Abstract
Objective
Unplanned hospital readmissions following surgical interventions are associated with adverse events and contribute to increasing healthcare costs. Despite numerous studies defining risk factors following lower extremity bypass surgery, evidence regarding readmission after endovascular interventions is limited. This study aims to identify predictors of 30-day unplanned readmission following infrainguinal endovascular interventions.
Methods
We identified all patients undergoing an infrainguinal endovascular intervention in the Targeted Vascular module of the American College of Surgeons National Surgical Quality Improvement Program between 2012 and 2014. Perioperative outcomes were stratified by symptom status (chronic limb-threatening ischemia [CLI] vs. claudication). Patients who died during index admission, and those who remained in the hospital after 30 days, were excluded. Indications for unplanned readmission related to the index procedure were evaluated. Multivariable logistic regression was used to identify preoperative and in-hospital (during index admission) risk factors of 30-day unplanned readmission.
Results
4449 patients underwent infrainguinal endovascular intervention, of which 2802 (63%) had CLI (66% tissue loss) and 1647 (37%) had claudication. The unplanned readmission rates for CLI and claudication patients were 16% (N=447) and 6.5% (N=107), respectively. Mortality after index admission was higher for readmitted patients compared to those not readmitted (CLI: 3.4% vs. 0.7%, P < .001; claudication: 2.8% vs. 0.1%, P < .01). Approximately 50% of all unplanned readmissions were related to the index procedure. Among CLI patients, the most common indication for readmission related to the index procedure was wound- or infection-related (42%), while patients with claudication were mainly readmitted for recurrent symptoms of peripheral vascular disease (28%). In patients with CLI, predictors of unplanned readmission included diabetes (OR: 1.3, 95% CI: 1.01–1.6), congestive heart failure (1.6, 1.1–2.5), renal insufficiency (1.7, 1.3–2.2), preoperative dialysis (1.4, 1.02–1.9), tibial angioplasty/stenting (1.3, 1.04–1.6), in-hospital bleeding (1.9, 1.04–3.5), in-hospital unplanned return to the operating room (1.9, 1.1–3.5), and discharge other than home (1.5, 1.1–2.0). Risk factors for those with claudication were dependent functional status (3.5, 1.4–8.7), smoking (1.6, 1.02–2.5), diabetes (1.5, 1.01–2.3), preoperative dialysis (3.6, 1.6–8.3), procedure time exceeding 120 minutes (1.8, 1.1–2.7), in-hospital bleeding (2.9, 1.2–7.4), and in-hospital unplanned return to the operating room (3.4, 1.2–9.4).
Conclusions
Unplanned readmission after endovascular treatment is relatively common, especially in patients with CLI, and is associated with substantially increased mortality. Awareness of these risk factors will help providers identify patients at high-risk who may benefit from early surveillance and prophylactic measures focused on decreasing postoperative complications may reduce the rate of readmission.
