Abstract
Objective
To determine the impact of pediatric hearing loss on quality of life (QOL).
Data Sources
A qualified medical librarian conducted a literature search for relevant publications that evaluate QOL in school-aged children with hearing loss (HL).
Review Methods
Studies were assessed independently by two reviewers for inclusion in the systematic review and meta-analysis.
Results
From 979 abstracts, 69 were identified as relevant; ultimately 41 articles were included in the systematic review. This review revealed that children with HL generally report a lower QOL than their normal hearing peers, and QOL improves after interventions. The extent of these differences is variable among studies, and depends on the QOL measure. Four studies using the Pediatric Quality of Life Inventory (PedsQL) had sufficient data for inclusion in a meta-analysis. After pooling studies, statistically and clinically significant differences in PedsQL scores were found between children with normal hearing and those with HL, specifically in the Social and School domains. Statistically significant differences were also noted in in total scores for children with unilateral HL and in the physical domain for children with bilateral HL as compared to normal hearing, however these differences were not clinically meaningful.
Conclusions
Our analysis reveals that decreased QOL in children with HL is detected in distinct domains of the PedsQL questionnaire. These domains of school functioning and social interactions are especially important for development and learning. Future work should focus on these specific aspects of QOL when assessing HL in the pediatric population.
Keywords: quality of life, pediatric hearing loss
INTRODUCTION
Hearing impairment is common among children and adolescents in the United States. A recent systematic review reported the incidence of neonatal hearing loss in the US to be 1.1 per 1000 infants and the average prevalence of mild or worse unilateral or bilateral hearing impairment in children and adolescents to be over 3%.1 Hearing impairment puts children at a clear disadvantage. In addition to being 21–39% less likely to attend college, persons with hearing loss experience twice as much work stress and have lower labor participation rates than normal hearing individuals.2 While it is clear that hearing loss is disabling in some ways, the true effect on quality of life remains unknown.
The World Health Organization defines quality of life (QOL) as individuals’ perception of their position in life in the context of culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.3 The definition encompasses six domains of quality of life including a physical domain, psychological domain, level of independence, social relationships, environment, and spirituality/religion/personal beliefs. There are multiple QOL assessment tools that have been used to evaluate pediatric hearing impairment, however few were designed to specifically address this common problem. Additionally, no single tool is routinely used to report quality of life in children with hearing loss, resulting in variability and inconsistencies between studies reporting outcomes in these patients. While some prior studies have suggested decreased quality of life in pediatric patients with hearing loss, others have shown similar findings in children with hearing impairment as compared to those with normal hearing. The true effect of unilateral and bilateral hearing loss on QOL in children remains unclear.
The objective of this study was to assess the impact of pediatric hearing loss on quality of life by reviewing available studies on this topic. We hypothesized that quality of life was negatively affected in children diagnosed with hearing loss as compared to their normal hearing peers. A secondary objective was to evaluate the expected improvement in quality of life after intervention.
METHODS
The PRISMA guidelines were consulted and all requirements have been met for this study.4 The published literature was searched using strategies created by a medical librarian for the concepts of “quality of life,” “hearing loss” and “children.” Abstracts that involved ongoing temporary or fluctuating conductive HL, such as that due to otitis media, were excluded, as were studies involving children with cognitive impairments. Only studies that used health-related or hearing-related quality of life instruments that had been previously validated in the literature, were included. These strategies were established using a combination of standardized terms and key words, and were implemented in PubMed 1946-, Embase 1947-, CINAHL, the Cochrane Database of Systematic Reviews, Cochrane Database of Abstracts of Review Effects (DARE), Cochrane Central Register of Controlled Trials (CENTRAL), clinicaltrials.gov, Proquest Dissertations and Theses, and FirstSearch Proceedings. Searches were limited to English using database supplied filters. The search was completed in June, 2014, exported to EndNote, and duplicates were removed. Our comprehensive search terms are available in the appendix.
Candidate articles were independently reviewed by two authors familiar with the subject material, and discrepancies were discussed amongst the two authors. Articles were considered eligible if they included pediatric patients with hearing loss who were assessed using a validated quality of life measure. Information was collected on a data extraction form created by the authors. Variables collected included quality of life measure used, number of patients included, age range of patients, and effect size of the outcome measure. Effect size was generally a comparison of means between two groups, or a point estimate of change in pre/post intervention studies.
Quality Assessment
Quality was assessed using a scale modified from the Newcastle-Ottawa Scale.5 Three factors were rated as either low, high or unclear risk. The 3 factors included selection bias, outcome bias and overall risk of bias. Selection bias was determined based on representativeness of the population and demographics of the non-respondents as compared to the respondents. Outcome was assessed based on the use of a validated measurement tool, and the use of an appropriate statistical test. Studies were rated as “unclear” if details of these categories were not specified in the manuscript. Due to small sample size, studies were not excluded from the meta-analyses due to high or unclear risk of bias.
Meta-analysis
A meta-analysis was performed for quality of life measures with more than 2 studies reporting outcomes. Studies were required to contain both children with hearing loss and those with normal hearing (control group), and were separated based on unilateral or bilateral hearing loss. Further analyses were done to evaluate distinct quality of life domains. For our secondary outcome, a meta-analysis was performed for measures with more than 2 studies comparing quality of life pre- and post-treatment. A random effects analysis was performed for all analyses. Analyses combining data from multiple studies were performed using STATA statistical software version 13.1 (STATA Corporation, College Station, TX).
Clinical significance was determined based on previous studies of these validated tools. Clinical significance for the PedsQL tool has not been previously investigated in children with hearing loss. However this tool has been previously interrogated in a very large study of over 4,000 pediatric patients with diabetes. The minimal clinically important difference (MCID) scores for this quality of life measure was found to be dependent on type of diabetes, as well as parent versus child report, and ranged between 4 and 6 points on the PedsQL survey.6 This reference range was used when analyzing the results from our current study, and results were considered clinically significant if the absolute value of the effect size was 4 points or greater.
RESULTS
Description of studies
Following our comprehensive search and exclusion of duplicate studies, 1068 articles were identified. After reviewing titles, 979 abstracts were assessed for complete review of text. Sixty-nine complete articles were read, and 37 studies met criteria for inclusion. An additional 5 articles were identified during the review process and were included in the study. One article was removed due to use of duplicate data and patients. Ultimately, we included 41 articles in our systematic review (Figure 1). Information for the included studies is shown in tables 2–4.
Figure 1.

Flow chart of systematic review
Table 2.
Quality of life assessments: pediatric patients with hearing loss as compared to normal hearing peers
| Year | Authors | Age (years) | NH (n) | HL (n) | QOL tools | Conclusions |
|---|---|---|---|---|---|---|
| 2010 | Borton, et al.57 | 6–17 | 25 | 61 | PedsQL | No statistical difference in quality of life between children with normal vs impaired hearing (total, psychosocial, physical) |
| 2013 | Elbasan, et al.25 | 5–7 | 28 | 27 | CHQ, PEDI | Children with HL as compared to normal hearing were found to have lower scores in the following domains: global general health, emotional, physical, behavior, mental health, general health, family activity and cohesion and parental time (CHQ-PF50) and self-care, mobility and social function (PEDI). (p<0.05 for all listed comparisons above.) |
| 2008 | Fellinger, et al.26 | 6–16 | 0 | 99 | Inventory of Life Quality | As compared to a normative sample of normal hearing children, deaf pupils reported worse quality of life. (p<0.05 for the following comparisons: emotional problems, conduct problems, peer problems, social behavior and hyperactivity.) |
| 2005 | Huber, et al.27 | 8–16 | 1501 | 29 | KINDLR | As compared to normalized scores, children with CI had lower quality of life (ES: −1.6, p<0.001 for females with CI: age 8–12, self and ES: −1.1, p<0.025 for males with CI: age 8–12, self). |
| 2010 | Lovett, et al.28 | 1–16 | 56 | 50 | HUI3 | There were no significant differences between the 3 groups, normal hearing, unilateral CI and bilateral CI in health utility or QOL. |
| 2010 | Loy, et al.29 | 11–16 | 1501 | 88 | KINDLR | The two participant groups, those with Cis for hearing loss and their normal hearing peers, did not differ in their reported overall quality of life. |
| 2007 | Petrou, et al.30 | 7–9 | 63 | 120 | HUI3 | As compared to their normal hearing peers, children with bilateral permanent hearing loss were found to have significantly lower scores in the following domains of HUI3: vision, hearing, speech, ambulation, dexterity and cognition (p<0.05 for all comparisons listed). |
| 2012 | Schick, et al.31 | 11–18 | 0 | 221 | YQOL-R, YQOL-DHH | When compared to scores for their normal hearing peers, participants who were deaf or hard of hearing scored lower in “self” (p=0.036) and “relationship” domains (p=0.003). |
| 2011 | Umansky, et al.22 | 7–12 | 35 | 80 | PedsQL, HEAR-QL | Children with hearing loss reported significantly lower scores than their normal hearing peers on the HEAR-QL (71[18] vs 98[5]; p<0.001). PedsQL scores were not statistically different between hearing loss and normal hearing patients. |
| 2004 | Wake, et al.32 | 7–8 | 895 | 83 | CHQ | This study compared children with hearing loss fitted for hearing aids or CI compared to their normal hearing peers. Parent reported psychosocial well-being was lower in children with hearing loss (p = 0.001). |
| 2004 | Wake, et al.33 | 7–8 | 865 | 86 | CHQ | Compared to a normative sample, children with hearing loss had statistically significantly lower scores in quality of life measures related to psychosocial skills than their normal hearing peers (ES: 0.5, p<0.001). There were no differences in the physical domain. |
| 2006 | Wake, et al.34 | not given | 6516 | 55 | PedsQL | Compared to a normative sample of normal hearing peers, there were no significant differences in quality of life in hearing impaired children. |
| 2009 | Warner-czyz, et al35 | 4–7 | 25 | 50 | KINDLR | This study compared patients with hearing impairment and CI and those with normal hearing. There were no differences found in quality of life between these two groups. |
| 2014 | Rachakonda et al.23 | 13–18 | 54 | 172 | PedsQL, HEAR-QL | As compared to normal hearing peers, children with hearing loss reported significantly poorer hearing related QOL on the HEAR-QL in all categories (p<0.001) as well as lower scores on the school domain of the PedsQL (79[17] vs 70[20] p=0.001). |
| 2011 | Hintermair, et al.36 | 6–18 | 0 | 212 | Inventory of Life Quality | Compared to a normative sample, those with hearing loss reported worse quality of life in school (p<0.001) and social domains (p<0.001) than their normal hearing peers. |
| 2012 | Clark, et al.37 | 0–5 | 97 | 188 | VAS-HRQoL | Baseline deficits of CI candidates as compared to normal hearing peers were found in development domains, cognition (ES: 1.4, p=0.01) and speech recognition (ES: 1.4, p=0.02). Children implanted at a younger age had greater improvement in development. |
| 2010 | Rajendran, et al.56 | 6–11 | 100 | 100 | PedsQL | Compared to age-matched controls, children with hearing loss had lower scores in the physical and social domains. Specific domain scores and effect size were not available from this paper and it was not included in the meta-analysis. |
Table 4.
