Abstract
Association of dengue fever with transverse myelitis in the form of extensive spinal cord involvement is a rare entity described in the literature. We describe a middle-aged man who presented with dengue fever and in whom weakness of the bilateral lower limbs and urinary incontinence developed on the third day of fever. Magnetic resonance imaging confirmed the diagnosis of longitudinally extensive transverse myelitis. Over a four-week course of corticosteroids with supportive management, the patient recovered without any residual neurologic deficit.
INTRODUCTION
Dengue virus is a cause of widespread morbidity and mortality in the tropical and subtropical areas of India, with 47,209 cases and 242 deaths reported in 2012 from the government hospital sector in India alone.1 Of the 4 strains of dengue virus implicated in the disease, DEN1, DEN2, and DEN3 are the prominent serotypes in India. DEN2 has been reported in more than 75% of the cases in breakouts since 2010.2,3 Although the first recognized epidemics of dengue fever were known as early as the 1780s, the neurotropic effects came to light only 2 decades ago. Neurologic involvement owing to direct central nervous system involvement of the virus during the acute phase leads to encephalitis, meningitis, and myelitis.4 The postinfection phase may be associated with acute disseminated encephalomyelitis, neuromyelitis optica, optic neuritis, Guillain-Barré syndrome, myelitis, oculomotor palsy, phrenic neuropathy, and chronic fatigue syndrome, with encephalitis being the most common. Involvement of the spinal cord appears to be rare and occurs mostly in the form of transverse myelitis. Spinal cord involvement in the form of longitudinally extensive transverse myelitis (LETM) has been described only once in the literature to our knowledge.5
We report a case of LETM in a previously healthy middle-aged man presenting with dengue fever associated with bilateral lower limb weakness and urinary incontinence. The patient responded to corticosteroids and eventually had complete neurologic recovery.
CASE SUMMARY
A 42-year-old man, a resident of an ongoing dengue outbreak area, presented with 4 days of fever and 1 day of bilateral lower limb weakness to the Emergency Department of Guru Teg Bahadur Hospital in Delhi, India. The fever was high grade with chills, myalgia, arthralgia, headache, and petechial rash. Bilateral lower limb weakness that had developed 3 days after the onset of fever was associated with urinary retention. The motor weakness was associated with sensory impairment in the lower limbs extending to the level of the umbilicus. However, there was no associated bowel involvement. There was no history of bleeding tendency, recent vaccination, or unusual medical history. The patient was admitted to the hospital.
Results of the general examination were unremarkable except for hyperthermia (temperature = 38.9°C [102°F]) and multiple petechiae all over the body. Neurologic findings revealed flaccid paralysis of bilateral lower limbs with hypotonia and muscle strength of 2/5 at the hip, knee, ankle flexors, and extensors. Deep tendon reflexes were absent, and Babinski sign was positive. Abdominal reflexes were absent. The level of sensory deficit extended upward until the umbilicus, corresponding to T10. Neurologic examination of the upper limbs and the cranial nerves were normal.
Initial laboratory investigations revealed a hemoglobin level of 10.2 g/dL, leukopenia (leukocytes = 3 × 103/µL), and thrombocytopenia (platelets = 18 × 103/µL).
The platelet count increased during the hospital stay, without the need for transfusion. Results of the NS1 (non-structural protein 1) antigen test and the immunoglobulin M antibody test detected using a single-step immunochromatographic assay were positive for dengue. Cerebrospinal fluid analysis could not be carried out because the patient did not consent to a lumbar puncture. Table 1 denotes the laboratory investigations of the patient at hospital admission and at discharge. Magnetic resonance imaging of the spine revealed continuous intramedullary T2 hyperintense signal intensity in the long segment of the dorsal cord extending from T5 to the conus medullaris and from the C2 to C4 level of the cervical spinal cord (Figure 1). Magnetic resonance imaging of the brain revealed unusual mild diffuse cerebral atrophy.
Table 1.
Laboratory values at admission and discharge
| Investigation | At admission | At discharge |
|---|---|---|
| Hemoglobin (g/dL) | 10.2 | 12.5 |
| Total leukocyte count (103/µL) | 3 | 3.4 |
| Platelet count (103/µL) | 18 | 265 |
| Blood glucose (mg/dL) | 103 | NA |
| Serum sodium (mEq/L) | 137 | 134 |
| Serum potassium (mEq/L) | 4.7 | 4.1 |
| Serum calcium (mEq/L) | 7.3 | 8.4 |
NA = unable to find a documented value in the records.
Figure 1.
