Abstract
Purpose
The management of distal radius fractures differs based on the nature of the fracture and the experience of the surgeon. We hypothesized that patients requiring surgical intervention would undergo different procedures when in the care of a surgeon with subspecialty training in hand surgery as compared to surgeons with no subspecialty training in hand surgery. The null hypothesis was that intervention, as measured in the American Board of Orthopaedic Surgery (ABOS) database, would be the same, independent of subspecialty training.
Methods
We queried the ABOS database for case log information submitted for part II of the ABOS Examination. Queries for all codes involved with distal radius fractures management were combined with associated codes for management of median nerve neropathy, triangular fibrocartilage complex tears, ulnar shaft and styloid fractures. Hand fellowship trained orthopaedic surgeons were compared to those completing other fellowships and non-fellowship trained orthopaedic surgeons during their board collection period.
Results
During the study period, 2317 Orthopedic surgeons reported treatment of 15,433 distal radius fractures. Of these surgeons, 411 had hand fellowship training. On a per surgeon basis, fellowship trained hand surgeons operatively treated more multi-fragment intra-articular distal radius fractures than their non-hand fellowship trained counterparts (5.3 vs 1.2). Additional procedures associated with the management of distal radius fractures were also associated with the fellowship training of the treating surgeon.
Conclusions
Among orthopaedic surgeons taking part II of the American Board of Orthopaedic Surgery certifying examination, differences exist in the type, management and reporting of distal radius fractures among surgeons with different areas of fellowship training.
Clinical Relevance
This study describes the association of hand surgery fellowship training on the choice of intervention for distal radius fractures and associated conditions.
Keywords: Distal Radius, Specialty Training, Population Outcomes
INTRODUCTION
Fractures of the distal radius are common injuries and account for roughly 1/6 of all fractures [1]. Prior to about 1995 most distal radius fractures (DRF), independent of fracture type, were treated without surgery [2]. Since that time there has been considerable change in the treatment of these injuries with a trend towards increased operative management. Today, a wide variety of surgical and non-surgical options are available for the treatment of DRF. These include percutaneous pinning, external fixation, volar or dorsal plating, fragment specific fixation and spanning internal fixation or some combination of these techniques [3–6].
The clinical practice guideline, published by the American Academy of Orthopaedic Surgeons (AAOS) [7], highlights the dearth of high quality evidence to guide the management of distal radius fractures. Some surgeons believe that recommendations regarding treatment are based primarily on level IV evidence, fostering debate with regards to the optimal management of these fractures as well as their associated conditions. With this in mind, the AAOS work group was unable to recommend for or against surgical treatment of associated median nerve neuropathy or ulnar styloid fractures. However, based on a single level II study by Varitimidis et al. they did recommend repair of ligamentous injuries such as triangular fibrocartilage complex (TFCC) tears [8].
The management of conditions associated with DRF can also affect patient outcomes, however the treatment of these conditions is also not well defined in the current literature [9].
A previous study by Chung et al. [10] demonstrated regional differences in the treatment of DRF among Medicare beneficiaries. Further work by Chung et al. [11] revealed that members of the American Society for Surgery of the Hand (ASSH) are more likely than non-members to treat DRF with internal fixation. Ward et al. [12] found that increasing surgeon experience was correlated with a decrease in early complication rates in patients with DRF treated with volar plating.
The purpose of this study was to assess the management and reporting of DRF and concurrent conditions in relation to the fellowship training of ABOS candidates in order to determine if any association exists between fellowship training, complexity of fracture, and method of treatment. We hypothesized that surgeons within their board collection period would perform different surgical procedures in the setting of DRF and that these differences would be related to the nature of the surgeons’ subspecialty training in hand surgery among other subspecialties.
