Abstract
The mechanism by which aspirin consumption is linked to significant reductions in the incidence of multiple forms of cancer and metastatic spread to distant tissues, resulting in increased cancer patient survival is not well understood. In this study, using colon cancer as an example, we provide both in vitro (cell culture) and in vivo (chemically-induced mouse model of colon cancer) evidence that this profound anti-neoplastic action may be associated with aspirin’s ability to irreversibly inhibit COX-1 mediated platelet activation, thereby blocking platelet-cancer cell interactions, which promote cancer cell number and invasive potential. This process may be driven by platelet-induced Epithelial-Mesenchymal Transition (EMT), as assessed using confocal microscopy, based upon changes in cell morphology, growth characteristics and fibronectin expression, and biochemical/molecular analysis by measuring changes in the expression of the EMT markers; vimentin, β-catenin, and SNAIL. We also provide evidence that a novel, GI-safer phosphatidylcholine (PC)-associated aspirin, PL2200 Aspirin, possesses the same or more pronounced actions vs unmodified aspirin with regard to antiplatelet effects (in vitro-reducing platelet activation as determined by measuring the release of thromboxane and VEGF release in culture medium; in vivo-inhibiting platelet number/activation and extravasation into tumor tissue) and chemoprevention (in vitro-inhibiting colonic cell growth, and invasive activity; in vivo-inhibiting colonic dysplasia, inflammation and tumor mass). These results suggest that aspirin’s chemopreventive effects may be due, in part, to the drug blocking the pro-neoplastic action of platelets; and the potential use of Aspirin-PC/PL2200 as an effective and safer chemopreventive agent for colorectal cancer and possibly other cancers.
Keywords: aspirin, chemoprevention, platelet, colorectal cancer, COX-1
Introduction
Ever since its discovery in 1897, in addition to its activity to inhibit fever/pain/inflammation, aspirin when used chronically has been linked to a reduced incidence of a number of diseases including: thrombosis/heart disease, arthritis and cancer activity (1). Insight into the cardiovascular preventive action of aspirin came with Vanes’ discovery that aspirin and related NSAIDs act by inhibiting cyclooxygenase (COX) enzyme activity, that regulate the generation of eicosanoids, providing a mechanism for the class’ anti-inflammatory/antiplatelet activity (1). Indeed, aspirin’s unique ability to irreversibly inhibit platelet COX-1 (via acetylation), led to its wide-spread use in patients at risk of heart disease/thrombosis (2, 3).
Interestingly, there is a long history connecting blood coagulation disorders with late-stage cancer that dates back to the pioneering observation of Armand Trousseau who, in 1865, made the observation linking latter-stage cancer and venous-thrombosis (4–6). It is now well established that thrombocytosis and elevated circulating tissue factor levels are predictors of latter stage cancer along with increased incidence (4–8 fold) of venous thrombosis. A body of work demonstrates that platelets have the capability of interacting with circulating tumor cells (CTC) either directly or as a fibrin-associated network with neutrophils, and in so doing, prolonging the CTC circulatory half-life (7). Additionally, platelets have been reported to trigger Epithelial-Mesenchymal Transition (EMT) of cancer cells (8–10).
The association between low-dose (75–325 mg) aspirin consumption and a significant (20–40%) reduction in cancer incidence was shown for colorectal cancer (CRC) and the development of nine different non-GI cancers (11). It was also reported that aspirin use was significantly associated with a profound increase in patient survival, thereby reducing the risk of fatal adenocarcinoma (1, 11, 12). Of interest was the observation that the metastatic spread of cancer could also be reduced, even if aspirin consumption was initiated post-diagnosis (12, 13). Aspirin use has now been linked to a reduced cancer incidence in >20 cancers, including the major cancers afflicting our current population that are responsible for the preponderance of cancer-related hospitalizations/costs, morbidity and mortality activity (1, 12, 14–20).
Due to this compelling evidence, we designed studies using in vitro and in vivo models of colon cancer, to explore the fundamental question of whether aspirin’s anti-neoplastic activity is linked to its established ability to irreversibly inactivate platelets via COX-1 inhibition. The experiments focus on whether aspirin blocks platelets from promoting EMT, cancer cell growth, and the metastatic spread of cancer. In the current study, we also evaluated the chemopreventive activity of a novel phosphatidylcholine (PC)-associated aspirin, which has been formulated based upon its reported improved GI safety in both pre-clinical studies (21, 22), as well as a pilot clinical trial (23). There is an unmet need for a GI-safer aspirin, as the toxicity of aspirin to cause peptic ulceration and excessive GI bleeding in susceptible individuals has limited the recommendations of this commonly available drug to the public at-large as a chemopreventive agent. These issues are reflected by the September, 2015 recommendations of the US Preventive Services Task Force (USPSTF) where individuals aged 50–69yrs are advised to take low-dose aspirin on a daily basis to prevent CRC, under the physician consultation (24).
Materials and Methods
Ethics statement
Mice were maintained in accordance and compliance with policies approved by the Animal Welfare Committee (AWC), the Institutional Animal Care and Use Committee (IACUC) for The University of Texas Health Science Center at Houston (UTHealth). Samples of human blood for platelet isolation were obtained from normal subjects after obtaining informed consent under Institutional Review Board (IRB)-approved protocols at the Baylor College of Medicine and UTHealth.
Mouse strains
Young adult (20–24g) male BALB/c mice and young adult (22–24g) female Swiss Webster mice were supplied by Harlan Laboratories, Inc. (now Envigo) and housed in the Center for Laboratory Animal Medicine & Care (CLAMC) facility at UTHealth.
Cancer cells
Colon cancer cells (human Caco-2; HTB37™) were purchased from the American Type Culture Collection (ATCC®) and murine colon cancer cells (MC-26) were obtained from the NIH National Cancer Institute. The cell lines were cultured in suggested growth medium with 10% fetal bovine serum (Sigma-Aldrich). All the cell lines were regularly authenticated on the basis of viability, morphology and growth. Tests for mycoplasma were negative and were conducted with the MycoAlert Mycoplasma Detection Kit from Lonza (Rockland ME).
Chemicals and reagents
All chemicals, buffers, and cell culture media were purchased from Sigma-Aldrich, unless described separately. Matrigel Membrane Matrix (354234) was from Corning. Azoxymethane (AOM) and dextran sulfate sodium salt (DSS, 36,000–50,000 MW) were purchased from MP Biomedicals LLC.
Aspirin test drugs
For in vitro studies, pharmaceutical grade aspirin was purchased from Novacyl Inc. (Robbinsville, NJ) and was dissolved in RPMI 1640 culture media before undergoing sterile filtration. Aspirin-PC was prepared from aspirin and soy PC (S100 from Lipoid LLC). Initially, the PC was dissolved in chloroform and dried in a sterile glass vial under nitrogen gas. Then solubilized aspirin (in culture media) was added to the PC vial at a 1:1 ratio by weight and the vial was bath sonicated for 30 minutes. For in vivo studies, aspirin was purchased from a local pharmacy (Walgreens) and was prepared by crushing a tablet and suspending in water with sonication to a concentration of 2.5 mg/ml for intragastric administration. Aspirin-PC was prepared by mixing Novacyl aspirin with Lipoid Phosal 35SB cGMP which is the PC in the commercial formulation of Aspirin-PC. This mixture was suspended by bath sonication in water for animal studies.
