonagy et al., 1991). Thus, we used the Experiences in Close Relationships-Revised (ECR-R; Fraley et al., 2000), a 36-item self-report measure of attachment related avoidance and anxiety, to characterize adult-attachment behaviors in close relationships at baseline as a potential predictor of therapy response. Ratings are made on a 7-point Likert scale with higher scores indicating greater endorsement of anxiety and avoidance behaviors.
Acceptability of the intervention at 37–39 weeks gestation was measured with the Client Satisfaction Questionnaire (CSQ; Clifford and Greenfield, 1999), a brief 8-item questionnaire. Items are rated 1 through 4, with higher scores indicating greater satisfaction. We also examined session attendance and drop-out rates as indicators of program acceptability. Feasibility indicators included engagement and adherence to study protocols. We utilized participant tracking logs to monitor rescheduled appointments, no-shows, and telephone calls/texts.
The Edinburgh Depression Scale (EDS;(Cox et al., 2014), the primary clinical outcome, is a commonly used measure of depressive symptoms during the perinatal period. The EDS has shown acceptable reliability and validity and is sensitive to symptom severity and change over time (Bergink et al., 2011; Cox et al., 2014; Murray and Cox, 1990). We measured anxiety symptoms using the Brief State Trait Anxiety Inventory (Brief-STAI; Berg et al., 1998), a 6-item questionnaire assessing acute feelings of distress or anxiety. We measured social support using the Social Support Questionnaire Revised (SSQR; Sarason et al., 1987). The SSQR is a 12-item self-report scale that assesses the perception of people available for support in various life situations and satisfaction with perceived support availability. For this study, we focused on the satisfaction subscale, with higher scores indicating greater satisfaction with support available (scores range from 0 to 36).
Data Analysis
Demographic and categorical variables were compared using Chi-square and Fisher’s Exact test. As this study was designed to be a pilot feasibility study and does not have sufficient power to detect statistical significance between groups, we instead report descriptive statistics, and effect sizes and confidence intervals for our three clinical outcome measures (EDS, brief STAI, and SSQR)(Lee et al., 2014; Thabane et al., 2010).
An intent-to-treat approach was taken for analyses of clinical outcome measures. Effect sizes (Cohen’s d based on pooled standard deviations) and confidence intervals were calculated first using observed data (or completers). Inspection of the data revealed all data was missing at random, thus missing data were imputed using maximum likelihood methods with 20 iterations. Effect sizes and confidence intervals were then calculated using imputed data. To examine clinically meaningful changes in individual participant EDS scores, we calculated a reliable change index (Jacobson and Truax, 1991) to determine the statistical reliability of the magnitude of change for an individual patient that accounts for measurement fluctuation. Previous work has suggested a four point change is needed to be 95% confident of clinical significant change in depressive symptoms using the EDS (Matthey, 2004). Once the reliable change index value was determined a validated cut-off score (12; Cox et al., 2014) was used to categorize whether the change indicated improvement or deterioration. All data analyses were computed using SAS version 9.4.
Results
Participant Characteristics
Table 1 shows participant characteristics. Participants were primarily single, poor, African American females with a high school education. Half reported current symptoms of PTSD (determined using DSM-IV SCID criteria). A majority of women (35 out of 42 or 83%) reported incomes below poverty level. Several women in our sample experienced homelessness or near homelessness (the absence of a permanent address as they stayed with different friends/relatives) over the course of the study and many reported food insecurity (insufficient food to feed herself and her family) and/or utility cut-offs. Constant worry about her ability to provide basic needs for herself and her family became a daily concern for many women. On average, participants reported experiencing 5 (range 0 to 15) life events between baseline and 37–39 weeks gestation; scoring just below the clinically elevated risk score of 6 (Barnard, 2010). Seventy percent of women reported ECR-R scores indicative of relatively insecure adult attachment (Fraley, 2012); a factor associated with negative treatment engagement (Ciechanowski et al., 2006). There were no significant differences between groups on any demographic variables.
Table 1.
