Graphical abstract
Keywords: Aging, Proprioception, Neck, Position sense, Kinesthesia, Somatic sensation
Abstract
This study quantitatively assesses the association between age and cervical joint position error (JPE) and compares JPE between young and older asymptomatic subjects. Subjects (n = 230) ranging in age from 17 to 70 years volunteered to participate in the study. Cervical JPE was measured for all subjects with the active movement angle reproduction test in degrees using a digital inclinometer; testing was done in all cervical movement directions (flexion, extension, side-bending right and left, rotation right and left). Subjects were divided into two groups: young (n = 169, mean age: 32.4 years; range 17–49 years) and older (n = 61, mean age: 61.9 years; range 50–70 years) and JPE was compared. Pearson’s product-moment correlation coefficients were significant and positive for the association of age on cervical JPE in flexion (r = 0.71), extension (r = 0.81), side-bending right (r = 0.77), side-bending left (r = 0.84), rotation right (r = 0.84), and rotation left (r = 0.84). JPE was significantly larger (for all movement directions) in the older subject group (P < 0.001). Advancing age was significantly associated with the increasing cervical JPE and older subjects showed greater errors when compared to younger subjects.
Introduction
Proprioception refers to information sent by afferent receptors from peripheral muscles, capsules, ligaments and joints to the central nervous system that contributes to efficient neuromuscular control of movement and joint stability [1], [2], [3], [4], [5]. Proprioception encompasses the sensation of joint position and joint movement (kinesthesia) [5], [6].
Position sense of the head and neck is mediated by cervical proprioceptors, visual stimuli, and vestibular systems [7], [8]. Sensory information from mechanoreceptors in structures in and around a joint plays an important role in joint stability [9]. Abnormal cervical afferent inputs result in an impaired cervical position sense, which is measured as cervical joint position error (JPE) [10], [11], [12]. Cervical position sense primarily reflects ascending inputs (afferent) from the neck muscle, capsule and ligament receptors of the cervical spine [13], [14]. Head positioning tests are frequently adapted to assess cervical JPE [8], [15], [16], [17], [18], [19]. Several methods exist to investigate cervical JPE, and the most commonly used is the active movement angle reproduction test, which requires the subject to relocate a neutral head position or a target head position selected by the investigator [8], [15]. In head position sense measurement studies, the variable measured is the difference between the reference point position entrenched initially (either a neutral or target position) and the position produced by the subject when attempting to match the target position [8]. This difference is called JPE and has angular units of degrees (°). As humans age, the cervical spine undergoes degeneration, leading to decreased cervical range of motion (ROM), decreased cervical muscle strength and an altered length-tension relationship [20], [21], [22]. These changes may contribute to a reduced cervical joint position sense [22]. Age-related reduction of joint position sense in peripheral joints such as the hip [23], knee [24], [25], [26], ankle [27], [28], [29] and upper extremity joints [30], [31] of asymptomatic subjects has been documented, and JPE is associated with injury, joint pain, muscle fatigue, and chronic pain [27], [32], [33], [34]. However, literature on the effect of age on cervical joint position sense in asymptomatic subjects is lacking. A study on patients with whiplash injury (ages 18–66 years) suggests a positive correlation between age and cervical JPE [35]. This supports the idea that age can influence cervical JPE in cervical pathological conditions. This study hypothesizes that cervical joint position sense and cervical JPE correlate with age in asymptomatic subjects, and that cervical JPE is larger in older subjects compared to younger subjects. The objective of this study was to quantitatively assess the association of age on cervical JPE in asymptomatic individuals and to compare cervical JPE of younger and older subjects.
Subject and methods
Subjects
Volunteer participants were recruited through advertisements in the physical therapy department of the university and in the local city, in the form of posters and verbal announcements. A total of 230 asymptomatic subjects (age range: 17–70 years) were recruited to participate in the study. Subjects were divided into two groups: younger (n = 169, mean age = 32.4 years; range = 17–49 years) and older (n = 61, mean age = 64.9 years; range = 50–70 years). All subjects included in the study reported having no neck pain at the time of the study. Subjects were excluded if they had prior treatment for neck pain; any history of traumatic spinal injury; a whiplash-associated disorder; central nervous system impairment such as paresthesia; vestibular impairment such as vertigo, dizziness or motor imbalance; or neck pain elicited by cervical motion in the range used for the study. All subjects were required to attend two sessions. In the first session, subjects were familiarized with the equipment and re-positioning tasks and in the second session, cervical JPE was assessed. Demographic data (age, height, weight) were recorded. Subjects were required to sign an informed consent prior to participating in the study. This study was approved by the university ethics review board committee (REC/2016-01-06).