Introduction
Unplanned readmissions following surgical intervention are associated with poor outcomes and additional healthcare costs.1 In 2004, it was estimated that the costs of potentially avoidable re-hospitalizations were as high as 17.4 billion dollars among Medicare beneficiaries.2 Consequently, several regional and national initiatives began focusing on this issue.3,4 The federal government also made this issue a priority with the Hospital Readmission Reduction Program, introduced in 2012 as a part of the Affordable Care Act, which was initiated to impose financial penalties against hospitals with excessive readmissions within 30 days of discharge for Medicare beneficiaries. An algorithm was developed to omit planned readmissions from the penalty calculation; however, hospitals are accountable for all-cause unplanned readmissions, including those not related to the initial admission. While the readmission rates nationwide remained stable between 2007–2011, after initiation of this policy, rates declined slightly by 0.5%.5 Within this act, conditions known to have a particularly high risk of readmission (myocardial infarction, heart failure, and pneumonia) were identified as target areas, with vascular procedures as a likely target in the near future. Subsequently, the readmission rate continued to decline in 2015 for both targeted and non-targeted conditions, with 17.8% and 13.1% of all Medicare beneficiaries readmitted within 30 days, respectively.6
Readmission following vascular surgery is higher than other major operations, with prior reports citing a range of 18% to 24%, compared to 10% for general, bariatric, and colorectal surgery.1,2 Among vascular surgery patients, those undergoing lower extremity open or endovascular procedures have amongst the highest risk for readmission with a reported rate of 23%, third only to congestive heart failure and psychoses. Previous studies have identified several risk factors following infrainguinal bypass surgery, including: age, diabetes, renal insufficiency, critical limb ischemia, return to the operating room during the index admission, and longer hospital stay.7–12 Despite endovascular procedures now being the most commonly used method for lower extremity revascularization, predictors of readmission after infrainguinal endovascular intervention are limited.13,14 While Davenport et al. analyzed readmission data for both open and endovascular interventions, no predictors specific to endovascular procedures were identified.15 In addition, Vogel et al. only evaluated outcomes in a limited set of patients who underwent tibioperoneal angioplasty for chronic limb-threatening ischemia in the US Medicare population.16
Therefore, the purpose of this study was to assess the incidence of 30-day unplanned readmission following infrainguinal endovascular intervention and to identify preoperative and in-hospital risk factors using a large national representative clinical registry.
Methods
Data source
Patients were identified using the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Targeted Vascular module. NSQIP is a prospective clinical registry of surgical perioperative outcomes collected nationwide for the purpose of quality assessment and improvement. The registry consists of patient demographic, operative, and postoperative variables up to 30 days after surgery. Additionally, the Targeted Vascular module contains detailed anatomic and intraoperative characteristics, as well as procedure-related outcomes from 83 participating sites. According to NSQIP protocol, trained clinical nurses first identify surgical procedures by reviewing operative case logs then collect data and categorize these procedures using Current Procedural Terminology (CPT) codes. While not all cases are included, a systematic sampling system was developed by NSQIP to select cases and prevent bias in selection. Data collection and quality control have been validated by annual audits and previous reports.17–19 In 2011, NSQIP began collecting 30-day readmission events; however, the time to readmission, indication, and whether the readmission was related to the principal procedure only became available in 2012. Therefore, the data were evaluated for 2012–2014 only. Readmission data captured by NSQIP have been previously validated.4 More details on this registry can be found at www.acsnsqip.org. The Beth Israel Deaconess Medical Center Institutional Review Board approved this study with informed consent waived due to the de-identified nature of NSQIP.
Patients
Patients undergoing an infrainguinal endovascular intervention as a principal procedure were included (CPT: 37224–37233). Extra procedural detail regarding treatment approach was not captured by NSQIP, which precluded us from determining whether the endovascular intervention was a percutaneous or an open procedure. Those not at risk for readmission due to death during the index admission (N=75; 1.7%) or patients with a hospital stay longer than 30 days (N=51; 1.1%) were excluded from the analysis. We stratified patients by symptom status, either intermittent claudication or chronic limb-threatening ischemia (CLI). Patients with and without unplanned readmission were compared on baseline characteristics, intraoperative details, and postoperative outcomes.
Pre- and intraoperative characteristics
Baseline characteristics consisted of demographics, comorbidities, and pre-procedural medication. Age was considered as a categorical and a continuous variable; however, all patients 90 years of age or older are recorded as 90+ by NSQIP to prevent individual patient identification. Smoking included current tobacco use or within the last year prior to intervention. Preoperative documentation of an open wound or infection was captured, although the location could not be determined with NSQIP data. Dependent functional status was defined as partial or total assistance for activities of daily living (ADL) captured within 30 days prior to the procedure. Intraoperative details captured were type of procedure, the American Society of Anesthesiologist (ASA) class, procedure time, and whether the procedure was elective. Concurrent procedures were identified with corresponding CPT codes (Supplemental table I); however, we were unable to distinguish whether the concomitant procedure was ipsilateral or contralateral based on these billing codes.