Demographic and participant characteristics at baseline (n=42).
| Brief-IPT n=21 | Enhanced TAU n=21 | ||
|---|---|---|---|
| Age, mean (SD) | 26.90 (5.81) | 26.38 (5.90) | |
| Range | 18 – 36 | 18 – 40 | |
| Weeks pregnant at enrollment, mean (SD) | 23.38 (6.58) | 25.76 (4.57) | |
| Number of pregnancies, mean (SD) | 1.52 (1.47) | 1.81 (1.88) | |
| Race, % (n) | Black | 81 (17) | 76 (16) |
| White | 19 (4) | 14 (3) | |
| Other | 0 | 10 (2) | |
| Marital Status, % (n) | Never Married | 76 (16) | 52 (11) |
| Married/Living in marriage-like relationship | 19 (5) | 33 (7) | |
| Separated/Divorced | 5 (1) | 14 (3) | |
| Education, % (n) | Some high school | 29 (6) | 24 (5) |
| High school diploma/GED | 19 (4) | 29 (6) | |
| Some college or 2 year degree | 38 (8) | 38 (8) | |
| 4-year college/graduate degree | 14 (3) | 10 (2) | |
| Annual Income, % (n)a | (n=20) | (n=20) | |
| Less than $10,000 | 62 (13) | 52 (11) | |
| Between $10,001 and $20,000 | 24 (5) | 14 (3) | |
| Between $20,001 and $30,000 | 0 (0) | 10 (2) | |
| Between $30,001 and $60,000 | 10 (2) | 14 (3) | |
| Greater than $60,001 | 0 (0) | 5 (1) | |
| Income-to-Needs Ratiob, mean (SD) | .79 (.64) | 1.15 (.96) | |
| Range | .32 – 2.83 | .36 – 3.20 | |
| Household Support, % | Employed | 38 (8) | 43 (9) |
| (n) | Food Stamps | 76 (16) | 76 (16) |
| Medicaidc | 57 (12) | 86 (18) | |
| WIC | 67 (14) | 62 (13) | |
| Other (child support, unemployment, etc.) | 48 (10) | 10 (2) | |
| Comorbid Conditions, % | Post -Traumatic Stress Disorder | 52 (11) | 43 (9) |
| (n) | Social Phobia | 14 (3) | 19 (4) |
| Generalized Anxiety Disorder | 19 (4) | 14 (3) | |
| Panic Disorder | 19 (4) | 10 (2) | |
| Alcohol Abuse (Lifetime) | 19 (4) | 29 (6) | |
| Cannabis Abuse (Lifetime) | 29 (6) | 24 (5) | |
| Other Drug Dependence (Lifetime) | 5 (1) | 10 (2) | |
Brief IPT, Brief Interpersonal Psychotherapy; Enhanced TAU, enhanced treatment as usual
n=2 participants refused to answer household income question
Income-to-needs ratio calculated as defined by U.S. Census Bureau 2014 Poverty Thresholds, Ratios below 1.00 are below the official poverty definition, ratios between 1.00 and 1.25 are described as “near poverty”, ratios below .50 are described as “severe poverty”
E-TAU more likely to report enrollment in Medicaid, X2= 4.20, p=.04
Feasibility and Acceptability
Study retention: Two participants in each group dropped out of the study after randomization (9%). There were no differences on any baseline variables between participants who dropped-out of the study versus those that completed the 37–39 weeks assessment. Two participants in the ETAU group were lost to follow-up; one immediately after randomization and after 8 weeks for the other. One participant in the brief-IPT group was lost to follow-up after randomization prior to any session attendance, while the other dropped out of the study after one session because of an out-of-state move. Treatment adherence: As shown in Figure 1, 71% of participants assigned to brief-IPT competed at least 4 sessions (the minimum “dose” as suggested in American Psychiatric Association Practice guidelines (Work Group on Major Depressive Disorder, 2010), and 43% completed at least 7 sessions (considered full dose). The number of sessions completed was correlated with income–to-needs ratio (r=.48, p=.03, n=20/21); those with higher incomes attended more sessions. Participants rescheduled sessions on average twice over the course of therapy (range 0 – 9), no-showed to sessions on average 1.76 times (range 0 – 6), and received an average of 5.19 (range 1–12) phone calls between sessions. Per participant tracking logs, session non-attendance was usually due to medical complications, earlier than anticipated delivery, difficulty keeping appointments due to changing work schedules, and non-working cell phone numbers. Intervention satisfaction: Participants assigned to brief-IPT reported high scores on the CSQ at the 37–39 weeks assessment (IPT x=30.60, SD= 1.89, range 25–32) indicating acceptability of brief-IPT intervention. For many participants this was their first experience with psychotherapy and the opportunity to openly express their feelings and gain insight was a vital component of the program. For example, one mom wrote, “I like [the] program. Helped me a lot to kind of talk about things I usually don’t express. The program opened my mind to talk [to] other people about my problems”.