Instrumentation
Cervical JPE was measured using a Dualer IQ digital inclinometer (J-Tech Medical, Midvale, UT, USA; Fig. 1). The digital inclinometer is reliable, fast, and high in measurement precision [36], [37]. Digital inclinometer spine evaluation protocols are well established and endorsed by the American Medical Association (AMA) [38]. The digital inclinometer allows clinicians to evaluate range of motion and proprioception using dynamic inclinometry similar to that used in other goniometric protocols [39]. The digital inclinometer has shown test-retest reliability for measuring spine range of motion [38], [40].
Fig. 1.
Cervical joint position error testing using digital inclinometer.
Measurement of cervical joint position error
For the test, subjects sat upright in a chair with back support. An erect posture with hips and knees at approximately 90 degrees and feet placed firmly on the ground was maintained throughout the test. A strap secured the thoracic spine to the chair during cervical movements. The active movement angle reproduction test with target position reproduction was used to measure cervical JPE. The target head position to be reproduced by the subjects was selected by the examiner as 50% of the available range of motion (ROM) for the subject. Subjects were asked to keep their eyes closed during the test. To measure cervical JPE, subjects adopted two positions: (1) a sitting position, which measures JPE in flexion, extension, and side-bending right and left; and (2) a supine position, which measures JPE in rotation to right and left. A digital inclinometer was placed on the side of the head to measure JPE in flexion and extension, on the center of forehead to measure JPE in side-bending right and left, and at the vertex of the head in the supine lying position to measure JPE in rotation to right and left.
Cervical ROM was measured first to determine target head position. The examiner then moved the subject’s head slowly to the predetermined target position (50% of maximum range of motion). The head was maintained in the target position for 3 s and subjects were asked to remember that position. The head was then brought to the neutral position by the examiner, and the subject asked to actively re-position their head to the target position. When the subject indicated that he or she had reached the reference position, relocation accuracy was measured in degrees. Subjects were instructed to perform the test as accurately as possible and to verbally indicate when they felt sure that they had reached the target position. No visual or verbal feedback was given to subjects during the test. Subjects performed three trials in each movement direction (cervical JPE in flexion, extension, side bending right and left, rotation right and left), and the average JPE of the three trials was used for analysis. The order of testing movement directions was randomized using a simple lottery method. The assessor recording the cervical JPE was blinded to the aim of the study to eliminate the bias. All measurements were recorded by the same evaluator and the inclinometer device was calibrated between tests and directions. Absolute error was taken as a measurement of JPE; absolute error is the unsigned difference between the actual angle and the target angle and, unlike constant or relative error, it has no directional bias [41].
Statistical analysis
All statistical analyses were done using SPSS v. 20.0 (IBM Corp., 2011), using a statistical significance criterion of 0.05 with a 95% confidence interval. A Shapiro-Wilk’s test was used to confirm that data were normally distributed. Pearson’s product-moment correlation was used to test the relationship between each cervical JPE measure and age. An independent sample t-test was used to compare cervical JPE between age groups (young vs. old). Minimal detectable change (MDC) is a clinically useful measure used to estimate true change versus error change, and indicates how much of change must occur in a measure with a given random error variance and a 95% certainty to conclude that the change is due to true change [42], [43]. MDC was calculated as follows: (Standard Error Mean (SEM) × 1.65 × √2) [42], where SEM is the estimated standard deviation of the sample mean [43]. This value is estimated as the standard deviation of one sample divided by the square root of sample size.
