Abstract
Introduction:
The exact etiology of lower urinary tract symptoms caused by benign prostatic hyperplasia (BPH) has not yet been determined, and the etiology of erectile dysfunction (ED) is often multicausal and includes organic and/or psychogenic causes, as well as their combinations. Although the relation of BPH, and thus the volume of the prostate (VP) with ED is indisputable, precise mechanisms of integration are still under examination.
Goal:
The objective was to evaluate the correlation between prostate volume and degree of erectile dysfunction in patients with symptoms of lower urinary tract caused by benign prostatic hyperplasia. Material and Methods. 150 subjects with BPH, and before starting the BPH treatment, which can affect the sexual function, were divided into three groups: 50 patients with prostate volume of 30 to 40 ml (group A), 50 patients with a volume of 40 to 60 ml (group B) and 50 patients with prostate volume above 60 ml (group C). Quantification of erectile function is performed in all respondents by International Index of Erectile Function with five questions (IIEF-5).
Results:
The mean IIEF-5 in group A was 20.52 points with a standard deviation of 3.22, in group B 17.08 points with a standard deviation of 4.10, while in group C 10.78 points, with a standard deviation of 3.29. Comparing the results of a statistical analysis from all three groups of patients with the degree of ED, Group A had the highest value of IIEF-5, group C the lowest mean value of IIEF-5. The results of ANOVA (F=96.375, p=0.000) indicated that there was a statistically significant difference (p<0.05) between groups at high values of IIEF-5. Additional analysis by Turkey test revealed that there was a statistically significant difference between the first and second groups (p=0.000 <0.05), the first and third groups (p=0.000 <0.05) and the second and third groups (p=0.000 <0.05). Results of Fisher’s exact test (p=0.000) confirmed that there was a statistically significant relationship (p<0.05) between prostate volume and the degree of erectile function. Results of Spearman correlation (ρ=-0.720; p=0.000) showed that prostate volume is negatively correlated with IIEF-5 score with a reliability of 99% (p<0.05), or that increase in the volume of the prostate reduces the IIEF score.
Conclusion:
Results of IIEF-5 score are inversely proportional to the volume of the prostate or the prostate volume increase, the more severe erectile dysfunction, because the increase in prostate volume leads to a decline in IIEF score.
Keywords: symptoms of the lower urinary tract, benign prostatic hyperplasia, prostate volume, erectile dysfunction
1. INTRODUCTION
Benign prostatic hyperplasia (BPH) is defined as benign, noncancerous enlargement of the prostate caused by the growth of new stromal and epithelial cells. One of the most common disease that affects older men aged over 50 years and which leads to the symptoms of the lower urinary tract (LUTS- lower urinary tract symptoms) (1). The prevalence of BPH increases with age of patients after the age of forty and one in four men have symptomatic BPH, while in the sixties, four out of ten men are faced with this problem, suggesting the progressive nature of the disease (2).
Parameters affecting the higher risk of disease progression are higher International Prostate Symptom Score (IPSS), prostate specific antigen (PSA) and prostate volume (VP), reduced urine flow, and older age. According to many authors, the incidence of BPH has not been established because of the lack of BPH epidemiological definition (2, 3).
Erectile dysfunction (ED) is defined as the persistent inability to attain and maintain an erection sufficient to provide a satisfactory sexual intercourse (4). Although considered “benign” disease, ED can dramatically affect the quality of life of many men and their partners (5, 6).
The incidence of BPH and ED in older men increases with age (7).
According to the Massachusetts Male Aging Study (MMAS) data, the incidence of ED is 26 newly discovered in 1,000 men annually, and ED was present in all age groups, although there is evident correlation with age (8). The prevalence of ED in data standardized International Index of Erectile Function-5 (IIEF-5) between the ages of 20-50 years amounted to 26-29%. Over 50 years, this percentage was slightly higher, at 37.5%, while in the age of 71-80 years the percentage distribution was 71.2% (9). The true prevalence is often masked by the refusal of men to talk about their sexual problems (10).
The etiology of ED is often multicausal and includes organic and psychogenic causes, as well as their combination, while the etiology of BPH is not exactly determined (11).
