Abstract
The primary aim of the Million Hearts initiative is to prevent 1 million cardiovascular events over 5 years. Concordant with the Million Hearts’ focus on achieving more than 70% performance in the “ABCS” of aspirin for those at risk, blood pressure control, cholesterol management, and smoking cessation, we outline the cardiovascular events that would be prevented and a road map to achieve more than 70% participation in cardiac rehabilitation (CR)/secondary prevention programs by the year 2022. Cardiac rehabilitation is a class Ia recommendation of the American Heart Association and the American College of Cardiology after myocardial infarction or coronary revascularization, promotes the ABCS along with lifestyle counseling and exercise, and is associated with decreased total mortality, cardiac mortality, and rehospitalizations. However, current participation rates for CR in the United States generally range from only 20% to 30%. This road map focuses on interventions, such as electronic medical record–based prompts and staffing liaisons that increase referrals of appropriate patients to CR, increase enrollment of appropriate individuals into CR, and increase adherence to longer-term CR. We also calculate that increasing CR participation from 20% to 70% would save 25,000 lives and prevent 180,000 hospitalizations annually in the United States.
Million Hearts is a national initiative co-led by the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services launched in 2012 and renewed in 2017 that brings together health care professionals and systems, federal and private sector organizations, communities, and individuals to prevent 1 million cardiovascular events over 5 years.1,2 Million Hearts is designed to drive the implementation of evidence-based interventions across communities and health care settings. A major component is focused on achieving at least 70% performance in the “ABCS”—aspirin for those at risk, blood pressure control, cholesterol management, and smoking cessation.3 In recognition of the impact that cardiac rehabilitation (CR) has on outcomes for those who have cardiovascular disease, Million Hearts convened representatives from over 30 organizations and agencies as well as CR graduates and family members in November 2015 to address the barriers to and facilitators of participation. Represented organizations included the American Association of Cardiovascular and Pulmonary Rehabilitation, American Heart Association (AHA), American College of Cardiology (ACC), American Association of Nurse Practitioners, American College of Physicians, American Hospital Association, Heart Failure Society of America, Preventive Cardiovascular Nurses Association, Blue Cross Blue Shield Association, and others. Summit participants formed the Million Hearts Cardiac Rehabilitation Collaborative, developed a 2016 action plan, and have set an aim to boost participation in CR from 20% to 70% by 2022 through individual and collective action. Representing the Cardiac Rehabilitation Collaborative, we describe the potential benefits of CR and provide a road map to attain a similar rate of participation in CR of at least 70%. Although others have previously outlined the importance of CR and described several broad strategies to improve referrals,4 no prior work has systematically compiled and applied strategies to target the combination of increasing referrals to CR and, as or more importantly, increasing program enrollment and adherence. This effort is supported by a concurrent initiative at the Centers for Medicare and Medicaid Services designed to encourage the use of CR services for Medicare beneficiaries after a myocardial infarction (MI) or coronary artery bypass surgery.5
Participation in CR is a class Ia recommendation of the AHA/ACC for individuals with an acute MI or coronary revascularization.6 Additionally, for patients with stable chronic systolic heart failure, exercise training is a class I recommendation, whereas CR is a class IIa recommendation.7 Despite these high levels of recommendation of CR by the AHA and ACC, participation in CR remains low, and effective strategies to increase referral and enrollment are needed. In that adherence with CR is related to the magnitude of the clinical benefit, we also address strategies to sustain participation in CR.8
BACKGROUND
Benefits of CR participation are broad and compelling and include a 13% to 24% reduction in total mortality over 1 to 3 years, a 31% decrease in rehospitalizations over 1 year, and an increase in physical function and quality of life.9–13 Much of the clinical benefit of CR has been ascribed to increases in fitness from a structured exercise program14,15 and the associated favorable physiologic effects on coronary endothelial function, insulin resistance, blood pressure, inflammatory markers, and fibrinolytic state.15–17 However, CR programs have also evolved to become disease management and secondary prevention centers that assist with medication adherence to the ABCS and the management of behavioral weight loss, smoking cessation, hypertension, diabetes, depression, and mental stress.13,17,18 In this way, CR programs and the peer networks therein help patients develop essential skills in healthy living as well as medication management.