Antibodies
A mouse monoclonal antibody of β-catenin (sc-7963), rabbit polyclonal antibody of vimentin (sc-5565), HRP conjugated goat anti-rabbit IgG (sc-2054), and HRP conjugated goat anti-mouse IgG (sc-2055) were from Santa Cruz Biotech. A rabbit polyclonal antibody of β-actin (PA1183) and Texas Red-X conjugated goat anti-mouse IgG (T6390) were from Thermo Scientific.
Human and mouse platelet isolation
Using a previously described technique to isolate platelets (25), human blood was drawn into an acid/citrate/dextrose (ACD) anticoagulant at a ratio of 1:9 (vol/vol) from healthy fasting donors. Platelet rich plasma (PRP) was prepared by centrifuging blood at 200×g for 15 minutes at room temperature. PRP supplemented with 75 nM of PGE1 was centrifuged at 1000×g for 10 minutes at room temperature to obtain a platelet pellet that was resuspended and washed with buffer and adjusted to 2.5×108 platelets/ml. Mouse blood (BALB/c) was collected from the inferior vena cava of random isoflorane-anesthetized mice into 3.8% sodium citrate at the ratio of 1:10 (vol/vol) for studies with PRP, and into ACD at the ratio of 1:10 (vol/vol) for washed platelet studies. Blood was diluted 1:1 with PBS and PRP was isolated following centrifugation at 68×g for 10 minutes. Washed platelets were obtained following additional centrifugation of PRP as we have described before (26). Platelets were resuspended in RPMI-1640 with 0.01 U/ml of apyrase and counts adjusted to 2.5×108 platelets/ml.
Cancer cell growth assay
At the time of drug testing, human and murine colon cancer cells were seeded onto the Transwell chamber (purchased from Corning, Corning, NY) with 0.4 µM porous membrane at 6.25×104 in 250 µl of serum free RPMI-1640 and washed platelets that were freshly collected from human or mouse were added in the bottom well at 5×107 in 500 µl of serum free RPMI-1640. Cells without platelet incubation served as a control. After 36 hours incubation, 3-(4,5-dimethylthiazolyl-2) 2,5-diphenyltetra-zolium bromide (MTT, Sigma-Aldrich) solution was added to the media of cells in the Transwell at a final concentration of 0.5 mg/ml for 4 hrs and the cells extracted and stained for MTT as previously described (27). The membrane was cut and extracted into plate wells containing 200 µl of the formazan solvent (90% isopropanol, 0.2% sodium dodecyl sulfate and 0.01N HCl) in a 48-well plate, and read at an absorbance of 570nm.
Cancer cell invasion assay
To assess invasive activity, 2.5×105 mouse MC-26 colon cancer cells (and 1×108 washed platelets were mixed in 500 µl of serum free RPMI 1640 and applied to the uppermost Transwell chamber with 8 µm porous membrane pre-coated with Matrigel (BD Biosciences), and 750 µl of serum free RPMI 1640 were added into the lower chamber in a 48-well culture plate. Cells without platelets served as control. After 16–20 hours of incubation at 37°C and 5% CO2, the non-invading cells and extracellular matrix were gently removed with a cotton swab and the number of invading cancer cells located on the lower side of the Transwell membrane was assessed by fixing and staining with Hema 3 stain kit (Fisher HealthCare Protocol), and counting under a microscope.
Co-culture of cancer cells and washed platelets
In studies to assess EMT activity, MC-26 cancer cells were co-cultured with mouse washed platelets (mWPs) at a ratio of 1:400 at 37°C, 5% CO2 for 18–24 hours. The 1: 400 was ratio was modeled after published studies, where a clear platelet effect on cancer cell growth and invasive activity was reported (28). The cultured cells were washed one time with PBS and then lysed with RIPA buffer (Fisher Scientific) for Western blot of vimentin. To assess β-catenin translocation into the nucleus, subcellular fractionation was performed according to the Abcam subcellular fractionation protocol. Briefly, the above co-cultured cells were collected in cold fractionation buffer, and cell membrane/cytosolic fraction and nucleus fraction were prepared by two rounds of differential centrifugation. The cell fraction samples were used for Western blot of β-catenin. For immunofluorescence staining, the MC-26 cells were co-cultured with mWPs at ratio of 1:400 on 18-mm coverslips with or without the test drugs in a 12-well plate for 18–24 hours.
Western blot analysis
Protein concentration of the cell extracts (whole cell lysates or subcellular fractions) was first determined by the BCA assay (Pierce), and then extracts were resolved by SDS-PAGE, transferred to PVDF membrane and analyzed by Western blot with the indicated antibodies.
mRNA analysis
RNA was extracted from the MC-26 cells supplemented with aspirin test drugs in the presence or absence of platelets, and reverse transcribed using Quantitect Reverse Transcription kit (Qiagen). RT-qPCR was then performed using QuantiFast SYBR Green PCR Kit (Qiagen) with primers specific for mouse snail (Snail forward 5’GGAAGCCCAACTATAGCGAGC3’ and Snail reverse 5’CAGTTGAAGATCTTCCGCGAC3’). Expression of GAPDH was used to normalize the data and the relative mRNA analysis was calculated using the comparative CT method.
AOM/DSS mouse model of colon cancer
Based upon a previously described technique alone (29), young (40–50 days old) female Swiss Webster mice were randomly assigned to treatment groups. Based on our previous experience, a minimum of five animals per group were needed to detect significant differences. They were administered a single i.p. injection of azoxymethane (AOM) at 7.5 mg/kg. One week after the AOM challenge, the mice were placed on drinking water containing dextran sulfate sodium (DSS) at 2%, 3%, or 4% for 7 days, and then provided normal diet and drinking water for the next 2 weeks. The DSS challenge was repeated two more times (in total 3-cycles of DSS) and the protocol took 10 weeks.
The test-drugs, aspirin and Aspirin-PC, at a daily aspirin dose (20 mg/kg) were administered intragastrically starting a week before the AOM challenge. The AOM control group was daily intragastrically administered the same volume of saline. The absolute control group did not receive AOM, DSS or test drugs. During the study, body weight was determined every week as a measure of general health and fecal samples were also collected weekly for hemoglobin analysis as a measure of gastrointestinal (GI) bleeding (potential side effect of aspirin). At the end of the 10-week study period, blood was collected, the mice were euthanized by overdose of isoflurane anesthesia followed by thoracotomy, and the colon measured in length and weighed and biopsies taken and snap frozen in liquid N2 for biochemical analysis or fixed and stained for aberrant crypt foci (ACF) counts and immunohistochemical (IHC) staining; hematocrit was assessed to detect blood loss due to GI bleeding. Whole blood from the four mice groups were used to isolate PRP, count platelets and TXB2 analysis. PRP was further challenged with 2.5 microgram/ml of collagen or left untreated (basal). The degree of platelet activation was assessed by flow cytometry using anti-P-selectin FITC and isotype control antibodies, as published (26).