Data from epidemiological studies suggest a link between the symptoms of BPH and ED in older men, regardless of the impact of age, co-morbidity or differences in lifestyle (12). Possible connection between these two diseases lies in the mechanism of action of α-1 adrenergic receptor. It is assumed that patients via these receptors increases the tone of the smooth muscle cells of the prostatic capsule and bladder neck. Penile erection depends on a balanced contraction and relaxation of the cavernous smooth muscle. In the ED, through the aforementioned receptors through noradrenaline and androgens, favoring the contraction of smooth muscle, which complicates the process of relaxation of the same, which would lead to erectile dysfunction (13).
Although the link of BPH, and thus the volume of the prostate with ED is indisputable, precise mechanisms of integration are still the subject of many research (14).
2. GOAL
The objective was to evaluate the correlation between prostate volume and degree of erectile dysfunction in patients with symptoms of lower urinary tract caused by benign prostatic hyperplasia.
3. MATERIAL AND METHODS
The study was conducted as a prospective study which included males aged 40-60 years of age with present symptoms of lower urinary tract caused by benign prostatic hyperplasia. The survey included respondents who were first contacted the doctor for symptoms of BPH, or newly discovered patients with BPH, where is considered initially, prior to introduction of treatments that may affect sexual function or dysfunction. The clinical sample was collected during the six-month period. The survey was conducted in the Cantonal Hospital “Dr. Irfan Ljubijankić” Bihac.
The study included 150 patients with symptoms of BPH. All patients, as part of the diagnostic process, also underwent ultrasonic measurement of prostate volume. In determining the volume by ultrasonography, we determined the three diameters of the prostate: transverse, anteroposterior and cranio-caudal. Prostate volume was determined by multiplying the three diameters and dividing the product by 2.5. This volume is calculated with the best correlation with the severity of tissue of benign prostatic hyperplasia, or weight corresponding to the calculated volume, the fact that the specific weight of the prostatica tissue to 1.05 gr/cm³.
According to the obtained value of prostate volume subjects were divided into three groups (groups A, B and C): patients with prostate volume of 30 to 40 ml (group A), patients with a volume of 40 to 60 ml (group B) and the third group patients with prostate volume over 60 ml (group C).
After that, all the respondents were evaluated by International Index of Erectile Function-IIEF-5. IIEF-5 questionnaire related to ED, is composed of five questions. The first question relates to the safety of achieving and maintaining erections. The second question assesses erection itself–sufficient for the sexual act. The third and fourth questions relate to the success of maintaining erections after immission of sexual organs and to the completion of sexual activity. The answer to the fifth question describes the pleasure of sexual intercourse. The maximum score is 25 points. Score 1-7 points indicates severe erectile dysfunction, 8-11 points a moderate ED, 12-16 points mild to moderate ED, 17-21 points mild ED, and 22-25 points normal erectile function.
4. RESULTS
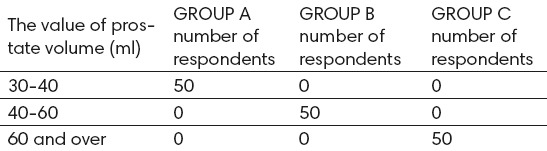
According to the values of prostate volume respondents were divided into three groups (Table 1).
Table 1.
Respondents according to the prostate volume
The average age of the subjects in Group A (patients with prostate volume 30 to 40 ml) was 51.06 years, with a standard deviation of 6.80. The oldest patient was 60 years old and the youngest 40 years old. In group B (patients with a prostate volume of 40-60 ml), the average age of the patients was 52.52 years with a standard deviation of 6.18. The oldest patient was 60 years old, and the youngest is 40 years of age. The average age of patients in group C (patients with prostate volume over 60 ml) was 55.96 years, with a standard deviation of 4.81. The youngest patient was 42 years old, and the oldest 60 years (Table 2).
Table 2.
The average age of respondents
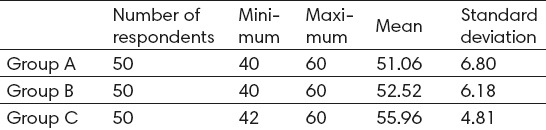
Based on the results of Levin’s test of homogeneity of variance (F=4.464; p=0.013), it was concluded that the variance of the first, second and third groups are not equal (p<0.05). The results of ANOVA (F=8.822; p=0.000) showed that there was a statistically significant difference (p<0.05) between groups in the average age of the patients. Additional analysis by Tamhane test showed that there was present statistically significant difference in average age between the first and third groups (p=0.000 <0.05), and between the second and third groups (p=0.008 <0.05). A statistically significant difference (p=0.601> 0.05) in the average age was not present between the first and second group.