Despite the fact that CR services are covered by Medicare and by private payers and are cost-effective,19 CR participation rates are very low, ranging from 19% to 34% in national analyses20,21 with strong state-by-state geographic variations and differences by cardiac diagnosis.20 States also vary in the availability of center-based CR programs.20 The highest participation rates are in the Midwestern states, with lowest participation rates in the South.20 Participation rates are higher after coronary bypass surgery than after MI.20,22 Whether CR disproportionately benefits patients with one cardiac diagnosis vs another is unclear, although a survival benefit of CR has been documented for patients after MI, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG), systolic heart failure, and heart transplant, whereas no such benefit has yet been reported after heart valve replacement.23–25 High-performing CR programs and entire states have attained CR participation rates in the range of 60% for eligible patients.20,22,26 Therefore, it is challenging, but not unreasonable, to target 70% utilization as a national goal concordant with the Million Hearts ABCS 70% targets for risk factor management.
POTENTIAL IMPACT
What would be the impact of increasing CR participation from 20% to 70% in terms of cardiovascular events prevented as a component of Million Hearts? We performed this calculation with a simple model using published literature. We first summed the annual number of CR-qualifying events: acute MI (735,000), CABG surgery (395,000), PCI (454,000), and new cases of systolic heart failure discharged from the hospital (504,000).27–30 We then obtained contemporary 1-year mortality rates and rehospitalization rates by these indications from the medical literature.31–33 To estimate the number of unduplicated individuals, correcting for overlap, we divided the totals by 1.94 based on rates of CABG, PCI, or congestive heart failure at or within 1 year of referral to CR in a cohort study.34 We derived the associated benefits of CR based on a systematic review of randomized trials, which found that CR reduced all-cause mortality by 13% and subsequent all-cause hospitalizations by 31%.9 Thus, an initial calculation reveals that in the first year after CR, 12,000 lives could be saved and 87,000 hospitalizations averted. Furthermore, an observational study of 70,040 matched pairs of Medicare beneficiaries found that the benefits of CR extended throughout the 5-year study.35 The 5-year mortality reductions were 2.08 times those observed in the first year after CR (ie, about 18 months after the index hospitalization). Assuming that a comparable factor applies to hospitalizations, an estimated 25,000 lives could be saved and 180,000 hospitalizations prevented annually over the long term by increasing CR participation from 20% to 70%. These rough estimates do not include other important benefits of CR, such as fewer emergency department visits,34 increased exercise tolerance, reduced symptoms, and improved quality of life.13
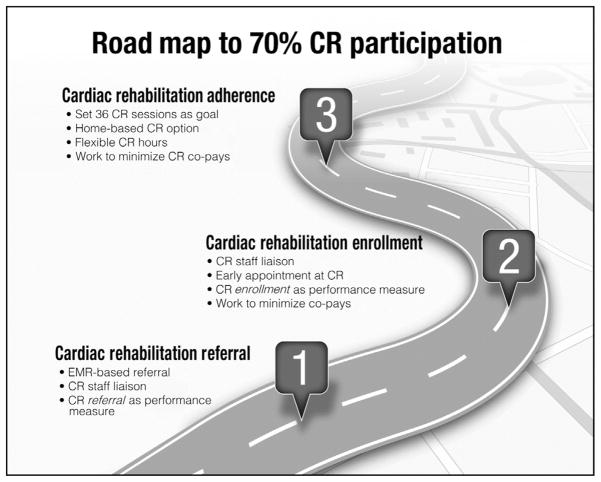
To increase CR participation so substantially, from the current rate of 20% to 30% to the goal rate of 70%, improvements in 2 critical steps are necessary. First, the systematic referral of eligible patients to a CR program needs to be increased, and second, the successful enrollment of referred patients into a CR program needs to be optimized. Cardiac rehabilitation referral is defined by the combination of an order in the medical record, a discussion between a clinician and patient regarding CR participation, and receipt of the order by a CR program. Enrollment in CR is defined by participation in at least one CR session (Medicare and most commercial insurers cover up to 36 sessions). Although improvements in these 2 areas are needed for all patient groups, they are particularly important in subgroups of the population in which CR participation rates are the lowest, including older patients, women, individuals with multiple comorbidities, people from underserved racial/ethnic groups, and those of lower socioeconomic status.34–36 Because the benefits of CR are dose related,8,34,35 CR adherence is also important and is addressed subsequently.