MATERIALS AND METHODS
In the United States, the American Board of Orthopaedic Surgery (ABOS) confers board certification on orthopaedic surgeons. To be eligible to take the board examination, a surgeon must have graduated from an accredited orthopaedic surgery residency program and take a two-part examination. Successful completion of part I, a computerized multiple-choice examination, is a prerequisite to take part II. Part II is a practice-based oral exam taken after 20 months of practice. Surgical cases performed during a predetermined six-month period are submitted for review. The data submitted for each case includes International Classification of Diseases (ICD-9) codes, Current Procedural Terminology (CPT) codes, patient age and gender, geographical region of the surgeon’s practice, surgical complications, fellowship training of the surgeon and a brief verbal description of the procedure and indications. These cases are entered into a secure database [13]. Cases where the surgeon neither manipulates nor operates can be under-reported in this database, resulting in certain codes being under-represented. Prior to submitting their cases to the ABOS, surgeons are informed that the data that they submit may be used for research purposes. This de-identified data is the subject of our study.
This database was queried for cases of DRF treated by orthopaedic surgeons using the CPT codes 25600 (closed treatment of distal radius fracture or epiphyseal separation, with or without fracture of ulnar styloid; without manipulation) and 25605(closed treatment of distal radial fracture or epiphyseal separation), 25606 (percutaneous skeletal fixation of distal radial fracture or epiphyseal separation), 25607 (open treatment of distal radial extra-articular fracture or epiphyseal separation, with internal fixation), 25608 (open reduction of distal radial intra-articular fracture or epiphyseal separation; with internal fixation of 2 fragments), 25609 (open reduction of distal radial intra-articular fracture or epiphyseal separation; with internal fixation of 3 fragments) between the years 2007 to 2011. The resulting data set was then examined to ascertain if any associated procedures were performed. The following CPT codes were used; 64721 and 29848 (carpal tunnel release), 25107 (TFCC repair), 25651 and 25652 (ulnar styloid fixation) and 25545 (open reduction and internal fixation of an ulnar shaft fracture). The reported complications for each case were also gathered. The cases were then grouped based on whether or not the treating surgeon reported fellowship training.
Statistical Analysis
The proportion of DRF treated with closed reduction, percutaneous fixation or open reduction and internal fixation (ORIF) w determined. The ORIF group could then be further subdivided into extra- or intra-articular fractures and whether or not there were multiple intra-articular fracture fragments. The data was initially divided into three groups based on whether the surgeon reported hand surgery fellowship, a fellowship other than hand surgery or no fellowship. During our statistical analyses, surgeons who reported a fellowship other than hand surgery and surgeons who did not complete a fellowship were combined. This was done because some orthopedic residency programs include a mandatory PGY 6 trauma fellowship year making it difficult to discern those who graduated from these programs from those who participated in a separate trauma fellowship. The two-tailed Fisher’s exact test was then used to compare the proportions of cases for each fracture type between surgeons who reported hand fellowship training and those who did not. Alpha was set to 0.05 for all statistical tests.
Source of Funding
There was no external funding source for this study.
RESULTS
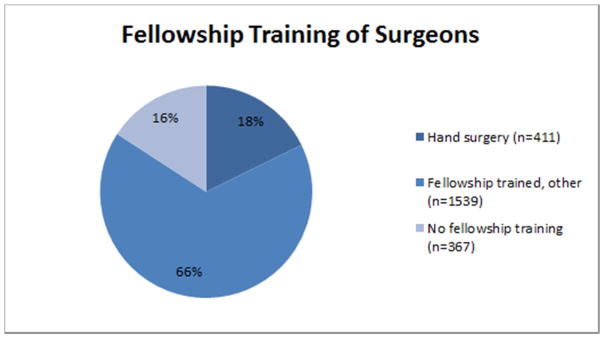
From 2007 to 2011, 2317 orthopaedic surgeons taking the ABOS part II examination submitted 15,433 cases of DRF. Of these surgeons, 367 (15.8%) had not undergone post residency fellowship training. There were 411 (17.7%) fellowship trained hand surgeons and 1539 (66.4%) surgeons with fellowship training other than hand surgery included in the study, Figure 1.