The average value of IIEF-5 in group A was 20.52 points with a standard deviation of 3.22. Minimum value of the score in group A was 8 points, and the maximum 25 points. In group B, the average was 17.08 points with a standard deviation of 4.10. Minimum and maximum value score in group B was 7 or 25 points. The average value of the IIEF-5 in the group C was 10.78 points, with standard deviation of 3.29, while the minimum value or the maximum score was 5 and 19 points respectively (Table 3).
Table 3.
The average value of IIEF-5
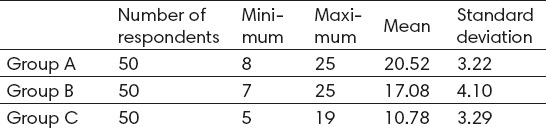
Comparing the results of a statistical analysis of all three groups of patients with the degree of ED, we see that Group A had the highest value of IIEF-5, a group C the lowest mean value of the same. The results of ANOVA (F=96.375, p=0.000) showed that there was a statistically significant difference (p<0.05) between groups with higher values of IIEF-5. Additional analysis by Turkey test revealed that there was a statistically significant difference between the first and second groups (p=0.000 <0.05), the first and third groups (p=0.000 <0.05) and the second and third groups (p=0.000 <0.05). When we performed additional analysis, it was assumed that the variance of the first, second and third groups were the same as confirmed by Levin’s test (p=0.357 >0.05).
Results of Fisher’s exact test (p=0.000) confirmed that there was a statistically significant relationship (p<0.05) between prostate volume and degree of erectile function (Table 4).
Table 4.
Correlation of prostate volume with the degree of erectile dysfunction in patients from all three groups
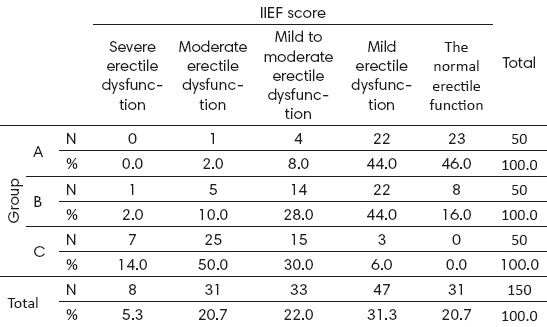
Based on the results of Spearman correlation (ρ=-0.720; p=0.000), it was concluded that the volume of the prostate is negatively correlated with IIEF-5 score with the reliability of 99% (p<0.05), and that the increase in the volume of the prostate leads to a decline in IIEF score. Therefore, it can be said that, as prostate volume increased, the erectile dysfunction is more severe.
5. DISCUSSION
The exact etiology of BPH has not yet been determined. In fact, some patients with significant enlargement of the prostate does not express the symptoms of LUTS, whereas others have symptoms of lower urinary tract, which significantly affect the quality of life and do not have a significant enlargement of the prostate (15). However, LUTS caused by benign prostatic hyperplasia include substantially larger volume of the prostate. Connection of BPH with erectile dysfunction is quite complex, but according to the data of many studies indisputable. Multinational Survey of the Aging Male (MSAM-7) study, which is based on the results of testing 12,815 men in the US and six European countries, aged 50-80 years, found a significant association of BPH with ED (49% of respondents) and even 10% of the total lack of erection (16). BPH and ED are also associated with comorbidities such as cardiovascular disease, diabetes, obesity and dyslipidemia (17). Although, proper causal relationship has not been established, it is believed that 70% of men with BPH has an associated ED (18). Men with severe BPH have significantly decreased libido, greater difficulty in achieving an erection, and lower level of sexual satisfaction as compared to men with milder form of BPH (19).
Data of some studies indicate a lower prevalence of self-reported ED in patients with BPH compared to the prevalence of ED based on the IIEF questionnaire. This discrepancy can be contributed to socioeconomic factors, level of education, socio-cultural factors. Wu and colleagues therefore suggest that the prevalence of ED should not be based on self-reporting by patients, because they significantly underestimate the actual prevalence of the disease (20). Therefore, the present recommendations, patients with LUTS symptoms caused by benign prostatic hyperplasia should be evaluated and the presence of ED using the IIEF questionnaire, all the more, as some studies even prove that the severity of BPH better predictor of ED, but as the age of the patient (21).