It is important to note that there would not be an instant ability of CR programs to increase capacity to accommodate both an enrollment rate of 70% and improved patient adherence. Given current CR capacity in the United States, expanding capabilities to accommodate a large increase in participation and adherence would need to be gradual and require both improvement in program operations and broadening of the current facility-based model. This process should include the use of a hybrid model with on-site coordination of home programs and mobile monitoring technologies.37 Furthermore, the methods of increasing CR referral and participation may vary based on the local environment, with each program and hospital having unique patient populations and barriers to improving the quality of and access to care. Nonetheless, widespread adoption of a few specific strategies to improve referral and enrollment, along with programmatic adaptations to efficiently and effectively deliver care to more patients, will have a profound impact on morbidity and mortality in those at high risk for future events.
IMPROVING CR REFERRAL
Cardiac rehabilitation referral rates can be almost tripled by using the systematic approach to referral developed by Grace et al,38 which includes an automatic electronic medical record–based CR referral system. This “default” or “opt-out” order for patients with qualifying diagnoses results in efficient, systematic referral to outpatient CR during the hospital discharge process. Additionally, a staff member or “liaison” meets with each patient to introduce CR and help coordinate the referral process38 (Table 1).4,38–43 In the study by Grace et al,38 an automatic referral combined with a liaison attained referral rates of 86% compared with 32% in controls who received neither intervention. Automatic referral alone increased the referral rate to 70%. If all hospitals in the United States were able to adopt such a combined strategy, CR referral rates in the United States could be almost tripled from the current level of approximately 20% to 30%, to an estimated level of 54% to 81% (Figure).
TABLE 1.
Strategies That Influence Referral and Enrollment to Cardiac Rehabilitation
| Strategy | Brief description | Outcome | Reference |
|---|---|---|---|
| Automatic in-patient CR referral system | CR referral is carried out as an automatic EMR order for all eligible patients | CR referral was 70% (compared with 32% for usual care); enrollment was 61% (compared with 29% for usual care) | 38 |
| Inpatient “liaison” to help educate and refer patients to out-patient CR | A liaison or “coach” meets with inpatients who are eligible for CR, educating and guiding them in the CR enrollment process | CR referral was 59% (compared with 32% for usual care); enrollment was 51% (compared with 29% for usual care) | 38 |
| Combination of automatic CR referral system and “liaison” | Combination of the 2 strategies listed above | CR referral was 85% (compared with 32% for usual care); enrollment was 74% (compared with 29% for usual care) | 38 |
| Limit or eliminate out-of-pocket expenses to patients for CR services | Negotiate with insurance companies to limit or eliminate co-payments and other out-of-pocket expenses for patients enrolled in CR | Studies of preventive medication adherence suggest that reducing or eliminating co-payments improves utilization and adherence | 39,40 |
| Inclusion of home-based CR option for patients who are not able to attend a center-based CR program | Protocol-driven, nurse-managed home- based approaches to CR delivery provide CR services to patients at home for low- to moderate-risk patients | Outcomes are similar and participation rates may be higher in home-based CR programs compared with center-based CR programs | 41 |
| Flexible hours of operation | Increased flexibility of CR center hours to include early morning, noontime, after work, and weekend hours | 10% Improvement in enrollment and participation; will require creative staff scheduling to avoid increasing costs of program delivery | 4 |
| Early outpatient appointment established before hospital discharge | Inpatient staff members work and EMR set up an outpatient CR enrollment appointment for each eligible patient within 12 days of hospital discharge | 20%–25% Improvement in CR enrollment | 42 |
| Use of CR referral performance measures in a quality improvement system | CR referral is assessed, reported, and acted upon in a systematic quality improvement program | CR referral rates improved by 12.5% over 5 years in centers participating in a quality improvement program | 43 |
CR = cardiac rehabilitation; EMR = electronic medical record.
FIGURE.
Conceptual framework for increasing cardiac rehabilitation (CR) participation from 20% to 70%. EMR = electronic medical record.
The use of CR referral as a “quality of care indicator” also appears to be a promising tool to improve CR referral.44 Performance measures for CR referral have been developed, endorsed, and implemented to promote improvements in CR referral. One study by Beatty et al43 using the ACC’s National Cardiovascular Data Registry documented a significant 8% absolute improvement in CR referral rate to over 80% in hospitals participating in the quality improvement activities.