Cytokine ELISA
Serum or cell culture medium was measured by using the TXB2 EIA kit (Cayman Chemical, Cat. #501020) or a mouse VEGF-A ELISA Kit (Pierce, Cat. #EMVEGFA) according to the manufacturer's specifications. Sera were collected from the blood samples of individual mice at the end of the experiment under terminal anesthesia following a protocol for cardiac puncture. Serum samples were separated from blood within 1 h following blood collection by centrifugation at 500g for 10 min, and then aliquotted and stored at −80 °C for subsequent testing. Cell culture media were collected at the end of the experiments and cleared by centrifugation at 17,000g for 10 min and then stored at −80 °C for subsequent testing.
Aberrant crypt foci (ACF)
ACF were identified in colonic tissue using a previously described technique (30) . The excised colonic tissue was opened and placed mucosal-side-up onto paper, fixed in 10% buffered formalin, and briefly stained with 0.3% methylene blue. A 40X magnifying lens was used for tissue examination. All measurements were performed by persons who were unaware of the treatment group.
Immunofluorescence
The cultured cells on coverslips were fixed in 4% formaldehyde, permeabilized by incubation in 0.5% Triton X-100, blocked with 10% goat serum, and then stained with polyclonal anti-fibronectin (Sigma-Aldrich) followed by Alexa-647 conjugated goat anti-rabbit antibody (Molecular Probes/Invitrogen). Afterwards, the samples were stained for f-actin, g-actin by Alexa Fluor® 488 phalloidin and the nuclei by DAPI (Molecular Probes/Invitrogen). To assess the presence of platelets in the colonic mucosa, sectioned colonic tissue mounted on the slides were stained with a rat anti-CD41 antibody, followed by a FITC conjugated goat anti-rat polyclonal antibody, and the nuclei by DAPI, based upon a previously described technique (31, 32).
Finally, samples were mounted on slides with elvanol (DuPont). Specimens were then visualized either by Deconvolution Microscopy employing an Olympus IX-70 microscope connected to a DeltaVision imaging system (Applied Precision, Issaquah WA), or Nikon A1R confocal laser microscope system and the NIS-Elements C software. The quantitation of immunofluorescence density was done using ImageJ software by measuring pixel units.
Statistics
Statistical analyses were performed using the statistics application StatView 5.01 (SAS Institute Inc., Cary, NC). Values are expressed as the mean ± standard error of the mean, and were evaluated by ANOVA followed by Fisher’s PLSD test. The association of colonic tumor mass with circulation platelet number was evaluated by Percentiles by correlation/covariance. A P value < 0.05 with 2-tailed testing was deemed statistically significant.
Results
Platelet-induced proliferation of colon cancer cells can be attenuated by aspirin test drugs
We initially assessed the growth stimulatory effect of platelets on mouse (MC-26 cells, Fig. 1A) and human (Caco-2, Fig. 1B) colon cancer cell lines. The ability of both mouse and human platelets to promote the proliferation of cancer cells within 48h was, in turn, dose-dependently reduced by aspirin and Aspirin-PC, with evidence that the Aspirin-PC may possess greater growth-inhibitory efficacy, within a dose-range of 0.1–1.0mM (Fig. 1A & B).
Figure 1. Platelet-induced proliferation and invasion of colon cancer cells can be attenuated by aspirin test drugs.
Mouse or human washed platelets (mWPs or hWPs) promote the growth of (A) mouse MC-26 or (B) human Caco2 and this effect is blocked by aspirin and Aspirin-PC. (C) Evidence that mouse washed platelets (mWPs) promoted the invasion of mouse MC-26 colon cancer cells, and this effect was blocked by both aspirin and Aspirin-PC. (D) Co-culture of platelets with colon cancer cells stimulated medium TXB2 and VEGF levels which were respectively inhibited by aspirin and Aspirin-PC. Values in each group were calculated from triplicates of 3 separate studies (n=9).
Platelets ability to promote the invasive potential of cancer cells can be blocked by aspirin test drugs
Using culture plates where the upper and lower chambers were separated by a porous membrane insert, we investigated the ability of platelets to promote translocation/invasion of the cancer cells to the lower chamber. The results in Fig.1C using MC-26 cells demonstrate that co-culture with mouse platelets promoted invasive activity, as we measured a ~20-fold increase in cell number across the membrane. Interestingly, this platelet-induced invasion was dose-dependently attenuated by addition of the aspirin test drugs to the medium at concentrations >0.3mM, with a tendency for Aspirin-PC to be more effective (Fig. 1C). Co-culture of cancer cells and platelets promoted the generation of the COX-1 product, TXB2, indicative of platelet activation, and both aspirin drugs significantly reduced TXB2 levels by >80% (Fig. 1D). We also screened the culture medium for alterations in the concentration of other growth mediators and determined that co-culture of platelets with MC-26 cells resulted in a significant increase in levels of VEGF in the medium, which was blocked by both aspirin and Aspirin-PC (Fig. 1D). In contrast, platelet-derived TGFβ1 was not increased when co-cultured with mouse or human cells, and its release was not affected by either of the aspirin test drugs (Supplementary Fig. S1).
Platelets promote EMT of cancer cells: attenuation with aspirin test drugs
As platelets have been reported to induce EMT in cancer cells, we performed in vitro experiments to assess whether aspirin interferes with the EMT process. We initially observed that, in addition to a marked increase in cell number, MC-26 cells underwent a profound morphological transformation within 48h after being co-cultured with platelets. Both a change in shape to a more mesenchymal cell type and the formation of fibronectin-associated microfilamentous structures that formed an extra-cellular network connecting adjacent cells were seen (Fig. 2A&B). These platelet-induced morphological changes were less evident when aspirin or Aspirin-PC was added to the culture medium (Fig. 2C). We also demonstrated that platelets promoted the translocation of β-catenin from the membrane/cytoplasm to the nucleus as shown by Western blot analysis of subcellular fractions (Fig. 3A), which was reduced when the aspirin test drugs were added to the culture medium, with Aspirin-PC being a more effective EMT inhibitor (Fig 3B). Furthermore, platelet co-culture induced an increase in vimentin expression of whole cell lysates (Fig. 3C), and similar to the effects on β-catenin, this platelet-induced pre-cancerous change was reduced if the cells were incubated with the aspirin test drugs with Aspirin-PC being consistently more effective (Figs. 3D). Lastly, platelets increased mRNA expression of snail (Snai1) in MC-26 cells, an EMT-inducing transcription factor, which was dose-dependently inhibited by both aspirin and Aspirin-PC (Supplementary Fig. S2).
Figure 2. Co-culture of MC-26 with mWPs results in Epithelial-Mesenchymal Transition (EMT).
De-convolution confocal microscopy of representative MC-26 cell growth pattern (f-actin in green) and expression of EMT marker (fibronectin in red) in the absence (A) and presence of mouse platelets (B). Fibronectin expression was quantified (C) by assessing fluorescent intensity/cell number which was increased in the presence of platelets and reduced by aspirin and Aspirin-PC (n=4/group).
Figure 3. The effect of aspirin and Aspirin-PC to reverse platelet-induced EMT changes.