Results
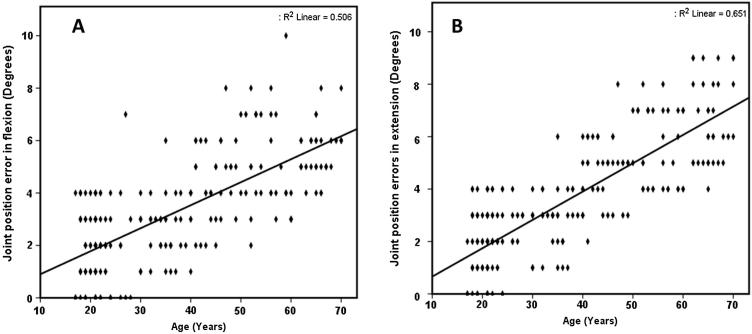
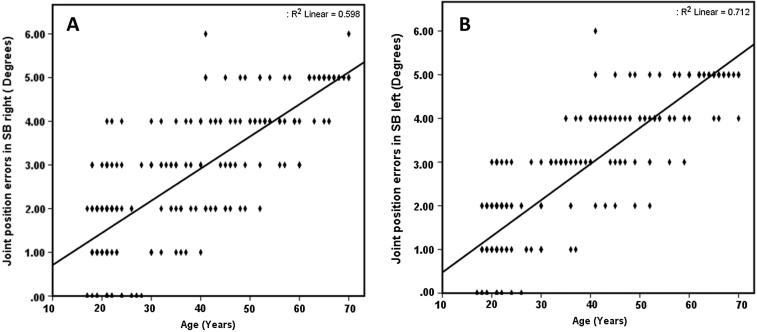
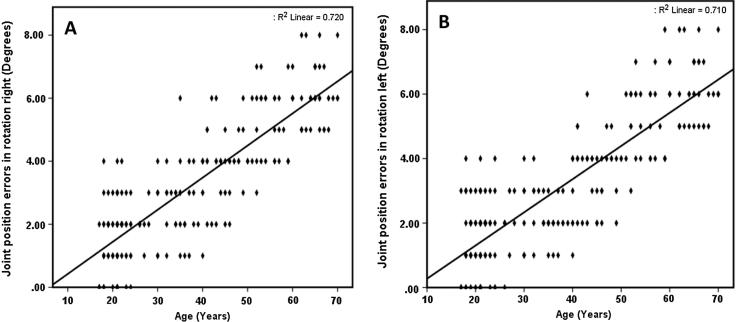
Sample size for all tests was 230. Age was significantly positively correlated with JPE in flexion (Pearson’s r = 0.71; 95% CI = 0.62–0.80; P < 0.001) and extension (Pearson’s r = 0.81; 95% CI = 0.73–0.88; P < 0.001) tests (Fig. 2). A positive correlation was also present between age and JPE for side-bending right (Pearson’s r = 0.77; 95% CI = 0.69–0.85; P < 0.001) and side-bending left (Pearson’s r = 0.84; 95% CI = 0.77–0.91; P < 0.001) measures (Fig. 3). Finally, significant positive correlations were also found for right and left rotation tests (rotation right: Pearson’s r = 0.84; 95% CI = 0.78–0.91, P < 0.001; rotation left: Pearson’s r = 0.84; 95% CI = 0.77–0.91; P < 0.001) (Fig. 4).
Fig. 2.
(A) Positive correlation between age and JPE in flexion (Pearson’s r = 0.71; 95% CI, 0.62–0.80; P < 0.001). (B) Positive correlation between age and JPE in extension (Pearson’s r = 0.81; 95% CI, 0.73–0.88; P < 0.001).
Fig. 3.
(A) Positive correlation between age and JPE in side bending right (Pearson’s r = 0.77; 95% CI, 0.69–0.85; P < 0.001). (B) Positive correlation between age and JPE inside bending left (Pearson’s r = 0.84; 95% CI, 0.77–0.91; P < 0.001).
Fig. 4.
(A) Positive correlation between age and JPE in rotation right (Pearson’s r = 0.84; 95% CI, 0.78–0.91; P < 0.001). (B) Positive correlation between age and JPE in rotation left (Pearson’s r = 0.84; 95% CI, 0.77–0.91; P < 0.001).
Cervical JPE is significantly lower in younger subjects compared to older subjects for all cervical movement directions (P < 0.001; Table 1). Overall, JPE errors are largest in cervical extension (mean degrees ± SD; young age = 3.11 ± 1.92; old age = 6.53 ± 1.61) with SEM of 0.340 and MDC of 0.793. The smallest JPE was noted in side bending left (young age = 2.27 ± 1.46; old age = 4.66 ± 0.63) with SEM of 0.248 and MDC of 0.578.