IMPROVING CR ENROLLMENT
The transition from CR referral to CR enrollment is a crucial step in the overall CR participation process. Systematic approaches to CR enrollment substantially increase CR participation rates (Table 1). First, the systematic CR referral strategy of Grace et al38 was also associated with a higher overall CR enrollment rate, 74% in centers that used a computerized automatic referral system with liaisons to help patients navigate the enrollment process vs 29% in centers using “usual care” procedures.38 This increase exceeds the 70% national goal outlined previously. Other approaches and their estimated impact on CR enrollment rates include (1) inclusion of a home-based CR option for patients (estimated 20% relative improvement),41 (2) flexible hours of operation for CR centers (estimated 10% relative improvement),4 and (3) scheduling the first CR appointment before patient discharge from the hospital at 10 to 12 days after hospital discharge (18% improvement in enrollment over standard care, from 59% to 77% participation).42 Whether these effects are additive or overlapping is unknown. It is also important to note that for every 1-day delay in starting CR, there is an approximate 1% less likelihood of the patient enrolling.42,45 Although use of a performance measure for CR enrollment has not yet been implemented or tested, it likely represents an additional promising tool in helping to improve CR enrollment for eligible patients.
Participation rates also depend somewhat on cardiac diagnosis because patients who have undergone surgical revascularization have higher participation rates than patients who have MI or undergo percutaneous revascularization.20,22 Cardiac rehabilitation participation rates for individuals with chronic systolic heart failure have yet to be determined, although given that many of these patients are of advanced age and present with multiple comorbidities, the present enrollment rates are most likely lower than for patients in other diagnostic categories.
INCREASING ADHERENCE TO CR
Another challenge and opportunity for CR programs is ensuring that all patients receive the largest “dose” possible of program participation. Specifically, several studies suggest that the magnitude of clinical benefit derived from participation in CR is related to the number of sessions completed by patients.8,34,35 Cardiac rehabilitation participants face a variety of barriers in attending and completing the program. Among these barriers are the need to return to work, the cost burden, inconvenient hours, transportation issues, and cultural barriers. Cardiac rehabilitation programs can substantially boost adherence and help patients receive an ideal dose of CR by incorporating specific strategies that optimize adherence.
Table 241,46–55 summarizes adherence strategies that have been studied to maximize adherence, such as an expectation that patients complete all 36 sessions of the CR protocol and small motivational rewards or incentives for completing blocks of sessions.46,47 Contemporary CR programs are encouraged to incrementally adopt and apply many of these strategies, eventually incorporating them as routine elements of daily operations. Other strategies to consider include record keeping by participants (eg, diaries, logs, step counts), matching program hours of operation to patient rather than to staff needs, and offering program content that is culturally and linguistically appropriate and considerate of age, sex, comorbidities, and coexisting disabilities. Although not all patients have co-payments for CR sessions, insurers can reduce or eliminate these co-payments or cost share to encourage more and longer participation, which leads to better outcomes for users.39,40
TABLE 2.
Strategies That Influence Adherence in Patients Enrolled in Cardiac Rehabilitation
| Strategy/factor | Brief description | Outcome | Reference |
|---|---|---|---|
| Incorporate motivational and financial incentives. Introductory video | Rewards (shirts with program logo or similar items) based on session attendance. Video to describe CR program and impact on health outcomes. Video shown before hospital discharge or at beginning of outpatient CR | Improved program completion rates | 46,47 |
| Change program procedures to recommend 36 visits for all patients | Provide 36 visits using a 2-visit vs 3-visit per week schedule | Observed increase in number of attended visits per patient | 46–48 |
| Modify program structure to accommodate more total patients and more patients per day. Align frequency of visits to clinical status and patient preferences | Incorporate group orientations; develop hybrid model of home-based and facility-based program that includes key components of CR; shift from class structure to open-gym model; minimize (de-emphasize) frequency/use of ECG telemetry monitoring | Improved cost efficiency of delivery | 41,49,50 |
| Gender-tailored delivery of CR | Women-only CR = traditional CR + structured behavioral learning strategies on decision balance, self- efficacy, and processes of change | Attendance to women-only classes was 90%, compared with 77% in women undergoing traditional CR only | 51 |
| Text messaging | Use TM for appointment reminders and to augment classroom education; participation in TM should be voluntary; limit to 3–5 texts per week | Program completion rates were higher with SMS messaging; number of sessions attended was 20% greater with use of TM | 52 |
| Establish philanthropic fund to partly underwrite CR costs for patients with high co-payments or without insurance | Annual appeal letter to CR “graduates” (and past fund contributors) asking for contributions; emphasize the purpose to help others with limited resources | Return rates (with contributions) to direct mail solicitation as high as 7% | 53 |
| Altering program structure and design | Programs in the Wisconsin CR registry were surveyed and analyzed for factors that improve adherence | Factors that influenced adherence included adequate space and equipment, medical director on site >15 min/wk, assessment of patient satisfaction, individual/group diet counseling, relaxation training, group education, and group psychological counseling | 54 |
| Use of motivational letter | Intervention letter based on theory of planned behavior; targeted attitude toward best recovery, assistance with control and choices, and importance of following recommendations | Attendance rates for the intervention group were substantially higher than those for the control group | 55 |
CR = cardiac rehabilitation; ECG = electrocardiographic; SMS = short message service; TM = text messaging.