This strongly implies the need to take sexuality into consideration in the initial evaluation of patients with BPH, and adequate therapeutic choice for the same. Given the potential impact of the same on sexual function, it is essential to evaluate the presence of ED patients before starting treatment of BPH (22).
In general, a lot of research has been performed on the correlation of BPH symptoms with the degree of ED, and the same has shown that severity of LUTS significantly correlated with IIEF-5 questionnaire, but very few studies determined the correlation between prostate volume with erectile function (23).
The results of our study showed that the average score of erectile function by IIEF-5 was 20.52 points with SD 3.22 in subjects with BPH and prostate volume of 30-40 ml, which meant normal erectile function. Respondents with prostate volume of 40 to 60 ml had an average score of erectile function according to IIEF-5 of 17.08 points with SD 4.10, which was a mild to moderate ED. The subjects of the third group, with prostate volume over 60 ml had an average value of EF 10.78 points with SD 3.29, and these patients most often had moderate to severe ED. Based on the results of Spearman correlation (ρ=-0.720; p=0.000), prostate volume was negatively correlated with IIEF-5 score with the reliability of 99% (p<0.05), and an increase in prostate volume leads to a decline in IIEF score.
Understanding the causal link between LUTS/BPH, and thus the volume of the prostate with ED is very important, because the treatment of one illness can significantly affect the other and vice versa (24, 25).
6. CONCLUSION
The age of the patients was correlated with the volume of the prostate, and elderly patients had a higher prostate volume. Results of IIEF score of -5 were inversely proportional to the volume of the prostate or as the prostate volume increased, the erectile dysfunction was more severe, because the increase in prostate volume led to a decline in IIEF score.
Footnotes
• Authors contribution: Amel Kardasevic contributed in all phases of preparing this article (concept, design, data collection, research, drafting etc.). Snjezana Milicevic contributed to concept and design of the study, including final editing and critical revision of the scientific content.
• Conflict of interest: none declared.
REFERENCES
- 1.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU BPH Guidelines. Eur Urol. 2004;46:547–54. doi: 10.1016/j.eururo.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Bosch JL. Natural history of benign prostatic hyperplasia: appropriate case definition and estimation of its prevalence in the community. Urology. 1995;46:34–40. doi: 10.1016/s0090-4295(99)80248-9. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JB, Roehrborn CG, Schalken JA, Emberton M. The Progression of Benign Prostatic Hyperplasia: Examining the Evidence and Determining the Risk. Eur Urol. 2001;39:390–9. doi: 10.1159/000052475. [DOI] [PubMed] [Google Scholar]
- 4.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocialcorrelates: results of the Massachusetts Male Aging Study. J Urol. 1994 Jan;151(1):54–61. doi: 10.1016/s0022-5347(17)34871-1. http://www.ncbi.nlm.nih.gov/pubmed/8254833. [DOI] [PubMed] [Google Scholar]
- 5.Lue TF, Giuliano F, Montorsi F, Rosen RC, Andersson KE, Althof S, et al. Summary of the recommendations on sexual dysfunctions in men. J Sex Med. 2004;1:6–23. doi: 10.1111/j.1743-6109.2004.10104.x. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch M, Donatucci C, Glina S, Montauge D, Montorosi F, Wyllie M. Standards for clinical trials in male sexual dysfunction: erectile dysfunction and rapid ejaculation. J Sex Med. 2004;1:87–91. doi: 10.1111/j.1743-6109.2004.10113.x. [DOI] [PubMed] [Google Scholar]
- 7.Song J, Shao Q, Tian Y, Na YQ, Chen S, Wang Y, et al. Association between lower urinary tract symptoms and erectile dysfunction in males aged 50 years and above: results from a multicenter community-based cross-sectional survey (BPC-BPH) Zhonghua Yi Xue Za Zhi. 2011 Oct 18;91(38):2706–9. [PubMed] [Google Scholar]
- 8.Johannes CB, Araujo AB, Feldman HA, Derby CA, Kleinman KP, McKinlay JB. Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts Male Aging Study. J Urol. 2000 Feb;163(2):460–3. http://www.ncbi.nlm.nih.gov/pubmed/10647654. [PubMed] [Google Scholar]
