Abstract
Background:
Ultrasound-guided transversus abdominis plane (TAP) block has recently come up as a modality to take care of postoperative pain. It can somewhat avoid the use of intravenous opioid analgesics and hence to avoid its complications. We have performed a prospective, double-blinded, randomized study to assess the analgesic effect of adding dexmedetomidine to local ropivacaine on TAP block for patients undergoing lower abdominal surgeries.
Aim:
The aim is to assess whether addition of dexmedetomidine to ropivacaine may bring some improvements to the analgesic efficacy of TAP blocks in patients undergoing lower abdominal surgeries.
Materials and Methods:
The study was conducted on forty patients undergoing lower abdominal surgeries under general anesthesia. The patients were divided into two groups: one receiving plain ropivacaine (Group 1) and other receiving ropivacaine with dexmedetomidine (Group 2) during TAP block. The patients in the two groups were compared for age, sex, body mass index, incidence of postoperative nausea, and vomiting and pain as measured on visual analog scale (VAS).
Results:
There was significantly lower pain score on VAS at 1, 3, 6, 12, and 18 h in Group 2 than in Group 1.
Conclusion:
The addition of dexmedetomidine to ropivacaine during TAP block improves analgesic effect of TAP block and prolongs the duration of analgesia as well.
Key words: Dexmedetomidine, ropivacaine, transversus abdominis plane block, ultrasound
Introduction
Ultrasound-guided transversus abdominis plane (TAP) block has recently come up as a modality to take care of postoperative pain. It can somewhat avoid the use of intravenous opioid analgesics and hence to avoid its complications.[1] The studies have shown that TAP block provides significant analgesic effect, especially below T10 up to L1 level; hence, it is perfectly suited for use after lower abdominal and gynecological surgeries.[1] The performance of procedure under ultrasound guidance improves the outcome because of better localization of the plane for blockade. Prolonged analgesic effect can be achieved by continuous blockade using catheter for drug delivery.
Although most of the available studies on TAP block have used local anesthetic (LA) agent, few studies have reported that the adjuvant medications were added to LA to prolong the effect of TAP block.[2] Dexmedetomidine is a selective alpha 2 adrenergic agonist, with both analgesic and sedative properties.[3] The use of LA agents with dexmedetomidine epidurally or intrathecally associated with prolongation of the LA effect.[4,5,6,7,8] We have performed a prospective, double-blinded, randomized study to assess the analgesic effect of adding dexmedetomidine to local ropivacaine on TAP block for patients undergoing lower abdominal surgeries.
Aims
The aim of this study was to assess whether addition of dexmedetomidine to ropivacaine may bring some improvement to the analgesic efficacy of TAP block in patients undergoing lower abdominal surgeries.
Materials and Methods
The study was conducted in the Department of General Surgery and Anesthesiology, UP Rural Institute of Medical Sciences and Research, Saifai, Etawah (UP), India. After approval from the Ethical Committee of our institution, written informed consent was obtained from forty patients of the American Society of Anesthesiologists Physical Class I or II patients and scheduled for lower abdominal surgeries such as appendectomy, repair of incisional hernia, and abdominal hysterectomy. Exclusion criteria were patient's refusal, patients with a history of cardiac, respiratory, renal or hepatic disease, local infection at the site of block, psychological disorders, allergy to study medications, coagulation disorders, and any other contraindication for general anesthesia.
During the preoperative anesthetic assessment of patients, visual analog scale (VAS) for pain assessment from 0 to 10 cm with 0 refers no pain and 10 refers the worst pain imaginable was explained to patients. The patients were monitored by noninvasive blood pressure, heart rate, pulse oximetry, temperature, and electrocardiography. General anesthesia with endotracheal intubation was standardized for all patients in the both groups. All surgical interventions were performed by the same surgical team. The patients were randomly divided into two groups. In Group R (n = 20), patients received TAP block on each side using 22 ml of study medication which consisted of 20 ml of ropivacaine 0.2% and 2 ml of normal saline. However, Group RD (n = 20) patients received TAP block on each side with 22 ml, in which dexmedetomidine 0.5 mcg/kg was dissolved in 2 ml of normal saline and added to 20 ml of ropivacaine 0.2%.
Following skin preparation, TAP blocks were performed by one of the investigators under dynamic ultrasound guidance (MTurbo, Sonosite Inc., Bothell, WA, USA). Broadband linear array ultrasound probe was placed in the axial plane across the midaxillary line midway between costal margin and iliac crest. Following identification of the three different layers of the abdominal wall, 22-gauge insulated nerve block needle was inserted in plane until its tip was located in between the internal oblique and transverse abdominal muscles. After careful aspiration injection of the study, medication was performed and hypoechoic layer was detected on ultrasound.