Quality of life in hearing impaired children: Miscellaneous studies evaluating children with hearing impairment
| Year | Authors | Age (years) | HL (n) | QOL tools | Conclusions |
|---|---|---|---|---|---|
| 2007 | Keilmann, et al.49 | 6–11 | 131 | Frankfurt Self Concept Scales for Children | This study evaluated children placed in assistive schools as compared to mainstream schools. Physical well-being was not affected, however children with hearing impairment placed in special schools had lower confidence and worse quality of life than those with hearing impairment who were in mainstream schools (p<0.05). |
| 2010 | Korver, et al.50 | 3–5 | 301 | PedsQL | This study evaluated children who underwent newborn screening as compared to screening at a later date. Quality of life was found to be statistically higher in the group of patients who underwent newborn hearing screening as compared to later assessment (mean between-group difference of 5.3(95% CI: 1.7–8.9)). |
| 2011 | Kushalnagar, et al.51 | 11–18 | 230 | YQoL-R, YQOL-DHH | Multiple cofactors were assessed. Quality of life scores were associated with an ability to understand parental expression and communication. |
| 2013 | Meyer, et al.52 | 11–18 | 157 | YQOL-DHH | Quality of life was assessed as related to multiple aspects of hearing impairment. Youth who were not using cochlear implants or technology scored higher on this stigma-related QoL (p<0.05) as compared to those with hearing aids or CI. |
| 2011 | Patrick, et al.53 | 11–18 | 230 | YQOL-R, YQOL-DHH | Patients had a variable amount of hearing loss in this study, and approximately 1/4 had previously received CI. Interestingly, quality of life was not significantly associated with hearing level. |
| 2008 | Smith-Olinde, et al.54 | 5–10 | 103 | HUI3 QWB |
Parents reported that QOL correlated with pure-tone average and was positively associated with CI status. |
| 2011 | Warner-Czyz, et al.55 | 4–16 | 138 | KINDL | All children in this study were CI users. Younger children rated HRQoL more positively than older children (mean 75.4[9.2] vs 70.4[12.4]). |
Outcome measures
There were multiple assessment tools used to assess quality of life in these pediatrics patients, ranging from generic quality of life measurements to those specifically assessing aspects of hearing loss (tables 2–4). The most commonly used assessment tools in this review are described below.
Glasgow Children’s Benefit Inventory (GCBI)7
This tool is used to assess benefit retrospectively after an intervention. There are 4 domains: emotion, physical health, learning and vitality. Answers are provided on a 5 point likert scale and converted to a scale ranging from −100 to +100. Higher positive scores indicate more improvement.
Health Utilities Index Mark 3 (HUI3)8,9
This tool is a utility-based measure of overall quality of life. There are 8 domains including vision, hearing, speech, ambulation, dexterity, emotion, cognition and pain. Higher scores indicate higher quality of life.
Pediatric Quality of Life Inventory (PedsQL)10
This measurement of overall health related quality of life is rated on a 5-point likert scale and converted to a scale from 0–100. There are 4 domains including physical, emotion, social and school. Higher scores indicate higher quality of life.
Hearing Environments and Reflection on Quality of Life Questionnaire (HEAR-QL)11
This tool is comprised of 26 questions focused on 3 domains, situations affecting interaction with family and friends, participation in school and social activities and the impact of impaired hearing on emotional well-being. Higher scores indicate higher quality of life.
Speech, Spatial and Qualities of Hearing Scale (SSQ)12
This tool has 3 domains, speech, spatial and qualities of hearing. The measurement was designed to evaluate the effects of hearing impairment specifically, with higher scores representing less disability.
Quality assessment
Quality assessment is shown in Table 1. Overall, there was low overall risk of bias in these studies. All studies used an appropriate statistical test and a validated quality of life metric although one study received an “unclear” rating for outcome bias as the quality of life metric used was validated, but then slightly modified for use. Fifteen studies were rated “unclear” for the selection category due to lack of detail regarding the selection process or the demographics of the non-responding population. No studies were considered high risk for the selection category as they used appropriate methods for recruitment.
Table 1.
Quality Assessment
| Year | Author | Selection bias | Outcome bias | Overall risk of bias |
|---|---|---|---|---|
| 2010 | Borton, et al24 | Low | Low | Low |
| 2013 | Elbasan, et al25 | Low | Low | Low |
| 2008 | Fellinger, et al26 | Unclear | Low | Unclear |
| 2005 | Huber, et al27 | Unclear | Low | Unclear |
| 2010 | Lovett, et al28 | Unclear | Low | Unclear |
| 2010 | Loy, et al29 | Unclear | Low | Unclear |
| 2007 | Petrou, et al30 | Low | Low | Low |
| 2012 | Schick, et al31 | Low | Low | Low |
| 2011 | Umansky, et al22 | Low | Low | Low |
| 2004 | Wake, et al32 | Low | Low | Low |
| 2004 | Wake, et al (b)33 | Low | Low | Low |
| 2006 | Wake, et al34 | Low | Low | Low |
| 2009 | Warner-czyz, et al35 | Unclear | Low | Unclear |
| 2014 | Rachakonda et al23 | Low | Low | Low |
| 2011 | Hintermair, et al36 | Unclear | Low | Unclear |
| 2012 | Clark, et al37 | Low | Low | Low |
| 2013 | Banga, et al18 | Unclear | Low | Unclear |
| 2011 | de Wolf, et al17 | Low | Low | Low |
| 2013 | Doshi, et al16 | Low | Low | Unclear |
| 2010 | Dun, et al13 | Low | Low | Low |
| 2014 | Fan, et al14 | Low | Low | Low |
| 2008 | Kunst, et al19 | Low | Low | Low |
| 2011 | Ricci, et al38 | Low | Low | Low |
| 2006 | Barton, et al39 | Unclear | Low | Unclear |
| 2006 | Stacey, et al40 | Low | Unclear | Unclear |
| 2000 | Cheng, et al41 | Low | Low | Low |
| 2009 | Huttunen, et al42 | Low | Low | Low |
| 2007 | Sach, et al43 | Unclear | Low | Unclear |
| 2009 | Schorr, et al44 | Low | Low | Low |
| 2012 | Necula, et al45 | Low | Low | Low |
| 2011 | Briggs, et al46 | Low | Low | Low |
| 2012 | Sparreboom, et al47 | Low | Low | Low |
| 2007 | Beijen, et al48 | Low | Low | Low |
| 2007 | Keilmann, et al49 | Unclear | Low | Unclear |
| 2010 | Korver, et al50 | Low | Low | Low |
| 2011 | Kushalnagar, et al51 | Unclear | Low | Unclear |
| 2013 | Meyer, et al52 | Unclear | Low | Unclear |
| 2011 | Patrick, et al53 | Unclear | Low | Unclear |
| 2008 | Smith-Olinde, et al54 | Low | Low | Low |
| 2011 | Warner-Czyz, et al55 | Unclear | Low | Unclear |
| 2010 | Rajendran, et al56 | Unclear | Low | Unclear |
Systematic Review
Sixteen studies attempted to address the potential difference in quality of life between children with hearing impairment and their normal hearing peers (table 2). Ten of these studies directly surveyed normal hearing children as a comparison group and 6 used databases of normative scores for commonly used assessment tools. Of these 16 studies, 11 (6 using a control group and 5 using normative scores for comparison) identified statistical differences between patients with hearing loss and those with normal hearing using one or more assessment tools, or by specifically looking at individual domains of a questionnaire. The remaining 5 studies (4 using control group and 1 using normative scores) did not identify any differences in quality of life between the two pediatric groups.
There were 21 studies evaluating quality of life improvement following an intervention, such as CI, BAHA or hearing aid use (table 3). Ten studies evaluated children following BAHA or soft band, 2 studies assessed children after hearing aid fitting, 7 studies included patients following cochlear implantation and 2 studies addressed the benefit of a second cochlear implantation. Overall, using a variety of assessment tools, both general and those specific to hearing impairment, interventions were convincingly helpful in improving quality of life from both patient and parental perspectives.
Table 3.
Quality of life assessments following intervention for hearing impairment
| Year | Authors | Age (years) | HL (n) | QOL tools | Intervention | Conclusions |
|---|---|---|---|---|---|---|
| 2013 | Banga, et al.18 | 6–16 | 27 | GCBI | BAHA | 26 of 27 children reported an improvement on GCBI after surgery. |
| 2011 | de Wolf, et al.17 | 6–17 | 31 | GCBI, HUI3, APHAB | BAHA | Patients reported an improvement in GCGI (+32[25] for bilateral hearing loss and +26[22] for unilateral hearing loss) following use of their BAHAs. |
| 2013 | Doshi, et al.16 | 7–12 | 8 | GCBI, SSQ | BAHA | 7 of the 8 children showed an increase in GCGI score (+40[24]) after surgery and 5/8 children felt that their quality of life had improved. |
| 2010 | Dun, et al.13 | 5–28 | 21 | GCBI | BAHA | A benefit from using the BAHA implant was found using the GCGI (+38[18]), with the learning domain showing the most positive change. |
| 2014 | Fan, et al.14 | 6–28 | 16 | GCBI | BAHA | There was an improvement in all GCBI scores following surgery (+46[14]). |
| 2008 | Kunst, et al.19 | 5–18 | 10 | GCBI, SSQ | BAHA | GCBI scores increased following BAHA implantation (+34). |
| 2011 | Ricci, et al.38 | 5–14 | 31 | GCBI | BAHA | Quality of life improved for all patients who underwent BAHA (+52[21]). |
| 2006 | Barton, et al.39 | not given | 2266 | HUI3 | CI | This study compared patients who were implanted as compared to those with hearing-impairment who were not implanted. There was a significant health utility benefit of implantation, especially with young age at implantation. |
| 2006 | Stacey, et al.40 | 3–20 | 2858 | Quality of life questionnaire | CI | Parents and teachers completed questionnaires. Pediatric CI at less than 5 years of age was associated with improvement in communication, education and quality of life. Of note, this study used a validated QOL measure, but then modified it before use. |
| 2000 | Cheng, et al41 | not given | 22 | HUI3 | CI | Following implantation, 95% of HUI3 scores increased (increase from 0.25 to 0.39), this finding was due to improvements in hearing and speech domains. |
| 2009 | Huttunen, et al.42 | 1–12 | 36 | Children with cochelar implants: parental perspectives | CI | Following implantation, parents reported improvement in social relations, communication and general functioning. |
| 2007 | Sach, et al.43 | not given | 222 | EuroQoL | CI | Quality of life was not significantly improved following implantation. |
| 2009 | Schorr, et al.44 | 5–14 | 37 | Children’s quality of life questionnaire | CI | Children reported an improvement in quality of life from their CI (mean of 26 points out of 35). |
| 2012 | Necula, et al.45 | 2–12 | 134 | Nijmegen CI HRQoL | CI/hearing-aid | CI improved auditory performance and speech production much more than hearing aids (p<0.05 in all domains). |
| 2011 | Briggs, et al.46 | 7–12 | 8 | HEAR-QL | Hearing aids | There was an improvement in quality of life following hearing aid use (difference of 20.1[10.5], p=0.002) |
| 2012 | Sparreboom, et al.47 | 1–7 | 39 | HUI3, PedsQL, GCBI, SSQ, NCIQ | second CI | Generic quality of life measures did not detect any differences following second implant. Higher scores were found for bilaterally implanted children in all domains of the GCBI as well as the SSQ and in sound perception, speech production and activity domains of the NCIQ. Bilaterally implanted children showed continued improvement in QoL over time, as compared to unilaterally implanted patients. |
| 2007 | Beijen, et al.48 | 1–2 | 10 | SSQ, PedsQL | second CI | This study compared bilaterally implanted children to unilaterally implanted children. No significant differences were found between SSQ and PedsQL scores. |
Lastly, there were 7 additional studies addressing quality of life in pediatric patients with hearing loss (table 4). These studies varied in their objective from evaluating the timing of identification of hearing loss on quality of life to noting differences in self-reporting of quality of life based on age.