Readmissions
The primary outcome was any unplanned readmission within 30 days of the principal endovascular procedure to any hospital, which will be referred to as unplanned readmission in this manuscript. Unplanned readmission was captured by a NSQIP variable and excluded elective or planned readmissions. In addition, unplanned readmissions were further categorized within NSQIP as related or unrelated to the principal procedure and this distinction cannot be made for planned readmissions. Related unplanned readmission indications were determined with a specific list of NSQIP complications or International Classification of Diseases (ICD-9) codes (Supplemental table II). Limb-related readmissions were defined as all readmissions related to the ipsilateral index limb or endovascular procedure. An infection or wound complication refers to a composite variable using ICD-9 codes, which subsequently does not allow us to differentiate between pre-existing wounds or postoperative complications. We defined recurrent symptoms of peripheral vascular disease as worsening of peripheral vascular symptoms likely related to atherosclerotic disease, stenosis, occlusion, or failure of treatment.
Outcomes
Other postoperative outcomes included mortality after index admission and 30-day adverse events. Both 30-day and in-hospital (during the index admission) complications were captured, provided that a time-to-event variable was documented. Major adverse limb event (MALE) refers to a composite variable containing major amputation (above or below knee) and/or major reintervention (new or revision bypass graft, thrombectomy or thrombolysis, or major surgical revision such as jump or interposition graft). Surgical site infection or complication included any surgical site infection or wound dehiscence. Bleeding was defined as any transfusion or secondary procedure with the indication of bleeding. A respiratory complication was considered present when one of the following was documented: pneumonia, unplanned reintubation, or ventilator requirement >48 hours. Any complication included myocardial infarction, stroke, bleeding, surgical site infection or complication, renal deterioration (creatinine >2mg/dL and/or need for dialysis), respiratory complications, sepsis, septic shock, untreated loss of patency, and unplanned return to the operating room. Discharge other than home was defined as any discharge to a skilled or unskilled nursing facility in those patients who were originally admitted from home. These variable definitions were determined by NSQIP prior to data collection and thus were not modifiable.
Statistical analysis
Differences between patients with and without unplanned readmission were determined using the Pearson’s χ2 and Fisher’s exact test for categorical variables, while continuous variables were analyzed by Student’s t-test and Mann Whitney U test, where appropriate. Multivariable logistic regression was performed to establish independent associations with 30-day unplanned readmission. For adjusted analysis, models were constructed using purposeful selection of covariates, incorporating backward elimination after univariate testing (P-value = ≤.1).20 Separate regression models were constructed for patients with CLI and claudication and the cut-off value for procedure time and length of stay was the 75th percentile. Statistical significance was defined as P-value < .05 (two-sided test). Analyses were conducted with SPSS Statistics 23 (IBM Inc., Chicago, IL).
Results
A total of 4449 patients were included in the study, of which 63% (N=2802) had CLI (66% of these had tissue loss) and 37% (N=1647) had claudication. Among patients with CLI, the 30-day unplanned readmission rate was 16% (N=447), and of those patients 5.1% (N=23) were readmitted more than once. The unplanned readmission rate in patients with claudication was 6.5% (N=107), and of those patients 2.8% (N=3) had more than one readmission. To put this into perspective, planned readmissions within 30 days occurred in 2.2% (N=62) for CLI patients and in 1.5% (N=25) in those with claudication.
Baseline characteristics
Table I summarizes patients’ baseline characteristics. Compared to CLI patients without an unplanned readmission, those with an unplanned readmission were less likely to be white (53% vs. 60%, P = .04), more often functionally dependent (19% vs. 15%, P = .02), and more frequently had tissue loss (71% vs. 65%, P = .02). Patients who were readmitted more often had diabetes (70% vs. 61%, P < .001), congestive heart failure (7.4% vs. 3.9%, P = .001), renal insufficiency (49% vs. 31%, P < .001), dialysis (24% vs. 12%, P < .001), and a preoperative open wound or infection (60% vs. 51%, P < .001). Finally, among patients with CLI, preoperative use of statin (73% vs. 67%, P = .02) and beta blocker medications (71% vs. 65%, P = .01) were more frequent in those readmitted.
Table I.