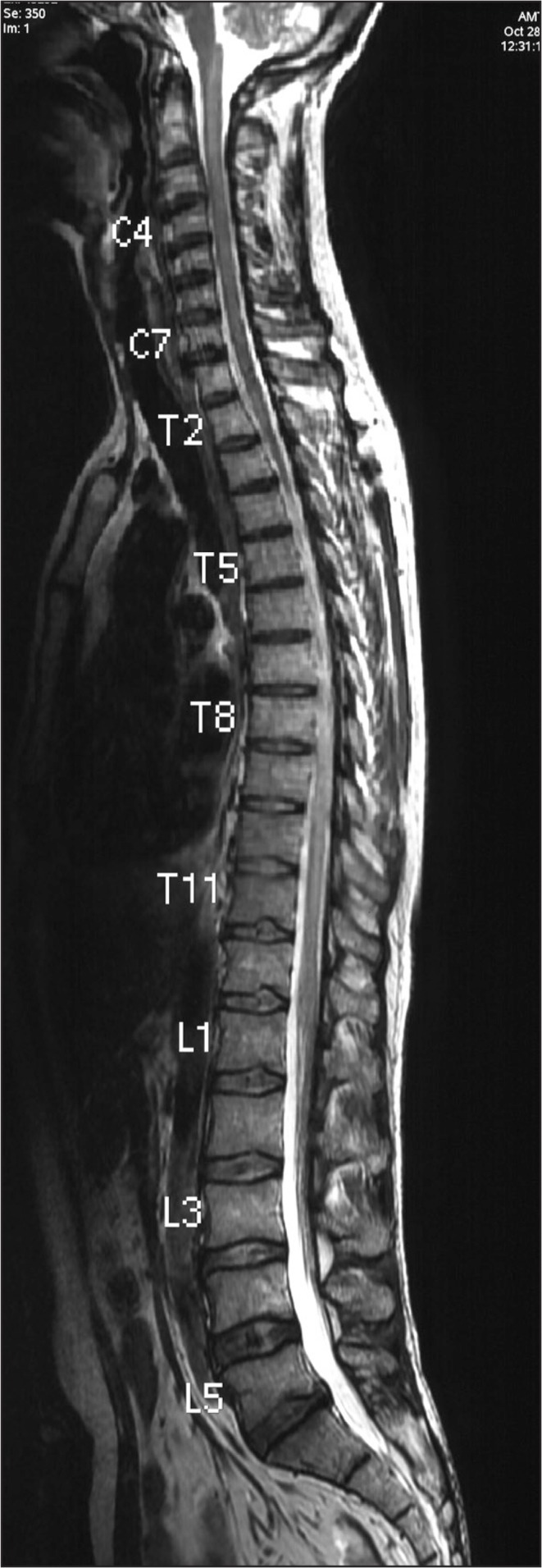
Magnetic resonance image of spinal cord. Continuous intramedullary T2 hyperintense signal intensity in the long segment of the dorsal cord extending from T5 to the conus medullaris and from the C2 to C4 level of the cervical cord.
The patient was treated with supportive management and intravenous pulse therapy with methylprednisolone at a dosage of 1 g/day for 3 days and then was shifted to a regimen of oral prednisolone. The oral prednisolone dosage was started at 40 mg/day and then was tapered gradually over 4 weeks. The patient’s bladder was catheterized for the first 3 weeks, and then the catheter was removed after intermittent clamping and bladder training. Rehabilitation physical therapy exercises were done simultaneously with medical treatment.
The weakness dramatically improved with corticosteroids, and the patient was able to walk by the third week of treatment. He was discharged after 27 days of inpatient treatment, with no residual neurologic deficits.
DISCUSSION
Neurologic manifestations associated with dengue fever received little attention initially, but in the last 20 years there has been increasing recognition of their possible importance. After a thorough search of the literature, we found only 5 case reports of dengue illness associated with spinal cord involvement in the form of transverse myelitis. The association between dengue infection and LETM has been described only once in the literature to our knowledge.5
Our patient had typical features of dengue fever with a clinical history, rash, thrombocytopenia, leukopenia, and positive NS1 antigen and immunoglobulin M serologic findings for dengue virus. With all these features and the lack of any other important physical findings, LETM in this patient was probably the result of active dengue infection. The patient responded dramatically to corticosteroid treatment, and the neurologic deficit recovered fully by 3 weeks.