Meta analyses
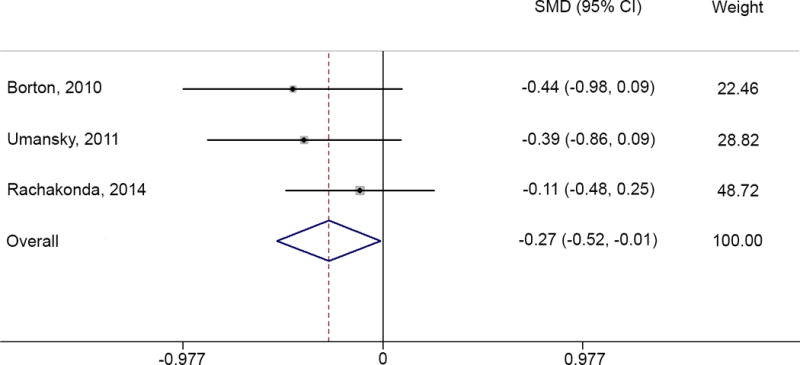
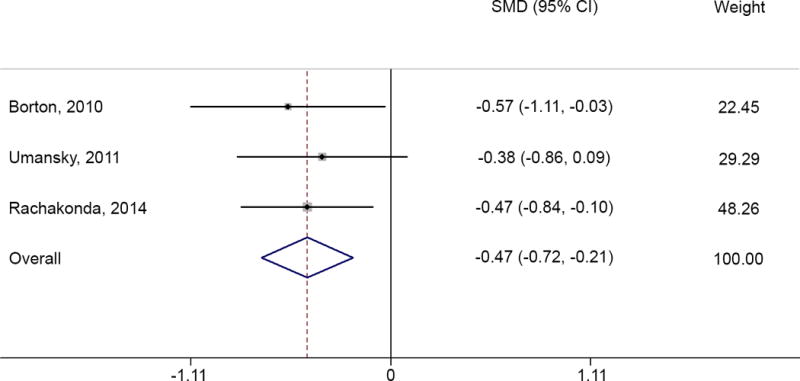
Four studies using child-reported PedsQL scores had sufficient data for inclusion in a meta-analysis. After pooling studies, statistically and clinically significant differences in PedsQL scores were found between children with normal hearing and those with hearing loss, both unilateral and bilateral, specifically in the School domain (difference of 8.79 points, 95% CI: 4.03–13.55 for unilateral hearing loss and difference of 6.93 points, 95% CI: 3.47–10.40 for bilateral hearing loss) and the Social domain (difference of 4.31 points, 95% CI: 0.26–9.22 for unilateral hearing loss and difference of 4.31 points, 95% CI: 0.07–8.54 for bilateral hearing loss). Additionally, statistically significant differences were seen in total scores for children with unilateral hearing loss only (difference of 3.8 points, 95% CI: 0.2–7.4) and in the physical domain between normal hearing and those with bilateral hearing loss (difference of 3.15 points, 95% CI: 0.23–6.07) however these differences were not clinically significant (table 5, and figures 2–5). Clinically significant differences were considered those with an absolute value of 4 or more, as previous studies have identified an MCID of 4–6 points for the PedsQL.
Table 5.
PedsQL Meta-Analysis
| Comparison | Effect size (SE) |
Difference in means (SE) |
95% CI of point difference* | p-value* | Statistical significance | Clinical significance | |
|---|---|---|---|---|---|---|---|
| Total NH and UHL | −0.27 (0.13) | −3.80 (1.84) | −7.40 | −0.20 | 0.038 | √ | |
| Total NH and BHL | −0.26 (0.11) | −3.41 (1.76) | −6.86 | 0.05 | 0.053 | ||
| Physical NH and UHL | −0.11 (0.13) | −1.52 (1.78) | −5.01 | 1.98 | 0.395 | ||
| Physical NH and BHL | −0.21 (0.10) | −3.15 (1.49) | −6.07 | −0.23 | 0.034 | √ | |
| Emotional NH and UHL | −0.18 (0.13) | −3.53 (2.53) | −8.49 | 1.43 | 0.163 | ||
| Emotional NH and BHL | −0.13 (0.10) | −2.61 (1.96) | −6.44 | 1.23 | 0.183 | ||
| Social NH and UHL | −0.27 (0.13) | −4.74 (2.29) | −9.22 | −0.26 | 0.038 | √ | √ |
| Social NH and BHL | −0.25 (0.11) | −4.31 (2.16) | −8.54 | −0.07 | 0.046 | √ | √ |
| School NH and UHL | −0.47 (0.13) | −8.79 (2.43) | −13.55 | −4.03 | <0.001 | √ | √ |
| School NH and BHL | −0.39 (0.10) | −6.93 (1.77) | −10.40 | −3.47 | <0.001 | √ | √ |
Variance, 95% CI and p-value based on difference in means.
NH = normal hearing, UHL = unilateral hearing loss, BHL = bilateral hearing loss
Figure 2.

PedsQL – School Domain: comparing normal hearing (NH) to bilateral hearing loss (BHL)
Figure 5.
PedsQL – Social Domain: comparing normal hearing (NH) to unilateral hearing loss (UHL)
The GCBI was the only quality of life measure with enough data for a combined analysis for pre/post intervention studies. A meta-analysis was used to combine the change in scores on GCBI following BAHA placement in children with both unilateral and bilateral hearing loss. Three studies included children with bilateral hearing loss only,13–15 1 study included children with unilateral hearing loss only,16 and 1 study included children with both unilateral and bilateral hearing loss,17 but with the data separated in the results. There were two other studies which used the GCBI in patients with BAHA placement,18,19 however after reaching out to authors by email, the appropriate necessary data for inclusion in the meta-analysis was only available from a total of 5 studies. As all studies showed a positive change in GCBI scores, it was not surprising that the meta-analysis revealed a positive change when combining all children (bilateral and unilateral hearing loss) as well as when studying only children with bilateral hearing loss. The mean change in GCBI scores were +40.35 (95% CI 24.60–56.09) for all children with hearing loss, and +43.02 points (95% CI 24.91–61.13) for children with bilateral hearing loss only (figures 5–6). Unfortunately, clinical significance has not yet been determined for this quality of life measure, so while GCBI scores show statistically significant improvement, we are unable to comment on clinical significance.
Figure 6.

GCBI Improvement following BAHA placement – all children with hearing loss
DISCUSSION
In this study, we have shown that there is high variability in reported quality of life in children with hearing loss. Using the only measure with adequate studies for meta-analysis, we found that the only domains with both statistically and clinically significantly differences between children with hearing loss and those with normal hearing are school and social categories. In this analysis, the differences in physical and emotional domains were not found to be clinically significant. While these findings are intuitive, our study is the first to show this in a comprehensive fashion.
A second aim of this study was to evaluate the potential improvement of quality of life in children following intervention. As seen in table 2, our review of the literature suggests that quality of life is significantly improved following aided hearing, BAHA and CI implantation. Two studies evaluated the effect of a second implant, however the results were inconsistent. In the larger study of the two, differences in quality of life were found only in disease-specific quality of life assessments, suggesting the importance of using measures which are specific to the hearing loss. Our meta-analysis combing GCBI scores in children after BAHA placement confirms that there is improvement in this measure following intervention, however we are unable to comment on clinical significance at this time, as it has not been determined for this quality of life tool.
There are multiple limitations of this study. The inherent limitations of a systematic review and meta-analysis exist, including that our analysis is dependent on the studies that our search returns. While statistical significance was addressed in several studies, few studies addressed the issue of clinical significance. As shown in our quality assessment, the risk of selection bias was often unclear, as many studies did not address the non-responders in the study, an important factor to consider in a survey study. A second limitation is that we are only able to perform a meta-analysis on quality of life measures with an adequate number of studies, and the number of studies included is relatively low. Additionally, while the PedsQL tool has been validated for use for overall total scores and the physical domain, the emotional, social and school domains have not been validated separately, which limits the strength of the conclusions drawn from these results. A third and major weakness of this study is the variability in age, hearing level and type of hearing loss of the participants in these studies. Unfortunately, due to small sample size, we are unable to stratify based on level of hearing loss or age of patients. Lastly, the wide range of quality of life measures used in these studies makes them difficult to combine in an organized fashion. Multiple measures are used commonly in assessing quality of life in children suffering from various disabilities; however there is no single, accepted quality of life tool used for pediatric hearing loss. The need for such a tool is obvious as pediatric hearing loss is a common problem and there appears to be substantial effects on quality of life, at least in certain specific aspects of functioning.
While previous studies have evaluated the effect of hearing loss on quality of life in pediatric patients,20,21 we believe that this is the first attempt to analytically differentiate between specific domains of quality of life measures. Previous work has been inconsistent in identifying quality of life deficits in children with hearing loss. One possible explanation for this is that while overall quality of life may not be clinically or statistically significantly affected in pediatric patients with hearing loss, there may be certain aspects of life in which quality is severely affected. The quality of life measures currently used may not be sensitive to these specific aspects. An instrument addressing the relevant domains of quality of life in hearing impaired children, such as the Youth Quality of Life Instrument (YQOL) and the Hearing Environments and Reflection on Quality of Life Questionnaire (HEAR-QL) may be more sensitive in detecting differences in hearing related quality of life. Thus far, the HEAR-QL has been shown to be valid and reliable as well as more sensitive to quality of life differences in children with hearing loss than the PedsQL, the most commonly used measure in our review.11 HEAR-QL has only a moderate correlation to the PedsQL22,23 and likely the addition of the “physical” domain in the PedsQL, as well as many other commonly used quality of life questionnaires, dilutes the clinical difference in quality of life when comparing children with hearing loss to their normal hearing peers. We believe that a focus on social interactions and school activities is especially important when considering quality of life in hearing impaired children as communication and learning are adversely affected in this patient population.
CONCLUSION
While there is variability in reported influences on quality of life from pediatric hearing loss, our analysis reveals that decreased quality of life in children with hearing loss is detected in distinct domains of the PedsQL questionnaire, school activities and social interactions. There is a need for a quality of life tool with a focus on these specific aspects when assessing hearing loss in the pediatric population.
Figure 3.
PedsQL – School Domain: comparing normal hearing (NH) to unilateral hearing loss (UHL)
Figure 4.

PedsQL – Social Domain: comparing normal hearing (NH) to bilateral hearing loss (BHL)
Figure 7.

GCBI Improvement following BAHA placement – bilateral hearing loss only
Acknowledgments
Funding support:
This work was supported by the T32DC00022 grant from the National Institutes of Deafness and Other Communications Disorders, and the Washington University Institute of Clinical and Translational Sciences grants UL1 TR000448 and TL1 TR000449 from the National Center for Advancing Translational Sciences.