(A&B) Mouse platelets (P) promote β-catenin translocation into nucleus of MC-26 cells is reduced by aspirin (ASA) and ASA-PC. (A) Western blot: Lanes 1–4 Membrane cytosol fraction; Lanes 5–8 Nucleus fraction; (B) Densitometry ratio of nucleus vs membrane/cytosol fractions. (C&D) Increased expression of Vimentin promoted by co-culture of MC-26 with mouse washed platelets was inhibited by aspirin and Aspirin-PC. (C) Western blot of vimentin of cell culture total lysates; (D) Histogram of densitometric analysis from 3 separate studies.
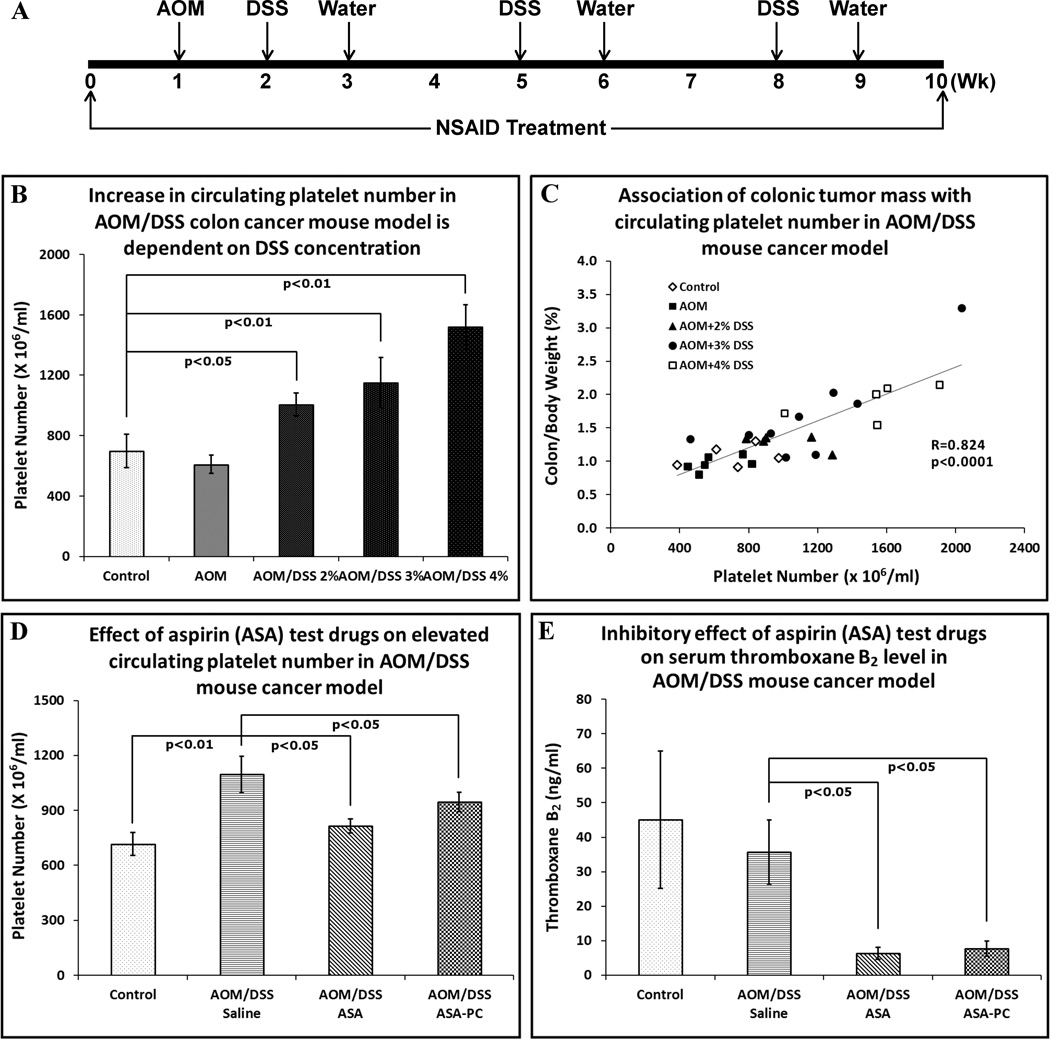
Anti-neoplastic efficacy of Aspirin-PC and aspirin in a murine colon cancer model
The in vivo model system chosen to study anti-neoplastic drug efficacy was an established mouse model of colon cancer, in which a chemical carcinogen that induces colonic dysplasia/neoplasia, azoxymethane (AOM), is used in combination with a chemical, dextran sodium sulfate (DSS), which induces colonic inflammation/colitis (schematically depicted in Fig. 4A). This combination induces the formation of aberrant colonic crypts which progresses to adenoma at an accelerated rate in comparison to AOM alone (29).
Figure 4. AOM/DSS mouse cancer model.
(A) Timeline (in weeks) of AOM/DSS model. (B) Demonstration that platelet number was dose-dependently increased with DSS concentration. (C) Mouse colon weight and body weight were recorded and the correlation between platelet number and ratio of colon weight to body weight was analyzed, as a reflection of colonic tumor mass. For (B) and (C): control (n=5), AOM (n=6), AOM/2% DSS (n=5), AOM/3% DSS (n=8), AOM/4% DSS (n=5). (D) Evidence that daily aspirin (ASA) treatment reduced platelet number in AOM/DSS challenged mice. (E) Detection of TXB2 in the mouse serum samples from AOM/DSS study, demonstrating the antiplatelet efficacy of both ASA and ASA-PC. For (D) and (E): control (n=6), AOM/DSS+Saline (n=5), AOM/DSS+aspirin (n=14), AOM/DSS+Aspirin-PC (n=11).
To optimize the DSS concentration, a study was performed to test cyclic use of 2%, 3% or 4% DSS in the drinking water after a single AOM injection. At the end of the study, it was found that the circulating platelet number was increased dose-dependently with 2–4% DSS, with significant differences observed in AOM/3% DSS and AOM/4% DSS groups compared to that of the mice in the saline control group (Fig. 4B). This is in contrast to the lack of effect of AOM, in the absence of DSS, on platelet number (Fig. 4B), emphasizing the importance of colonic inflammation as the driver of thrombocytosis. Most interestingly, the ratio of colon weight to body weight, which is a measure of colonic tumor mass was tightly associated (R= 0.82, p<0.001) with the number of circulating platelets (Fig. 4C).
Subsequently, we used 3% DSS post AOM to evaluate the chemopreventive activity of the aspirin test drugs. Mice were intragastrically administered aspirin or Aspirin-PC commencing 1-week prior to AOM injection, at a daily aspirin dose (20 mg/kg) that is comparable to low-dose aspirin (75–150mg/d) in man. As shown in Fig. 4D, the circulating platelet number increased in the AOM/DSS/saline group (p<0.01 vs controls), and the aspirin test drugs reversed the thrombocytosis induced by AOM/DSS treatment (p<0.05). We also determined that serum TXB2 levels were decreased 80–90% (p<0.01) in the two aspirin treatment groups (Fig. 4E), indicating the drugs’ ability to inhibit platelet COX-1 activity, as well as platelet number. Compared to platelets from the control mice, AOM/DSS/saline treatment appeared to increase basal platelet activation as observed by an increase in P-selectin staining. Importantly, platelets from the mice treated with aspirin and Aspirin-PC also failed to demonstrate collagen-induced platelet activation, as measured by P-selectin expression (Supplementary Fig. S3).