Clinical Outcomes
Table 2 shows differences for clinical outcomes measured at baseline and 37–39 weeks gestation. As shown in the tables, depression symptoms significantly decreased in both IPT and ETAU. Using the reliable change index plus cut-off criteria (EDS<12) (Jacobson and Truax, 1991; Matthey, 2004) we found: 58% (11/19) of participants assigned to brief-IPT reported reliable and clinically significant improvement from baseline to 39 weeks gestation; 37% (7/19) report no clinically significant changes in scores; and 5% (1/19) reported significant worsening of symptoms. In the ETAU group, 63% (12/19) reported reliable and clinically significant improvements in depressive symptoms. Notably, 67% (8/12) of the women reporting improvements were receiving depression treatment (either medication or therapy). Thirty-two percent (6/19) reported no change on the EDS and 5% reported clinically significant worsening of symptoms. Both the brief-IPT participants and ETAU participants reported very little change in anxiety symptoms as measured by the brief-STAI. Participants randomized to brief-IPT reported improvements in social support satisfaction at 37–39 weeks gestation compared to baseline with medium to large effect sizes. Changes in social support satisfaction between baseline and 37–39 weeks gestation were less marked in the ETAU group.
Table 2.
Changes in scores on clinical variables from baseline to 37–39 weeks gestation.
| Brief IPT | ETAU | Between Group | |||||
|---|---|---|---|---|---|---|---|
| Baseline | 37–39 week | Baseline | 37–39 week | 37–39 week | |||
| Measure | M (SD) | M(SD) | Cohen’s d (95% CIs) | M (SD/SE) | M (SD/SE) | Cohen’s d (95%CIs) | Mean Difference Cohen’s d (95%CIs) |
| EDS | |||||||
| Observed | 17.81 (3.71) | 12.12 (5.33) | 1.25 (.55–1.90) | 17.90 (4.60) | 11.21 (6.80) | 1.16 (.47–1.81) | .15 (−.49–.78) |
| Imputed | n/a | 12.04 (1.22) | 2.09 (1.30–2.80) | n/a | 11.41 (1.72) | 1.87 (1.11–2.55) | .42 (−.20–1.03) |
| Brief-STAI | |||||||
| Observed | 15.57 (4.11) | 13.67 (4.50) | .44 (−.19–1.06) | 15.05 (4.31) | 14.16 (4.83) | .20 (−.43–.81) | −.10 (−.74–.53) |
| Imputed | 15.56 (0.64) | 14.02 (1.09) | 1.72 (.99–2.40) | 15.25 (0.97) | 14.37 (1.23) | .79 (.15–1.41) | −.30 (−.90–.31) |
| SSQR | |||||||
| Observed | 28.40 (6.49) | 32.22 (3.21) | −.73 (−1.36–−.08) | 28.20 (6.36) | 29.18 (6.07) | −.16 (−.78–.47) | .63 (−.04–1.26) |
| Imputed | 28.32 (1.42) | 31.66 (0.95) | −2.76 (−3.55–−1.87) | 28.36 (1.41) | 28.61 (1.79) | −.16 (−.76–.45) | 2.13 (1.34–2.84) |
Note. CI=confidence interval. EDS= Edinburgh Depression Scale; Brief-STAI= Brief State Trait Anxiety Inventory; SSQR= Social Support Questionnaire Revised.