Appendix: Search Terms
Deaf
“Deafness”[Mesh] OR “Deafness” OR “Deaf” OR “Bilateral Deafness” OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf-Mutism” OR “Deaf Mutism” OR “Acquired Deafness” OR “Extreme Hearing Loss”
Embase
‘Deafness’ OR ‘Deaf’ OR ‘Bilateral Deafness’ OR ‘Complete Hearing Loss’ OR ‘Prelingual Deafness’ OR ‘Deaf-Mutism’ OR ‘Deaf Mutism’ OR ‘Acquired Deafness’ OR ‘Extreme Hearing Loss’
CINAHL
MH “Deafness+” OR “Deafness” OR “Deaf” OR “Bilateral Deafness” OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf-Mutism” OR “Deaf Mutism” OR “Acquired Deafness” OR “Extreme Hearing Loss”
AND
Children, 5–18
PubMed
“Child”[Mesh] OR “Disabled Children”[Mesh] OR “Adolescent”[Mesh] OR “Child, Preschool”[Mesh] OR “Preschool Child” OR “Preschool Children” OR “Child” OR “Children” OR “Disabled Child” OR “Handicapped Children” OR “Children with Disability” OR “Children with Disabilities” OR “Adolescent” OR “Adolescents” OR “Teens” OR “Teen” OR “Teenagers” OR “Teenager” OR “Youth” OR “Youths” OR “Adolescence” OR “girl” OR “girls” OR “boy” OR “boys” OR “juvenile” OR “juveniles”
Embase
‘pediatrics’/exp OR ‘child’/exp OR ‘adolescent’/exp OR ‘Child’ OR ‘Children’ OR ‘Children’ OR ‘Disabled Child’ OR ‘Handicapped Children’ OR ‘Children with Disability’ OR ‘Children with Disabilities’ OR ‘Preschool Child’ OR ‘Preschool Children’ OR ‘Adolescent’ OR ‘Adolescents’ OR Teen* OR ‘Youth’ OR ‘Youths’ OR ‘Adolescence’ OR ‘girl’ OR ‘girls’ OR ‘boy’ OR ‘boys’ OR ‘juvenile’ OR ‘juveniles’ OR ‘Pediatrics’ OR ‘pediatric’ OR ‘pediatry’ OR ‘section 7’
CINAHL
MH “Child+” OR MH “Adolescence+” OR MH “Minors (Legal)” OR “Preschool Child” OR “Preschool Children” OR “Child” OR “Children” OR “Disabled Child” OR “Handicapped Children” OR “Children with Disability” OR “Children with Disabilities” OR “Adolescent” OR “Adolescents” OR “Teens” OR “Teen” OR “Teenagers” OR “Teenager” OR “Youth” OR “Youths” OR “Adolescence” OR “girl” OR “girls” OR “boy” OR “boys” OR “juvenile” OR “juveniles”
AND
Quality of Life
PubMed
“Quality of Life”[Mesh] OR “Quality of Life” OR “Life Qualities” OR “Life Quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”
Embase
‘quality of life’/exp OR ‘Quality of Life’ OR ‘Life Qualities’ OR ‘Life Quality’ OR ‘HRQL’ OR ‘health related quality of life’ OR ‘HRQOL’
CINAHL
MH “Quality of Life” OR “Quality of Life” OR “Life Qualities” OR “Life Quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”
AND
Validated HRQL Instruments (Specific)
PubMed
(instrumentation[sh] OR Validation Studies[pt] OR “Reproducibility of Results”[Mesh] OR reproducib*[tiab] OR “Psychometrics”[Mesh] OR psychometr*[tiab] OR clinimetr*[tiab] OR clinometr*[tiab] OR “Observer Variation”[Mesh] OR “observer variation”[tiab] OR “Discriminant Analysis”[Mesh] OR reliab*[tiab] OR valid*[tiab] OR coefficient[tiab] OR “internal consistency”[tiab] OR “item correlation”[tiab] OR “item correlations”[tiab] OR “item selection”[tiab] OR “item selections”[tiab] OR “item reduction”[tiab] OR “item reductions”[tiab] OR agreement[tw] OR precision[tw] OR imprecision[tw] OR “precise values”[tw] OR test–retest[tiab] OR stability[tiab] OR interrater[tiab] OR inter-rater[tiab] OR intrarater[tiab] OR intra-rater[tiab] OR intertester[tiab] OR inter-tester[tiab] OR intratester[tiab] OR intra-tester[tiab] OR interobserver[tiab] OR inter-observer[tiab] OR intraobserver[tiab] OR intra-observer[tiab] OR intertechnician[tiab] OR intertechnician[tiab] OR intratechnician[tiab] OR intra-technician[tiab] OR interexaminer[tiab] OR inter-examiner[tiab] OR intraexaminer[tiab] OR intra-examiner[tiab] OR interassay[tiab] OR inter-assay[tiab] OR intraassay[tiab] OR intra-assay[tiab] OR interindividual[tiab] OR inter-individual[tiab] OR intraindividual[tiab] OR intra-individual[tiab] OR interparticipant[tiab] OR inter-participant[tiab] OR intraparticipant[tiab] OR intra-participant[tiab] OR kappa[tiab] OR kappa’s[tiab] OR kappas[tiab] OR “coefficient of variation”[tiab] OR repeatab*[tw] OR generaliza*[tiab] OR generalisa*[tiab] OR concordance[tiab] OR discriminative[tiab] OR “known group”[tiab] OR “factor analysis”[tiab] OR “factor analyses”[tiab] OR “factor structure”[tiab] OR “factor structures”[tiab] OR dimensionality[tiab] OR subscale*[tiab] OR “multitrait scaling analysis”[tiab] OR “multitrait scaling analyses”[tiab] OR “item discriminant”[tiab]OR “interscale correlation”[tiab] OR “interscale correlations”[tiab] OR “individual variability”[tiab] OR “interval variability”[tiab] OR “rate variability”[tiab] OR “variability analysis”[tiab] OR “standard error of measurement”[tiab] OR sensitiv*[tiab] OR responsive*[tiab] OR “minimal detectable concentration”[tiab] OR interpretab*[tiab] OR “meaningful change”[tiab] OR “minimal important change”[tiab] OR “minimal important difference”[tiab] OR “minimally important change”[tiab] OR “minimally important difference”[tiab] OR “minimal detectable change”[tiab] OR “minimal detectable difference”[tiab] OR “minimally detectable change”[tiab] OR “minimally detectable difference”[tiab] OR “minimal real change”[tiab] OR “minimal real difference”[tiab] OR “minimally real change”[tiab] OR “minimally real difference”[tiab] OR “ceiling effect”[tiab] OR “floor effect”[tiab] OR “Item response model”[tiab] OR IRT[tiab] OR Rasch[tiab] OR “Differential item functioning”[tiab] OR DIF[tiab] OR “computer adaptive testing”[tiab] OR “item bank”[tiab] OR “cross-cultural equivalence”[tiab])
Embase
‘instrumentation’/exp OR ‘validation study’/exp OR ‘reproducibility’/exp OR reproducib* OR ‘psychometry’/exp OR psychometr*OR clinimetr*OR clinometr* OR ‘observer variation’/exp OR ‘observer variation’ OR ‘discriminant analysis’/exp OR reliab* OR valid* OR coefficient OR ‘internal consistency’ OR ‘item correlation’ OR ‘item correlations’ OR ‘item selection’ OR ‘item selections’ OR ‘item reduction’ OR ‘item reductions’ OR agreement OR precision OR imprecision OR ‘precise values’ OR test–retest OR stability OR interrater OR inter-rater OR intrarater OR intra-rater OR intertester OR inter-tester OR intratester OR intra-tester OR interobserver OR inter-observer OR intraobserver OR intra-observer OR intertechnician OR intertechnician OR intratechnician OR intra-technician OR interexaminer OR inter-examiner OR intraexaminer OR intra-examiner OR interassay OR inter-assay OR intraassay OR intra-assay OR interindividual OR inter-individual OR intraindividual OR intra-individual OR interparticipant OR inter-participant OR intraparticipant OR intra-participant OR kappa OR kappas OR ‘coefficient of variation’ OR repeatab* OR generaliza* OR generalisa* OR concordance OR discriminative OR ‘known group’ OR ‘factor analysis’ OR ‘factor analyses’ OR ‘factor structure’ OR ‘factor structures’ OR dimensionality OR subscale* OR ‘multitrait scaling analysis’ OR ‘multitrait scaling analyses’ OR ‘item discriminant’ OR ‘interscale correlation’ OR ‘interscale correlations’ OR ‘individual variability’ OR ‘interval variability’ OR ‘rate variability’ OR ‘variability analysis’ OR ‘standard error of measurement’ OR sensitiv* OR responsive* OR ‘minimal detectable concentration’ OR interpreta* OR ‘meaningful change’ OR ‘minimal important change’ OR ‘minimal important difference’ OR ‘minimally important change’ OR ‘minimally important difference’ OR ‘minimal detectable change’ OR ‘minimal detectable difference’ OR ‘minimally detectable change’ OR ‘minimally detectable difference’ OR ‘minimal real change’ OR ‘minimal real difference’ OR ‘minimally real change’ OR ‘minimally real difference’ OR ‘ceiling effect’ OR ‘floor effect’ OR ‘Item response model’ OR IRT OR Rasch OR ‘Differential item functioning’ OR DIF OR ‘computer adaptive testing’ OR ‘item bank’ OR ‘cross cultural equivalence’
CINAHL
MH “Validation Studies” OR MH “Reproducibility of Results” OR MH “Psychometrics” OR psychometr*OR clinimetr*OR clinometr* OR “observer variation”/exp OR “observer variation” OR “discriminant analysis” OR reliab* OR valid* OR coefficient OR “internal consistency” OR “item correlation” OR “item correlations” OR “item selection” OR “item selections” OR “item reduction” OR “item reductions” OR agreement OR precision OR imprecision OR “precise values” OR test–retest OR stability OR interrater OR inter-rater OR intrarater OR intra-rater OR intertester OR inter-tester OR intratester OR intra-tester OR interobserver OR inter-observer OR intraobserver OR intra-observer OR intertechnician OR intertechnician OR intratechnician OR intra-technician OR interexaminer OR inter-examiner OR intraexaminer OR intra-examiner OR interassay OR inter-assay OR intraassay OR intra-assay OR interindividual OR inter-individual OR intraindividual OR intra-individual OR interparticipant OR inter-participant OR intraparticipant OR intra-participant OR kappa OR kappas OR “coefficient of variation” OR repeatab* OR generaliza* OR generalisa* OR concordance OR discriminative OR “known group” OR “factor analysis” OR “factor analyses” OR “factor structure” OR “factor structures” OR dimensionality OR subscale* OR “multitrait scaling analysis” OR “multitrait scaling analyses” OR “item discriminant” OR “interscale correlation” OR “interscale correlations” OR “individual variability” OR “interval variability” OR “rate variability” OR “variability analysis” OR “standard error of measurement” OR sensitiv* OR responsive* OR “minimal detectable concentration” OR interpreta* OR “meaningful change” OR “minimal important change” OR “minimal important difference” OR “minimally important change” OR “minimally important difference” OR “minimal detectable change” OR “minimal detectable difference” OR “minimally detectable change” OR “minimally detectable difference” OR “minimal real change” OR “minimal real difference” OR “minimally real change” OR “minimally real difference” OR “ceiling effect” OR “floor effect” OR “Item response model” OR IRT OR Rasch OR “Differential item functioning” OR DIF OR “computer adaptive testing” OR “item bank” OR “cross cultural equivalence”