After completion of the surgical procedure and reversal from anesthesia, patients were transferred to the postanesthesia care unit (PACU). An observer who was unaware of the study protocol recorded the pain score on VAS. Intravenous tramadol was given as rescue analgesia for postoperative pain relief if pain score >4 or when it was requested by the patients; the time to first dose of rescue analgesic given was recorded and worst pain score was also noted. In PACU and the first 24 h postoperatively, VAS will be recorded at 1, 3, 6, 12, and 18 h postoperatively.
Statistical analysis
Statistical analysis was done using SPSS software version 16.0 (IBM). For categorical variables, Chi-square test was done. For comparing two groups of mean, independent Student's t-test was used. P < 0.05 is considered statistical significance.
Observation and Results
The study included total forty patients undergoing lower abdominal surgeries under general anesthesia and received TAP block for postoperative analgesia, who were randomly assigned into two groups. Group 1 received only ropivacaine for TAP block while Group 2 received ropivacaine with dexmedetomidine.
Table 1 shows comparison of various parameters between the two groups. The mean age of the patients in Group 1 was 43.80 ± 12.10 years while in Group 2 was 42.60 ± 10.67 years. This was not significant having P = 0.741. Group 1 comprised 7 males and 13 females while Group 2 consisted of 6 males and 14 females, and the difference was again not significant statistically (P = 0.736). The mean body mass index in Group 1 was 29.03 ± 5.92 kg/m2 while in Group 2 was 26.87 ± 5.94 kg/m2. This difference was again not significant statistically (P = 0.257). The incidence of postoperative nausea and vomiting in Group 1 was found in 7 out of 20 patients while in 4 out of 20 patients of Group 2 and again this difference was not significant (P = 0.288).
Table 1.
Comparison of various parameters between the two groups
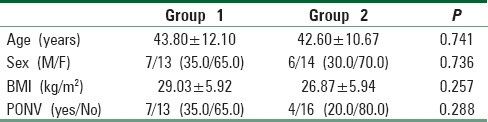
Table 2 shows the mean of pain score measured on visual analog score in Groups 1 and 2 at 1, 3, 6, 12, and 18 h postoperatively.
Table 2.
Pain score measured on visual analogue score
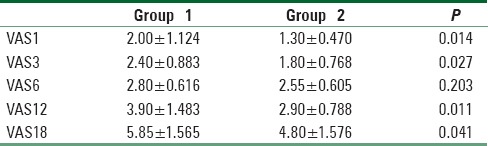
It was found that mean of VAS scores in Group 1 was 2.00 ± 1.124, 2.40 ± 0.883, 2.80 ± 0.616, 3.90 ± 1.483, and 5.85 ± 1.565 at 1, 3, 6, 12, and 18 h, respectively. Whereas in Group 2, mean of VAS scores at 1, 3, 6, 12, and 18 h was 1.30 ± 0.470, 1.80 ± 0.768, 2.55 ± 0.605, 2.90 ± 0.788, and 4.80 ± 1.576, respectively. On analysis, we found that pain scores in Group 2 were significantly lower than pain scores in Group 1 at 1 h (P = 0.014), 3 h (0.027), 12 h (0.011), and 18 h (0.041). Although the pain scores in Group 1 were higher than that in Group 2 at 6 h as well, the difference was not statistically significant (P = 0.203).
Discussion
The management of postoperative pain is an important issue. The uncontrolled postoperative pain is the major limiting factor for early ambulation and thereby puts patient to the increased risk of various complications as well. The desirable properties of an analgesic agent are that it provides safe and effective analgesia, with minimal side effects. The multimodal pain management is the answer of this. The TAP block is used for postoperative analgesia following abdominal surgeries. It provides blockade of the nociceptive inputs from the abdominal wall but not from the abdominal organs. Therefore, the block is used as a part of multimodal approach.
Ranjit et al. in the study of comparison of ultrasound-guided TAP block versus local wound infiltration for postoperative analgesia in patients undergoing gynecological surgery under general anesthesia found that bilateral TAP block was effective in reducing postoperative pain scores for 8–12 h postoperatively. This block was also successful in reducing postoperative opioid requirement.[9]
Yu et al. conducted a study titled, “TAP block versus LA wound infiltration in lower abdominal surgery: A systematic review and meta-analysis of randomized controlled trials.” They found that TAP block and LA infiltration provide comparable short-term postoperative analgesia, but TAP block has better long-lasting effect, especially up to 24 h after surgery.[10]
Another study by Mishra et al. comparing TAP block versus wound infiltration of local anesthesia for postoperative analgesia concluded that TAP block and wound infiltration of local anesthesia both provide significant postoperative analgesia initially but the effects are more long-lasting in TAP block.[11]
Therefore, we can presume that the potent prolonged analgesic effects of TAP block remain the issue beyond doubt. Now, the next issue of concern can be that how we can prolong the analgesic effects of TAP block even further. The current studies were performed on patients undergoing lower abdominal surgeries under general anesthesia and were offered ultrasound-guided TAP block for postoperative analgesia. One study group received only ropivacaine for TAP block while other group received ropivacaine with dexmedetomidine for TAP block. The results of this study showed that the group receiving combination of ropivacaine and dexmedetomidine has significantly lower pain scores postoperatively that the group receiving only ropivacaine.
