Abstract
Background
Temperamental behavioral inhibition (BI) in children predicts later anxiety disorders. However, many children with BI do not develop anxiety disorders, suggesting the importance of identifying moderating factors. The current study examined whether parents’ history of BI moderates the associations between preschoolers’ BI and anxiety disorders at age 9.
Methods
The sample was 392 children and their parents from the community. Child BI was measured at age 3 using observational (Laboratory Temperament Assessment Battery; Lab-TAB) and parent report (Behavior Inhibition Questionnaire; BIQ) measures. In addition, both parents reported on their own history of childhood BI using the Retrospective Measure of Behavioral Inhibition (RMBI). When the children were 9 years old, a parent and the child were interviewed using the Kiddie Schedule for the Affective Disorders and Schizophrenia – Present and Lifetime version (K-SADS-PL).
Results
Parents’ reports of their own BI moderated the associations of both observed and parent-reported child BI at age 3 with children’s anxiety disorders at age 9. Among children whose parents reported having had higher childhood BI, those who exhibited high BI at age 3 were more likely to meet criteria for anxiety disorders at age 9.
Limitations
The major limitation is the use of a retrospective measure of parental BI.
Conclusions
These findings demonstrate that parents’ histories of childhood BI moderate the association between their young children’s BI and subsequent anxiety disorders. Thus, parental BI appears to identify a subgroup of BI children at particularly high risk for developing anxiety disorders by late childhood.
Keywords: Behavioral Inhibition, Anxiety, Child, Parent, Risk
Introduction
Behavioral inhibition (BI) is a temperamental style characterized by fear, wariness and avoidance of unfamiliar people, objects, and situations (Kagan, Reznick, Clarke, Snidman & Garcia-Coll, 1984). BI has been shown to be moderately stable (Degnan & Fox, 2007; Fox et al., 2005) and heritable (Dilalla et al., 1994; Robinson et al., 1992), although environmental variables, such as overprotective and intrusive parenting, also appear to play an important role (Degnan et al., 2008; Hane et al., 2008; Kiel & Buss, 2010; Rubin et al., 2002).
A number of studies have shown that BI is a risk factor for anxiety disorders, particularly social anxiety disorder (SAD), in late childhood and adolescence (Chronis-Tuscano et al., 2009; Clauss & Blackford, 2012; Hirshfeld-Becker et al., 2008; Muris et al., 2010; Schwartz et al., 1999). These findings have been obtained using laboratory observations (Hirshfeld-Becker et al., 2007; Schwartz et al., 1999), parent reports (Chronis-Tuscano et al., 2009; Muris et al., 2010), and composites of observations, parent reports, child self-reports and teacher reports of BI (Essex et al., 2010). A meta-analysis concluded that 43% of behaviorally inhibited children develop SAD compared to 12% of uninhibited children (Clauss & Blackford, 2012). In addition, childhood BI has been shown to predict generalized anxiety disorder, separation anxiety disorder, agoraphobia, specific phobias, and multiple anxiety disorders (Biederman et al., 1993; Hirshfeld et al., 1992; Hudson et al., 2011; Paulus et al., 2014).
However, many children with high BI do not develop anxiety disorders, which implies that there are other risk or resilience factors that influence the trajectories of inhibited children (Buss & Kiel, 2013; Buss & McDoniel, 2016; Lahat et al., 2011). A number of studies have examined which factors moderate the association between BI and subsequent anxiety. For example, among children with stable high BI, high maternal overcontrol predicted greater social anxiety symptoms in adolescence (Lewis-Morrarty et al., 2012). In addition, the association between high BI in middle childhood and non-social anxiety symptoms a year later was moderated by insecure attachment (Muris et al., 2010). Among 2-year olds with high BI, high levels of inhibitory control at age 4 were associated with greater anxiety symptoms at age 4–5, whereas high levels of attention shifting control were linked to lower anxiety symptoms (White, et al., 2011). Finally, two studies have reported that error monitoring, as indexed by the error-related negativity (ERN) in event-related potentials paradigms, moderate the association between BI and anxiety. One study reported that among children with high BI, those with an increased ERN in adolescence exhibited a higher rate of anxiety disorders (McDermott et al., 2009); the other study found that behaviorally inhibited 2–3 year olds with an increased ERN at age 7 exhibited greater social anxiety symptoms at age 9 (Lahat et al., 2014).
In light of evidence for the familial transmission of temperament (Saudino, & Micalizzi, 2015), another plausible moderator is parental history of BI. Parental BI may increase children’s risk for anxiety through a variety of environmental (e.g., overprotective parenting, modeling of reticence and avoidance), and genetic pathways that are only starting to be elucidated (e.g., Degnan & Fox, 2007; Degnan et al., 2008; Fox et al., 2005; Hane et al., 2008; Kiel & Buss, 2010; Rubin et al., 2002). Thus, it may represent an easily assessed proxy for the sum of these complex and still poorly understood processes (Yoon et al., 2002). Surprisingly, to our knowledge no previous study has explored whether a parental history of BI influences vulnerability to anxiety disorders among children with elevated levels of BI.
We investigated the role of parental history of BI in moderating the relationship between BI in a large community sample of 3-year old children and the child’s risk for developing an anxiety disorder by age 9. We hypothesized that behaviorally inhibited children whose parents reported having had elevated BI in childhood would be more likely to develop anxiety disorders by late childhood. As adults who retrospectively report having a high level of BI as children exhibit an elevated rate of anxiety disorders (Gladstone et al., 2005), and parental anxiety disorders are associated with both BI (Rosenbaum et al., 2005) and anxiety disorders (Micco et al., 2009) in their offspring, we adjusted for parental anxiety disorders in our analyses. Although the literature emphasizes the link between BI and risk for social anxiety disorder, BI also predicts other anxiety disorders (e.g., Hudson et al., 2011; Paulus et al., 2014) and there is considerable heterotypic continuity of anxiety disorders in children and adolescents (Copeland et al., 2014). Therefore, we focused on the broader group of anxiety disorders in our main analyses.
Method
Participants
The sample was drawn from a suburban community using commercial mailing lists. Families eligible for participation had a 3-year old child with no significant medical disorders or developmental disabilities and at least one biological English-speaking parent living in the household. Only one child per family was assessed. The primary caregiver served as the primary parent for our assessments; co-parents were also asked to complete a subset of the measures. 94.9% of the primary parents were mothers. Mean age for mothers at the initial assessment was 36.25 years (SD=4.51), and the mean age for fathers was 38.47 years (SD=5.38). Informed, voluntary, written consent was obtained from parents prior to participation. The study was approved by the Stony Brook University Institutional Review Board, and families were compensated. Families were assessed again when children were 6 and 9 years old. A battery of behavioral tasks and self-report measures was completed at every follow up. We chose to use the BI assessment from age 3 because in the literature BI is typically assessed in preschool or earlier. We used the diagnostic assessment at 9, rather than age 6, in order to maximize the number of new onsets and to be able to include children’s self-reports in the assessment, as parents’ reports alone tend to underestimate internalizing psychopathology (De Los Reyes & Kazdin, 2005). The only variable used from the age 6 follow up was the measure of retrospective parental BI – this was the only time it was administered.