Baseline characteristics and comorbidities among CLI and claudication patients with and without an unplanned readmission following endovascular intervention
| CLI | Claudication | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Unplanned Readmission (N=447) | No readmission (N=2355) | P-value | Unplanned Readmission (N=107) | No readmission (N=1540) | P-value | |||||
|
| ||||||||||
| N | % | N | % | N | % | N | % | |||
| Male gender | 254 | (57) | 1330 | (57) | .89 | 63 | (59) | 957 | (62) | .50 |
| Age - (y ± SD) | 70.0 (12) | 69.9 (12) | .90 | 67.0 (10) | 67.8 (11) | 48 | ||||
| Age categories | .83 | .47 | ||||||||
| < 60 | 93 | (21) | 514 | (22) | 22 | (21) | 342 | (22) | ||
| 60 to 69 | 124 | (28) | 612 | (26) | 43 | (40) | 507 | (33) | ||
| 70 to 79 | 124 | (28) | 635 | (27) | 32 | (30) | 469 | (31) | ||
| 80 to 89 | 84 | (19) | 487 | (21) | 9 | (8.4) | 202 | (13) | ||
| > 89 | 22 | (4.9) | 107 | (4.5) | 1 | (0.9) | 20 | (1.3) | ||
| Smoking | 109 | (24) | 641 | (27) | .22 | 48 | (45) | 564 | (37) | .09 |
| BMI > 30 | 128 | (30) | 677 | (30) | .96 | 32 | (31) | 544 | (36) | .32 |
| Race | .04 | .30 | ||||||||
| White | 236 | (53) | 1409 | (60) | 69 | (65) | 1099 | (71) | ||
| Black | 102 | (23) | 441 | (19) | 19 | (18) | 220 | (14) | ||
| Hispanic | 61 | (14) | 258 | (11) | 10 | (9.3) | 79 | (5.1) | ||
| Other | 12 | (2.7) | 45 | (1.9) | 1 | (0.9) | 19 | (1.2) | ||
| Unknown/not reported | 36 | (8.1) | 202 | (8.6) | 8 | (7.5) | 123 | (8) | ||
| Symptom status | .02 | |||||||||
| CLI: rest pain | 131 | (29) | 827 | (35) | ||||||
| CLI: tissue loss | 316 | (71) | 1528 | (65) | ||||||
| Not admitted from home | 71 | (16) | 345 | (15) | .50 | 3 | (2.8) | 24 | (1.6) | .42 |
| Dependent functional status | 84 | (19) | 346 | (15) | .02 | 7 | (6.6) | 25 | (1.6) | <.001 |
|
| ||||||||||
| Hypertension | 397 | (89) | 2010 | (85) | .05 | 94 | (88) | 1286 | (84) | .24 |
| Diabetes | 312 | (70) | 1429 | (61) | <.001 | 55 | (51) | 620 | (40) | .02 |
| CHF | 33 | (7.4) | 92 | (3.9) | .001 | 4 | (3.7) | 24 | (1.6) | .10 |
| Renal insufficiency | 215 | (49) | 701 | (31) | <.001 | 24 | (25) | 246 | (17) | .05 |
| Dialysis | 106 | (24) | 282 | (12) | <.001 | 9 | (8.4) | 36 | (2.3) | <.001 |
| COPD | 51 | (11) | 227 | (9.6) | .25 | 12 | (11) | 170 | (11) | .96 |
| History of revascularization in same segment | .12 | .66 | ||||||||
| No prior revascularization | 288 | (64) | 1407 | (60) | 58 | (54) | 879 | (57) | ||
| Prior bypass surgery | 74 | (17) | 403 | (17) | 19 | (18) | 290 | (19) | ||
| Prior endovascular intervention | 85 | (19) | 545 | (23) | 30 | (28) | 371 | (24) | ||
| Preprocedural medication | ||||||||||
| Antiplatelet | 365 | (82) | 1924 | (82) | .80 | 90 | (84) | 1345 | (88) | .25 |
| Statin | 323 | (73) | 1566 | (67) | .02 | 76 | (71) | 1135 | (74) | .45 |
| Beta blocker | 317 | (71) | 1517 | (65) | .01 | 71 | (66) | 860 | (57) | .047 |
| Preoperative open wound or infection | 269 | (60) | 1199 | (51) | <.001 | 17 | (16) | 58 | (3.8) | <.001 |
y: years, SD: standard deviation, CHF: congestive heart failure, COPD: chronic obstructive pulmonary disease
In claudication patients, unplanned readmission was associated with dependent functional status (6.6% vs. 1.6%, P < .001), diabetes (51% vs. 40%, P = .02), dialysis (8.4% vs. 2.3%, P < .001), preoperative open wound or infection (16% vs. 3.8%, P < .001), and preoperative use of beta blocker medications (66% vs. 57%, P = .047).