INSTITUTING SYSTEM-BASED APPROACHES
The widespread use of system-based approaches for both CR referral and enrollment would improve CR participation rates substantially. If all hospitals adopted the systematic CR referral approach with liaisons, CR referral rates could approach 90%.38 If all hospitals and CR programs adopted the CR enrollment strategies outlined previously, then overall enrollment rates could exceed 70%, assuming the geographic availability of a CR program. Even if only half of US hospitals and CR programs adopted such strategies, CR referral and enrollment rates would still improve substantially, approaching rates of 60% and 50%, respectively.
Cardiac rehabilitation is a class Ia AHA/ACC recommendation for patients after an acute MI or coronary revascularization,6 and exercise training is similarly a class I indication for individuals with chronic systolic heart failure.7 Yet, unlike medications taken for secondary prevention (eg, statins, aspirin) and despite its proven benefits, CR participation among those eligible and known to benefit is presently in the range of only 20% to 30%. Indeed, many consider exercise “like a pill that should be taken daily.”56,57 Achieving a 70% enrollment rate in CR, concordant with targets set for the Million Hearts ABCS, is possible through individual and collective action to implement the evidence-based strategies described previously. Doing so will save lives, reduce avoidable hospitalizations, and improve the quality of life for hundreds of thousands of individuals each year in the United States.
IMPLEMENTATION AND PRACTICAL CONSIDERATIONS
Implementation of this road map should begin with CR programs and their affiliated hospitals instituting process improvements designed to accommodate more patients in an efficient manner, as well as working with their information systems department and electronic medical record personnel to develop an automated CR referral during the hospital discharge process. Patients with appropriate diagnoses should leave the hospital with a written CR referral and a scheduled individual or group visit at the CR program within 1 week of discharge. This referral should be discussed with a CR liaison while the patient is still in the hospital, and communication should be maintained until the patient’s case manager assumes CR care. Cardiac rehabilitation programs and their affiliated hospitals and clinics can work together to identify local gaps in CR delivery and work to continuously reduce those gaps by implementing the additional interventions to increase CR referral and participation listed in Table 1 and the strategies for adherence in Table 2. Practical aspects of systematizing CR referral and enrollment in the Canadian system of care have been well described.58 Taken together, these efforts should increase CR referral rates to over 90%, with CR participation rates that approach or exceed 70%.
CONCLUSION
The benefits of CR are broad and compelling, ranging from decreased mortality and decreased hospitalizations to improvements in functional capacity, insulin sensitivity, depression, and quality of life. Secondary prevention practices in CR support and align with the ABCS of Million Hearts. Improving CR participation from 20% to 70% in 5 years or less is achievable through individual and collective action to implement evidence-based strategies that increase CR referral, enrollment, and adherence. A concordant effort from hospitals and CR programs to increase capacity will also be needed. Doing so will save lives, reduce avoidable hospitalizations, and improve the quality of life for hundreds of thousands of individuals in the United States.
Acknowledgments
Grant Support: This work was supported in part by National Institutes of Health Center of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences (P.A.A., D.S.S.).