Of the 559 families who entered the study, the 392 with complete data for all of the variables used in the main analyses were included in this paper. Slightly over half the children were male (53.6%), and most were of White/European-American descent and non-Hispanic (87.1%). The majority of children’s parents were married at the time of the first assessment (94.9%), and 73.0% of children had at least one parent with a college degree. The participants included in the analyses did not differ significantly from those excluded on any baseline variables used in the analyses or any of the demographic variables.
Measures
Child Behavioral Inhibition
Child BI was assessed when children were 3 years old using laboratory and parent-report measures.
Laboratory Temperament Assessment Battery (Lab-TAB)
Our observational measure of BI consisted of 3 episodes from the Lab-TAB (Goldsmith et al., 1995). The Lab-TAB has good interrater reliability (Durbin et al., 2005), exhibits moderate stability from age 3 to age 7 (Durbin et al., 2007; Majdandžić & van den Boom, 2007), and exhibits convergent validity with home observations (Durbin et al., 2007), parent-report temperament questionnaires (Pfeifer et al., 2002), and observer ratings (Gagne et al., 2011).
The 3 episodes were:
Risk Room. Child explored a set of novel and ambiguous stimuli, including a Halloween mask, balance beam, and black box.
Stranger Approach. Child was left alone briefly in the room before a male accomplice entered, speaking to the child while slowly walking closer.
Exploring New Objects. Child was given the opportunity to explore a set of novel and ambiguous stimuli, including a mechanical spider, a mechanical bird, and sticky soft gel balls.
Following previous studies (Durbin et al., 2005; Pfeifer et al., 2002; Kagan et al., 1988), the episodes were divided into 20- or 30-s epochs, and a series of affective and behavioral codes were rated for each epoch. BI was computed as the average standardized ratings of latency to fear (reversed); and facial, vocal, and bodily fear (Risk Room, Stranger Approach, and Exploring New Objects); latency to touch objects; total number of objects touched (reversed); tentative play; referencing the parent; proximity to parent; referencing the experimenter; and time spent playing (reversed; Risk Room and Exploring New Objects); startle (Exploring New Objects); sad facial affect (Exploring New Objects and Stranger Approach); latency to vocalize; approach toward the stranger (reversed); avoidance of the stranger; gaze aversion; and verbal and nonverbal interaction with the stranger (reversed, Stranger Approach) (Goldsmith et al., 1995; Durbin et al., 2005; Pfeifer et al., 2002). BI scores exhibited good internal consistency (α = .80) and interrater reliability (intraclass correlation [ICC] = .88, N = 28).
Behavioral Inhibition Questionnaire (BIQ)
The BIQ (Bishop et al., 2003) is a 30-item questionnaire designed to measure the frequency of a child’s BI across six contexts in three different domains: social novelty (unfamiliar adults, peers, and performing in front of others), situational novelty (unfamiliar situations, preschool/separation), and novel physical activities with risk of injury. Items are rated on a 7-point scale ranging from 1 (hardly ever) to 7 (almost always). The BIQ has good reliability and convergent and discriminant validity (Bishop, Spence & McDonald, 2003; Kim et al., 2011). It was completed by the child’s primary caregiver at the initial assessment (α=.96).
Parent Behavioral Inhibition
Retrospective Measure of Behavioral Inhibition (RMBI)
The RMBI (Gladstone & Parker, 2005) is an 18-question measure designed to assess adults’ retrospective perceptions of their own BI as children before age 13. The scale assesses the main behavioral features of BI included in observational measures. Examples of items include “At school, did you find it difficult to approach and play with new children?”, “Did you prefer parties with crowds of children rather than small gatherings?” and “Were you outgoing and talkative with other children?” Items are rated on a 3-point scale (0=no/hardly ever; 1=some of the time; 2=yes/most of the time) and include a “do not remember option” to discourage guessing. The RMBI is highly correlated with the Retrospective Self-Report of Inhibition (Reznick et al., 1992) as well as with informants’ reports on the RMBI (Gladstone & Parker, 2005). Both of the children’s parents completed the RMBI at the second (age 6) assessment. In this sample coefficient alpha was .85 for mothers and .84 for fathers. Both parents’ responses were averaged to create a composite score; where only one parent’s report was available, that score was used. We opted to average parent scores under the assumption that the child is influenced by both parents’ BI, and to reduce the number of analyses. However, we report supplementary analyses for each parent separately. Data were available from both parents for 296 families; 78 families had data for mothers only, and 18 families had data for fathers only.
Child Anxiety
Preschool Age Psychiatric Assessment (PAPA)
The PAPA (Egger et al., 1999) is an interviewer-based structured diagnostic interview that assesses parent-reported psychiatric disorders in preschoolers from ages 2–6. The interview was administered to the child’s primary caregiver at the initial assessment and covers the common DSM-IV-TR disorders (American Psychiatric Association, 2000) using the past 3 months as the time frame. The child’s primary parent (384 mothers, 7 fathers, and 1 both parents) was interviewed by graduate students in clinical psychology who received training on the administration of the PAPA by its developers. Interviews were conducted by telephone. Parent reports of child psychopathology obtained by telephone interviews are generally consistent with face-to-face interviews (Lyneham & Rapee, 2005). DSM-IV anxiety disorder diagnoses were derived using algorithms created by the PAPA’s developers (see Table 1 for rates of child anxiety diagnoses at age 3). Although diagnoses were based on algorithms, a second diagnostician independently rated a small number of audiotapes of interviews enriched for children with evidence of psychopathology (N = 21). Kappa, for interrater reliability, was 1.00.
Table 1.
Childrens’ current diagnoses at ages 3 and 9.
| Age 3 | Age 9 | |||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Specific Phobia | 37 | 9.4% | 38 | 9.7% |
| GAD | 16 | 4.1% | 20 | 5.1% |
| Separation Anx | 23 | 5.9% | 24 | 6.1% |
| Social Phobia | 13 | 3.3% | 12 | 3.1% |
| Panic | – | – | 1 | .3% |
| Agoraphobia | – | – | 2 | .5% |
| OCD | – | – | – | – |
| PTSD | – | – | – | – |
| Multiple Anxiety | 15 | 3.9% | 13 | 3.3% |
| MDD | 5 | 1.3% | 2 | .5% |
| ADHD | 9 | 2.3% | 49 | 12.5% |
| Disruptive Behavior | 43 | 11.0% | 14 | 3.6% |
Kiddie Schedule for the Affective Disorders and Schizophrenia – Present and Lifetime version (K-SADS-PL)
The K-SADS-PL (Axelson et al., 2009) is a widely used semi-structured diagnostic interview for children and adolescents. It was administered separately to a parent and the child during the age 9 assessment wave. Current and lifetime diagnoses of anxiety disorders were derived using DSM-IV criteria (see Table 1).