Discussion
This study, to our knowledge, is the first independent replication of the brief-IPT model in a low-income perinatal population. Women reported high levels of satisfaction with the intervention and depressive symptoms and social support satisfaction were significantly improved. Although drop-out of the overall study was relatively low (10%), adherence to the brief-IPT protocol was more variable. Modifications to remove common barriers to psychotherapy engagement resulted in 71% of women engaging in a minimally adequate number of sessions; however, only 43% of women attended seven or more sessions. This is in contrast to Grote and colleagues (2009) original findings in which 68% of women randomized to brief-IPT engaged in a full course of therapy. A key difference between our study and the Grote study was our inability to consistently deliver brief-IPT by telephone (though it was an option available to participants). We experienced significant difficulty reaching participants by phone due to changing phone numbers, phones with no minutes or unpaid bills, participants ending a call, or not answering. We were also not able to provide brief-IPT sessions in the OB clinic in conjunction with prenatal care. It is likely, that this type of “co-location” within the healthcare system would have improved adherence. Indeed, a recent review recommended collaborative care models as effective at engaging underserved populations into mental health care (Interian et al., 2013). Further, our rate of depression symptom improvement as reported on the EDS was less robust in the brief-IPT group and more robust in the ETAU group than was reported by Grote and colleagues(2009). Potential reasons for these differences may be due to the higher rates of comorbid PTSD in our sample compared to Grote’s sample (50% vs. 26%, respectively). Lower adherence to the brief-IPT intervention and higher engagement in depression treatment by our ETAU group are also potential factors.
Our adherence and attrition rates are remarkably similar to other recent studies with pregnant women in low-income settings (O’Mahen et al., 2013). Other studies have also reported high treatment attrition (up to 50% in some studies) despite strategies such as paying for session attendance, extensive outreach, flexible scheduling, and home visits (Miranda J et al., 2003; O’Mahen et al., 2013; Sacks et al., 2014; Spinelli and Endicott, 2003). We were under-resourced to sufficiently provide for the substantial case management needs of this highly impoverished sample. Miranda and colleagues have previously demonstrated that this component is essential to better address depressive symptoms in this population (Miranda et al., 2003). Two recent studies have employed innovative models of care utilizing lay navigators or community supports to address this issue with promising results (Diaz-Linhart et al., 2016; Poleshuck et al., 2015). These types of strategies may be necessary to better address the complex needs of low-income women experiencing depression during pregnancy.
Women in both brief-IPT and ETAU demonstrated clinically significant improvements in depressive symptoms as reported on the EDS, despite high rates of comorbid trauma and psychosocial stressors as described above. While our sample is too small to investigate the effects of trauma on treatment adherence or response, this is an important are for future research. It should be noted that many women assigned to ETAU did receive depression treatment, much higher than anticipated given previous reports (though the full extent of treatment receipt is unknown), and contact with study staff was relatively high. This finding is similar to other recent studies demonstrating significant depressive symptom improvement using parenting education and peer support groups as active controls (Field et al., 2013; Spinelli and Endicott, 2003). Future work with much larger samples is clearly needed to help better identify women who will benefit from psychotherapy versus less intensive interventions. Our data also suggests that comparisons with “treatment as usual conditions” may no longer be adequate comparators. We conclude that brief-IPT is a promising intervention for perinatal depression, but further modifications to treatment delivery are necessary to meet the high needs of women living in poverty.
There are a few limitations to the current study. The primary outcome was measured by self-report rather than by blinded independent interview which may bias study results. Independent ratings regarding fidelity to the treatment model were unavailable. While the PI utilized ratings on an established fidelity measure to guide supervision and prevent therapist drift, the possibility of bias remains. Additionally, this sample consisted of primarily low-income African American pregnant women, which limits generalizability of the study findings. Finally, we did not have the resources to compare brief-IPT to an active psychotherapy which limits the interpretation of study findings. While many women in the ETAU condition did receive mental health treatment or services, we are unable to determine the quality of those services received.