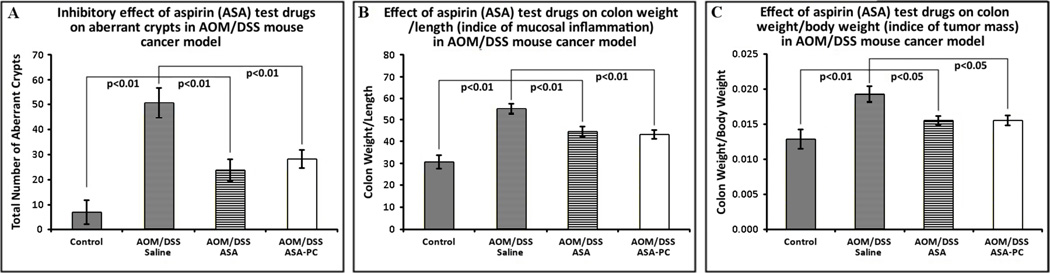
Mice treated with AOM/DSS appeared to gain less body weight than controls, with only the AOM/DSS/saline group being significantly lower than that of the control group at the study’s end, (Supplementary Figs. S4 & S5), suggesting that the animals’ developed systemic disease. The measurement of colonic aberrant crypts presented in Fig. 5A, demonstrates that AOM/DSS treatment increased this dysplastic change in the colonic mucosa (p<0.001), and both aspirin and Aspirin-PC treatments were effective (p<0.01) in reducing aberrant crypt number toward control values. Additionally it was found that the colon weight/length in the AOM/DSS groups was higher than that of the control group (p<0.01), which is reflective of mucosal edema/inflammation and that this ratio was lower in animals in both aspirin treatment groups (Fig. 5B, p<0.05). To assess colonic tumor mass, the ratio of colon weight to body weight was calculated, as shown in Fig. 5C. Consistent with the above observations, there was an increase in this measure of colonic tumor mass over control values in the AOM/DSS/saline group (p<0.01), which was reduced (p<0.05) by both aspirin test drugs.
Figure 5. The effect of aspirin and Aspirin-PC on mouse colon cancer model.
(A) Efficacy of aspirin and Aspirin-PC in significantly reducing the number of colonic aberrant crypts from the elevated values observed in mice treated with AOM/DSS. (B) Colon weight per length of animal in all groups, which is indicative of colonic inflammation induced by AOM/DSS, is reduced by both aspirin test drugs. (C) Ratio of colon weight to body weight, as an index of colonic tumor mass. The AOM/DSS/saline group values are significantly increased over the values of the control group. More importantly, the colon weight/body weight ratio is significantly reduced from elevated AOM/DSS values by treatment with aspirin and Aspirin-PC. Control (n=6), AOM/DSS+Saline (n=5), AOM/DSS+aspirin (n=14), AOM/DSS+Aspirin-PC (n=11).
Changes in fecal hemoglobin (Supplementary Fig. S6) reflect GI bleeding at the times of DSS administration, which was resolved by the end of the study period (week 10). Furthermore, at euthanasia, the hematocrit did not show any differences among groups (Supplementary Fig. S7), indicating the transient DSS-induced GI blood-loss was not lasting and there was no detectable GI bleeding from any of the drug treatments. This supports the GI safety of chronic dosing with the relatively low aspirin dose of 20 mg/kg dose of aspirin and Aspirin-PC in mice.
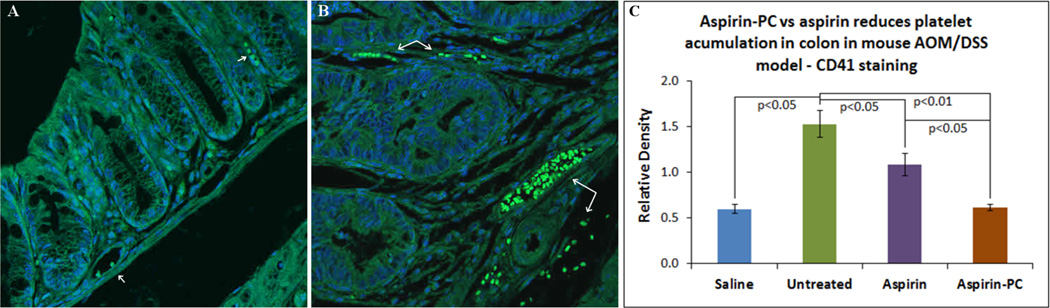
Using an immunofluorescent chemical (IFC) stain for CD41 platelet surface integrin, we assessed whether platelets seed into colonic tissue undergoing dysplasia/neoplasia, and if so, whether this pattern was affected by treatment with aspirin or Aspirin-PC. Representative IFC results shown in Fig. 6A&B, provides evidence that platelets are generally present at a low density and restricted to the large vessels present in the submucosa of control colonic mucosal tissue, whereas their number is noticeably increased within the major blood vessels of the dysplastic/hypertrophic colonic mucosa of AOM/DSS-challenged mice with evidence of translocation across the endothelium and traffic to adjacent submucosal/sub-epithelial tissues. This morphological pattern was less evident in the aspirin and Aspirin-PC treated mice, where infiltration of the platelets into the submucosa of the colonic mucosa was rarely observed, which was quantitatively supported by a reduction in fluorescent intensity of colonic tissue, with Aspirin-PC tissues having a substantial inhibitory effect, similar to values seen in normal (non-cancerous) tissue (Fig. 6C).
Figure 6. Localization of platelets in mouse cancer model.
FITC-labelling of antibodies directed against mouse CD41 surface antigen in representative colonic tissue of: (A) control mice; and (B) mice challenged with AOM/DSS to induce colonic dysplasia/ adenoma. Arrows indicate localizations of platelet-specific immunoreactivity within blood vessels and surrounding submucosal and mucosal tissue. Both micrographs were taken using a 20X objective. (C) Quantification of platelet immunoreactivity in colonic tissue of AOM/DSS-treated mice, was performed using ImageJ software by measuring pixel units, showing reductions with aspirin and Aspirin-PC treatments. Slides per group: (saline) control=2; AOM/DSS/saline (untreated)=8; AOM/DSS/(aspirin)=7; AOM/DSS/(Aspirin-PC)=4.