Graduate students in clinical psychology and M.A. level staff members conducted the K-SADS interviews after receiving training from an expert diagnostic interviewer. All interviews were conducted in-person. Parents (91.8% mothers) were interviewed first, with interviews lasting 1–2 hours, and children were interviewed immediately after, with their interviews lasting approximately 1 hour. Differences between parent and child reports were reconciled by the interviewer as necessary.
To examine interrater reliability, a second rater from the pool of interviewers independently rated 74 videotapes. Kappas for lifetime and current anxiety disorder diagnoses (including Anxiety Not-Otherwise-Specified [NOS]) were .67 and .55, respectively, which fall in the substantial and moderate ranges (Landis & Koch, 1977).
Parent Anxiety
Structured Clinical Interview for DSM-IV non-patient version (SCID)
The SCID (First et al., 1996) is one of the most widely used structured diagnostic interviews for adults. As part of the age 3 and age 9 assessment, 489 mothers and 429 fathers were interviewed by Master’s level raters via telephone and diagnoses were derived using DSM-IV criteria. Lifetime anxiety disorder diagnosis was based on interviews conducted at the age 3 and age 9 follow ups. Interrater reliability for a lifetime anxiety disorder diagnosis, based on audiotapes, was К =.72 (N=45), which falls in the substantial range (Landis & Koch, 1977). 194 children had at least one parent with a lifetime anxiety diagnosis (49.5%), including 140 mothers (35.7%) and 91 fathers (23.1%).
Results
Table 2 provides descriptive data and correlations for all variables used in these analyses. The correlation between observed (Lab-TAB) and parent-reported (BIQ) BI was .26 (p < .01), which is consistent with other studies reporting associations between laboratory observations and parent reports of temperament (e.g., Gartstein, & Marmion, 2008; Hayden et al., 2010). Parents’ averaged reports of their own childhood BI was significantly associated with the primary parent’s report of the child’s BI, but the correlation reached only a trend level of significance (p < .08) with the child’s Lab-TAB BI score.
Table 2.
Correlations and descriptive statistics for main variables used in analyses.
| Age 3 Lab-TAB BI | Age 3 Parent-reported BI | Age 3 Anxiety | Age 9 Current Anxiety | Age 9 Lifetime Anxiety | Average Parental Retrospective BI | Parent Lifetime Anxiety | Mean/% of sample | SD/N | Range | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age 3 Lab-TAB BI | – | .26** | .10* | .06 | .07 | .09+ | −.02 | .63 | .20 | 0.00–1.37 |
| Age 3 Parent-reported BI | – | .32** | .15** | .17** | .15** | .07 | 88.42 | 31.40 | 30.00–196.00 | |
| Age 3 Child Anxiety | – | .09+ | .16** | .04 | .07+ | 19.4 % | 76 | – | ||
| Age 9 Current Anxiety | – | .90** | .02 | .05 | 19.6 % | 77 | – | |||
| Age 9 Lifetime Anxiety | – | .01 | .09+ | 23.7 % | 93 | – | ||||
| Average Parental Retrospective BI | – | .18** | 12.29 | 4.82 | 2.12–29.65 | |||||
| Parent Lifetime Anxiety | – | 49.5 % | 194 | – |
p<.01;
p<.05;
p<.10
Preliminary analyses
Multiple logistic regression models were used to test whether parents’ reports of their own childhood BI moderated the association between their child’s BI at age 3 and the child’s lifetime and current anxiety disorder at age 9. Significant interactions were decomposed using Aiken & West’s (1991) procedures. In each of the analyses, we controlled for child sex, child age 3 anxiety disorder, and lifetime history of parental anxiety disorder. In the initial set of analyses, we determined whether mothers’ versus fathers’ retrospective reports of their own childhood BI differentially moderated the associations between child BI and subsequent child anxiety disorders. We tested two pairs of models that included age 3 child BI and mothers’ and fathers’ reports of their own BI as independent variables and child sex, child age 3 anxiety disorder, and lifetime maternal and paternal anxiety disorders as covariates. The first model in each pair used the Lab-TAB to assess child BI; the second model in each pair used the BIQ to index child BI. For the first pair of models, the dependent variable was child current anxiety disorder at age 9; in the second pair of models, the dependent variable was child lifetime anxiety disorder through age 9.
None of the three-way interactions between mothers’ retrospectively reported BI, fathers’ retrospectively reported BI, and age 3 child BI (assessed with either the Lab-TAB or BIQ) significantly predicted current or lifetime child anxiety disorder at age 9 (for current anxiety disorder, OR=1.004, 95% CI= .964–1.046, p=.84 for observed child BI, and OR=.9999, 95% CI=.9997–1.0002, p=.59 for parent-reported child BI; for lifetime anxiety disorder, OR= 1.004, 95% CI= .965–1.046, p=.83 for observed child BI and OR:1.00001, 95% CI=.99977–1.00026, p=.91 for parent-reported child BI). As these analyses indicate that mothers’ and fathers’ retrospective reports of their own childhood BI did not have significantly different effects on the associations between children’s BI and their subsequent risk for anxiety disorders, in our primary analyses we averaged parents’ retrospective reports of their own BI. However, we also conducted secondary analyses examining maternal and paternal BI separately.
Primary Analyses
In the first set of primary analyses, we examined whether the relationship between laboratory observations of children’s BI at age 3 and child anxiety disorders by age 9 was moderated by parents’ averaged retrospective reports of their own childhood BI (see Table 3). There was a significant main effect for age 3 child anxiety disorder on age 9 child lifetime (but not current) anxiety disorder. In addition, we found significant interactions between parents’ averaged reports of their own childhood BI and their children’s observed BI at age 3 in predicting both current and lifetime child anxiety disorder at age 9. When decomposed, the interactions revealed that among children of parents who reported having had higher levels of BI in childhood, child BI at age 3 was significantly associated with risk for developing a current (OR=9.24, 95% CI=1.50–57.00, p=.02) and lifetime (OR=7.86, 95% CI=1.33–46.34, p=.02) anxiety disorder (see Figure 1). Among children of parents who reported having had lower levels of BI, there was no relationship between the child’s BI and their likelihood of developing an anxiety disorder by age 9 (current: OR=.37, 95% CI=.06–2.26, p>.10; lifetime: OR=.42, 95% CI=.08–2.29, p>.10). When child Anxiety NOS diagnoses were excluded, the interactions remained significant in predicting both lifetime (OR=1.43, 95% CI=1.10–1.87, p=.008) and current (OR=1.49, 95% CI=1.13–1.96, p = .004) age 9 anxiety disorders.