Figure 1.
The fellowship training of the surgeons included in the study.
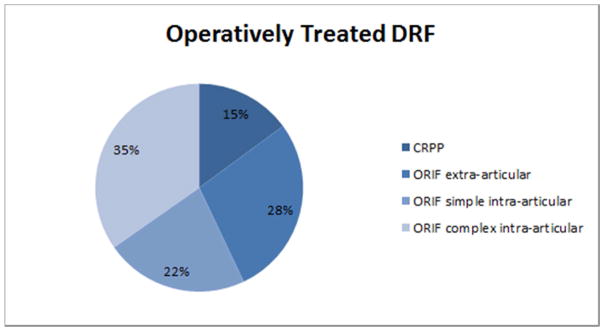
Of the cases submitted, 16.4% (2536) were for closed treatment, with or without manipulation, leaving 83.6% (12897) operatively treated DRF. Of these cases, 14.9% (1922) were treated with closed reduction and percutaneous pinning (CRPP). The remaining, operatively treated fractures were; 28.1% (3617) extra-articular treated with open reduction and internal fixation (ORIF), 22.3% (2881) simple intra-articular, corresponding to fixation of 2 articular fragments and CPT code 25608, treated with ORIF and 34.7% (4477) complex intra-articular, corresponding to fixation of 3 or more articular fragments and CPT code 25609, treated with ORIF. The breakdown of operatively treated DRF is shown in Figure 2.
Figure 2.
The majority, 84% of the DRF included in this study was treated with surgery. Of the fractures treated operatively, 85% underwent an open reduction and internal fixation. Over ⅓ of the operatively treated injuries were multifragmented intra-articular DRF.
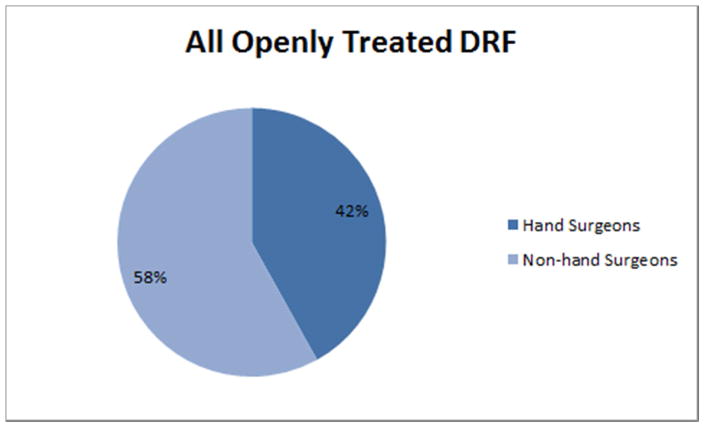
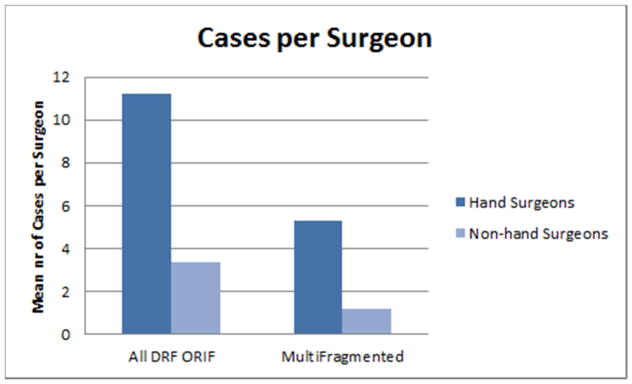
ORIF was employed in 71.1% (10975) of surgical procedures, 59% of which were performed by hand surgeons. In 41.9% (4601) of operatively treated fractures the treating physician was a hand surgeon, Figure 3. On average, each hand surgeon performed 11.2 ORIF for DRF during their board collection period compared with 3.3 for the non-hand surgeons. Hand surgeons also submitted more interventions for complex intra-articular DRF. Of the submitted DRFs treated by ORIF among hand surgeons, almost half (47.1%) were complex intra-articular fractures compared with 36.3% for the non-hand surgeons (p < 0.05). The per surgeon ratio of complex intra-articular fracture was 5.3:1.2 for hand surgeons vs non-hand surgeons, Figure 4.