The authors thank David Whellan, MD, for his helpful suggestions after reviewing the submitted manuscript. We also express gratitude for the commitment, expertise, and actions of members of the Million Hearts Cardiac Rehabilitation Collaborative, an outgrowth of the Million Hearts Cardiac Rehabilitation Leadership Summit held in November 2015 in Washington, DC, with representatives from over 30 organizations and agencies as well as CR graduates and their families. Represented organizations include the American Association of Cardiovascular and Pulmonary Rehabilitation, AHA, ACC, American Association of Nurse Practitioners, American College of Physicians, American Hospital Association, Heart Failure Society of America, Preventive Cardiovascular Nurses Association, Blue Cross Blue Shield Association, National Medical Association, Patient-Centered Outcomes Research Institute, America’s Essential Hospitals, Mended Hearts, WomenHeart, and Med-Star Health. More about the Million Hearts initiative can be found on the Million Hearts website.2
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Abbreviations and Acronyms
- ABCS
aspirin for those at risk, blood pressure control, cholesterol management, and smoking cessation
- ACC
American College of Cardiology
- AHA
American Heart Association
- CABG
coronary artery bypass graft
- CR
cardiac rehabilitation
- MI
myocardial infarction
- PCI
percutaneous coronary intervention
Footnotes
Potential Competing Interests: Dr Keteyian reports personal fees from NimbleHeart, Inc, unrelated to the submitted work. Ms Lui reports that GRQ, LLC, represents the American Association of Cardiovascular and Pulmonary Rehabilitation regarding regulatory and legislative issues that affect cardiac rehabilitation.
References
- 1.Wright JS, Wall HK, Briss PA, Schooley M. Million hearts— where population health and clinical practice intersect. Circ Cardiovasc Qual Outcomes. 2012;5(4):589–591. doi: 10.1161/CIRCOUTCOMES.112.966978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. [Accessed October 10, 2016];Million Hearts website. http://millionhearts.hhs.gov/
- 3.Frieden TR, Berwick DM. The “Million Hearts” initiative— preventing heart attacks and strokes. N Engl J Med. 2011;365(13):e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- 4.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health and Human Services, Centers for Medicare and Medicaid Services. 42 CFR Parts 510 and 512. Medicare program; advancing care coordination through episode payment models (EPMS); cardiac rehabilitation incentive payment model; and changes to the comprehensive care for joint replacement model (CJR); proposed rule. Fed Regist. 2016;81(148):50794–51039. [Google Scholar]
- 6.Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update; a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association [published correction appears in J Am Coll Cardiol. 2015;65(14):1495] J Am Coll Cardiol. 2011;58(23):2432–2446. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- 7.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121(1):63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7):CD001800. doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Connor GT, Buring JE, Yusuf S, et al. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80(2):234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- 11.Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction: combined experience of randomized clinical trials. JAMA. 1988;260(7):945–950. [PubMed] [Google Scholar]
- 12.Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 13.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345(12):892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- 14.Vanhees L, Fagard R, Thijs L, Amery A. Prognostic value of training-induced change in peak exercise capacity in patients with myocardial infarcts and patients with coronary bypass surgery. Am J Cardiol. 1995;76(14):1014–1019. doi: 10.1016/s0002-9149(99)80287-2. [DOI] [PubMed] [Google Scholar]
- 15.Lavie CJ, Arena R, Swift DL, et al. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ Res. 2015;117(2):207–219. doi: 10.1161/CIRCRESAHA.117.305205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hambrecht R, Wolf A, Gielen S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342(7):454–460. doi: 10.1056/NEJM200002173420702. [DOI] [PubMed] [Google Scholar]
- 17.Ades PA, Savage PD, Toth MJ, et al. High-calorie–expenditure exercise: a new approach to cardiac rehabilitation for overweight coronary patients. Circulation. 2009;119(20):2671–2678. doi: 10.1161/CIRCULATIONAHA.108.834184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease: a meta-analysis [published correction appears in Arch Intern Med. 1996;156(20):2302] Arch Intern Med. 1996;156(7):745–752. [PubMed] [Google Scholar]
- 19.Ades PA, Pashkow FJ, Nestor JR. Cost-effectiveness of cardiac rehabilitation after myocardial infarction. J Cardiopulm Rehabil. 1997;17(4):222–231. doi: 10.1097/00008483-199707000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116(15):1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC) Receipt of outpatient cardiac rehabilitation among heart attack survivors— United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57(4):89–94. [PubMed] [Google Scholar]
- 22.Mueller E, Savage PD, Schneider DJ, Howland LL, Ades PA. Effect of a computerized referral at hospital discharge on cardiac rehabilitation participation rates. J Cardiopulm Rehabil Prev. 2009;29(6):365–369. doi: 10.1097/HCR.0b013e3181b4ca75. [DOI] [PubMed] [Google Scholar]
- 23.Pack QR, Lahr BD, Squires RW, et al. Survey reported participation in cardiac rehabilitation and survival after mitral or aortic valve surgery. Am J Cardiol. 2016;117(12):1985–1991. doi: 10.1016/j.amjcard.2016.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sibilitz KL, Berg SK, Tang LH, et al. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3:CD010876. doi: 10.1002/14651858.CD010876.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Rosenbaum AN, Kremers WK, Schirger JA, et al. Association between early cardiac rehabilitation and long-term survival in cardiac transplant recipients. Mayo Clin Proc. 2016;91(2):149–156. doi: 10.1016/j.mayocp.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Witt BJ, Jacobsen SJ, Weston SA, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44(5):988–996. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics. [Accessed October 31, 2016];Number of all-listed procedures for discharges from short-stay hospitals, by procedure category and age: United States. 2010 http://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf.