Table 3.
Effects of parents’ retrospective reports of their own behavioral inhibition (BI) and child age 3 laboratory observed BI on child age 9 anxiety
| Step 1 | Age 9 Lifetime Anxiety Disorder | Age 9 Current Anxiety Disorder | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Wald | OR | 95% CI | Wald | OR | 95% CI | |
| Child Sex | 1.438 | 1.345 | .829–2.181 | .255 | 1.411 | .684–1.904 |
| Age 3 Anxiety | 6.358 | 2.045* | 1.173–3.567 | 1.294 | 1.420 | .776–2.597 |
| Parental lifetime history of Anxiety | 2.692 | 1.506 | .923–2.456 | 1.116 | 1.322 | .787–2.221 |
| Age 3 Child Lab-TAB BI | .919 | 1.799 | .542–5.975 | 1.034 | 1.933 | .543–6.885 |
| Average Parent BI | .052 | 1.006 | .957–1.058 | .239 | 1.013 | .961–1.068 |
| Step 2 | ||||||
| Child Sex | .955 | 1.277 | .782–2.085 | .073 | 1.074 | .638–1.807 |
| Age 3 Anxiety | 5.672 | 1.986* | 1.129–3.492 | .937 | 1.356 | .732–2.510 |
| Parental lifetime history of Anxiety | 2.392 | 1.474 | .902–2.408 | .915 | 1.290 | .768–2.174 |
| Age 3 Child Lab-TAB BI | .866 | 1.805 | .521–6.257 | .848 | 1.857 | .497–6.934 |
| Average Parent BI | .004 | .998 | .948–1.051 | .014 | 1.003 | .950–1.060 |
| Age 3 Child BI X Avg Parental BI | 5.578 | 1.354* | 1.053–1.742 | 6.428 | 1.392* | 1.078–1.798 |
OR = Odds ratio; Lab-TAB = Laboratory Temperament Assessment Battery
p < .001;
p < .01;
p < .05;
p < .10
Figure 1.
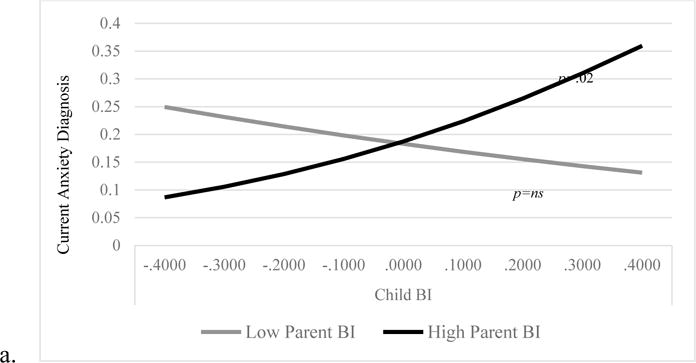
The interaction between age 3 child Laboratory Temperament Assessment Battery Behavioral Inhibition (BI) and parental retrospective self-reported BI predicting child current anxiety diagnosis at age 9 (top) and child lifetime anxiety diagnosis at age 9 (bottom). Variables on the x-axis are centered. The upper and lower values represent +/− 1 SD of the mean, which is 0.
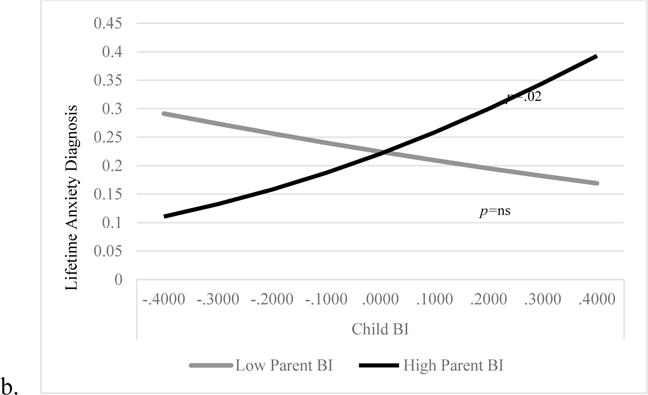
Next, we examined whether the relationship between the primary parent’s report of their child’s BI at age 3 and children’s anxiety disorders at age 9 was moderated by parents’ averaged retrospective reports of their own childhood BI (see Table 4). There was a main effect of child age 3 parent-reported BI in predicting both child age 9 current and lifetime anxiety disorders. For child current anxiety disorders, however, this was qualified by a significant interaction with parents’ retrospective reports of their own childhood BI. Decomposition of the interaction revealed that among children of parents who reported having had higher levels of childhood BI, higher levels of parent-reported child BI at age 3 significantly predicted a higher rate of current anxiety disorder at age 9 (OR=1.02, 95% CI=1.01–1.03, p<.01). Conversely, among children of parents who reported having had lower levels of childhood BI, there was no relationship between parents’ reports of the child’s BI at age 3 and the child’s probability of having an anxiety disorder at age 9 (OR=1.00, 95% CI=.99–1.01, p>.10; see Figure 2). When Anxiety NOS diagnoses were excluded, the interaction for child current anxiety disorder was reduced to a trend (OR=1.002, 95% CI=1.000–1.003, p=.07). The interaction between averaged parental retrospective self-reports of their own childhood BI and primary parent-reported child BI at age 3 in predicting children’s lifetime anxiety disorder at age 9 was not significant.1,2
Table 4.
Effects of parents’ retrospective reports of their own behavioral inhibition (BI) and parent-reported child age 3 BI on child age 9 anxiety
| Step 1 | Age 9 Lifetime Anxiety Disorder | Age 9 Current Anxiety Disorder | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Wald | OR | 95% CI | Wald | OR | 95% CI | |
| Child Sex | 2.270 | 1.461 | .892–2.393 | .600 | 1.229 | .729–2.072 |
| Age 3 Anxiety | 2.630 | 1.642 | .902–2.990 | .073 | 1.095 | .567–2.116 |
| Parental lifetime history of Anxiety | 1.888 | 1.424 | .860–2.357 | .553 | 1.225 | .717–2.094 |
| Age 3 Child Parent-Reported BI | 5.000 | 1.009* | 1.001–1.018 | 4.397 | 1.009* | 1.001–1.018 |
| Average Parent BI | .045 | .994 | .942–1.049 | .002 | 1.001 | .946–1.060 |
| Step 2 | ||||||
| Child Sex | 2.077 | 1.440 | .877–2.364 | .462 | 1.200 | .709–2.032 |
| Age 3 Anxiety | 2.418 | 1.612 | .883–2.944 | .032 | 1.062 | .547–2.064 |
| Parental lifetime history of Anxiety | 2.087 | 1.451 | .876–2.406 | .700 | 1.259 | .734–2.158 |
| Age 3 Child Parent-Reported BI | 5.150 | 1.010* | 1.001–1.018 | 4.533 | 1.010* | 1.001–1.019 |
| Average Parent BI | .295 | .984 | .930–1.042 | .231 | .985 | .927–1.047 |
| Age 3 Child BI X Avg Parental BI | 2.412 | 1.001 | 1.000–1.003 | 4.538 | 1.002* | 1.000–1.004 |
OR = Odds ratio.
p < .001;
p < .01;
p < .05;
p < .10
Figure 2.