NOT
Cognitive impairment
PubMed
“cognition disorder” OR “cognition disorders” OR “cognitive defects” OR “cognitive deficit” OR “cognitive disability” OR “cognitive disorder” OR “cognitive disorders” OR “cognitive dysfunction” OR “cognitive impairment” OR “delirium” OR “dementia” OR “amnestic” OR “cognitive disorders” OR “overinclusion” OR “response interference” OR “Cognition Disorders”[Mesh] OR “Cognition Disorders” OR “Auditory Perceptual Disorder” OR “Psychoacoustical Disorders” OR “Psychoacoustical Disorder” OR “Auditory Comprehension Disorder” OR “Auditory Comprehension Disorders” OR “Auditory Processing Disorder” OR “Auditory Processing Disorders” OR “Acoustic Perceptual Disorder” OR “Acoustic Perceptual Disorders” OR “Auditory Inattention” OR “Auditory Inattentions” OR “Huntington Disease” OR “Huntington Chorea” OR “Huntington’s Disease” OR “Huntington Chronic Progressive Hereditary Chorea” OR “Chronic Progressive Hereditary Chorea” OR “Huntington’s Chorea” OR “Late-Onset Huntington Disease” OR “Late Onset Huntington Disease” OR “Juvenile Huntington Disease” OR “Juvenile-Onset Huntington Disease” OR “Juvenile Onset Huntington Disease” OR “Akinetic-Rigid Variant of Huntington Disease” OR “Akinetic Rigid Variant of Huntington Disease” OR “Dementia”OR “Delirium” OR “Amnesia” OR “Dementias” OR “Amentia” OR “Amentias” OR “Deliriums”
Embase
‘cognition disorder’ OR ‘cognition disorders’ OR ‘cognitive defects’ OR ‘cognitive deficit’ OR ‘cognitive disability’ OR ‘cognitive disorder’ OR ‘cognitive disorders’ OR ‘cognitive dysfunction’ OR ‘cognitive impairment’ OR ‘delirium’ OR ‘dementia’ OR ‘amnestic’ OR ‘cognitive disorders’ OR ‘overinclusion’ OR ‘response interference’ OR ‘Cognition Disorders’ OR ‘Cognition Disorders’ OR ‘Auditory Perceptual Disorder’ OR ‘Psychoacoustical Disorders’ OR ‘Psychoacoustical Disorder’ OR ‘Auditory Comprehension Disorder’ OR ‘Auditory Comprehension Disorders’ OR ‘Auditory Processing Disorder’ OR ‘Auditory Processing Disorders’ OR ‘Acoustic Perceptual Disorder’ OR ‘Acoustic Perceptual Disorders’ OR ‘Auditory Inattention’ OR ‘Auditory Inattentions’ OR ‘Huntington Disease’ OR ‘Huntington Chorea’ OR ‘Huntington’s Disease’ OR ‘Huntington Chronic Progressive Hereditary Chorea’ OR ‘Chronic Progressive Hereditary Chorea’ OR ‘Huntington’s Chorea’ OR ‘Late-Onset Huntington Disease’ OR ‘Late Onset Huntington Disease’ OR ‘Juvenile Huntington Disease’ OR ‘Juvenile-Onset Huntington Disease’ OR ‘Juvenile Onset Huntington Disease’ OR ‘Akinetic-Rigid Variant of Huntington Disease’ OR ‘Akinetic Rigid Variant of Huntington Disease’ OR ‘Dementia’OR ‘Delirium’ OR ‘Amnesia’ OR ‘Dementias’ OR ‘Amentia’ OR ‘Amentias’ OR ‘Deliriums’
CINAHL
“cognition disorder” OR “cognition disorders” OR “cognitive defects” OR “cognitive deficit” OR “cognitive disability” OR “cognitive disorder” OR “cognitive disorders” OR “cognitive dysfunction” OR “cognitive impairment” OR “delirium” OR “dementia” OR “amnestic” OR “cognitive disorders” OR “overinclusion” OR “response interference” OR “Cognition Disorders” OR “Cognition Disorders” OR “Auditory Perceptual Disorder” OR “Psychoacoustical Disorders” OR “Psychoacoustical Disorder” OR “Auditory Comprehension Disorder” OR “Auditory Comprehension Disorders” OR “Auditory Processing Disorder” OR “Auditory Processing Disorders” OR “Acoustic Perceptual Disorder” OR “Acoustic Perceptual Disorders” OR “Auditory Inattention” OR “Auditory Inattentions” OR “Huntington Disease” OR “Huntington Chorea” OR “Huntington”s Disease” OR “Huntington Chronic Progressive Hereditary Chorea” OR “Chronic Progressive Hereditary Chorea” OR “Huntington”s Chorea” OR “Late-Onset Huntington Disease” OR “Late Onset Huntington Disease” OR “Juvenile Huntington Disease” OR “Juvenile-Onset Huntington Disease” OR “Juvenile Onset Huntington Disease” OR “Akinetic-Rigid Variant of Huntington Disease” OR “Akinetic Rigid Variant of Huntington Disease” OR “Dementia”OR “Delirium” OR “Amnesia” OR “Dementias” OR “Amentia” OR “Amentias” OR “Deliriums”
NOT
PubMed
“Tinnitus”[Mesh] OR “Otitis Media”[Mesh] OR “Tinnitus” OR “Middle Ear Inflammation” OR “ear buzzing” OR “false latent otitis” OR “middle ear infection” OR “middle ear infections” OR “tympanitis”
Embase
‘tinnitus’/exp OR ‘otitis media’/exp OR ‘tinnitus’ OR ‘Middle Ear Inflammation’ OR ‘ear buzzing’ OR ‘false latent otitis’ OR ‘middle ear infection’ OR ‘middle ear infections’ OR ‘tympanitis’
CINAHL
MH “Tinnitus” OR MH “Otitis Media” OR “Tinnitus” OR “Middle Ear Inflammation” OR “ear buzzing” OR “false latent otitis” OR “middle ear infection” OR “middle ear infections” OR “tympanitis”
NOT
(“addresses”[Publication Type] OR “biography”[Publication Type] OR “case reports”[Publication Type] OR “comment”[Publication Type] OR “directory”[Publication Type] OR “editorial”[Publication Type] OR “festschrift”[Publication Type] OR “interview”[Publication Type] OR “lectures”[Publication Type] OR “legal cases”[Publication Type] OR “legislation”[Publication Type] OR “letter”[Publication Type] OR “news”[Publication Type] OR “newspaper article”[Publication Type] OR “patient education handout”[Publication Type] OR “popular works”[Publication Type] OR “congresses”[Publication Type] OR “consensus development conference”[Publication Type] OR “consensus development conference, nih”[Publication Type] OR “practice guideline”[Publication Type])
NOT
Animals
PubMed
(“animals”[Mesh] NOT “humans”[Mesh])
Embase
([animals]/lim NOT [humans]/lim)
C&P PubMed (22)
(“Deafness”[Mesh] OR “Deafness” OR “Deaf” OR “Bilateral Deafness” OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf-Mutism” OR “Deaf Mutism” OR “Acquired Deafness” OR “Extreme Hearing Loss”) AND (“Child” [Mesh] OR “Infant” [Mesh] OR “Adolescent” [Mesh] OR “Pediatrics” [Mesh] OR Child OR children OR Adolescen* OR Teen* OR Youth OR Youths OR girl* OR boy OR boys OR juvenile* OR pediatrics OR pediatric OR pediatry OR “section 7” OR “disabled child” OR “handicapped child” OR “children with disability” OR “children with disabilities”) AND (“Quality of Life”[Mesh] OR “Quality of Life” OR “Life Qualities” OR “Life Quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”) AND (instrumentation[sh] OR Validation Studies[pt] OR “Reproducibility of Results”[Mesh] OR reproducib*[tiab] OR “Psychometrics”[Mesh] OR psychometr*[tiab] OR clinimetr*[tiab] OR clinometr*[tiab] OR “Observer Variation”[Mesh] OR “observer variation”[tiab] OR “Discriminant Analysis”[Mesh] OR reliab*[tiab] OR valid*[tiab] OR coefficient[tiab] OR “internal consistency”[tiab] OR “item correlation”[tiab] OR “item correlations”[tiab] OR “item selection”[tiab] OR “item selections”[tiab] OR “item reduction”[tiab] OR “item reductions”[tiab] OR agreement[tw] OR precision[tw] OR imprecision[tw] OR “precise values”[tw] OR test–retest[tiab] OR stability[tiab] OR interrater[tiab] OR inter-rater[tiab] OR intrarater[tiab] OR intra-rater[tiab] OR intertester[tiab] OR inter-tester[tiab] OR intratester[tiab] OR intra-tester[tiab] OR interobserver[tiab] OR inter-observer[tiab] OR intraobserver[tiab] OR intra-observer[tiab] OR intertechnician[tiab] OR intertechnician[tiab] OR intratechnician[tiab] OR intra-technician[tiab] OR interexaminer[tiab] OR inter-examiner[tiab] OR intraexaminer[tiab] OR intra-examiner[tiab] OR interassay[tiab] OR inter-assay[tiab] OR intraassay[tiab] OR intra-assay[tiab] OR interindividual[tiab] OR inter-individual[tiab] OR intraindividual[tiab] OR intra-individual[tiab] OR interparticipant[tiab] OR inter-participant[tiab] OR intraparticipant[tiab] OR intra-participant[tiab] OR kappa[tiab] OR kappa’s[tiab] OR kappas[tiab] OR “coefficient of variation”[tiab] OR repeatab*[tw] OR generaliza*[tiab] OR generalisa*[tiab] OR concordance[tiab] OR discriminative[tiab] OR “known group”[tiab] OR “factor analysis”[tiab] OR “factor analyses”[tiab] OR “factor structure”[tiab] OR “factor structures”[tiab] OR dimensionality[tiab] OR subscale*[tiab] OR “multitrait scaling analysis”[tiab] OR “multitrait scaling analyses”[tiab] OR “item discriminant”[tiab]OR “interscale correlation”[tiab] OR “interscale correlations”[tiab] OR “individual variability”[tiab] OR “interval variability”[tiab] OR “rate variability”[tiab] OR “variability analysis”[tiab] OR “standard error of measurement”[tiab] OR sensitiv*[tiab] OR responsive*[tiab] OR “minimal detectable concentration”[tiab] OR interpretab*[tiab] OR “meaningful change”[tiab] OR “minimal important change”[tiab] OR “minimal important difference”[tiab] OR “minimally important change”[tiab] OR “minimally important difference”[tiab] OR “minimal detectable change”[tiab] OR “minimal detectable difference”[tiab] OR “minimally detectable change”[tiab] OR “minimally detectable difference”[tiab] OR “minimal real change”[tiab] OR “minimal real difference”[tiab] OR “minimally real change”[tiab] OR “minimally real difference”[tiab] OR “ceiling effect”[tiab] OR “floor effect”[tiab] OR “Item response model”[tiab] OR IRT[tiab] OR Rasch[tiab] OR “Differential item functioning”[tiab] OR DIF[tiab] OR “computer adaptive testing”[tiab] OR “item bank”[tiab] OR “cross-cultural equivalence”[tiab]) NOT (“cognition disorder” OR “cognition disorders” OR “cognitive defects” OR “cognitive deficit” OR “cognitive disability” OR “cognitive disorder” OR “cognitive disorders” OR “cognitive dysfunction” OR “cognitive impairment” OR “delirium” OR “dementia” OR “amnestic” OR “cognitive disorders” OR “overinclusion” OR “response interference” OR “Cognition Disorders”[Mesh] OR “Cognition Disorders” OR “Auditory Perceptual Disorder” OR “Psychoacoustical Disorders” OR “Psychoacoustical Disorder” OR “Auditory Comprehension Disorder” OR “Auditory Comprehension Disorders” OR “Auditory Processing Disorder” OR “Auditory Processing Disorders” OR “Acoustic Perceptual Disorder” OR “Acoustic Perceptual Disorders” OR “Auditory Inattention” OR “Auditory Inattentions” OR “Huntington Disease” OR “Huntington Chorea” OR “Huntington’s Disease” OR “Huntington Chronic Progressive Hereditary Chorea” OR “Chronic Progressive Hereditary Chorea” OR “Huntington’s Chorea” OR “Late-Onset Huntington Disease” OR “Late Onset Huntington Disease” OR “Juvenile Huntington Disease” OR “Juvenile-Onset Huntington Disease” OR “Juvenile Onset Huntington Disease” OR “Akinetic-Rigid Variant of Huntington Disease” OR “Akinetic Rigid Variant of Huntington Disease” OR “Dementia” OR “Delirium” OR “Amnesia” OR “Dementias” OR “Amentia” OR “Amentias” OR “Deliriums” OR “Tinnitus”[Mesh] OR “Otitis Media”[Mesh] OR “Tinnitus” OR “Middle Ear Inflammation” OR “ear buzzing” OR “false latent otitis” OR “middle ear infection” OR “middle ear infections” OR “tympanitis”) NOT (“animals”[Mesh] NOT “humans”[Mesh])