Procedure details
Compared to CLI patients without an unplanned readmission, those who were readmitted had a significantly longer procedure time (102 min. vs. 92 min., P < .01; Table II), and were less likely to undergo an elective procedure (48% vs. 54%, P = .03). Similarly, ASA class ≥ 4 (29% vs. 21%, P < .001) and tibial angioplasty and/or stenting (34% vs. 26%, P = .001) were more common among readmitted CLI patients. In the vast majority of cases, vascular surgeons performed the procedure as opposed to other specialties (92% vs. 8%).
Table II.
Procedure details among CLI and claudication patients with and without an unplanned readmission following endovascular intervention
| CLI | Claudication | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Unplanned Readmission (N=447) | No readmission (N=2355) | P-value | Unplanned Readmission (N=107) | No readmission (N=1540) | P-value | |||||
|
| ||||||||||
| N | % | N | % | N | % | N | % | |||
| Type procedure | .001 | .046 | ||||||||
| Fem-pop angioplasty/stenting/atherectomy | 295 | (66) | 1734 | (74) | 92 | (86) | 1411 | (92) | ||
| Tibial angioplasty/stenting | 152 | (34) | 621 | (26) | 15 | (14) | 129 | (8.4) | ||
| Elective procedure | 215 | (48) | 1267 | (54) | .03 | 79 | (75) | 1377 | (89) | <.001 |
| Concurrent procedures | ||||||||||
| Open bypass | 1 | (0.2) | 12 | (0.5) | .71 | 2 | (1.9) | 7 | (0.5) | .11 |
| Thromboendarterectomy | 28 | (6.3) | 137 | (5.8) | .71 | 14 | (13) | 83 | (5.4) | .001 |
| ASA class ≥ 4 | 115 | (29) | 436 | (21) | <.001 | 22 | (24) | 119 | (8.9) | <.001 |
| Procedure time - (min ± IQR) | 102 (66–148) | 92 (63–136) | <.01 | 102 (62–161) | 81 (58–118) | <.001 | ||||
| Fem-pop angioplasty/stenting/atherectomy | 101 (66–154) | 93 (62–139) | .06 | 99 (61–190) | 80 (57–119) | <.001 | ||||
| Tibial angioplasty/stenting | 103 (67–141) | 89 (65–129) | .02 | 103 (74–137) | 82 (62–117) | .12 | ||||
min: minutes, IQR: interquartile range
Among patients with claudication, those with unplanned readmissions more often underwent tibial angioplasty and/or stenting compared to those without an unplanned readmission (14% vs. 8.4%, P = .046). In addition, readmitted patients had a longer procedure time (102 min. vs. 81 min., P < .001), and more frequently had an ASA class ≥ 4 (24% vs. 8.9%, P < .001). Vascular surgeons performed more endovascular procedures than other specialties (85% vs. 15%). Regarding concurrent procedures, readmitted patients with claudication more often underwent an additional thromboendarterectomy compared to those not readmitted (13% vs. 5.4%, P = .001).