Figure 3.
Fellowship trained hand surgeons made up 18% of the surgeons, however, 42% of the open reduction and internal fixation for DRF were performed by a hand surgeon in this study.
Figure 4.
On average, each hand surgeon performed three times as many DRF ORIF as their colleagues. They also treated over four times as many multifragmented intra-articular injuries. Almost half, 47.1% of all DRF treated with ORIF by a hand surgeon were multifragmented intra-articular injuries.
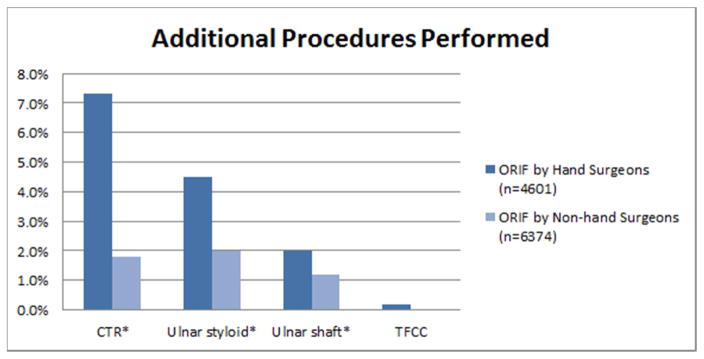
Figure 5 shows the rates of additional procedures performed at the time of DRF ORIF. Hand surgeons performed concomitant CTR in 7.3% (334) of cases whereas non-hand surgeons performed CTR in only 1.8% (116) (p <0.05). Ulnar styloid fixation was more often performed by hand surgeons than non-hand surgeons, 4.5% vs. 2.0% (p <0.05). The rate of concomitant ulnar shaft ORIF fixation for hand surgeons was 2.0% (168) vs. 1.2% (92) for the non-hand surgeons (p < 0.05). Hand surgeons also performed more TFCC repairs than did their non-hand surgeon colleagues, though there were too few cases to enable meaningful statistical analysis.
Figure 5.
Fellowship trained hand surgeons performed more CTR, ulnar styloid and shaft repairs, in association with ORIF of DRF, than did their colleagues. Hand surgeons also performed more TFCC repairs but the number of cases was not numerous enough for analysis.
* statistically significant difference.
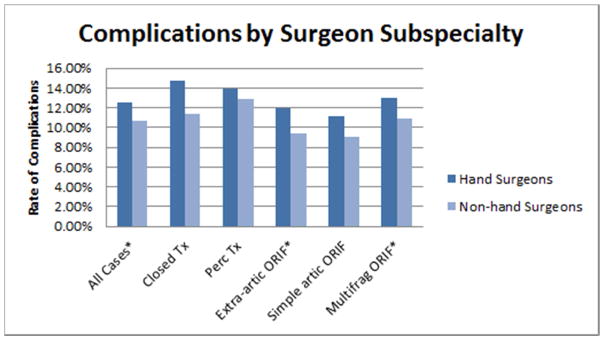
Fellowship trained hand surgeons reported higher complication rates (figure 6) (12.5% vs 10.7, p < 0.05). In all five treatment groups (closed treatment, percutaneous fixation, extra-articular fracture fixation, simple intra-articular fracture fixation and complex intra-articular fracture fixation), hand surgeons reported higher complication rates though the difference was only statistically significant for extra-articular and complex intra-articular fractures (figure 6).
Figure 6.
Fellowship trained hand surgeons reported higher rates of complications for all treatment groups. This difference was statistically significant for all cases combined, ORIF of extra-articular DRF and for ORIF of complex intra-articular fractures.
* statistically significant difference.