Limits: English
C&P Embase (80)
‘Deafness’ OR ‘Deaf’ OR ‘Bilateral Deafness’ OR ‘Complete Hearing Loss’ OR ‘Prelingual Deafness’ OR ‘Deaf-Mutism’ OR ‘Deaf Mutism’ OR ‘Acquired Deafness’ OR ‘Extreme Hearing Loss’ AND (‘pediatrics’/exp OR ‘child’/exp OR ‘adolescent’/exp OR ‘Child’ OR ‘Children’ OR ‘Children’ OR ‘Disabled Child’ OR ‘Handicapped Children’ OR ‘Children with Disability’ OR ‘Children with Disabilities’ OR ‘Preschool Child’ OR ‘Preschool Children’ OR ‘Adolescent’ OR ‘Adolescents’ OR Teen* OR ‘Youth’ OR ‘Youths’ OR ‘Adolescence’ OR ‘girl’ OR ‘girls’ OR ‘boy’ OR ‘boys’ OR ‘juvenile’ OR ‘juveniles’ OR ‘Pediatrics’ OR ‘pediatric’ OR ‘pediatry’ OR ‘section 7’) AND (‘quality of life’/exp OR ‘Quality of Life’ OR ‘Life Qualities’ OR ‘Life Quality’ OR ‘HRQL’ OR ‘health related quality of life’ OR ‘HRQOL’) AND (‘instrumentation’/exp OR ‘validation study’/exp OR ‘reproducibility’/exp OR reproducib* OR ‘psychometry’/exp OR psychometr*OR clinimetr*OR clinometr* OR ‘observer variation’/exp OR ‘observer variation’ OR ‘discriminant analysis’/exp OR reliab* OR valid* OR coefficient OR ‘internal consistency’ OR ‘item correlation’ OR ‘item correlations’ OR ‘item selection’ OR ‘item selections’ OR ‘item reduction’ OR ‘item reductions’ OR agreement OR precision OR imprecision OR ‘precise values’ OR test–retest OR stability OR interrater OR inter-rater OR intrarater OR intra-rater OR intertester OR inter-tester OR intratester OR intra-tester OR interobserver OR inter-observer OR intraobserver OR intra-observer OR intertechnician OR intertechnician OR intratechnician OR intra-technician OR interexaminer OR inter-examiner OR intraexaminer OR intra-examiner OR interassay OR inter-assay OR intraassay OR intra-assay OR interindividual OR inter-individual OR intraindividual OR intra-individual OR interparticipant OR inter-participant OR intraparticipant OR intra-participant OR kappa OR kappas OR ‘coefficient of variation’ OR repeatab* OR generaliza* OR generalisa* OR concordance OR discriminative OR ‘known group’ OR ‘factor analysis’ OR ‘factor analyses’ OR ‘factor structure’ OR ‘factor structures’ OR dimensionality OR subscale* OR ‘multitrait scaling analysis’ OR ‘multitrait scaling analyses’ OR ‘item discriminant’ OR ‘interscale correlation’ OR ‘interscale correlations’ OR ‘individual variability’ OR ‘interval variability’ OR ‘rate variability’ OR ‘variability analysis’ OR ‘standard error of measurement’ OR sensitiv* OR responsive* OR ‘minimal detectable concentration’ OR interpreta* OR ‘meaningful change’ OR ‘minimal important change’ OR ‘minimal important difference’ OR ‘minimally important change’ OR ‘minimally important difference’ OR ‘minimal detectable change’ OR ‘minimal detectable difference’ OR ‘minimally detectable change’ OR ‘minimally detectable difference’ OR ‘minimal real change’ OR ‘minimal real difference’ OR ‘minimally real change’ OR ‘minimally real difference’ OR ‘ceiling effect’ OR ‘floor effect’ OR ‘Item response model’ OR IRT OR Rasch OR ‘Differential item functioning’ OR DIF OR ‘computer adaptive testing’ OR ‘item bank’ OR ‘cross cultural equivalence’) NOT (‘cognition disorder’ OR ‘cognition disorders’ OR ‘cognitive defects’ OR ‘cognitive deficit’ OR ‘cognitive disability’ OR ‘cognitive disorder’ OR ‘cognitive disorders’ OR ‘cognitive dysfunction’ OR ‘cognitive impairment’ OR ‘delirium’ OR ‘dementia’ OR ‘amnestic’ OR ‘cognitive disorders’ OR ‘overinclusion’ OR ‘response interference’ OR ‘Cognition Disorders’ OR ‘Cognition Disorders’ OR ‘Auditory Perceptual Disorder’ OR ‘Psychoacoustical Disorders’ OR ‘Psychoacoustical Disorder’ OR ‘Auditory Comprehension Disorder’ OR ‘Auditory Comprehension Disorders’ OR ‘Auditory Processing Disorder’ OR ‘Auditory Processing Disorders’ OR ‘Acoustic Perceptual Disorder’ OR ‘Acoustic Perceptual Disorders’ OR ‘Auditory Inattention’ OR ‘Auditory Inattentions’ OR ‘Huntington Disease’ OR ‘Huntington Chorea’ OR ‘Huntingtons Disease’ OR ‘Huntington Chronic Progressive Hereditary Chorea’ OR ‘Chronic Progressive Hereditary Chorea’ OR ‘Huntingtons Chorea’ OR ‘Late-Onset Huntington Disease’ OR ‘Late Onset Huntington Disease’ OR ‘Juvenile Huntington Disease’ OR ‘Juvenile-Onset Huntington Disease’ OR ‘Juvenile Onset Huntington Disease’ OR ‘Akinetic-Rigid Variant of Huntington Disease’ OR ‘Akinetic Rigid Variant of Huntington Disease’ OR ‘Dementia’ OR ‘Delirium’ OR ‘Amnesia’ OR ‘Dementias’ OR ‘Amentia’ OR ‘Amentias’ OR ‘Deliriums’ OR ‘tinnitus’/exp OR ‘otitis media’/exp OR ‘tinnitus’ OR ‘Middle Ear Inflammation’ OR ‘ear buzzing’ OR ‘false latent otitis’ OR ‘middle ear infection’ OR ‘middle ear infections’ OR ‘tympanitis’) NOT ([animals]/lim NOT [humans]/lim) AND [english]/lim
C&P Scopus (181)
TITLE-ABS-KEY(“Deafness” OR “Deaf” OR “Bilateral Deafness” OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf Mutism” OR “Acquired Deafness” OR “Extreme Hearing Loss”)
AND
TITLE-ABS-KEY(“pediatrics” OR “child” OR “adolescent” OR “Child” OR “Children” OR “Children” OR “Disabled Child” OR “Handicapped Children” OR “Children with Disability” OR “Children with Disabilities” OR “Preschool Child” OR “Preschool Children” OR “Adolescent” OR “Adolescents” OR Teen* OR “Youth” OR “Youths” OR “Adolescence” OR “girl” OR “girls” OR “boy” OR “boys” OR “juvenile” OR “juveniles” OR “Pediatrics” OR “pediatric” OR “pediatry” OR “section 7”)
AND
TITLE-ABS-KEY(“quality of life” OR “Quality of Life” OR “Life Qualities” OR “Life Quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”)
AND
(“instrumentation” OR “validation study” OR “reproducibility” OR reproducibility OR “psychometry” OR “observer variation” OR “observer variation” OR “discriminant analysis” OR reliability OR validity OR coefficient OR “internal consistency” OR “item correlation” OR “item correlations” OR “item selection” OR “item selections” OR “item reduction” OR “item reductions” OR agreement OR precision OR imprecision OR “precise values” OR test retest OR stability OR interrater OR interrater OR intrarater OR intrarater OR intertester OR intertester OR intratester OR intratester OR interobserver OR interobserver OR intraobserver OR intraobserver OR intertechnician OR intertechnician OR intratechnician OR intratechnician OR interexaminer OR interexaminer OR intraexaminer OR intraexaminer OR interassay OR interassay OR intraassay OR intraassay OR interindividual OR interindividual OR intraindividual OR intraindividual OR interparticipant OR interparticipant OR intraparticipant OR intraparticipant OR kappa OR kappas OR “coefficient of variation” OR repeatability OR generalizability OR generalisation OR concordance OR discriminative OR “known group” OR “factor analysis” OR “factor analyses” OR “factor structure” OR “factor structures” OR dimensionality OR subscale OR subscales OR “multitrait scaling analysis” OR “multitrait scaling analyses” OR “item discriminant” OR “interscale correlation” OR “interscale correlations” OR “individual variability” OR “interval variability” OR “rate variability” OR “variability analysis” OR “standard error of measurement” OR sensitivity OR responsiveness OR “minimal detectable concentration” OR interpretability OR “meaningful change” OR “minimal important change” OR “minimal important difference” OR “minimally important change” OR “minimally important difference” OR “minimal detectable change” OR “minimal detectable difference” OR “minimally detectable change” OR “minimally detectable difference” OR “minimal real change” OR “minimal real difference” OR “minimally real change” OR “minimally real difference” OR “ceiling effect” OR “floor effect” OR “Item response model” OR IRT OR Rasch OR “Differential item functioning” OR DIF OR “computer adaptive testing” OR “item bank” OR “cross cultural equivalence”
NOT
“cognition disorder” OR “cognition disorders” OR “cognitive defects” OR “cognitive deficit” OR “cognitive disability” OR “cognitive disorder” OR “cognitive disorders” OR “cognitive dysfunction” OR “cognitive impairment” OR “delirium” OR “dementia” OR “amnestic” OR “cognitive disorders” OR “overinclusion” OR “response interference” OR “Cognition Disorders” OR “Cognition Disorders” OR “Auditory Perceptual Disorder” OR “Psychoacoustical Disorders” OR “Psychoacoustical Disorder” OR “Auditory Comprehension Disorder” OR “Auditory Comprehension Disorders” OR “Auditory Processing Disorder” OR “Auditory Processing Disorders” OR “Acoustic Perceptual Disorder” OR “Acoustic Perceptual Disorders” OR “Auditory Inattention” OR “Auditory Inattentions” OR “Huntington Disease” OR “Huntington Chorea” OR “Huntingtons Disease” OR “Huntington Chronic Progressive Hereditary Chorea” OR “Chronic Progressive Hereditary Chorea” OR “Huntingtons Chorea” OR “Late-Onset Huntington Disease” OR “Late Onset Huntington Disease” OR “Juvenile Huntington Disease” OR “Juvenile-Onset Huntington Disease” OR “Juvenile Onset Huntington Disease” OR “Akinetic-Rigid Variant of Huntington Disease” OR “Akinetic Rigid Variant of Huntington Disease” OR “Dementia” OR “Delirium” OR “Amnesia” OR “Dementias” OR “Amentia” OR “Amentias” OR “Deliriums” OR “tinnitus” OR “otitis media” OR “tinnitus” OR “Middle Ear Inflammation” OR “ear buzzing” OR “false latent otitis” OR “middle ear infection” OR “middle ear infections” OR “tympanitis”d
Limited to: (Human OR Humans) AND English
C&P CINAHL (13)