Postoperative outcomes
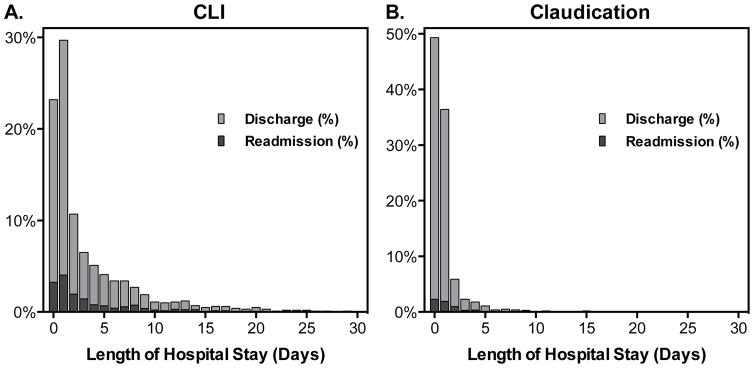
Postoperative outcomes are detailed in Table III. Mortality after index admission was higher in readmitted patients for both CLI (3.4% vs. 0.7%, P < .001) and claudication (2.8% vs. 0.1%, P < .01). Time to readmission occurred at a median of 12 days after discharge in patients with CLI (IQR: 6–19) and 13 days in those with claudication (IQR: 7–18). The 30-day rate of any complication in CLI patients with an unplanned readmission was higher than in those not readmitted (61% vs. 15%, P < .001). Readmitted patients with claudication also suffered more complications (66% vs. 4.9%, P < .001). In patients with an unplanned readmission, the following 30-day adverse events were more frequently found: MALE, major amputation, major reintervention, surgical site infection or complication, bleeding requiring transfusion or secondary procedure, myocardial infarction, stroke, progressive renal insufficiency and/or dialysis, respiratory complications, sepsis, and unplanned return to the operation room. Inhospital postoperative adverse events associated with unplanned readmission in patients with CLI and claudication were similar and included bleeding requiring transfusion or secondary procedure (CLI: 9.2% vs. 6.1%, P = .02; claudication: 8.4% vs. 1.6%, P < .001) and unplanned return to the operating room (CLI: 9.4% vs. 5.9%, P < .01; claudication: 6.5% vs. 1.2%, P < .001). The median length of hospital stay was 1 day among patients with CLI and claudication (Figure I), although those readmitted had a longer hospital stay (CLI: 2 days vs. 1 day, P < .01; claudication: 1 day vs. 0 days, P < .001).
Table III.
Postoperative outcomes among CLI and claudication patients with and without an unplanned readmission following endovascular intervention
| CLI | Claudication | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Unplanned Readmission (N=447) | No readmission (N=2355) | P-value | Unplanned Readmission (N=107) | No readmission (N=1540) | P-value | |||||
|
| ||||||||||
| N | % | N | % | N | % | N | % | |||
| Mortality after index admission | 15 | (3.4) | 17 | (0.7) | <.001 | 3 | (2.8) | 2 | (0.1) | <.01 |
| Length of stay - (d ± IQR) | 2 (1–5) | 1 (1–4) | <.01 | 1 (0–2) | 0 (0–1) | <.001 | ||||
| Discharge to home | 334 | (83) | 1952 | (88) | .001 | 99 | (95) | 1510 | (98) | .02 |
| 30-day MALE | 118 | (26) | 130 | (5.5) | <.001 | 34 | (32) | 12 | (0.8) | <.001 |
| Major amputation | 68 | (15) | 75 | (3.2) | <.001 | 5 | (4.7) | 4 | (0.3) | <.001 |
| Major reintervention | 57 | (13) | 69 | (2.9) | <.001 | 30 | (28) | 10 | (0.6) | <.001 |
|
| ||||||||||
| Surgical site infection or complication | 50 | (11) | 41 | (1.7) | <.001 | 11 | (10) | 14 | (0.9) | <.001 |
| In-hospital | 5 | (1.1) | 11 | (0.5) | .09 | 0 | (0) | 3 | (0.2) | >.99 |
| Myocardial infarction | 13 | (2.9) | 22 | (0.9) | .001 | 3 | (2.8) | 5 | (0.3) | .01 |
| In-hospital | 1 | (0.2) | 20 | (0.8) | .23 | 0 | (0) | 5 | (0.3) | >.99 |