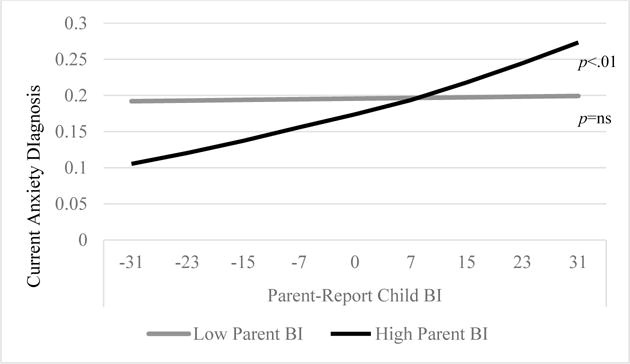
The interaction between age 3 parent-reported child BI and retrospectively self-reported parent BI predicting age 9 current anxiety diagnosis. Variables on the x-axis are centered. The upper and lower values represent +/− 1 SD of the mean, which is 0.
Secondary Analyses
In secondary analyses, we examined the effects of mothers’ and fathers’ retrospective reports of their own childhood BI separately. The findings described above for Lab-TAB BI appeared to be driven primarily by fathers’ reports of their own BI. Using only paternal retrospective reports, there was a significant interaction between fathers’ reports of their own childhood BI and child age 3 Lab-TAB BI in predicting both current and lifetime child anxiety disorder (OR=1.38, 95% CI= 1.10–1.73, p=.006 and OR= 1.26, 95% CI=1.02–1.55, p=.03 respectively). Among children of fathers who had had higher levels of BI, elevated age 3 Lab – TAB BI scores predicted higher rates of current and lifetime anxiety disorders at age 9. In contrast, among children of fathers with lower self-reported BI, age 3 Lab-TAB BI was not associated with subsequent anxiety disorders (data available upon request). In contrast, using only maternal retrospective reports of BI, the interactions with age 3 child Lab-TAB BI in predicting child age 9 anxiety disorder were not significant (current anxiety: OR= 1.12, 95% CI= .92–1.37, p=.28; lifetime anxiety: OR=1.17, 95% CI=.96–1.43, p=.12).
In contrast, the interactions between parent-reported child BI and parents’ retrospective reports of their own BI on child current and lifetime anxiety diagnosis appeared to be stronger for mothers. Using maternal retrospective reports of BI as a predictor, there were significant interactions with parent-reported child BI at age 3 in predicting both current (OR=1.0015, 95% CI=1.0001–1.0028, p=.03) and lifetime (OR=1.0014, 95% CI=1.0001–1.0027, p=.03) anxiety disorders at age 9. Among children of mothers who reported having had higher levels of childhood BI, higher parent-reported child BI at age 3 predicted a greater probability of the child exhibiting a current or lifetime anxiety disorder by age 9. However, among children of mothers with lower retrospective self-reported BI, parent-reported BI at age 3 was not associated with the children’s risk for anxiety disorders by age 9. When we used only paternal self-reports of their own childhood BI as a predictor, the interactions with primary parent-reported child BI at age 3 in predicting child current (OR=1.0004, 95% CI=.9988–1.0019, p=.66) and lifetime (OR=.9996, 95% CI=.9982–1.0010, p=.60) anxiety disorders at age 9 were not significant.
Lastly, we repeated the primary analyses predicting specific lifetime anxiety disorders at age 9 for those diagnoses with at least a dozen cases (Separation Anxiety Disorder, N = 24; Social Phobia, N = 13; Specific Phobia, N = 45; GAD N = 20). We used only lifetime diagnoses in order to maximize the number of cases in each analysis; participants with no lifetime history of anxiety disorder served as the comparison group. As above, all analyses controlled for child sex, parental anxiety disorder, and age 3 child anxiety disorder. The interactions between age 3 Lab-TAB BI and parents’ averaged retrospective reports of their own childhood BI were significant in predicting age 9 GAD (OR=1.74, 95% CI=1.20–2.51, p=.003) and Specific Phobia (OR=1.51, 95% CI=1.11–2.04, p=.008), as well as Separation Anxiety Disorder at a trend level (OR=1.41, 95% CI=.99–2.02, p=.058). Decomposition of these interactions revealed that among children of parents with higher levels of retrospectively-reported BI, those who exhibited higher age 3 observed BI had a greater risk of developing each of these specific anxiety disorders, whereas there were no associations among children of parents with lower levels of retrospectively-reported BI (data available on request). There were no significant interactions between parent-reported age 3 child BI and parents’ average retrospective reports of their own BI in predicting any of the individual anxiety disorders.
Discussion
Numerous studies have reported links between childhood BI and later development of anxiety disorders (Clauss & Blackford, 2012; Fox et al., 2005; Hirshfeld-Becker et al., 2008). However, only a subset of behaviorally inhibited children develop anxiety disorders, suggesting the importance of identifying moderators of this relationship (Buss & Kiel, 2013; Lahat et al., 2011). To our knowledge, this is the first study to examine the effects of parents’ own histories of BI on the association between children’s BI and risk for subsequent anxiety disorders.
After controlling for child sex, child baseline anxiety disorder, and lifetime history of parental anxiety disorder, parents’ retrospective reports of their own childhood BI moderated the relationship between age 3 child BI and the subsequent development of anxiety disorders by age 9. Specifically, among children of parents who retrospectively reported having had a higher level of childhood BI, both observed and parent-reported child BI at age 3 was associated with an increased risk for developing an anxiety disorder at age 9. Conversely, among children of parents who reported having had a lower level of childhood BI, there was no association between child age 3 BI and anxiety disorders 6 years later. Importantly, these findings were evident using both laboratory observation and parent-report measures of BI despite the modest correlation between these measures. Thus, behaviorally inhibited children whose parents also have a history of BI themselves appear to be a subgroup that is at particularly high risk for developing clinically significant anxiety and could be targeted for early intervention. At the same time, behaviorally inhibited children whose parents do not report a history of BI do not appear to have a particularly high likelihood of developing anxiety disorders in childhood, and therefore may not benefit from intervention efforts.