Discussion
The mechanism by which aspirin use is linked to a reduction in cancer incidence and metastases has yet to be fully elucidated. Since aspirin consumption has been associated with a reduced incidence of numerous cancers, it suggests that one way the drug may act is at a stage which is common for most tissues undergoing dysplasia (1, 11, 12). As tissue inflammation is tightly linked to many chronic disease states including cancer, and aspirin has clear anti-inflammatory actions, this drug action may be an important component in its chemopreventive activity (1, 33). Indeed, a number of laboratories (34, 35) reported that CRC tissue over-expresses COX-2, suggesting it may be the primary target enzyme by which NSAIDs and notably COX-2 selective inhibitors (coxibs) reduce cancer incidence and recurrence. Although this indeed is an attractive theory, it has a number of limitations. These include evidence that coxibs have chemopreventive activity that may be limited to Familial Adenomatous Polyposis patients. In comparison, there is more compelling evidence for aspirin protection in more common CRC, such as in Lynch Syndrome (hereditary non-polyposis) patients (36, 37). Also, not all cancers overexpress this COX isoform, and Rothwell reported that cancers affecting the proximal colon, which generally do not overexpress COX-2, are more responsive to aspirin use than those of the distal colon (38). Lastly, for aspirin to target COX-2 in most cancers and affect the metastatic spread of tumor cells would require that aspirin remain stable in circulation. However, pharmacokinetic data demonstrates that aspirin rapidly hydrolyzes to salicylic acid within 10–20 minutes after it enters the blood (39), and salicylic acid has a much lower (100–1000 fold) COX-2 inhibitory activity vs aspirin, especially in tissues undergoing inflammation (40).
Because of these aforementioned reasons, we felt an alternative mechanistic basis of aspirin’s anti-neoplastic action needed to be explored. Indeed, as indicated earlier, platelets are a primary target of aspirin and are involved in thrombosis of late-stage cancer patients. Platelets are known to promote EMT of cells in the early stage of dysplasia thereby playing a role in cancer cell invasiveness, attachment and growth, processes that are thought to be mediated in part by the release of mediators, notably platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF) and TGFβ (8–10). Thus, as speculated by a number of investigators (33, 41), the platelet is a likely target of aspirin, especially since the irreversible inhibition of platelet COX-1 via acetylation, will inactivate the platelet for its circulatory half-life (7–10d in humans and 5–7d in mice), until a new generation of platelets enters the circulation via megakaryopoiesis.
Based upon this background, we performed in vitro and in vivo studies to directly evaluate the role of aspirin’s antiplatelet activity in its ability to inhibit colon cancer growth and invasive potential. We also evaluated the chemopreventive activity of a novel phospholipid-associated aspirin, which was the result of our laboratory studies that showed surface-active lipids, such as phosphatidycholine (PC) play an intrinsic role in protecting the GI mucosa from surface-injury, as may be caused by NSAIDs (42) (43). Subsequently a family of PC-NSAIDs was developed that possesses reduced GI toxicity, primarily by attenuating the surface injurious action of NSAIDs, while maintaining the therapeutic activity of the drugs (44). These observations were the impetus for the commercial development of PL2200 Aspirin (PLx Pharma Inc, Houston TX) which combines aspirin with a PC-enriched soy lecithin. We have previously reported that PL2200 Aspirin induces significantly fewer gastroduodenal endoscopic ulcers than normal aspirin in a 7-day trial of healthy subjects, aged >55 years, who are most susceptible to the GI side-effects of NSAIDs (23). PL2200 Aspirin also appears to have profound antiplatelet activity in both healthy and diabetic subjects, supporting its potential use for both cardiovascular disease and possibly cancer. Results described above demonstrate that platelets promote the growth and invasive potential of both mouse (MC-26) and human (Caco-2) colon cancer cells, and that these actions can be dose-dependently blocked by both aspirin and Aspirin-PC. Similar to Hynes and colleagues studies(10), we confirmed that platelets promote EMT in colon cancer cells, and that these robust platelet-dependent cellular/biochemical changes can also be blocked by our aspirin test drugs.
We performed in vivo studies in mice with an established model of colon cancer that uses a regimen of AOM and DSS (29). It should be noted that we used this particular model, as it simulates the colonic inflammation and adenoma formation that occurs clinically in colorectal cancer, and has been demonstrated to be responsive to NSAIDs and other chemopreventive agents, whereas another CRC model, APC (Min/+) mice demonstrated little or no response to aspirin – possibly because the polypoid lesions occur primarily in the small intestine (45). Accordingly, using the AOM/DSS model we demonstrated that daily treatment of mice with 20 mg/kg of aspirin or the equivalent dose of Aspirin-PC, significantly reduced both the formation of aberrant crypts in the colon, which is a sign of dysplasia as well as colonic tumor mass in comparison to saline-treated controls. Interestingly the AOM/DSS challenged animals also had elevated platelet counts, which were reduced in the aspirin-treated groups, with little difference in the anti-cancer action observed between Aspirin-PC and the unmodified NSAID. This result thereby differs from our in vitro results where Aspirin-PC consistently possessed more pronounced potency/efficacy to inhibit cancer cell growth and invasive activity. Future experiments will be designed to provide an explanation for these results. Using the mouse colon cancer model system, we demonstrated that platelets migrated into the inflamed colonic mucosa and adjacent tumor tissue, appeared to be associated with the vasculature as well as surrounding areas of mucosal inflammation/dysplasia and this response was reduced in mice treated with aspirin and Aspirin-PC. These observations are consistent with studies by Granger’s lab (46) that reported increased platelet reactivity in colonic mucosa undergoing DSS-induced inflammation, and a recent study by Qi et al (31) that reported the presence of platelets in both intestinal tumors from APC Min mice and from clinical biopsies of patients with CRC, and a study from Miyashita et al (32) of platelet extravasation into the invasive front of pancreatic ductal adenocarcinomas. We extended these very interesting observations, to demonstrate that the ability of platelets to seed into areas of colonic dysplasia/neoplasia. Using a similar approach, Guillem-Llobat et al (47) recently reported that platelet-induced biochemical changes associated with EMT of human HT-29 colon carcinoma cells was blocked by COX-1 inhibitors including aspirin.
It is very important to emphasize that the findings presented above that aspirin’s chemopreventive activity is attributable to the NSAID’s ability to irreversibly inhibit platelet COX-1 and their subsequent activation, has limitations, being generally correlative in nature, and future experiments are planned to study aspirin sensitivity in animals where we experimentally manipulate platelet number and COX expression (e.g transgenic mice where platelet COX-1 is disrupted. Also, it has been reported that aspirin and related NSAIDs can inhibit cancer cell growth and/or promote apoptotic activity of cancer cells by COX-independent pathways, that involve activation of the tumor suppressor AMP kinase (AMPK), or inhibition of the transcription factors, NFκB and AP-1 or directly affecting mitochondrial function (48, 49).
In summary our findings suggest that aspirin’s anti-neoplastic actions can be explained, in part, by the drug’s ability to rapidly inhibit the number/activity of circulating platelets via irreversible COX-1 inhibition. Thus our results support the use of low-dose aspirin for chemoprevention, that is sufficient to block platelet-cancer cell interactions, which play a fundamental role in cancer formation and progression, while having limited anti-inflammatory activity. These findings address the initial actions of aspirin on cancer development and do not dismiss COX-2 and its downstream pro-inflammatory eicosanoid products as being important in certain cancers, which remains an attractive target in explaining the chemopreventive action of coxibs/NSAIDs when used at anti-inflammatory doses. Lastly, we present evidence that a novel lipid-based aspirin, Aspirin-PC/PL2200 Aspirin, possesses similar chemopreventive actions to low-dose aspirin and may be more effective. Future experiments are planned to determine the efficacy and safety of PL2200 Aspirin in subjects that are at high risk for the development of colorectal cancer.