- 28.Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics— 2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 29.Fang JC, Ewald GA, Allen LA, et al. Advanced (stage D) heart failure: a statement from the Heart Failure Society of America Guidelines Committee. J Card Fail. 2015;21(6):519–534. doi: 10.1016/j.cardfail.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 30.Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646–659. doi: 10.1161/CIRCRESAHA.113.300268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen HY, Tisminetzky M, Yarzebski J, Gore JM, Goldberg RJ. Decade-long trends in the frequency of 90-day rehospitalizations after hospital discharge for acute myocardial infarction. Am J Cardiol. 2016;117(5):743–748. doi: 10.1016/j.amjcard.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kostis WJ, Deng Y, Pantazopoulos JS, Moreyra AE, Kostis JB Myocardial Infarction Data Acquisition System (MIDAS14) Study Group. Trends in mortality of acute myocardial infarction after discharge from the hospital. Circ Cardiovasc Qual Outcomes. 2010;3(6):581–589. doi: 10.1161/CIRCOUTCOMES.110.957803. [DOI] [PubMed] [Google Scholar]
- 33.Davidson PM, Cockburn J, Newton PJ, et al. Can a heart failure-specific cardiac rehabilitation program decrease hospitalizations and improve outcomes in high-risk patients? Eur J Cardiovasc Prev Rehabil. 2010;17(4):393–402. doi: 10.1097/HJR.0b013e328334ea56. [DOI] [PubMed] [Google Scholar]
- 34.Martin BJ, Hauer T, Arena R, et al. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126(6):677–687. doi: 10.1161/CIRCULATIONAHA.111.066738. [DOI] [PubMed] [Google Scholar]
- 35.Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54(1):25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 36.Valencia HE, Savage PD, Ades PA. Cardiac rehabilitation participation in underserved populations: minorities, low socioeconomic, and rural residents. J Cardiopulm Rehabil Prev. 2011;31(4):203–210. doi: 10.1097/HCR.0b013e318220a7da. [DOI] [PubMed] [Google Scholar]
- 37.Pack QR, Squires RW, Lopez-Jimenez F, et al. The current and potential capacity for cardiac rehabilitation utilization in the United States. J Cardiopulm Rehabil Prev. 2014;34(5):318–326. doi: 10.1097/HCR.0000000000000076. [DOI] [PubMed] [Google Scholar]
- 38.Grace SL, Russell KL, Reid RD, et al. Cardiac Rehabilitation Care Continuity Through Automatic Referral Evaluation (CRCARE) Investigators. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med. 2011;171(3):235–241. doi: 10.1001/archinternmed.2010.501. [DOI] [PubMed] [Google Scholar]
- 39.Choudhry NK, Avorn J, Glynn RJ, et al. Post-Myocardial Infarction Free Rx Event and Economic Evaluation (MI FREEE) Trial. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 40.Sinnott SJ, Buckley C, O’Riordan D, Bradley C, Whelton H. The effect of copayments for prescriptions on adherence to prescription medicines in publicly insured populations: a systematic review and meta-analysis. PLoS One. 2013;8(5):e61914. doi: 10.1371/journal.pone.0064914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taylor RS, Dalal H, Jolly K, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2015;(8):CD007130. doi: 10.1002/14651858.CD007130.pub3. [DOI] [PubMed] [Google Scholar]
- 42.Pack QR, Mansour M, Barboza JS, et al. An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation. 2013;127(3):349–355. doi: 10.1161/CIRCULATIONAHA.112.121996. [DOI] [PubMed] [Google Scholar]
- 43.Beatty AL, Li S, Thomas L, Amsterdam EA, Alexander KP, Whooley MA. Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National Cardiovascular Data Registry 2007 to 2012. J Am Coll Cardiol. 2014;63(23):2582–2583. doi: 10.1016/j.jacc.2014.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thomas RJ, King M, Lui K, Oldridge N, Piña IL, Spertus J. AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation) Circulation. 2010;122(13):1342–1350. doi: 10.1161/CIR.0b013e3181f5185b. [DOI] [PubMed] [Google Scholar]