Table 1.
Mean ± SD in cervical JPE for young and older age groups.
| JPEa (degrees) variable | Young (n = 169) | Old (n = 61) | 95% CIb | SEMc | MDCd | P-valuee |
|---|---|---|---|---|---|---|
| Flexion | 2.95 ± 1.98 | 5.31 ± 1.22 | −3.06 to −1.68 | 0.342 | 0.797 | <0.001 |
| Extension | 3.11 ± 1.92 | 6.53 ± 1.61 | −4.09 to −2.75 | 0.340 | 0.793 | <0.001 |
| Side-bending right | 2.36 ± 1.43 | 4.72 ± 0.65 | −2.83 to −1.87 | 0.244 | 0.569 | <0.001 |
| Side-bending left | 2.27 ± 1.46 | 4.66 ± 0.63 | −2.88 to −1.90 | 0.248 | 0.578 | <0.001 |
| Rotation right | 2.68 ± 1.65 | 6.16 ± 0.94 | −4.04 to −2.91 | 0.284 | 0.569 | <0.001 |
| Rotation left | 2.54 ± 1.64 | 6.19 ± 0.98 | −4.21 to −3.09 | 0.283 | 0.660 | <0.001 |
JPE = joint position error.
CI = confidence interval.
SEM = standard error mean.
MDC = minimal detectable change.
P-values are based on two-sample independent t-tests.
A linear regression coefficient was calculated to predict cervical JPE in different directions based on age. A significant regression was found for all the directions tested i.e. JPE in flexion (F (1, 229) = 238.04), P < 0.001 with an R2 of 0.51, JPE in extension (F (1, 229) = 432.51), P < 0.001 with an R2 of 0.65, JPE in side bending right (F (1, 229) = 345.02), P < 0.001 with an R2 of 0.59, JPE in side bending left (F (1, 229) = 574.63), P < 0.001 with an R2 of 0.71, JPE in rotation right (F (1, 229) = 595.75), P < 0.001 with an R2 of 0.72, JPE in rotation left (F (1, 229) = 568.80), P < 0.001 with an R2 of 0.71. Study showed JPE in flexion is = 0.24 + 0.08 (age) degrees, JPE in extension = −0.41 + 0.11 (age) degrees, JPE inside bending right = −0.03 + 0.07 (age) degrees, JPE inside bending left = −0.35 + 0.08 (age) degrees, JPE inside rotation right = −0.59 + 0.10 (age) degrees, JPE inside rotation left = −0.75 + 0.10 (age) degrees when age was measured in years. Subjects average JPE in increased 0.08 degrees (Flexion), 0.11 degrees (extension), 0.07 degrees (side bending right), 0.08 (side bending left), 0.10 degrees (rotation right and left) each year of age.
Discussion
This study demonstrates that cervical JPE is significantly correlated with age, with joint positioning becoming worse (JPE increases) with age. Subjects ⩾50 years of age show a significantly higher cervical JPE compared to subjects ⩽49 years.
To measure cervical JPE (proprioceptive ability), this study adopted the active movement angle reproduction test method. Previous studies in the literature used similar methods to measure proprioceptive sensitivity in clinical settings [15], [44], [45], [46] and are found to be reliable [47], [48]. Armstrong et al. conducted a pilot test to confirm reproducibility and reliability of head and neck movements for repeated position-matching tasks at various angles and found good reliability with high intraclass correlation coefficient (ICC) > 0.91 [48]. Lee et al. investigated the test–retest reliability of target head position tests in three cardinal planes. They found good to excellent reliability with ICC 0.72–0.90 [11].
Age-related changes in peripheral and central somatosensation are likely to increase JPE in older subjects. Research in peripheral joints (knee, hip, ankle, and the upper extremity) has shown that older adults typically have some degree of decreased peripheral proprioception compared to younger individuals [23], [24], [25], [27], [30], [31]. Established evidence for peripheral changes includes a reduced number and function of muscle spindles, joint receptors and cutaneous receptors [14], [31], [49]. Muscle spindles contribute significantly to sense of body position, and the present results likely indicate a decrease in muscle spindle number and function with age [31] because both the lengthened antagonists and the activated agonists contribute to position sense afferent information [50], [51]. Larger cervical JPE in multiple directions indicates a decrease in sensory function of multiple neck muscles [32], [50], [51]. In older subjects, age-related changes in the cervical spine, such as intervertebral disk degeneration, decreased strength of neck muscles, poor physical fitness or a sedentary lifestyle, can all lead to changes in the musculoskeletal system [51], [52] that might result in impaired target head reproduction tests in this study.