Conclusion
The brief-IPT model is an acceptable psychotherapeutic intervention for depression in women during pregnancy. We found clinically significant reductions in depressive symptoms and improvements in social functioning. While brief-IPT is an important and effective intervention, more work is needed to better understand how to provide depression care to under-resourced perinatal populations. This is an important opportunity to improve long-term benefits for both mothers and their infants.
Table 3.
Treatment effects on depression, anxiety, and social functioning.
| Outcome | Baseline | 37–39 weeks | 95% CI (LL, UL) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | F | p | ||
| EDS | |||||||
| Brief IPT | 17.81 | 3.71 | 12.12 | 5.33 | .28 | .60 | 0, 6.1 |
| ETAU | 17.90 | 4.60 | 11.21 | 6.80 | |||
| Brief STAI | |||||||
| Brief IPT | 15.57 | 4.11 | 13.67 | 4.50 | .32 | .58 | 0, .15 |
| ETAU | 15.05 | 4.31 | 14.16 | 4.83 | |||
| SSQR | |||||||
| Brief IPT | 28.40 | 6.49 | 32.22 | 3.21 | 4.07 | .05 | 0, 16.2 |
| ETAU | 28.20 | 6.36 | 29.18 | 6.07 | |||
Note. Brief IPT= Brief Interpersonal Psychotherapy; ETAU= enhanced treatment as usual. CI=confidence interval; LL= lower limit; UL = upper limit. EDS= Edinburgh Depression Scale; Brief-STAI= Brief State Trait Anxiety Inventory; SSQR= Social Support Questionnaire Revised. Table reflects observed data. All models controlled for baseline values of outcome measures.
Highlights.
Brief-IPT is effective in reducing depressive symptoms during pregnancy.
Many women did not attend all therapy sessions despite intensive engagement effort.
Innovative models for perinatal depression care are needed for low-income women.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barnard KE. Difficult Life Circumstances (DLC) NCAST Programs; Seattle, Washington: 2010. [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of Depression During Pregnancy: Systematic Review: Obstet. Gynecol. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Berg CZ, Shapiro N, Chambless DL, Ahrens AH. Are emotions frightening? II: an analogue study of fear of emotion, interpersonal conflict, and panic onset1. Behav Res Ther. 1998;36:3–15. doi: 10.1016/S0005-7967(97)10027-4. [DOI] [PubMed] [Google Scholar]
- Bergink V, Kooistra L, Lambregtse-van den Berg MP, Wijnen H, Bunevicius R, van Baar A, Pop V. Validation of the Edinburgh Depression Scale during pregnancy. J Psychosom Res. 2011;70:385–389. doi: 10.1016/j.jpsychores.2010.07.008. [DOI] [PubMed] [Google Scholar]
- Carter FA, Carter JD, Luty SE, Wilson DA, Frampton CMA, Joyce PR. Screening and treatment for depression during pregnancy: a cautionary note. Aust N Z J Psychiatry. 2005;39:255–261. doi: 10.1080/j.1440-1614.2005.01562.x. [DOI] [PubMed] [Google Scholar]
- Cheng E, Kindig D. Disparities in Premature Mortality Between High- and Low-Income US Counties. Prev Chronic Dis. 2012 doi: 10.5888/pcd9.110120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciechanowski PS, Russo JE, Katon WJ, Von Korff M, Simon GE, Lin EHB, Ludman EJ, Young BA. The Association of Patient Relationship Style and Outcomes in Collaborative Care Treatment for Depression in Patients with Diabetes. Med Care. 2006;44:283–291. doi: 10.1097/01.mlr.0000199695.03840.0d. [DOI] [PubMed] [Google Scholar]
- Clifford C, Greenfield TK. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. 2. Lawrence Erlbaum Associates Publishers; Mahwah, NJ, US: 1999. The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8; pp. 1333–1346. [Google Scholar]
- Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The Perinatal Depression Treatment Cascade: Baby Steps Toward Improving Outcomes. J Clin Psychiatry. 2016:1189–1200. doi: 10.4088/JCP.15r10174. [DOI] [PubMed] [Google Scholar]