(MH “Deafness+” OR “Deafness” OR “Deaf” OR “Bilateral Deafness” OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf-Mutism” OR “Deaf Mutism” OR “Acquired Deafness” OR “Extreme Hearing Loss”) AND (MH “Child+” OR MH “Adolescence+” OR “Minors” OR “Preschool Child” OR “Preschool Children” OR “Child” OR “Children” OR “Disabled Child” OR “Handicapped Children” OR “Children with Disability” OR “Children with Disabilities” OR “Adolescent” OR “Adolescents” OR “Teens” OR “Teen” OR “Teenagers” OR “Teenager” OR “Youth” OR “Youths” OR “Adolescence” OR “girl” OR “girls” OR “boy” OR “boys” OR “juvenile” OR “juveniles”) AND (MH “Quality of Life” OR “quality of life” OR “Life Qualities” OR “Life Quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”) AND (MH “Validation Studies” OR MH “Reproducibility of Results” OR MH “Psychometrics” OR psychometr*OR clinimetr*OR clinometr* OR “observer variation” OR “observer variation” OR “discriminant analysis” OR reliab* OR valid* OR coefficient OR “internal consistency” OR “item correlation” OR “item correlations” OR “item selection” OR “item selections” OR “item reduction” OR “item reductions” OR agreement OR precision OR imprecision OR “precise values” OR test–retest OR stability OR interrater OR inter-rater OR intrarater OR intra-rater OR intertester OR inter-tester OR intratester OR intra-tester OR interobserver OR inter-observer OR intraobserver OR intra-observer OR intertechnician OR intertechnician OR intratechnician OR intra-technician OR interexaminer OR inter-examiner OR intraexaminer OR intra-examiner OR interassay OR inter-assay OR intraassay OR intra-assay OR interindividual OR inter-individual OR intraindividual OR intra-individual OR interparticipant OR inter-participant OR intraparticipant OR intra-participant OR kappa OR kappas OR “coefficient of variation” OR repeatab* OR generaliza* OR generalisa* OR concordance OR discriminative OR “known group” OR “factor analysis” OR “factor analyses” OR “factor structure” OR “factor structures” OR dimensionality OR subscale* OR “multitrait scaling analysis” OR “multitrait scaling analyses” OR “item discriminant” OR “interscale correlation” OR “interscale correlations” OR “individual variability” OR “interval variability” OR “rate variability” OR “variability analysis” OR “standard error of measurement” OR sensitiv* OR responsive* OR “minimal detectable concentration” OR interpreta* OR “meaningful change” OR “minimal important change” OR “minimal important difference” OR “minimally important change” OR “minimally important difference” OR “minimal detectable change” OR “minimal detectable difference” OR “minimally detectable change” OR “minimally detectable difference” OR “minimal real change” OR “minimal real difference” OR “minimally real change” OR “minimally real difference” OR “ceiling effect” OR “floor effect” OR “Item response model” OR IRT OR Rasch OR “Differential item functioning” OR DIF OR “computer adaptive testing” OR “item bank” OR “cross cultural equivalence”) NOT (“cognition disorder” OR “cognition disorders” OR “cognitive defects” OR “cognitive deficit” OR “cognitive disability” OR “cognitive disorder” OR “cognitive disorders” OR “cognitive dysfunction” OR “cognitive impairment” OR “delirium” OR “dementia” OR “amnestic” OR “cognitive disorders” OR “overinclusion” OR “response interference” OR “Cognition Disorders” OR “Cognition Disorders” OR “Auditory Perceptual Disorder” OR “Psychoacoustical Disorders” OR “Psychoacoustical Disorder” OR “Auditory Comprehension Disorder” OR “Auditory Comprehension Disorders” OR “Auditory Processing Disorder” OR “Auditory Processing Disorders” OR “Acoustic Perceptual Disorder” OR “Acoustic Perceptual Disorders” OR “Auditory Inattention” OR “Auditory Inattentions” OR “Huntington Disease” OR “Huntington Chorea” OR “Huntington”s Disease” OR “Huntington Chronic Progressive Hereditary Chorea” OR “Chronic Progressive Hereditary Chorea” OR “Huntington”s Chorea” OR “Late-Onset Huntington Disease” OR “Late Onset Huntington Disease” OR “Juvenile Huntington Disease” OR “Juvenile-Onset Huntington Disease” OR “Juvenile Onset Huntington Disease” OR “Akinetic-Rigid Variant of Huntington Disease” OR “Akinetic Rigid Variant of Huntington Disease” OR “Dementia”OR “Delirium” OR “Amnesia” OR “Dementias” OR “Amentia” OR “Amentias” OR “Deliriums” OR MH “Tinnitus” OR MH “Otitis Media” OR “Tinnitus” OR “Middle Ear Inflammation” OR “ear buzzing” OR “false latent otitis” OR “middle ear infection” OR “middle ear infections” OR “tympanitis”)
Grey Literature Search
Proquest Dissertations and Theses
TI,AB(Deaf OR deafness OR “Complete Hearing Loss” OR “Prelingual Deafness” OR “Deaf-Mutism” OR “Deaf Mutism” OR “Extreme Hearing Loss”) AND TI,AB(child OR children OR infant* OR adolescen* OR pediatrics OR teen* OR youth OR youths OR girl* OR boy* OR juvenile*) AND TI,AB(“Quality of Life” OR “life qualities” OR “life quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”)
FirstSearch Proceedings
(kw: deaf OR kw: deafness OR kw: complete w hearing w loss OR kw: prelingual w deafness OR kw: deaf-mutism OR kw: deaf w mutism OR kw: extreme w hearing w loss) AND (kw: child OR kw: children OR kw: infant OR kw: adolescent OR kw: pediatric OR kw: youth OR kw: girls OR kw: boys OR kw: juvenile OR kw: juveniles) AND (kw: quality w1 life OR kw: life w qualities OR kw: life w quality OR kw: HRQL OR kw: health w related w quality w1 life OR kw: HRQOL) and ln= “english”
ClinicalTrials.Gov
(Deaf OR deafness) AND (child OR children OR infant* OR adolescen* OR pediatrics OR teen OR juvenile*) AND (“Quality of Life” OR “life qualities” OR “life quality” OR “HRQL” OR “health related quality of life” OR “HRQOL”)
Footnotes
Conflicts of interest: none
Parts of this work will be presented at the American Academy of Otolaryngology-Head and Neck Surgery Annual Meeting, September 27–30, Dallas, Texas
References
- 1.Mehra S, Eavey RD, Keamy DG. The epidemiology of hearing impairment in the United States: newborns, children, and adolescents. Otolaryngology-Head and Neck Surgery. 2009;140(4):461–472. doi: 10.1016/j.otohns.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 2.Woodcock K, Pole JD. Educational attainment, labour force status and injury: a comparison of Canadians with and without deafness and hearing loss. International Journal of Rehabilitation Research. 2008;31(4):297–304. doi: 10.1097/MRR.0b013e3282fb7d4d. [DOI] [PubMed] [Google Scholar]
- 3.The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 5.Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000 [Google Scholar]
- 6.Hilliard ME, Lawrence JM, Modi AC, et al. Identification of minimal clinically important difference scores of the PedsQL in children, adolescents, and young adults with type 1 and type 2 diabetes. Diabetes care. 2013;36(7):1891–1897. doi: 10.2337/dc12-1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubba H, Swan IR, Gatehouse S. The Glasgow Children’s Benefit Inventory: a new instrument for assessing health-related benefit after an intervention. Annals of Otology, Rhinology & Laryngology. 2004;113(12):980–986. doi: 10.1177/000348940411301208. [DOI] [PubMed] [Google Scholar]
- 8.Furlong WJ, Feeny DH, Torrance GW, Barr RD. The Health Utilities Index (HUI®) system for assessing health-related quality of life in clinical studies. Annals of medicine. 2001;33(5):375–384. doi: 10.3109/07853890109002092. [DOI] [PubMed] [Google Scholar]
- 9.Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single‐attribute utility functions for the health utilities index mark 3 system. Medical care. 2002;40(2):113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Varni JW, Seid M, Kurtin PS. PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Medical care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Umansky AM, Jeffe DB, Lieu JE. The HEAR-QL: quality of life questionnaire for children with hearing loss. Journal of the American Academy of Audiology. 2011;22(10):644. doi: 10.3766/jaaa.22.10.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gatehouse S, Noble W. The Speech, Spatial and Qualities of Hearing Scale (SSQ) Int J Audiol. 2004;43(2):85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dun CA, de Wolf MJ, Mylanus EA, Snik AF, Hol MK, Cremers CW. Bilateral bone-anchored hearing aid application in children: the Nijmegen experience from 1996 to 2008. Otol Neurotol. 2010;31(4):615–623. doi: 10.1097/MAO.0b013e3181dbb37e. [DOI] [PubMed] [Google Scholar]
- 14.Fan Y, Zhang Y, Wang P, et al. The Efficacy of Unilateral Bone-Anchored Hearing Devices in Chinese Mandarin-Speaking Patients With Bilateral Aural Atresia. JAMA Otolaryngology–Head & Neck Surgery. 2014;140(4):357–362. doi: 10.1001/jamaoto.2013.6642. [DOI] [PubMed] [Google Scholar]
- 15.Ricci G, Della VA, Faralli M, et al. Results and complications of the Baha system (bone-anchored hearing aid) European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2010;267(10):1539–1545. doi: 10.1007/s00405-010-1293-0. [DOI] [PubMed] [Google Scholar]
- 16.Doshi J, Banga R, Child A, et al. Quality-of-life outcomes after bone-anchored hearing device surgery in children with single-sided sensorineural deafness. Otol Neurotol. 2013;34(1):100–103. doi: 10.1097/MAO.0b013e318277a3dd. [DOI] [PubMed] [Google Scholar]
- 17.de Wolf MJ, Hol MK, Mylanus EA, Snik AF, Cremers CW. Benefit and quality of life after bone-anchored hearing aid fitting in children with unilateral or bilateral hearing impairment. Arch Otolaryngol Head Neck Surg. 2011;137(2):130–138. doi: 10.1001/archoto.2010.252. [DOI] [PubMed] [Google Scholar]
- 18.Banga R, Doshi J, Child A, Pendleton E, Reid A, McDermott AL. Bone-anchored hearing devices in children with unilateral conductive hearing loss: a patient-carer perspective. Ann Otol Rhinol Laryngol. 2013;122(9):582–587. doi: 10.1177/000348941312200908. [DOI] [PubMed] [Google Scholar]