In this study there were positive correlations between cervical JPE and age in all three planes (sagittal – flexion and extension; frontal – side-bending right and left; and transverse – rotation right and left) evaluated. Teng et al. [22] show a positive correlation between cervical JPE in the sagittal plane (flexion and extension) and age, but found no correlation with age for JPE in the frontal or transverse planes. Teng et al. [22] used an ultrasound-based coordinate measuring system (CMS 70P, Zebris), while our study used a digital inclinometer for testing cervical JPE, and this may be responsible for differences in results. The methodological considerations for testing cervical JPE were also different, making comparisons between studies difficult. Our study findings are consistent with studies of weight-bearing joints (ankle, hip, knee, and lumbar spine), which find JPE is larger with increased age, and that movement threshold similarly changes with age [27], [32], [53], [54], [55].
Previous studies have discussed several ways in which proprioception (position sense) acuity may be compromised in older subjects. For example, it could be due to decreased attention, memory, and cognitive function in older versus younger subjects [56], [57]. JPE evaluation methods used in this study require short-term memory to accurately re-position to the target head position. Therefore, a larger JPE in older subjects might be attributable to diminished memory as well as cognitive or motor abilities. Neuroimaging studies conducted in older subjects have confirmed that decreased right-sided subcortical activity and structural changes (most notably, in the right putamen) may lead to increased JPE [56], [58]. Such structural and functional changes in both peripheral and central systems may have contributed to an increased JPE in older subjects in the current study.
The data of the current study show an age-related decline in cervical position sense as evaluated by JPE. Previous studies have shown that a decrease in position sense results in impaired postural control and balance and vice versa in elderly or injured individuals [55], [59]. Further studies are warranted to clarify how impaired cervical position sense might alter postural control in asymptomatic subjects and in subjects with different neck pathologies that affect somatosensation.
Limitations of the study
The cross-sectional study design adopted in this study limits the interpretation of the significant correlations found between age and cervical JPE. In the present study, all the old age subjects were independent, ambulatory and healthy, and thus the results of the research are not generalizable to older subjects with lower physical activity levels. This study recorded only absolute errors (JPE), including constant error and variable errors would have provided meaningful information regarding the direction and magnitude of errors in JPE tests.
Conclusions
Cervical JPE and age are significantly positively correlated, confirming that cervical joint position sense declines with age, as has been found for other joints. Older subjects have a significantly higher cervical JPE compared to younger subjects. Seeing this study results the therapists should consider the chance of showing higher cervical JPE in older subjects, and the assessment and rehabilitation goals should be considered different from younger subjects. This research provides further scope to evaluate the cervical JPE in different cervical pathologies and find how the cervical JPE would change with increasing age.
Conflict of Interest
The author has declared no conflict of interest.
Footnotes
Peer review under responsibility of Cairo University.