DISCUSSION
Distal radius fractures are common injuries seen by many orthopaedic surgeons. Hand fellowship trained surgeons operatively treated more DRFs than did non-hand surgeons. A large number of these cases are the more complex, multi-fragment, intra-articular fractures, which constitute almost half (47.1%) of those treated by hand surgeons. This may reflect the increased experience and level of comfort with complex upper extremity injuries gained from a year of post residency fellowship training, a greater availability of hand surgeons for treatment, more perceived interest in treating these fractures among surgeons with hand fellowship training or referral patterns within and outside of subspecialty group.
The literature on the rate of median nerve neuropathy (MNN) following operatively treated DRF is varied. Hove et al. and Zoubos et al. both reported a 0% incidence of MNN following ORIF of DRF[14,15]. Furthermore, not all cases of MNN following DRF surgery require surgical treatment [19]. Thus, the number of patients undergoing ORIF for a DRF that would benefit from a carpal tunnel release (CTR) is not clear. In this study, it is not known whether there was a greater baseline incidence of MNN in the patients treated with CTR, whether the hand surgeons may be more likely to diagnose this condition, or if CTR was done prophylactically due to the nature of the injury, which was reportedly more severe based on treatment chosen by hand surgeons.
Ulnar styloid fractures are commonly associated with DRF, but several studies have reported that ulnar styloid fractures might not have an impact on the final outcome following DRFs [20–22]. Other studies have found an association between fractures of the ulnar styloid and decreased grip strength, distal radioulnar joint instability, and decreased range of motion [23–27]. The role that a fracture of the ulnar styloid will play in the overall outcome of a patient with a DRF likely depends on the size and location of the styloid fracture fragment and whether there is associated disruption of the TFCC. In cases where the DRUJ is unstable following DRF fixation, some surgeons consider fixing the ulnar styloid [28,29].
We found that fellowship trained hand surgeons performed ulnar styloid fixation at more than twice the rate as those without fellowship training in hand surgery (4.5% vs. 2.0%; p <0.05). Similarly, hand surgeons performed more repairs of the triangular fibrocartilage complex. Although it may appear that these differences represent different propensities to treat ulnar sided injuries, in fact they may simply suggest a different likelihood of these injuries occurring in the practices of hand surgeons. Additionally, these differences are small and may not represent true clinical differences.
The complication rate reported by hand surgeons treating DRF was higher than that reported by non-hand surgeons. There are several possible explanations for this. More complex injuries are more likely to result in complications and, as previously noted in our data, fellowship trained hand surgeons may treat a higher proportion of complex DRF. Within each treatment group, more challenging cases may also be more likely to be referred to a hand surgeon. This varying degree of complexity may not be amenable to the limited categorization by treatment codes. While the differences in complication rates may, in fact, be small, we believe that it may represent some difference in the accuracy of which these two cohorts report complications. Hand surgeons also performed associated procedures such as CTR, ulnar styloid repair and ulnar shaft ORIF more frequently than did non-hand surgeons and perhaps performing additional procedures increases the likelihood of experiencing a complication. Odumala et al. reported higher rates of transient median nerve dysfunction in patients with DRF where a prophylactic CTR was performed [16].