In this paper, we did not attempt to identify the mechanisms through which parental BI potentiated the effects of child BI on children’s risk for anxiety. However, it is reasonable to hypothesize that parents with a history of BI engage in parenting practices, such as being overprotective and/or modeling avoidant behavior, that increase susceptibility to anxiety in temperamentally vulnerable offspring (Degnan et al., 2008; Hane et al., 2008; Kiel & Buss, 2010; Lewis-Morrarty et al., 2012). Parental BI may also be a marker for a more genetic or severe subtype of BI that is associated with greater vulnerability. Thus, we regard parental BI as a proxy for more complex and still poorly understood processes, such as genetic and epigenetic mechanisms, parenting, and other contextual influences. It is important to continue to elucidate these processes. However, in the meanwhile retrospective reports of parental BI have the virtue of being easily assessed and provide a simple risk indictor that reflects the influence of multiple additive or interactive processes.
Secondary analyses suggested that when laboratory observations of child BI were used, fathers’ reports of their own childhood BI drove the interaction, but when parent-reports of child BI were used, the interaction was primarily due to mothers’ reports of their own BI. The reasons for this difference are unclear, although one consideration in the latter analyses is that mothers were typically the primary caregivers, hence were likely to be the informant for both the BIQ and the K-SADS. Importantly, however, the difference between the effects of mothers’ versus fathers’ BI on the association between child BI and the later development of anxiety disorders was not significant. Hence, these results must be viewed cautiously and should not be overinterpreted.
Our primary analyses focused on anxiety disorders as a whole, rather than on specific anxiety disorders, such as social anxiety, which has the strongest link to BI. We chose a broader focus due to concerns about statistical power, given our use of a community sample, and evidence suggesting that BI predisposes to a range of anxiety psychopathology (Biederman et al., 1993; Hirshfeld et al., 1992; Hudson et al., 2011; Paulus et al., 2014). For example, Paulus and colleagues (2014) recently reported that BI in early childhood predicted all forms of anxiety disorder. In our secondary analyses examining specific anxiety disorders, parents’ retrospective reports of their own childhood BI moderated the relationship between child age 3 Lab-TAB BI and age 9 lifetime GAD and specific phobia, as well as separation anxiety disorder at trend level. Interestingly, the effect was not significant for social phobia. However, there were fewer cases of social phobia in our sample. Moreover, there is substantial heterotypic continuity between anxiety disorders in childhood and later in development, and social anxiety disorder is often not apparent until adolescence (Copeland et al., 2014), hence the results may differ if children are assessed in adolescence or adulthood.
Parent anxiety predicted child 9 lifetime anxiety only at a trend level (r=.09, p<.10). While we expected a larger effect for parental transmission, it is important to note that child anxiety was assessed at age 9, which is before the peak age of onset for this disorder. Thus, this effect is likely to increase as the children get older. In addition, the correlation between age 3 child anxiety and age 9 child lifetime anxiety was small, albeit significant (r=.16, p<.01). This may reflect the uncertain boundaries for diagnosing anxiety disorders in preschoolers (Egger & Emde, 2011), and the fact that different measures and informants were used in assessing anxiety at age 3 and at age 9. At age 3, we used the PAPA and only parents were interviewed. At age 9, we used the K-SADS and interviewed both parents and children.
Finally, the current study adds to the evidence supporting the construct validity of the RMBI (Gladstone & Parker, 2005, 2006; Myers et al., 2012). Obtaining parents’ reports of their own history of childhood BI takes relatively little time, and can be readily incorporated into clinical practice and screening programs in order to refine risk prediction for pediatric anxiety (Rapee, 2013).
Strengths of this study include a large sample, a longitudinal design spanning six years, inclusion of fathers as well as mothers, use of both observational and parent-reported measures of child BI, and semi-structured interviews to assess anxiety disorders. In addition, we conservatively adjusted analyses for child age 3 anxiety disorder and parents’ lifetime histories of anxiety disorder to guard against spurious results caused by correlated risk factors.
However, the findings should be interpreted in light of the study’s limitations. First, there are differing opinions in the literature about whether to treat BI as a category or dimension. Some studies regard it as a type, whereas others consider it as a continuous variable (Clauss & Blackford, 2012). We chose to use a dimensional measure due to the greater reliability and validity of continuous variables (Markon et al., 2011), the lack of consensus about the optimal cut-point, and because our design used an unselected sample rather than selecting extreme groups.
Second, we used a retrospective measure of parental BI, and cannot be certain that parents are accurately recalling their own behaviors as children, or that their self-ratings are not influenced by observations of their child’s temperament or their own current mood. However, Yancura and Aldwin (2009) found moderate to high stability between reports at two time points 5 years apart on a similar retrospective measure, with little influence of mood state on participants’ reports (Yancura & Aldwin, 2009). In addition, Gladstone et al., (2005) found that the RMBI was uniquely associated with anxiety disorders over and above the effects of current anxiety and BI. In the current sample, correlations between the RMBI and lifetime anxiety disorder were fairly low (for mothers, r = .27; for fathers, r = .19, and for both parents combined, r = .18).
It is also important to consider the timing of assessments when interpreting these findings. Although Clauss & Blackford (2012) concluded that age at BI assessment and age at anxiety assessment had very little impact on study effect sizes, the risk period for anxiety disorders continues through young adulthood. Hence, continued follow-up of this sample is warranted.
Finally, the current sample is relatively homogeneous. Further work is needed to determine whether these findings can be generalized to a more diverse population.
In conclusion, these findings extend the growing literature on moderators of the relationship between early BI and later child anxiety disorders. Obtaining information on parents’ history of BI as part of an evaluation of behaviorally inhibited children may help identify the best candidates for early intervention, thus reducing costs and unnecessary treatment in temperament-based anxiety prevention programs (Rapee, 2013).
Highlights.
Parental behavioral inhibition moderates the link between childhood BI and anxiety disorders
These findings are significant using both observational and parent reports of child BI
Parents’ histories of BI may be useful in predicting outcomes of BI children
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All analyses were also conducted using current and lifetime anxiety symptoms, and yielded a very similar pattern of results.
We also created a composite of both measures of BI by standardizing both scores and summing them. Again, the pattern of results was the same; there was a significant interaction between averaged retrospective reports of parental BI and summed standardized scores of age 3 child BI predicting both age 9 current (OR=1.05, 95% CI=1.016–1.087, p=.004) and lifetime (OR=1.041, 95% CI=1.008–1.076, p=.014) anxiety disorder diagnosis.