References
- 1.Abrahams V. The physiology of neck muscles; their role in head movement and maintenance of posture. Can J Physiol Pharmacol. 1977;55:332–338. doi: 10.1139/y77-047. [DOI] [PubMed] [Google Scholar]
- 2.Richmond F., Abrahams V. What are the proprioceptors of the neck? Prog Brain Res. 1978;50:245–254. doi: 10.1016/S0079-6123(08)60825-0. [DOI] [PubMed] [Google Scholar]
- 3.Goodwin G.M., McCloskey D.I., Matthews P.B. Proprioceptive illusions induced by muscle vibration: contribution by muscle spindles to perception? Science. 1972;175:1382–1384. doi: 10.1126/science.175.4028.1382. [DOI] [PubMed] [Google Scholar]
- 4.Riemann B.L., Lephart S.M. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37:80. [PMC free article] [PubMed] [Google Scholar]
- 5.Kalaska J.F. Central neural mechanisms of touch and proprioception. Can J Physiol Pharmacol. 1994;72:542–545. doi: 10.1139/y94-078. [DOI] [PubMed] [Google Scholar]
- 6.Proske U. Kinesthesia: the role of muscle receptors. Muscle Nerve. 2006;34:545–558. doi: 10.1002/mus.20627. [DOI] [PubMed] [Google Scholar]
- 7.Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13:2–11. doi: 10.1016/j.math.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Hillier S., Immink M., Thewlis D. Assessing proprioception a systematic review of possibilities. Neurorehabil Neural Repair. 2015;1545968315573055 doi: 10.1177/1545968315573055. [DOI] [PubMed] [Google Scholar]
- 9.Ageberg E., Flenhagen J., Ljung J. Test-retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord. 2007;8:1. doi: 10.1186/1471-2474-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knox J.J., Beilstein D.J., Charles S.D., Aarseth G.A., Rayar S., Treleaven J. Changes in head and neck position have a greater effect on elbow joint position sense in people with whiplash-associated disorders. Clin J Pain. 2006;22:512–518. doi: 10.1097/01.ajp.0000210997.53082.c9. [DOI] [PubMed] [Google Scholar]
- 11.Lee H.-Y., Teng C.-C., Chai H.-M., Wang S.-F. Test–retest reliability of cervicocephalic kinesthetic sensibility in three cardinal planes. Man Ther. 2006;11:61–68. doi: 10.1016/j.math.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Strimpakos N., Sakellari V., Gioftsos G., Kapreli E., Oldham J. Cervical joint position sense: an intra-and inter-examiner reliability study. Gait Posture. 2006;23:22–31. doi: 10.1016/j.gaitpost.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Röijezon U., Clark N.C., Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: basic science and principles of assessment and clinical interventions. Man Ther. 2015;20:368–377. doi: 10.1016/j.math.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Scott S., Loeb G. The computation of position sense from spindles in mono-and multiarticular muscles. J Neurosci. 1994;14:7529–7540. doi: 10.1523/JNEUROSCI.14-12-07529.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loudon J.K., Ruhl M., Field E. Ability to reproduce head position after whiplash injury. Spine. 1997;22:865–868. doi: 10.1097/00007632-199704150-00008. [DOI] [PubMed] [Google Scholar]
- 16.Heikkilä H.V., Wenngren B.I. Cervicocephalic kinesthetic sensibility active range of cervical motion and oculomotor function in patients with whiplash injury. Arch Phys Med Rehabil. 1998;79:1089–1094. doi: 10.1016/s0003-9993(98)90176-9. [DOI] [PubMed] [Google Scholar]
- 17.Heikkila H., Astrom P.-G. Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med. 1996;28:133–138. [PubMed] [Google Scholar]
- 18.Revel M., Andre-Deshays C., Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991;72:288–291. [PubMed] [Google Scholar]
- 19.Revel M., Minguet M., Gergoy P., Vaillant J., Manuel J.L. Changes in cervicocephalic kinesthesia after a proprioceptive. Arch Phys Med Rehabil. 1994;75 doi: 10.1016/0003-9993(94)90115-5. [DOI] [PubMed] [Google Scholar]
- 20.Villareal D.T., Chode S., Parimi N., Sinacore D.R., Hilton T., Armamento-Villareal R. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–1229. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kristjansson E., Dall'Alba P., Jull G. A study of five cervicocephalic relocation tests in three different subject groups. Clin Rehabil. 2003;17:768–774. doi: 10.1191/0269215503cr676oa. [DOI] [PubMed] [Google Scholar]