As with all database driven studies, the strengths and weaknesses of this study reflect the quality of the database and its verifiers. The ABOS database is structured; its contents monitored by the board through the review process. Surgeons are sanctioned when complications are under-reported. It therefore provides a relatively accurate reflection of management when intervention by the surgeon is undertaken. It contains detailed and specific information about a large number of cases performed by a cohort of orthopaedic surgeons early in their practices. The case lists contain all the surgical procedures performed by those surgeons during a defined six month period each year and they are certified by medical records personnel at each hospital as being complete and accurate. Although the data is self-reported, we believe that the candidates for board certification take great care to be complete and accurate in the data they enter, because they know that some cases will be selected and examined in detail as part of a high-stakes exam process and because there are adverse consequences (potential failure) associated with discovery of incorrect or incomplete information. Information on the general medical condition of the specific patient, signs and symptoms of the injury, or presence of other injuries are not included in the database and we were therefore unable to account for these factors in our analysis. Another limitation of the study is the lack of a more granular classification of the fractures included in the study which may have allowed selection bias to occur with the more difficult distal radius fractures in each category being treated by the hand surgeon, thereby allowing more of an opportunity for the hand surgeons to recognize and treat more associated conditions. Lastly, it should be noted that not every code associated with DRF management could be included in our analysis. Codes specific for the closed treatment of the ulna as well as DRUJ instability were not included as their use among data collected from the ABOS database was so sporadic that statistical analysis with the inclusion of these codes was impossible. In the end we cannot say if hand surgeons care for more complex fractures, suffer more complications or both. In the absence of controlling for case mix, few comparisons can be accepted at face value. We can say that hand surgeons report worse fractures, perform more procedures and care for more distal radius fracture patients.
CPT terminology does not define the type of fixation method used. It only defines the type of fracture fixed. As such, a key problem with the data used involves correlating the type of fracture with method of fixation utilized by the surgeon. We do not believe that the hardware fixation method is the most critical point in the decision making process, although it is clearly important. Without reviewing the xrays from hundreds of surgeons, it would be impossible to determine a surgeon’s predilection towards one type of hardware, despite the type of fracture remaining the same.
Lastly, the surgeons in this study are in the early stages in their career, as most have been in practice for approximately two years. This allows comparison of surgeons with relatively up-to-date training. Thus, these results may not be entirely reflective of all practicing orthopaedic surgeons. Future studies will need to compare data from surgeons recertifying at ten-year intervals, to investigate the practice patterns of surgeons further on in their surgical career.
In summary, we found that DRF is a common injury managed by orthopaedic surgeons taking part II of the ABOS certification exam. Within this population of surgeons, fellowship trained hand surgeons operatively treat more DRF than their non-hand surgeon colleagues. Hand surgeons report operative treatment for a greater number of complex, intra-articular wrist fractures than non-hand surgeons. Lastly, hand surgeons are more likely to perform a CTR, repair an ulnar styloid or ulnar shaft fracture than non-hand surgeons.
Footnotes
All named authors hereby declare that they have no conflicts of interest to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Graff S, Jupiter J. Fracture of the distal radius: classification of treatment and indications for external fixation. Injury. 1994;25(Suppl 4):S-D14–25. doi: 10.1016/0020-1383(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 2.Green DP. Green’s operative hand surgery. 6. Philadelphia: Elsevier/Churchill Livingstone; 2011. [Google Scholar]
- 3.Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87:837–840. doi: 10.1302/0301-620X.87B6.15608. [DOI] [PubMed] [Google Scholar]