- Cox J, Holden J, Henshaw C. The Edinburgh Postnatal Depression Scale (EPDS) Manual. 2. RCPsych Publications; London: 2014. Perinatal Mental Health. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression. Scale Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis C-L, Ross LE, Grigoriadis S. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2007. Psychosocial and psychological interventions for treating antenatal depression. [DOI] [PubMed] [Google Scholar]
- Diaz-Linhart Y, Silverstein M, Grote N, Cadena L, Feinberg E, Ruth BJ, Cabral H. Patient Navigation for Mothers with Depression who Have Children in Head Start: A Pilot Study. Soc Work Public Health. 2016;0:1–7. doi: 10.1080/19371918.2016.1160341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego M, Delgado J, Medina L. Peer support and interpersonal psychotherapy groups experienced decreased prenatal depression, anxiety and cortisol. Early Hum Dev. 2013;89:621–624. doi: 10.1016/j.earlhumdev.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders. New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Flynn HA, Blow FC, Marcus SM. Rates and predictors of depression treatment among pregnant women in hospital-affiliated obstetrics practices. Gen Hosp Psychiatry. 2006;28:289–295. doi: 10.1016/j.genhosppsych.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Steele H, Steele M. Maternal Representations of Attachment during Pregnancy Predict the Organization of Infant-Mother Attachment at One Year of Age. Child Dev. 1991;62:891–905. doi: 10.1111/j.1467-8624.1991.tb01578.x. [DOI] [PubMed] [Google Scholar]
- Fraley RC. [accessed 7.8.16];Information on the Experiences in Close Relationships-Revised (ECR-R) Adult Attachment Questionnaire [WWW Document] 2012 http://internal.psychology.illinois.edu/~rcfraley/measures/ecrr.htm.
- Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78:350–365. doi: 10.1037/0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- Grote NK, Bledsoe SE, Swartz HA, Frank E. Feasibility of Providing Culturally Relevant, Brief Interpersonal Psychotherapy for Antenatal Depression in an Obstetrics Clinic: A Pilot Study. Res Soc Work Pract. 2004;14:397–407. doi: 10.1177/1049731504265835. [DOI] [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A Randomized Controlled Trial of Culturally Relevant, Brief Interpersonal Psychotherapy for Perinatal Depression. Psychiatr Serv. 2009;60:313–321. doi: 10.1176/ps.2009.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interian A, Lewis-Fernández R, Dixon LB. Improving Treatment Engagement of Underserved U.S. Racial-Ethnic Groups: A Review of Recent Interventions. Psychiatr Serv. 2013;64:212–222. doi: 10.1176/appi.ps.201100136. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol, Seeking New Clinical Research Methods. 1991;59:12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and Treatment Among U.S. Pregnant and Nonpregnant Women of Reproductive Age, 2005–2009. J Womens Health. 2012;21:830–836. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: should significance thresholds be reconsidered? BMC Med Res Methodol. 2014;14:41. doi: 10.1186/1471-2288-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze SN, Rodgers J, Luby J. A pilot, exploratory report on dyadic interpersonal psychotherapy for perinatal depression. Arch Womens Ment Health. 2015;18:485–491. doi: 10.1007/s00737-015-0503-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy LB, O’Hara MW. Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clin Psychol Rev. 2010;30:934–950. doi: 10.1016/j.cpr.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Matthey S. Calculating clinically significant change in postnatal depression studies using the Edinburgh Postnatal Depression Scale. J Affect Disord. 2004;78:269–272. doi: 10.1016/S0165-0327(02)00313-0. [DOI] [PubMed] [Google Scholar]
- McGregor M, Coghlan M, Dennis CL. The effect of physician-based cognitive behavioural therapy among pregnant women with depressive symptomatology: a pilot quasi-experimental trial. Early Interv Psychiatry. 2014;8:348–357. doi: 10.1111/eip.12074. [DOI] [PubMed] [Google Scholar]