- 22.Teng C.-C., Chai H., Lai D.-M., Wang S.-F. Cervicocephalic kinesthetic sensibility in young and middle-aged adults with or without a history of mild neck pain. Man Ther. 2007;12:22–28. doi: 10.1016/j.math.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Wingert J.R., Welder C., Foo P. Age-related hip proprioception declines: effects on postural sway and dynamic balance. Arch Phys Med Rehabil. 2014;95:253–261. doi: 10.1016/j.apmr.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Barrack R.L., Skinner H.B., Cook S.D., Haddad R.J. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol. 1983;50:684–687. doi: 10.1152/jn.1983.50.3.684. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan F.S., Nixon J.E., Reitz M., Rindfleish L., Tucker J. Age-related changes in proprioception and sensation of joint position. Acta Orthop Scand. 1985;56:72–74. doi: 10.3109/17453678508992984. [DOI] [PubMed] [Google Scholar]
- 26.Petrella R., Lattanzio P., Nelson M. Effect of age and activity on knee joint proprioception1. Am J Phys Med Rehabil. 1997;76:235–241. doi: 10.1097/00002060-199705000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Robbins S., Waked E., McClaran J. Proprioception and stability: foot position awareness as a function of age and footware. Age Age. 1995;24:67–72. doi: 10.1093/ageing/24.1.67. [DOI] [PubMed] [Google Scholar]
- 28.Verschueren S., Brumagne S., Swinnen S., Cordo P. The effect of aging on dynamic position sense at the ankle. Behav Brain Res. 2002;136:593–603. doi: 10.1016/s0166-4328(02)00224-3. [DOI] [PubMed] [Google Scholar]
- 29.You S.H. Joint position sense in elderly fallers: a preliminary investigation of the validity and reliability of the SENSERite measure. Arch Phys Med Rehabil. 2005;86:346–352. doi: 10.1016/j.apmr.2004.01.035. [DOI] [PubMed] [Google Scholar]
- 30.Adamo D.E., Martin B.J., Brown S.H. Age-related differences in upper limb proprioceptive acuity 1, 2. Percept Mot Skills. 2007;104:1297–1309. doi: 10.2466/pms.104.4.1297-1309. [DOI] [PubMed] [Google Scholar]
- 31.Kalisch T., Kattenstroth J.-C., Kowalewski R., Tegenthoff M., Dinse H.R. Age-related changes in the joint position sense of the human hand. Clin Interv Aging. 2012;7:499–507. doi: 10.2147/CIA.S37573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilsing M., Van den Bosch C., Lee S., Ashton-Miler J., Alexander N., Schultz A. Association of age with the threshold for detecting ankle inversion and eversion in upright stance. Age Age. 1995;24:58–66. doi: 10.1093/ageing/24.1.58. [DOI] [PubMed] [Google Scholar]
- 33.Han J.T., Lee J.-H. Effects of kinesiology taping on repositioning error of the knee joint after quadriceps musclefatigue. J Phys Ther Sci. 2014;26:921–923. doi: 10.1589/jpts.26.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pinsault N., Vuillerme N. Degradation of cervical joint position sense following muscular fatigue in humans. Spine. 2010;35:294–297. doi: 10.1097/BRS.0b013e3181b0c889. [DOI] [PubMed] [Google Scholar]
- 35.Heikkila H.V., Wenngren B.I. Cervicocephalic kinesthetic sensibility, active range of cervical motion, and oculomotor function in patients with whiplash injury. Arch Phys Med Rehabil. 1998;79:1089–1094. doi: 10.1016/s0003-9993(98)90176-9. [DOI] [PubMed] [Google Scholar]
- 36.Li Z., Durgin F.H. Design, data, and theory regarding a digital hand inclinometer: a portable device for studying slant perception. Behav Res Methods. 2011;43:363–371. doi: 10.3758/s13428-010-0047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bao H.P., Hu Y.X., Lv M., Zhang J. Trans Tech Publ; 2013. Design and implementation based on ADXL213 of the digital inclinometer. Applied mechanics and materials. [p. 400–6] [Google Scholar]
- 38.Nitschke J.E., Nattrass C.L., Disler P.B., Chou M.J., Ooi K.T. Reliability of the American Medical Association Guides’ model for measuring spinal range of motion: its implication for whole-person impairment rating. Spine. 1999;24:262–268. doi: 10.1097/00007632-199902010-00013. [DOI] [PubMed] [Google Scholar]
- 39.Santos C.M.d., Ferreira G., Malacco P.L., Sabino G.S., Moraes G.F.d.S., Felício D.C. Intra and inter examiner reliability and measurement error of goniometer and digital inclinometer use. Rev Bras Med Esporte. 2012;18:38–41. [Google Scholar]
- 40.Tousignant M., Boucher N., Bourbonnais J., Gravelle T., Quesnel M., Brosseau L. Intratester and intertester reliability of the Cybex electronic digital inclinometer (EDI-320) for measurement of active neck flexion and extension in healthy subjects. Man Ther. 2001;6:235–241. doi: 10.1054/math.2001.0419. [DOI] [PubMed] [Google Scholar]
- 41.Schutz R. Absolute, constant, and variable error: problems and solutions. In: Proceedings of the Colorado measurement symposium: University of Colorado Boulder, CO; 1977. p. 82–100.