- 45.Russell KL, Holloway TM, Brum M, Caruso V, Chessex C, Grace SL. Cardiac rehabilitation wait times: effect on enrollment. J Cardiopulm Rehabil Prev. 2011;31(6):373–377. doi: 10.1097/HCR.0b013e318228a32f. [DOI] [PubMed] [Google Scholar]
- 46.Pack QR, Johnson LL, Barr LM, et al. Improving cardiac rehabilitation attendance and completion through quality improvement activities and a motivational program. J Cardiopulm Rehabil Prev. 2013;33(3):153–159. doi: 10.1097/HCR.0b013e31828db386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gaalema DE, Savage PD, Rengo JL, Cutler AY, Higgins ST, Ades PA. Financial incentives to promote cardiac rehabilitation participation and adherence among Medicaid patients. Prev Med. 2016;92:47–50. doi: 10.1016/j.ypmed.2015.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamm LF, Kavanagh T, Campbell RB, et al. Timeline for peak improvements during 52 weeks of cardiac rehabilitation. J Cardiopulm Rehabil. 2004;24(6):374–380. doi: 10.1097/00008483-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Lee AJ, Shepard DS. Costs of cardiac rehabilitation and enhanced lifestyle modification program. J Cardiopulm Rehabil Prev. 2009;29(6):348–357. doi: 10.1097/HCR.0b013e3181b4cc0a. [DOI] [PubMed] [Google Scholar]
- 50.Clark RA, Conway A, Poulsen V, Keech W, Trimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015;22(1):35–74. doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 51.Beckie TM, Beckstead JW. Predicting cardiac rehabilitation attendance in a gender-tailored randomized clinical trial. J Cardiopulm Rehabil Prev. 2010;30(3):147–156. doi: 10.1097/HCR.0b013e3181d0c2ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lounsbury P, Elokda AS, Gylten D, Arena R, Clarke W, Gordon EEI. Text-messaging program improves outcomes in outpatient cardiovascular rehabilitation. Int J Cardiol Heart Vasculature. 2015;7:170–175. doi: 10.1016/j.ijcha.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keteyian S, Relyea B, Blount M, Bryant S. The design and philosophy of a hospital-based and community-based comprehensive cardiac rehabilitation program. J Cardiopulmonary Rehabil. 1985;5:492–495. [Google Scholar]
- 54.Turk-Adawi KI, Oldridge NB, Tarima SS, Stason WB, Shepard DS. Cardiac rehabilitation patient and organizational factors: what keeps patients in programs? J Am Heart Assoc. 2013;2(5):e000418. doi: 10.1161/JAHA.113.000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wyer SJ, Earll L, Joseph S, Harrison J, Giles M, Johnston M. Increasing attendance at a cardiac rehabilitation programme: an intervention study using the Theory of Planned Behaviour. Coronary Health Care. 2001;5(3):154–159. [Google Scholar]
- 56.Lobelo F, Stoutenberg M, Hutber A. The Exercise is Medicine Global Health Initiative: a 2014 update. Br J Sports Med. 2014;48(22):1627–1633. doi: 10.1136/bjsports-2013-093080. [DOI] [PubMed] [Google Scholar]
- 57.Fletcher GF, Ades PA, Kligfield P, et al. American Heart Association Exercise; Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology; Council on Nutrition, Physical Activity and Metabolism; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128(8):873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- 58.Grace SL, Chessex C, Arthur H, et al. Systematizing inpatient referral to cardiac rehabilitation 2010: Canadian Association of Cardiac Rehabilitation and Canadian Cardiovascular Society joint position paper endorsed by the Cardiac Care Network of Ontario. Can J Cardiol. 2011;27(2):192–199. doi: 10.1016/j.cjca.2010.12.007. [DOI] [PubMed] [Google Scholar]