- 9.Ponholzer A, Temml C, Mock K, Marszalek M, Obermayr R, Madersbacher S. Prevalence and Risk Factors for Erectile Dysfunction in 2869 Men Using a Validatet Questionnaire. Eur Urol. 2005;47:80–6. doi: 10.1016/j.eururo.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Culley C Carson, John D Dean. Management of Erectile Dysfunction in Clinical Practice. 1th ed. London: Springer-Verlag; 2007. [Google Scholar]
- 11.Lee JC, Benard F, Carrier S, Talwar V, Defoy I. Do men with mild erectile dysfunction have the same risk factors as the general erectile dysfunction clinical trial population? BJU Int. 2011 Mar;107(6):956–60. doi: 10.1111/j.1464-410X.2010.09691.x. http://www.ncbi.nlm.nih.gov/pubmed/20950304 . [DOI] [PubMed] [Google Scholar]
- 12.Seftel AD, de la Rosette J, Birt J, Porter V, Zarotsky V, Viktrup L. Coexisting lower urinary tract symptoms and erectile dysfunction: a systematic review of epidemiological data. Int J Clin Pract. 2013 Jan;67(1):32–45. doi: 10.1111/ijcp.12044. http://www.ncbi.nlm.nih.gov/pubmed/23082930 . [DOI] [PubMed] [Google Scholar]
- 13.O'Leary MP, Luts ED. QoL: alphabet soup or real concerns to aging man? Urology. 2000;56(Suppl 5A):7–11. doi: 10.1016/s0090-4295(00)00742-1. [DOI] [PubMed] [Google Scholar]
- 14.McVary KT. Erectile dysfunction and lower urinary tracts symptoms secondary to BPH. Eur Urol. 2005;47:838–45. doi: 10.1016/j.eururo.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Auffenberg GB, Helfand BT, McVary KT. Established medical therapy for benign prostatic hyperplasia. Urol Clin North Am. 2009;36:443–59. doi: 10.1016/j.ucl.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 16.Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003 Dec;44(6):637–49. doi: 10.1016/j.eururo.2003.08.015. http://www.ncbi.nlm.nih.gov/pubmed/14644114. [DOI] [PubMed] [Google Scholar]
- 17.Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population based survey of urinary incontinence, overactive baldder and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol.2006; 50:1306–14. doi: 10.1016/j.eururo.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 18.Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, et al. EAU Guidelines on treatment and follow up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64:118–40. doi: 10.1016/j.eururo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Kirby M, Chapple C, Jackson G, Eardley I, Edwards D, Hackett G, et al. Erectile dysfunction and LUTS: a consensus on the importance of co-diagnosis. Int J Clin Pract. 2013;67:606–18. doi: 10.1111/ijcp.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu CJ, Hsieh JT, Lin JS, Hwang TI, Jiann BP, Huang ST, et al. Comparison of Prevalence between self-reported erectile dysfunction and erectile dysfunction as defined by five-item International Index of Erectile Function in Taiwanese men older than 40 years. Urology. 2007;69:743–7. doi: 10.1016/j.urology.2006.12.019. [DOI] [PubMed] [Google Scholar]
- 21.Berry SJ, Coffey DS, Walsh PC, Ewing SJ. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474–9. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 22.Ozayar A, Zumrutbas AE, Yaman O. The relationship between lower urinary tract symptoms (LUTS), diagnostic indicators of benign prostatic hyperplasia(BPH) and erectile dysfunction in patients with moderate to severly symptomatic BPH. Int Urol Nephrol. 2008;40:933–9. doi: 10.1007/s11255-008-9386-z. [DOI] [PubMed] [Google Scholar]
- 23.Braun M, Wassmer G, Klotz T, Reinfenrath B, Matheis M, Engelman U. Epydemiological study of ED: results of the Cologne Male Survey. Int J Impot Res. 2000;6:305–11. doi: 10.1038/sj.ijir.3900622. [DOI] [PubMed] [Google Scholar]
- 24.McVary Kevin T. Erectile dysfunction and Lower Urinary Tract Symptoms Secondary to BPH. Eur Urol. 2005;47(6):838–45. doi: 10.1016/j.eururo.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Junuzovic D, Hasanbegovic M, Masic I. Risk Factors for Erectile Dysfunction in Patients with Newly Diagnozed Diabetes Mellitus. Med Arch. 2010;64(6):345–7. doi: 10.5455/medarh.2010.64.345-347. [DOI] [PubMed] [Google Scholar]