- 42.Ries J.D., Echternach J.L., Nof L., Blodgett M.G. Test-retest reliability and minimal detectable change scores for the timed “up & go” test, the six-minute walk test, and gait speed in people with Alzheimer disease. Phys Ther. 2009;89:569–579. doi: 10.2522/ptj.20080258. [DOI] [PubMed] [Google Scholar]
- 43.Stratford P.W. Getting more from the literature: estimating the standard error of measurement from reliability studies. Physiother Can. 2004;56:27–30. [Google Scholar]
- 44.Dover G., Powers M.E. Reliability of joint position sense and force-reproduction measures during internal and external rotation of the shoulder. J Athl Train. 2003;38:304. [PMC free article] [PubMed] [Google Scholar]
- 45.Heikkilä H., Aström P. Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med. 1996;28:133–138. [PubMed] [Google Scholar]
- 46.Palmgren P.J., Sandström P.J., Lundqvist F.J., Heikkilä H. Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. J Manipulative Physiol Ther. 2006;29:100–106. doi: 10.1016/j.jmpt.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 47.Pinsault N., Fleury A., Virone G., Bouvier B., Vaillant J., Vuillerme N. Test-retest reliability of cervicocephalic relocation test to neutral head position. Physiother Theory Pract. 2008;24:380–391. doi: 10.1080/09593980701884824. [DOI] [PubMed] [Google Scholar]
- 48.Armstrong B.S., McNair P.J., Williams M. Head and neck position sense in whiplash patients and healthy individuals and the effect of the cranio-cervical flexion action. Clin Biomech. 2005;20:675–684. doi: 10.1016/j.clinbiomech.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 49.Kulkarni V., Chandy M., Babu K. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001;49:355. [PubMed] [Google Scholar]
- 50.Inglis J., Frank J. The effect of agonist/antagonist muscle vibration on human position sense. Exp Brain Res. 1990;81:573–580. doi: 10.1007/BF02423506. [DOI] [PubMed] [Google Scholar]
- 51.Reddy R.S., Maiya G., Rao S.K. Proprioceptive reposition errors in subjects with cervical spondylosis. Int J Health Sci Res. 2012;1:65–73. [Google Scholar]
- 52.Waters R., Sie I., Adkins R. Aging with a Spinal Cord Injury Demos Publications New York; NY: 1993. The musculoskeletal system. [p. 53–71] [Google Scholar]
- 53.Gill K.P., Callaghan M.J. The measurement of lumbar proprioception in individuals with and without low back pain. Spine. 1998;23:371–377. doi: 10.1097/00007632-199802010-00017. [DOI] [PubMed] [Google Scholar]
- 54.Parkhurst T.M., Burnett C.N. Injury and proprioception in the lower back. J Orthop Sports Phys Ther. 1994;19:282–295. doi: 10.2519/jospt.1994.19.5.282. [DOI] [PubMed] [Google Scholar]
- 55.Taimela S., Kankaanpää M., Luoto S. The effect of lumbar fatigue on the ability to sense a change in lumbar position: a controlled study. Spine. 1999;24:1322. doi: 10.1097/00007632-199907010-00009. [DOI] [PubMed] [Google Scholar]
- 56.Doumas M., Krampe R.T. Adaptation and reintegration of proprioceptive information in young and older adults’ postural control. J Neurophysiol. 2010;104:1969–1977. doi: 10.1152/jn.00345.2010. [DOI] [PubMed] [Google Scholar]
- 57.Goble D.J., Mousigian M.A., Brown S.H. Compromised encoding of proprioceptively determined joint angles in older adults: the role of working memory and attentional load. Exp Brain Res. 2012;216:35–40. doi: 10.1007/s00221-011-2904-8. [DOI] [PubMed] [Google Scholar]
- 58.Goble D.J., Coxon J.P., Van Impe A., Geurts M., Van Hecke W., Sunaert S. The neural basis of central proprioceptive processing in older versus younger adults: an important sensory role for right putamen. Hum Brain Mapp. 2012;33:895–908. doi: 10.1002/hbm.21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lord S.R., Clark R.D., Webster I.W. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46:M69–M76. doi: 10.1093/geronj/46.3.m69. [DOI] [PubMed] [Google Scholar]