- 4.Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2:248–252. doi: 10.1097/00130911-199812000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Grewal R, Perey B, Wilmink M, Stothers K. A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation. J Hand Surg Am. 2005;30:764–772. doi: 10.1016/j.jhsa.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 6.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27:205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 7.Lichtman DM, Bindra RR, Boyer MI, Putnam MD, Ring D, Slutsky DJ, et al. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180–189. doi: 10.5435/00124635-201003000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Varitimidis SE, Basdekis GK, Dailiana ZH, Hantes ME, Bargiotas K, Malizos K. Treatment of intra-articular fractures of the distal radius: fluoroscopic or arthroscopic reduction? J Bone Joint Surg Br. 2008;90:778–785. doi: 10.1302/0301-620X.90B6.19809. [DOI] [PubMed] [Google Scholar]
- 9.Cooney WP, 3rd, Dobyns JH, Linscheid RL. Complications of Colles’ fractures. J Bone Joint Surg Am. 1980;62:613–619. [PubMed] [Google Scholar]
- 10.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung KC, Shauver MJ, Yin H. The relationship between ASSH membership and the treatment of distal radius fracture in the United States Medicare population. J Hand Surg Am. 2011;36:1288–1293. doi: 10.1016/j.jhsa.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 12.Ward CM, Kuhl TL, Adams BD. Early complications of volar plating of distal radius fractures and their relationship to surgeon experience. Hand (N Y) 2011;6:185–189. doi: 10.1007/s11552-010-9313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garrett WE, Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, et al. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660–667. doi: 10.2106/JBJS.E.01208. [DOI] [PubMed] [Google Scholar]
- 14.Hove LM, Nilsen PT, Furnes O, Oulie HE, Solheim E, Molster AO. Open reduction and internal fixation of displaced intraarticular fractures of the distal radius. 31 patients followed for 3–7 years. Acta Orthop Scand. 1997;68:59–63. doi: 10.3109/17453679709003977. [DOI] [PubMed] [Google Scholar]
- 15.Zoubos AB, Babis GC, Korres DS, Pantazopoulos T. Surgical treatment of 35 volar Barton fractures. No need for routine decompression of the median nerve. Acta Orthop Scand Suppl. 1997;275:65–68. [PubMed] [Google Scholar]
- 16.Odumala O, Ayekoloye C, Packer G. Prophylactic carpal tunnel decompression during buttress plating of the distal radius--is it justified? Injury. 2001;32:577–579. doi: 10.1016/s0020-1383(00)00198-4. [DOI] [PubMed] [Google Scholar]
- 17.Jupiter JB, Fernandez DL, Toh CL, Fellman T, Ring D. Operative treatment of volar intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1996;78:1817–1828. doi: 10.2106/00004623-199612000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Ruch DS, Papadonikolakis A. Volar versus dorsal plating in the management of intra-articular distal radius fractures. J Hand Surg Am. 2006;31:9–16. doi: 10.1016/j.jhsa.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Ho AW, Ho ST, Koo SC, Wong KH. Hand numbness and carpal tunnel syndrome after volar plating of distal radius fracture. Hand (N Y) 2011;6:34–38. doi: 10.1007/s11552-010-9283-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am. 2000;25:464–468. doi: 10.1053/jhsu.2000.6467. [DOI] [PubMed] [Google Scholar]
- 21.Richards RS, Bennett JD, Roth JH, Milne K., Jr Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22:772–776. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 22.Roysam GS. The distal radio-ulnar joint in Colles’ fractures. J Bone Joint Surg Br. 1993;75:58–60. doi: 10.1302/0301-620X.75B1.8421035. [DOI] [PubMed] [Google Scholar]
- 23.Hauck RM, Skahen J, 3rd, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg Am. 1996;21:418–422. doi: 10.1016/S0363-5023(96)80355-8. [DOI] [PubMed] [Google Scholar]
- 24.Oskarsson GV, Aaser P, Hjall A. Do we underestimate the predictive value of the ulnar styloid affection in Colles fractures? Arch Orthop Trauma Surg. 1997;116:341–344. doi: 10.1007/BF00433986. [DOI] [PubMed] [Google Scholar]
- 25.Stoffelen D, De Smet L, Broos P. The importance of the distal radioulnar joint in distal radial fractures. J Hand Surg Br. 1998;23:507–511. doi: 10.1016/s0266-7681(98)80134-4. [DOI] [PubMed] [Google Scholar]
- 26.Kaukonen JP, Karaharju EO, Porras M, Luthje P, Jakobsson A. Functional recovery after fractures of the distal forearm. Analysis of radiographic and other factors affecting the outcome. Ann Chir Gynaecol. 1988;77:27–31. [PubMed] [Google Scholar]
- 27.Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000;(376):229–235. doi: 10.1097/00003086-200007000-00031. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez DL. Fractures of the distal radius: operative treatment. Instr Course Lect. 1993;42:73–88. [PubMed] [Google Scholar]
- 29.May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am. 2002;27:965–971. doi: 10.1053/jhsu.2002.36525. [DOI] [PubMed] [Google Scholar]