- McKee MD, Zayas LH, JF, RCB, SHN Results of an Intervention to Reduce Perinatal Depression Among Low-Income Minority Women in Community Primary Care. J Soc Serv Res. 2006;32:63–81. doi: 10.1300/J079v32n04_04. [DOI] [Google Scholar]
- McMahon C, Barnett B, Kowalenko N, Tennant C. Psychological factors associated with persistent postnatal depression: past and current relationships, defence styles and the mediating role of insecure attachment style. J Affect Disord. 2005;84:15–24. doi: 10.1016/j.jad.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Holt C, Holt CJ, Ross J, Ericksen J, Gemmill AW. Feasibility study and pilot randomised trial of an antenatal depression treatment with infant follow-up. Arch Womens Ment Health. 2015;18:717–730. doi: 10.1007/s00737-015-0512-5. [DOI] [PubMed] [Google Scholar]
- Miranda J, Azocar F, Organista KC, Dwyer E, Areane P. Treatment of Depression Among Impoverished Primary Care Patients From Ethnic Minority Groups. Psychiatr Serv. 2003;54:219–225. doi: 10.1176/appi.ps.54.2.219. [DOI] [PubMed] [Google Scholar]
- Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Murray D, Cox JL. Screening for depression during pregnancy with the edinburgh depression scale (EDDS) J Reprod Infant Psychol. 1990;8:99–107. doi: 10.1080/02646839008403615. [DOI] [Google Scholar]
- O’Mahen H, Himle JA, Fedock G, Henshaw E, Flynn H. A Pilot Randomized Controlled Trial of Cognitive Behavioral Therapy for Perinatal Depression Adapted for Women with Low Incomes. Depress Anxiety. 2013;30:679–687. doi: 10.1002/da.22050. [DOI] [PubMed] [Google Scholar]
- Poleshuck E, Wittink M, Crean H, Gellasch T, Sandler M, Bell E, Juskiewicz I, Cerulli C. Using patient engagement in the design and rationale of a trial for women with depression in obstetrics and gynecology practices. Contemp Clin Trials. 2015;43:83–92. doi: 10.1016/j.cct.2015.04.010. [DOI] [PubMed] [Google Scholar]
- Poleshuck EL, Cerrito B, Leshoure N, Finocan-Kaag G, Kearney MH. Underserved Women in a Women’s Health Clinic Describe Their Experiences of Depressive Symptoms and Why They Have Low Uptake of Psychotherapy. Community Ment Health J. 2013;49:50–60. doi: 10.1007/s10597-012-9500-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks RM, Greene J, Burke R, Owen EC. Mental Health Care Among Low-Income Pregnant Women with Depressive Symptoms: Facilitators and Barriers to Care Access and the Effectiveness of Financial Incentives for Increasing Care. Adm Policy Ment Health Ment Health Serv Res. 2014;42:484–492. doi: 10.1007/s10488-014-0562-4. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A Brief Measure of Social Support: Practical and Theoretical Implications. J Soc Pers Relatsh. 1987;4:497–510. doi: 10.1177/0265407587044007. [DOI] [Google Scholar]
- Sleath B, West S, Tudor G, Perreira K, King V, Morrissey J. Ethnicity and depression treatment preferences of pregnant women. J Psychosom Obstet Gynecol. 2005;26:135–140. doi: 10.1080/01443610400023130A. [DOI] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J. Controlled Clinical Trial of Interpersonal Psychotherapy Versus Parenting Education Program for Depressed Pregnant Women. Am J Psychiatry. 2003;160:555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J, Goetz RR, Segre LS. Reanalysis of Efficacy of Interpersonal Psychotherapy for Antepartum Depression Versus Parenting Education Program: Initial Severity of Depression as a Predictor of Treatment Outcome. J Clin Psychiatry. 2016:535–540. doi: 10.4088/JCP.15m09787. [DOI] [PubMed] [Google Scholar]
- Stuart S. Interpersonal Psychotherapy Adherence and Quality Scale 2011 [Google Scholar]
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, Thabane M, Giangregorio L, Goldsmith CH. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Work Group on Major Depressive Disorder. American Psychiatric Association Practice Guildeline for the treatment of patients with Major Depressive Disorder. 3. American Psychiatric Association; Washington D.C: 2010. [Google Scholar]