References
- Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. Sage Publications; California: 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. fourth. Washington, DC: Author; 2000. [Google Scholar]
- Axelson D, Birmaher B, Zelazny J, Kaufman J, Gill MK. The schedule for affective disorders and Schizophrenia–Present and lifetime version (K-SADS-PL) 2009 working draft. Advanced Centre for Intervention and Services Research, Western Psychiatric Institute and Clinic; 2009. Available from: http://www.psychiatry.pitt.edu/research/tools-research/ksads-pl-2009-working-draft. [Google Scholar]
- Biederman J, Rosenbaum JF, Bolduc-Murphy EA, Farone SV, Chaloff J, Hirschfeld DR, Kagan J. A 3-year follow-up of children with and without behavioral inhibition. J Am Acad Child Adolesc Psychiatry. 1993;32(4):814–821. doi: 10.1097/00004583-199307000-00016. [DOI] [PubMed] [Google Scholar]
- Bishop G, Spence SH, McDonald C. Can parents and teachers provide a reliable and valid report of behavioral inhibition? Child Dev. 2003;74(6):1899–1917. doi: 10.1046/j.1467-8624.2003.00645.x. [DOI] [PubMed] [Google Scholar]
- Buss KA, Kiel E. Temperamental risk factors for pediatric anxiety disorders. In: Vasa R, Roy A, editors. Pediatric Anxiety Disorders: A Clinical Guide. New York: Springer; 2013. pp. 47–68. [Google Scholar]
- Buss KA, McDoniel ME. Improving the prediction of risk for anxiety development in temperamentally fearful children. Curr Dir Psychol. 2016;25:14–20. doi: 10.1177/0963721415611601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, Raggi VL, Fox NA. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. J Am Acad Child Adolesc Psychiatry. 2009;48(9):928–935. doi: 10.1097/CHI.0b013e3181ae09df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: A meta-analytic study. J Am Acad Child Adolesc Psychiatry. 2012;51(10):1066–1075. doi: 10.1016/j.jaac.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2014;53(1):21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degnan KA, Fox NA. Behavioral inhibition and anxiety disorders: Multiple levels of a resilience process. Dev Psychopathol. 2007;19(03):729–746. doi: 10.1017/S0954579407000363. [DOI] [PubMed] [Google Scholar]
- Degnan KA, Henderson HA, Fox NA, Rubin KH. Predicting social wariness in middle childhood: The moderating roles of childcare history, maternal personality and maternal behavior. Soc Dev. 2008;17(3):471–487. doi: 10.1111/j.1467-9507.2007.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilalla LF, Kagan J, Reznick J. Genetic etiology of behavioral inhibition among 2-year-old children. Infant Behav Dev. 1994;17(4):405–412. [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull. 2005;131(4):483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Hayden EP, Klein DN, Olino TM. Stability of laboratory-assessed temperamental emotionality traits from ages 3 to 7. Emotion. 2007;7(2):388. doi: 10.1037/1528-3542.7.2.388. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. J Abnorm Psychol. 2005;114(1):28. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- Durham, NC.Egger HL, Ascher BH, Angold A. The Preschool Age Psychiatric Assessment: Version 1.1. Duke University Medical Center, Department of Psychiatry and Behavioral Sciences, Center for Developmental Epidemiology; 1999. [Google Scholar]
- Egger HL, Emde RN. Developmentally sensitive diagnostic criteria for mental health disorders in early childhood: The Diagnostic and Statistical Manual of Mental Disorders—IV, the Research Diagnostic Criteria—Preschool Age, and the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood— Revised. Am Psychol. 2011;66(2):95–106. doi: 10.1037/a0021026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essex M, Klein M, Slattery M, Goldsmith H, Kalin N. Early risk factors and developmental pathways to chronic high inhibition and social anxiety disorder in adolescence. Am J Psychiatry. 2010;167(1):40–46. doi: 10.1176/appi.ajp.2009.07010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Williams J, Gibbon M. Version. Vol. 1. American Psychiatric; Washington, DC: 1995. Structured clinical interview for DSM-IV-non-patient edition (SCID-NP) p. 0. [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: Linking biology and behavior within a developmental framework. Annu Rev Psychol. 2005;56(1):235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- Gagne JR, Van Hulle CA, Aksan N, Essex MJ, Goldsmith HH. Deriving childhood temperament measures from emotion-eliciting behavioral episodes: Scale construction and initial validation. Psychol Assessment. 2011;23(2):337. doi: 10.1037/a0021746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartstein MA, Marmion J. Fear and positive affectivity in infancy: Convergence/discrepancy between parent-report and laboratory-based indicators. Infant Behav Dev. 2008;31:227–238. doi: 10.1016/j.infbeh.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladstone G, Parker G. Measuring a behaviorally inhibited temperament style: Development and initial validation of new self-report measures. Psychiatry Res. 2005;135(2):133–143. doi: 10.1016/j.psychres.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Gladstone GL, Parker GB. Is behavioral inhibition a risk factor for depression? Journal Affect Disord. 2006;95(1–3):85–94. doi: 10.1016/j.jad.2006.04.015. [DOI] [PubMed] [Google Scholar]
- Gladstone G, Parker G, Mitchell P, Wilhelm K, Malhi G. Relationship between self-reported childhood behavioral inhibition and lifetime anxiety disorders in a clinical sample. Depress Anxiety. 2005;22(3):103–113. doi: 10.1002/da.20082. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Reilly J, Lemery KS, Longley S, Prescott A. Preschool Laboratory Temperament Assessment Battery. University of Wisconsin; 1995. Unpublished instrument. [Google Scholar]
- Hane AA, Cheah C, Rubin KH, Fox NA. The role of maternal behavior in the relation between shyness and social reticence in early childhood and social withdrawal in middle childhood. Soc Dev. 2008;17(4):795–811. [Google Scholar]
- Hayden EP, Durbin CE, Klein DN, Olino TM. Maternal reports of child temperament: Associations with mothers’ personality and internalizing symptoms. J Pers Assess. 2010;92:586–593. doi: 10.1080/00223891.2010.513308. [DOI] [PubMed] [Google Scholar]
- Hirshfeld DR, Rosenbaum J, Biederman J, Bolduc EA, Farone SV, Snidman N, Reznick JS, Kagan J. Stable behavioral inhibition and its association with anxiety disorder. J Am Acad Child Adolesc Psychiatry. 1992;31(1):103–111. doi: 10.1097/00004583-199201000-00016. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Henin A, Farone SV, Davis S, Harrington K, Rosenbaum JF. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: A five-year follow-up. J Dev Behav Pediatr. 2007;28(3):225–233. doi: 10.1097/01.DBP.0000268559.34463.d0. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Micco J, Henin A, Bloomfield A, Biederman J, Rosenbaum J. Behavioral inhibition. Depress Anxiety. 2008;25(4):357–367. doi: 10.1002/da.20490. [DOI] [PubMed] [Google Scholar]