Supplementary Material
Acknowledgments
KVV is a research member of the Dan L. Duncan Comprehensive Cancer Center at Baylor College of Medicine. This material is the result of work supported in part with resources and the use of facilities of the Michael E. DeBakey VA Medical Center.
Financial support: This work was supported by NIH grants R41 CA171408 awarded to PLx Pharma Inc and L. Lichtenberger and R21 CA182798 awarded to L. Lichtenberger and K. Vijayan.
Footnotes
Disclosure of Potential Conflicts of Interest: L. Lichtenberger is a co-founder and shareholder in PLx Pharma Inc which is developing PC-NSAIDs for commercial use.
References
- 1.Cuzick J, Thorat MA, Bosetti C, Brown PH, Burn J, Cook NR, et al. Estimates of benefits and harms of prophylactic use of aspirin in the general population. Ann Oncol. 2015;26:47–57. doi: 10.1093/annonc/mdu225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vane J. Towards a better aspirin. Nature. 1994;367:215–216. doi: 10.1038/367215a0. [DOI] [PubMed] [Google Scholar]
- 3.Vane JR. Nobel lecture. Adventures and excursions in bioassay--the stepping stones to prostacyclin. Postgrad Med J. 1983;59:743–758. doi: 10.1136/pgmj.59.698.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nash GF, Turner LF, Scully MF, Kakkar AK. Platelets and cancer. Lancet Oncol. 2002;3:425–430. doi: 10.1016/s1470-2045(02)00789-1. [DOI] [PubMed] [Google Scholar]
- 5.Levin J, Conley CL. Thrombocytosis Associated with Malignant Disease. Arch Intern Med. 1964;114:497–500. doi: 10.1001/archinte.1964.03860100079008. [DOI] [PubMed] [Google Scholar]
- 6.Varki A. Trousseau's syndrome: multiple definitions and multiple mechanisms. Blood. 2007;110:1723–1729. doi: 10.1182/blood-2006-10-053736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitrugno A, Tormoen GW, Kuhn P, McCarty OJ. The prothrombotic activity of cancer cells in the circulation. Blood Rev. 2016;30:11–19. doi: 10.1016/j.blre.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salgado R, Benoy I, Bogers J, Weytjens R, Vermeulen P, Dirix L, et al. Platelets and vascular endothelial growth factor (VEGF): a morphological and functional study. Angiogenesis. 2001;4:37–43. doi: 10.1023/a:1016611230747. [DOI] [PubMed] [Google Scholar]
- 9.Kirwan CC, Byrne GJ, Kumar S, McDowell G. Platelet release of Vascular Endothelial Growth Factor (VEGF) in patients undergoing chemotherapy for breast cancer. J Angiogenes Res. 2009;1:7. doi: 10.1186/2040-2384-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Labelle M, Begum S, Hynes RO. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell. 2011;20:576–590. doi: 10.1016/j.ccr.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377:31–41. doi: 10.1016/S0140-6736(10)62110-1. [DOI] [PubMed] [Google Scholar]
- 12.Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet. 2012;379:1591–1601. doi: 10.1016/S0140-6736(12)60209-8. [DOI] [PubMed] [Google Scholar]
- 13.Chan AT, Ogino S, Fuchs CS. Aspirin use and survival after diagnosis of colorectal cancer. JAMA. 2009;302:649–658. doi: 10.1001/jama.2009.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trabert B, Ness RB, Lo-Ciganic WH, Murphy MA, Goode EL, Poole EM, et al. Aspirin, nonaspirin nonsteroidal anti-inflammatory drug, and acetaminophen use and risk of invasive epithelial ovarian cancer: a pooled analysis in the Ovarian Cancer Association Consortium. J Natl Cancer Inst. 2014;106:djt431. doi: 10.1093/jnci/djt431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sahasrabuddhe VV, Gunja MZ, Graubard BI, Trabert B, Schwartz LM, Park Y, et al. Nonsteroidal anti-inflammatory drug use, chronic liver disease, and hepatocellular carcinoma. J Natl Cancer Inst. 2012;104:1808–1814. doi: 10.1093/jnci/djs452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Dyke AL, Cote ML, Prysak G, Claeys GB, Wenzlaff AS, Schwartz AG. Regular adult aspirin use decreases the risk of non-small cell lung cancer among women. Cancer Epidemiol Biomarkers Prev. 2008;17:148–157. doi: 10.1158/1055-9965.EPI-07-0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fraser DM, Sullivan FM, Thompson AM, McCowan C. Aspirin use and survival after the diagnosis of breast cancer: a population-based cohort study. Br J Cancer. 2014;111:623–627. doi: 10.1038/bjc.2014.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sclabas GM, Uwagawa T, Schmidt C, Hess KR, Evans DB, Abbruzzese JL, et al. Nuclear factor kappa B activation is a potential target for preventing pancreatic carcinoma by aspirin. Cancer. 2005;103:2485–2490. doi: 10.1002/cncr.21075. [DOI] [PubMed] [Google Scholar]
- 19.Choe KS, Cowan JE, Chan JM, Carroll PR, D'Amico AV, Liauw SL. Aspirin use and the risk of prostate cancer mortality in men treated with prostatectomy or radiotherapy. J Clin Oncol. 2012;30:3540–3544. doi: 10.1200/JCO.2011.41.0308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gamba CA, Swetter SM, Stefanick ML, Kubo J, Desai M, Spaunhurst KM, et al. Aspirin is associated with lower melanoma risk among postmenopausal Caucasian women: the Women's Health Initiative. Cancer. 2013;119:1562–1569. doi: 10.1002/cncr.27817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lichtenberger LM, Romero JJ, de Ruijter WM, Behbod F, Darling R, Ashraf AQ, et al. Phosphatidylcholine association increases the anti-inflammatory and analgesic activity of ibuprofen in acute and chronic rodent models of joint inflammation: relationship to alterations in bioavailability and cyclooxygenase-inhibitory potency. J Pharmacol Exp Ther. 2001;298:279–287. [PubMed] [Google Scholar]
- 22.Lichtenberger LM, Romero JJ, Dial EJ. Surface phospholipids in gastric injury and protection when a selective cyclooxygenase-2 inhibitor (Coxib) is used in combination with aspirin. Br J Pharmacol. 2007;150:913–919. doi: 10.1038/sj.bjp.0707176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cryer B, Bhatt DL, Lanza FL, Dong JF, Lichtenberger LM, Marathi UK. Low-dose aspirin-induced ulceration is attenuated by aspirin-phosphatidylcholine: a randomized clinical trial. Am J Gastroenterol. 2011;106:272–277. doi: 10.1038/ajg.2010.436. [DOI] [PubMed] [Google Scholar]
- 24.Bibbins-Domingo K Force USPST. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164:836–845. doi: 10.7326/M16-0577. [DOI] [PubMed] [Google Scholar]