- 19.Kunst SJW, Leijendeckers JM, Mylanus EAM, Hol MKS, Snik AFM, Cremers CWRJ. Bone-Anchored Hearing Aid System Application for Unilateral Congenital Conductive Hearing Impairment: Audiometric Results. Otology & Neurotology. 2008;29(1):2–7. doi: 10.1097/mao.0b013e31815ee29a. [DOI] [PubMed] [Google Scholar]
- 20.Rajendran V, Roy FG, Jeevanantham D. Postural control, motor skills, and health-related quality of life in children with hearing impairment: a systematic review. European Archives of Oto-Rhino-Laryngology. 2012;269(4):1063–1071. doi: 10.1007/s00405-011-1815-4. [DOI] [PubMed] [Google Scholar]
- 21.Morettin M, Santos MJDd, Stefanini MR, Antonio FdL, Bevilacqua MC, Cardoso MRA. Measures of quality of life in children with cochlear implant: systematic review. Braz J Otorhinolaryngol. 2013;79(3):375–381. doi: 10.5935/1808-8694.20130066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Umansky AM, Jeffe DB, Lieu JE. The HEAR-QL: quality of life questionnaire for children with hearing loss. J Am Acad Audiol. 2011;22(10):644–653. doi: 10.3766/jaaa.22.10.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rachakonda T, Jeffe DB, Shin JJ, et al. Validity, discriminative ability, and reliability of the hearing‐related quality of life questionnaire for adolescents. The Laryngoscope. 2014;124(2):570–578. doi: 10.1002/lary.24336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borton SA, Mauze E, Lieu JE. Quality of life in children with unilateral hearing loss: a pilot study. Am J Audiol. 2010;19(1):61–72. doi: 10.1044/1059-0889(2010/07-0043). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elbasan B, Duzgun I, Oskay D. Is There any Difference in Health Related Quality of Life, Self Care and Social Function in Children with Different Disabilities Living in Turkey? Iran J Pediatr. 2013;23(3):281–288. [PMC free article] [PubMed] [Google Scholar]
- 26.Fellinger J, Holzinger D, Sattel H, Laucht M. Mental health and quality of life in deaf pupils. European child & adolescent psychiatry. 2008;17(7):414–423. doi: 10.1007/s00787-008-0683-y. [DOI] [PubMed] [Google Scholar]
- 27.Huber M. Health-related quality of life of Austrian children and adolescents with cochlear implants. Int J Pediatr Otorhinolaryngol. 2005;69(8):1089–1101. doi: 10.1016/j.ijporl.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 28.Lovett RE, Kitterick PT, Hewitt CE, Summerfield AQ. Bilateral or unilateral cochlear implantation for deaf children: an observational study. Archives of Disease in Childhood. 2010;95(2):107–112. doi: 10.1136/adc.2009.160325. [DOI] [PubMed] [Google Scholar]
- 29.Loy B, Warner-Czyz AD, Tong L, Tobey EA, Roland PS. The children speak: an examination of the quality of life of pediatric cochlear implant users. Otolaryngol Head Neck Surg. 2010;142(2):247–253. doi: 10.1016/j.otohns.2009.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petrou S, McCann D, Law CM, Watkin PM, Worsfold S, Kennedy CR. Health status and health-related quality of life preference-based outcomes of children who are aged 7 to 9 years and have bilateral permanent childhood hearing impairment. Pediatrics. 2007;120(5):1044–1052. doi: 10.1542/peds.2007-0159. [DOI] [PubMed] [Google Scholar]
- 31.Schick B, Skalicky A, Edwards T, Kushalnagar P, Topolski T, Patrick D. School placement and perceived quality of life in youth who are deaf or hard of hearing. J Deaf Stud Deaf Educ. 2012:ens039. doi: 10.1093/deafed/ens039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wake M, Hughes EK, Collins CM, Poulakis Z. Parent-reported health-related quality of life in children with congenital hearing loss: a population study. Ambul Pediatr. 2004;4(5):411–417. doi: 10.1367/A03-191R.1. [DOI] [PubMed] [Google Scholar]
- 33.Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of children with mild-profound congenital hearing loss at 7 to 8 years: a population study. Ear Hear. 2004;25(1):1–8. doi: 10.1097/01.AUD.0000111262.12219.2F. [DOI] [PubMed] [Google Scholar]
- 34.Wake M, Tobin S, Cone-Wesson B, et al. Slight/mild sensorineural hearing loss in children. Pediatrics. 2006;118(5):1842–1851. doi: 10.1542/peds.2005-3168. [DOI] [PubMed] [Google Scholar]
- 35.Warner-Czyz AD, Loy B, Roland PS, Tong L, Tobey EA. Parent versus child assessment of quality of life in children using cochlear implants. Int J Pediatr Otorhinolaryngol. 2009;73(10):1423–1429. doi: 10.1016/j.ijporl.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hintermair M. Health-related quality of life and classroom participation of deaf and hard-of-hearing students in general schools. J Deaf Stud Deaf Educ. 2011;16(2):254–271. doi: 10.1093/deafed/enq045. [DOI] [PubMed] [Google Scholar]
- 37.Clark JH, Wang N-Y, Riley AW, et al. Timing of cochlear implantation and parents’ global ratings of children’s health and development. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2012;33(4):545. doi: 10.1097/MAO.0b013e3182522906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ricci G, Volpe AD, Faralli M, et al. Bone-anchored hearing aids (Baha) in congenital aural atresia: personal experience. Int J Pediatr Otorhinolaryngol. 2011;75(3):342–346. doi: 10.1016/j.ijporl.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 39.Barton GR, Stacey PC, Fortnum HM, Summerfield AQ. Hearing-impaired children in the United Kingdom, IV: cost-effectiveness of pediatric cochlear implantation. Ear Hear. 2006;27(5):575–588. doi: 10.1097/01.aud.0000233967.11072.24. [DOI] [PubMed] [Google Scholar]
- 40.Stacey PC, Fortnum HM, Barton GR, Summerfield AQ. Hearing-impaired children in the United Kingdom, I: Auditory performance, communication skills, educational achievements, quality of life, and cochlear implantation. Ear Hear. 2006;27(2):161–186. doi: 10.1097/01.aud.0000202353.37567.b4. [DOI] [PubMed] [Google Scholar]
- 41.Cheng AK, Rubin HR, Powe NR, Mellon NK, Francis HW, Niparko JK. Cost-utility analysis of the cochlear implant in children. JAMA. 2000;284(7):850–856. doi: 10.1001/jama.284.7.850. [DOI] [PubMed] [Google Scholar]
- 42.Huttunen K, Rimmanen S, Vikman S, et al. Parents’ views on the quality of life of their children 2–3 years after cochlear implantation. Int J Pediatr Otorhinolaryngol. 2009;73(12):1786–1794. doi: 10.1016/j.ijporl.2009.09.038. [DOI] [PubMed] [Google Scholar]
- 43.Sach TH, Barton GR. Interpreting parental proxy reports of (health-related) quality of life for children with unilateral cochlear implants. Int J Pediatr Otorhinolaryngol. 2007;71(3):435–445. doi: 10.1016/j.ijporl.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 44.Schorr EA, Roth FP, Fox NA. Quality of life for children with cochlear implants: perceived benefits and problems and the perception of single words and emotional sounds. J Speech Lang Hear Res. 2009;52(1):141–152. doi: 10.1044/1092-4388(2008/07-0213). [DOI] [PubMed] [Google Scholar]
- 45.Necula V, Cosgarea M, Stanciu A. Health-Related Quality of Life in Romanian Cochlear Implanted Patients. Otolaryngology–Head and Neck Surgery. 2012;147(2 suppl):P210–P211. [Google Scholar]
- 46.Briggs L, Davidson L, Lieu JE. Outcomes of conventional amplification for pediatric unilateral hearing loss. Ann Otol Rhinol Laryngol. 2011;120(7):448–454. doi: 10.1177/000348941112000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sparreboom M, Snik AF, Mylanus EA. Sequential bilateral cochlear implantation in children: quality of life. Archives of Otolaryngology–Head & Neck Surgery. 2012;138(2):134–141. doi: 10.1001/archoto.2011.229. [DOI] [PubMed] [Google Scholar]
- 48.Beijen J-W, Snik AF, Mylanus EA. Sound localization ability of young children with bilateral cochlear implants. Otology & Neurotology. 2007;28(4):479–485. doi: 10.1097/MAO.0b013e3180430179. [DOI] [PubMed] [Google Scholar]
- 49.Keilmann A, Limberger A, Mann WJ. Psychological and physical well-being in hearing-impaired children. Int J Pediatr Otorhinolaryngol. 2007;71(11):1747–1752. doi: 10.1016/j.ijporl.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 50.Korver AM, Konings S, Dekker FW, et al. Newborn hearing screening vs later hearing screening and developmental outcomes in children with permanent childhood hearing impairment. JAMA. 2010;304(15):1701–1708. doi: 10.1001/jama.2010.1501. [DOI] [PubMed] [Google Scholar]
- 51.Kushalnagar P, Topolski TD, Schick B, Edwards T, Skalicky A, Patrick DL. Mode of communication, perceived level of understanding, and perceived quality of life in youth who are deaf or hard of hearing. J Deaf Stud Deaf Educ. 2011;16(4):512–523. doi: 10.1093/deafed/enr015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meyer A, Sie K, Skalicky A, et al. Quality of life in youth with severe to profound sensorineural hearing loss. JAMA Otolaryngol Head Neck Surg. 2013;139(3):294–300. doi: 10.1001/jamaoto.2013.35. [DOI] [PubMed] [Google Scholar]
- 53.Patrick DL, Edwards TC, Skalicky AM, et al. Validation of a quality-of-life measure for deaf or hard of hearing youth. Otolaryngol Head Neck Surg. 2011;145(1):137–145. doi: 10.1177/0194599810397604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith-Olinde L, Grosse SD, Olinde F, Martin PF, Tilford JM. Health state preference scores for children with permanent childhood hearing loss: a comparative analysis of the QWB and HUI3. Qual Life Res. 2008;17(6):943–953. doi: 10.1007/s11136-008-9358-x. [DOI] [PubMed] [Google Scholar]
- 55.Warner-Czyz AD, Loy B, Tobey EA, Nakonezny P, Roland PS. Health-related quality of life in children and adolescents who use cochlear implants. Int J Pediatr Otorhinolaryngol. 2011;75(1):95–105. doi: 10.1016/j.ijporl.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 56.Rajendran V, Roy FG. Comparison of health related quality of life of primary school deaf children with and without motor impairment. Ital J Pediatr. 2010;36:75. doi: 10.1186/1824-7288-36-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Borton SA, Mauze E, Lieu JEC. Quality of Life in Children With Unilateral Hearing Loss: A Pilot Study. American Journal of Audiology. 2010;19(1):61–72. doi: 10.1044/1059-0889(2010/07-0043). [DOI] [PMC free article] [PubMed] [Google Scholar]