In our patient, myelitis developed in the acute parainfectious phase of dengue illness, similar to earlier case reports.5–8 There is only a single case report of myelitis in the postinfectious phase, occurring 16 days after the onset of illness.9 The pathogenesis of myelitis in our case is likely direct spinal neuronal involvement of the dengue virus, but the exact mechanism is not clear. It has been shown that dengue virus can lead to involvement of the spinal cord by direct invasion of the cord or by active replication within the spinal cord.10 It was also postulated that acute parainfectious dengue infection presents with flaccid paralysis, whereas late-stage (postinfectious) dengue infection presents with spastic weakness, and our case had similar findings of flaccid paralysis.10 Usually, LETM is associated with a poor prognosis; however, our patient showed a dramatic improvement in neurologic deficit after treatment with corticosteroids.5 Contrary to the case previously reported by Larik et al,5 in which the patient showed improvement only after treatment with antivirals and intravenous immunoglobulins, our patient recovered with corticosteroids (similar to the case by Seet et al9) and other supportive treatment in the form of physical therapy.
We were unable to determine the strain of dengue in our patient, and a review of the previous case report on LETM5 failed to reveal the strain implicated in that case. However, it would be interesting to know the epidemiology for future such cases.
CONCLUSION
Even though transverse myelitis is a rare neurologic manifestation of dengue infection, manifesting mostly during parainfectious phases and sometimes after the infection has resolved, it is important that clinicians are aware of this entity. It is vital that clinicians look for dengue virus as a cause of transverse myelitis or other inflammatory neurologic manifestations in patients presenting with typical dengue fever symptoms and living in or visiting dengue-endemic areas.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Chaudhuri M. What can India do about dengue fever? BMJ. 2013 Feb 4;346:f643. doi: 10.1136/bmj.f643. DOI: http://dx.doi.org/10.1136/bmj.f643. [DOI] [PubMed] [Google Scholar]
- 2.Mishra G, Jain A, Prakash O, et al. Molecular characterization of dengue viruses circulating during 2009–2012 in Uttar Pradesh, India. J Med Virol. 2015 Jan;87(1):68–75. doi: 10.1002/jmv.23981. DOI: http://dx.doi.org/10.1002/jmv.23981. [DOI] [PubMed] [Google Scholar]
- 3.Afreen N, Deeba F, Naqvi I, et al. Molecular investigation of 2013 dengue fever outbreak from Delhi, India. PLoS Curr. 2014 Sep;2:6. doi: 10.1371/currents.outbreaks.0411252a8b82aa933f6540abb54a855f. DOI: http://dx.doi.org/10.1371/currents.outbreaks.0411252a8b82aa933f6540abb54a855f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murthy JM. Neurological complication of dengue infection. Neurol India. 2010 Jul-Aug;58(4):581–4. doi: 10.4103/0028-3886.68654. DOI: http://dx.doi.org/10.4103/0028-3886.68654. [DOI] [PubMed] [Google Scholar]
- 5.Larik A, Chiong Y, Lee LC, Ng YS. Longitudinally extensive transverse myelitis associated with dengue fever. BMJ Case Rep. 2012 May;11:2012. doi: 10.1136/bcr.12.2011.5378. DOI: http://dx.doi.org/10.1136/bcr.12.2011.5378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leão RN, Oikawa T, Rosa ES, et al. Isolation of dengue 2 virus from a patient with central nervous system involvement (transverse myelitis) Rev Soc Bras Med Trop. 2002 Jul-Aug;35(4):401–4. doi: 10.1590/s0037-86822002000400018. DOI: http://dx.doi.org/10.1590/S0037-86822002000400018. [DOI] [PubMed] [Google Scholar]
- 7.Kunishige M, Mitsui T, Tan BH, et al. Preferential gray matter involvement in dengue myelitis. Neurology. 2004 Nov 23;63(10):1980–1. doi: 10.1212/01.wnl.0000144194.29643.d0. DOI: http://dx.doi.org/10.1212/01.WNL.0000144194.29643.D0. [DOI] [PubMed] [Google Scholar]
- 8.Renganathan A, Keong W, Tin Tan C. Transverse myelitis in association with dengue infection. Neurol Asia. 1996;1(1):61–3. [Google Scholar]
- 9.Seet RC, Lim EC, Wilder-Smith EP. Acute transverse myelitis following dengue virus infection. J Clin Virol. 2006 Mar;35(3):310–2. doi: 10.1016/j.jcv.2005.08.006. DOI: http://dx.doi.org/10.1016/j.jcv.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 10.An J, Zhou DS, Kawasaki K, Yasui K. The pathogenesis of spinal cord involvement in dengue virus infection. Virchows Arch. 2003 May;442(5):472–81. doi: 10.1007/s00428-003-0785-3. DOI: http://dx.doi.org/10.1007/s00428-003-0785-3. [DOI] [PubMed] [Google Scholar]