In the study by Rai et al., it was found that the addition of dexmedetomidine to ropivacaine in TAP block led to further prolongation of analgesia, less requirement of rescue analgesia, and lower VAS pain scores.[12] The study done by Marhofer et al. found that there was prolongation of ulnar nerve block duration after addition of dexmedetomidine in ropivacaine used for the block by approximately 60%.[13] Almarakbi andKaki reported that the addition of dexmedetomidine to bupivacaine in TAP block in patients undergoing abdominal hysterectomy provides better pain control postoperatively.[14]
The major limitation of this study is the small sample size which may or may not be the representative population.
Conclusion
The addition of dexmedetomidine to local anesthesia during TAP block tends to increase the analgesic effect as well as prolongs the duration of analgesia achieved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mishra M, Mishra SP. Transversus abdominis plane block: The new horizon for postoperative analgesia following abdominal surgery. Egypt J Anaesth. 2016;32:243–7. [doi.org/10.1016/j.egja. 2015.12.003] [Google Scholar]
- 2.Sivapurapu V, Vasudevan A, Gupta S, Badhe AS. Comparison of analgesic efficacy of transversus abdominis plane block with direct infiltration of local anesthetic into surgical incision in lower abdominal gynecological surgeries. J Anaesthesiol Clin Pharmacol. 2013;29:71–5. doi: 10.4103/0970-9185.105807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belavy D, Cowlishaw PJ, Howes M, Phillips F. Ultrasound-guided transversus abdominis plane block for analgesia after caesarean delivery. Br J Anaesth. 2009;103:726–30. doi: 10.1093/bja/aep235. [DOI] [PubMed] [Google Scholar]
- 4.Skjelsager A, Ruhnau B, Kistorp TK, Kridina I, Hvarness H, Mathiesen O, et al. Transversus abdominis plane block or subcutaneous wound infiltration after open radical prostatectomy: A randomized study. Acta Anaesthesiol Scand. 2013;57:502–8. doi: 10.1111/aas.12080. [DOI] [PubMed] [Google Scholar]
- 5.Araco A, Pooney J, Araco F, Gravante G. Transversus abdominis plane block reduces the analgesic requirements after abdominoplasty with flank liposuction. Ann Plast Surg. 2010;65:385–8. doi: 10.1097/SAP.0b013e3181cc2a24. [DOI] [PubMed] [Google Scholar]
- 6.Sforza M, Andjelkov K, Zaccheddu R, Nagi H, Colic M. Transversus abdominis plane block anesthesia in abdominoplasties. Plast Reconstr Surg. 2011;128:529–35. doi: 10.1097/PRS.0b013e31821e6f51. [DOI] [PubMed] [Google Scholar]
- 7.Sahin L, Sahin M, Gul R, Saricicek V, Isikay N. Ultrasound-guided transversus abdominis plane block in children: A randomised comparison with wound infiltration. Eur J Anaesthesiol. 2013;30:409–14. doi: 10.1097/EJA.0b013e32835d2fcb. [DOI] [PubMed] [Google Scholar]
- 8.Sandeman DJ, Bennett M, Dilley AV, Perczuk A, Lim S, Kelly KJ. Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: A prospective randomized trial. Br J Anaesth. 2011;106:882–6. doi: 10.1093/bja/aer069. [DOI] [PubMed] [Google Scholar]
- 9.Ranjit S, Shrestha SK. Comparison of ultrasound guided transversus abdominis plane block versus local wound infiltration for post operative analgesia in patients undergoing gynaecological surgery under general anaesthesia. Kathmandu Univ Med J (KUMJ) 2014;12:93–6. doi: 10.3126/kumj.v12i2.13652. [DOI] [PubMed] [Google Scholar]
- 10.Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014;14:121. doi: 10.1186/1471-2253-14-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra M, Mishra SP, Singh SP. Transversus abdominis plane block versus wound infiltration of local anesthesia for post operative analgesia. J Med Sci Clin Res. 2016;4:9916–22. [Google Scholar]
- 12.Rai P, Singh D, Singh SK, Malviya D, Bagwans MC. Effect of addition of dexmedetomidine to ropivacaine in transversus abdominis plane block on postoperative pain in lower segment caesarean section: A randomized controlled trial. J Dent Med Sci. 2016;15:122–5. [Google Scholar]
- 13.Marhofer D, Kettner SC, Marhofer P, Pils S, Weber M, Zeitlinger M. Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: A volunteer study. Br J Anaesth. 2013;110:438–42. doi: 10.1093/bja/aes400. [DOI] [PubMed] [Google Scholar]
- 14.Almarakbi WA, Kaki AM. Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates post-operative pain relief among abdominal hysterectomy patients: A prospective randomized controlled trial. Saudi J Anaesth. 2014;8:161–6. doi: 10.4103/1658-354X.130683. [DOI] [PMC free article] [PubMed] [Google Scholar]