- Hudson J, Dodd H, Lyneham H, Bovopoulous N. Temperament and family environment in the development of anxiety disorder: Two-year follow-up. J Am Acad Child Adolesc Psychiatry. 2011;50(12):1255–1264. doi: 10.1016/j.jaac.2011.09.009. [DOI] [PubMed] [Google Scholar]
- Kagan J, Reznick JS, Clarke C, Snidman N, Garcia-Coll C. Behavioral inhibition to the unfamiliar. Child Dev. 1984;55(6):2212–2225. [Google Scholar]
- Kagan J, Reznick JS, Snidman N, Gibbons J, Johnson MO. Childhood derivatives of inhibition and lack of inhibition to the unfamiliar. Child Dev. 1988;59(6):1580–1589. doi: 10.1111/j.1467-8624.1988.tb03685.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Method Psych. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiel EJ, Buss KA. Maternal accuracy and behavior in anticipating children’s responses to novelty: Relations to fearful temperament and implications for anxiety development. Soc Dev. 2010;19(2):304–325. doi: 10.1111/j.1467-9507.2009.00538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Klein DN, Olino TM, Dyson MW, Dougherty LR, Durbin CE. Psychometric properties of the Behavioral Inhibition Questionnaire in preschool children. Journal Pers Assess. 2011;93(6):545–555. doi: 10.1080/00223891.2011.608756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahat A, Hong M, Fox NA. Behavioural inhibition: Is it a risk factor for anxiety? Int Rev Psychiatry. 2011;23(3):248–257. doi: 10.3109/09540261.2011.590468. [DOI] [PubMed] [Google Scholar]
- Lahat A, Lamm C, Chronis-Tuscano A, Pine DS, Henderson HA, Fox NA. Early behavioral inhibition and increased error monitoring predict later social phobia symptoms in childhood. J Am Acad Child Adolesc Psychiatry. 2014;53(4):447–455. doi: 10.1016/j.jaac.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lewis-Morrarty E, Degnan KA, Chronis-Tuscano A, Rubin KH, Cheah CS, Pine DS, Henderon HA, Fox NA. Maternal over-control moderates the association between early childhood behavioral inhibition and adolescent social anxiety symptoms. J Abnorm Child Psychol. 2012;40(8):1363–1373. doi: 10.1007/s10802-012-9663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyneham HJ, Rapee RM. Agreement between telephone and in-person delivery of a structured interview for anxiety disorders in children. J Am Acad Child Adolesc Psychiatry. 2005;44(3):274–282. doi: 10.1097/00004583-200503000-00012. [DOI] [PubMed] [Google Scholar]
- Majdandžić M, Van Den Boom DC. Multimethod longitudinal assessment of temperament in early childhood. J Pers. 2007;75(1):121–168. doi: 10.1111/j.1467-6494.2006.00435.x. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychol Bull. 2011;137(5):856. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- McDermott JM, Perez-Edgar K, Henderson HA, Chronis-Tuscano A, Pine DS, Fox NA. A history of childhood behavioral inhibition and enhanced response monitoring in adolescence are linked to clinical anxiety. Biol Psychiatry. 2009;65(5):445–448. doi: 10.1016/j.biopsych.2008.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micco JA, Henin A, Mick E, Kim S, Hopkins CA, Biederman J, Hirshfeld-Becker DR. Anxiety and depressive disorders in offspring at high risk for anxiety: A meta-analysis. J Anxiety Disord. 2009;23(8):1158–1164. doi: 10.1016/j.janxdis.2009.07.021. [DOI] [PubMed] [Google Scholar]
- Muris P, Brakel AM, Arntz A, Schouten E. Behavioral inhibition as a risk factor for the development of childhood anxiety disorders: A longitudinal study. J Child Fam Stud. 2010;20(2):157–170. doi: 10.1007/s10826-010-9365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers CE, VanMeenen KM, Servatius RJ. Behavioral inhibition and PTSD symptoms in veterans. Psychiatry Res. 2012;196(2–3):271–276. doi: 10.1016/j.psychres.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus F, Backes A, Sander C, Weber M, von Gontard A. Anxiety disorders and behavioral inhibition in preschool children: A population-based study. Child Psychiatry Hum Dev. 2014;46(1):150–157. doi: 10.1007/s10578-014-0460-8. [DOI] [PubMed] [Google Scholar]
- Pfeifer M, Goldsmith HH, Davidson RJ, Rickman M. Continuity and change in inhibited and uninhibited children. Child Development. 2002;73(5):1474–1485. doi: 10.1111/1467-8624.00484. [DOI] [PubMed] [Google Scholar]
- Rapee RM. The preventative effects of a brief, early intervention for preschool-aged children at risk for internalising: follow-up into middle adolescence. J Child Psychol Psychiatry. 2013;54(7):780–788. doi: 10.1111/jcpp.12048. [DOI] [PubMed] [Google Scholar]
- Reznick JS, Hegeman IM, Kaufman ER, Woods SW, Jacobs M. Retrospective and concurrent self-report of behavioral inhibition and their relation to adult mental health. Dev Psychopathol. 1992;4(2):301–321. [Google Scholar]
- Robinson JL, Kagan J, Reznick JS, Corley R. The heritability of inhibited and uninhibited behavior: A twin study. Dev Psychol. 1992;28(6):1030–1037. [Google Scholar]
- Rosenbaum JF, Biederman J, Hirshfeld-Becker DR, Kagan J, Snidman N, Friedman D, Nineberg A, Gallery DJ, Faroe SV. A controlled study of behavioral inhibition in children of parents with panic disorder and depression. Am J Psychiatry. 2000;157(12):2002–2010. doi: 10.1176/appi.ajp.157.12.2002. [DOI] [PubMed] [Google Scholar]
- Rubin KH, Burgess KB, Hastings PD. Stability and social-behavioral consequences of toddlers’ inhibited temperament and parenting behaviors. Child Dev. 2002;73(2):483–495. doi: 10.1111/1467-8624.00419. [DOI] [PubMed] [Google Scholar]
- Saudino KJ, Micalizzi L. Emerging trends in behavioral genetic studies of child temperament. Child Dev Perspect. 2015;9(3):144–148. doi: 10.1111/cdep.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz C, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry. 1999;38:1008–1015. doi: 10.1097/00004583-199908000-00017. [DOI] [PubMed] [Google Scholar]
- White L, McDermott J, Degnan K, Henderson H, Fox NA. Behavioral inhibition and anxiety: The moderating roles of inhibitory control and attention shifting. J Abnorm Child Psychol. 2011;39(5):735–747. doi: 10.1007/s10802-011-9490-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancura LA, Aldwin CM. Stability and change in retrospective reports of childhood experiences over a 5-year period: findings from the Davis Longitudinal Study. Psychol Aging. 2009;24(3):715. doi: 10.1037/a0016203. [DOI] [PubMed] [Google Scholar]
- Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]