- 25.Bynagari YS, Nagy B, Jr, Tuluc F, Bhavaraju K, Kim S, Vijayan KV, et al. Mechanism of activation and functional role of protein kinase Ceta in human platelets. J Biol Chem. 2009;284:13413–13421. doi: 10.1074/jbc.M808970200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khatlani T, Pradhan S, Da Q, Gushiken FC, Bergeron AL, Langlois KW, et al. The beta isoform of the catalytic subunit of protein phosphatase 2B restrains platelet function by suppressing outside-in alphaII b beta3 integrin signaling. J Thromb Haemost. 2014;12:2089–2101. doi: 10.1111/jth.12761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dial EJ, Doyen JR, Lichtenberger LM. Phosphatidylcholine-associated nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit DNA synthesis and the growth of colon cancer cells in vitro. Cancer Chemother Pharmacol. 2006;57:295–300. doi: 10.1007/s00280-005-0048-x. [DOI] [PubMed] [Google Scholar]
- 28.Cho MS, Bottsford-Miller J, Vasquez HG, Stone R, Zand B, Kroll MH, et al. Platelets increase the proliferation of ovarian cancer cells. Blood. 2012;120:4869–4872. doi: 10.1182/blood-2012-06-438598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clapper ML, Cooper HS, Chang WC. Dextran sulfate sodium-induced colitis-associated neoplasia: a promising model for the development of chemopreventive interventions. Acta Pharmacol Sin. 2007;28:1450–1459. doi: 10.1111/j.1745-7254.2007.00695.x. [DOI] [PubMed] [Google Scholar]
- 30.Wargovich MJ, Jimenez A, McKee K, Steele VE, Velasco M, Woods J, et al. Efficacy of potential chemopreventive agents on rat colon aberrant crypt formation and progression. Carcinogenesis. 2000;21:1149–1155. [PubMed] [Google Scholar]
- 31.Qi C, Li B, Guo S, Wei B, Shao C, Li J, et al. P-Selectin-Mediated Adhesion between Platelets and Tumor Cells Promotes Intestinal Tumorigenesis in Apc(Min/+) Mice. Int J Biol Sci. 2015;11:679–687. doi: 10.7150/ijbs.11589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miyashita T, Tajima H, Makino I, Nakagawara H, Kitagawa H, Fushida S, et al. Metastasis-promoting role of extravasated platelet activation in tumor. J Surg Res. 2015;193:289–294. doi: 10.1016/j.jss.2014.07.037. [DOI] [PubMed] [Google Scholar]
- 33.Thun MJ, Jacobs EJ, Patrono C. The role of aspirin in cancer prevention. Nat Rev Clin Oncol. 2012;9:259–267. doi: 10.1038/nrclinonc.2011.199. [DOI] [PubMed] [Google Scholar]
- 34.Cha YI, DuBois RN. NSAIDs and cancer prevention: targets downstream of COX-2. Annu Rev Med. 2007;58:239–252. doi: 10.1146/annurev.med.57.121304.131253. [DOI] [PubMed] [Google Scholar]
- 35.Roelofs HM, Te Morsche RH, van Heumen BW, Nagengast FM, Peters WH. Over-expression of COX-2 mRNA in colorectal cancer. BMC Gastroenterol. 2014;14:1. doi: 10.1186/1471-230X-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steinbach G, Lynch PM, Phillips RK, Wallace MH, Hawk E, Gordon GB, et al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med. 2000;342:1946–1952. doi: 10.1056/NEJM200006293422603. [DOI] [PubMed] [Google Scholar]
- 37.Movahedi M, Bishop DT, Macrae F, Mecklin JP, Moeslein G, Olschwang S, et al. Obesity, Aspirin, and Risk of Colorectal Cancer in Carriers of Hereditary Colorectal Cancer: A Prospective Investigation in the CAPP2 Study. J Clin Oncol. 2015;33:3591–3597. doi: 10.1200/JCO.2014.58.9952. [DOI] [PubMed] [Google Scholar]
- 38.Birkenkamp-Demtroder K, Olesen SH, Sorensen FB, Laurberg S, Laiho P, Aaltonen LA, et al. Differential gene expression in colon cancer of the caecum versus the sigmoid and rectosigmoid. Gut. 2005;54:374–384. doi: 10.1136/gut.2003.036848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Voelker M, Hammer M. Dissolution and pharmacokinetics of a novel micronized aspirin formulation. Inflammopharmacology. 2012;20:225–231. doi: 10.1007/s10787-011-0099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mitchell JA, Akarasereenont P, Thiemermann C, Flower RJ, Vane JR. Selectivity of nonsteroidal antiinflammatory drugs as inhibitors of constitutive and inducible cyclooxygenase. Proc Natl Acad Sci U S A. 1993;90:11693–11697. doi: 10.1073/pnas.90.24.11693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruno A, Dovizio M, Tacconelli S, Patrignani P. Mechanisms of the antitumoural effects of aspirin in the gastrointestinal tract. Best Pract Res Clin Gastroenterol. 2012;26:e1–e13. doi: 10.1016/j.bpg.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 42.Lichtenberger LM. The hydrophobic barrier properties of gastrointestinal mucus. Annu Rev Physiol. 1995;57:565–583. doi: 10.1146/annurev.ph.57.030195.003025. [DOI] [PubMed] [Google Scholar]
- 43.Lichtenberger LM, Wang ZM, Romero JJ, Ulloa C, Perez JC, Giraud MN, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) associate with zwitterionic phospholipids: insight into the mechanism and reversal of NSAID-induced gastrointestinal injury. Nat Med. 1995;1:154–158. doi: 10.1038/nm0295-154. [DOI] [PubMed] [Google Scholar]
- 44.Lichtenberger LM, Barron M, Marathi U. Association of phosphatidylcholine and NSAIDs as a novel strategy to reduce gastrointestinal toxicity. Drugs Today (Barc) 2009;45:877–890. doi: 10.1358/dot.2009.45.12.1441075. [DOI] [PubMed] [Google Scholar]
- 45.Corpet DE, Pierre F. How good are rodent models of carcinogenesis in predicting efficacy in humans? A systematic review and meta-analysis of colon chemoprevention in rats, mice and men. Eur J Cancer. 2005;41:1911–1922. doi: 10.1016/j.ejca.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 46.Mori M, Salter JW, Vowinkel T, Krieglstein CF, Stokes KY, Granger DN. Molecular determinants of the prothrombogenic phenotype assumed by inflamed colonic venules. Am J Physiol Gastrointest Liver Physiol. 2005;288:G920–G926. doi: 10.1152/ajpgi.00371.2004. [DOI] [PubMed] [Google Scholar]
- 47.Guillem-Llobat P, Dovizio M, Bruno A, Ricciotti E, Cufino V, Sacco A, et al. Aspirin prevents colorectal cancer metastasis in mice by splitting the crosstalk between platelets and tumor cells. Oncotarget. 2016;7:32462–32477. doi: 10.18632/oncotarget.8655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alfonso L, Ai G, Spitale RC, Bhat GJ. Molecular targets of aspirin and cancer prevention. Br J Cancer. 2014;111:61–67. doi: 10.1038/bjc.2014.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Usman MW, Luo F, Cheng H, Zhao JJ, Liu P. Chemopreventive effects of aspirin at a glance. Biochim Biophys Acta. 2015;1855:254–263. doi: 10.1016/j.bbcan.2015.03.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.