| Stroke | 1 | (0.2) | 4 | (0.2) | .58 | 3 | (2.8) | 1 | (0.1) | .001 |
| In-hospital | 0 | (0) | 4 | (0.2) | >.99 | 0 | (0) | 1 | (0.1) | >.99 |
| Bleeding (requiring transfusion or secondary procedure) | 79 | (18) | 160 | (6.8) | <.001 | 26 | (24) | 31 | (2) | <.001 |
| In-hospital | 41 | (9.2) | 143 | (6.1) | .02 | 9 | (8.4) | 24 | (1.6) | <.001 |
| Creatinine >2 mg/dL | 12 | (2.7) | 11 | (0.5) | <.001 | 1 | (0.9) | 1 | (0.1) | .13 |
| In-hospital | 2 | (0.4) | 11 | (0.5) | >.99 | 1 | (0.9) | 1 | (0.1) | .13 |
| New dialysis dependence | 5 | (1.1) | 3 | (0.1) | <.01 | 1 | (0.9) | 1 | (0.1) | .13 |
| In-hospital | 1 | (0.2) | 3 | (0.1) | .50 | 1 | (0.9) | 1 | (0.1) | .13 |
| Respiratory complications | 24 | (5.4) | 23 | (1) | <.001 | 3 | (2.8) | 1 | (0.1) | .001 |
| In-hospital | 3 | (0.7) | 21 | (0.9) | >.99 | 1 | (0.9) | 1 | (0.1) | .13 |
| Sepsis | 20 | (4.5) | 10 | (0.4) | <.001 | 2 | (1.9) | 0 | (0) | <.01 |
| In-hospital | 0 | (0) | 9 | (0.4) | .37 | 1 | (0.9) | 0 | (0) | .07 |
| Septic shock | 8 | (1.8) | 2 | (0.1) | <.001 | 3 | (2.8) | 0 | (0) | <.001 |
| In-hospital | 1 | (0.2) | 1 | (0) | .29 | 1 | (0.9) | 0 | (0) | .07 |
| Untreated loss of patency | 13 | (2.9) | 35 | (1.5) | .03 | 2 | (1.9) | 10 | (0.6) | .18 |
| In-hospital | 1 | (0.2) | 14 | (0.6) | .49 | 0 | (0) | 1 | (0.1) | >.99 |
| Unplanned return to the operating room | 198 | (44) | 174 | (7.4) | <.001 | 56 | (52) | 29 | (1.9) | <.001 |
| In-hospital | 42 | (9.4) | 139 | (5.9) | <.01 | 7 | (6.5) | 19 | (1.2) | <.001 |
|
| ||||||||||
| Any complication | 274 | (61) | 362 | (15) | <.001 | 71 | (66) | 76 | (4.9) | <.001 |
| In-hospital | 70 | (16) | 271 | (12) | .01 | 13 | (12) | 42 | (2.7) | <.001 |
d: days, IQR: interquartile range, MALE: major adverse limb event
Figure I.
Proportions of discharge and readmission at different lengths of hospital stay after endovascular intervention for patients with A. CLI and B. claudication
Indications for readmission
Of all unplanned readmissions, approximately half were considered related to the index endovascular procedure in patients with CLI (49%) and claudication (53%). Indications for readmission varied by symptom status and are listed in Table IV. In CLI patients, readmissions were limb-related in 72%, which included 42% infection or wound complications, and 14% due to recurrent symptoms of peripheral vascular disease. Readmission indications in patients with claudication were also primarily limb-related (68%), with 8.8% readmitted due to infection or wound complications and 28% of patients readmitted for recurrent symptoms of peripheral vascular disease.
Table IV.
Indications of 30-day unplanned related readmissions among patients with CLI and claudication following endovascular intervention
| CLI (N=220) | Claudication (N=57) | |||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Limb-related readmissions | 158 | (72) | 39 | (68) |
| Infection or wound complications | 92 | (42) | 5 | (8.8) |
| Recurrent symptoms of peripheral vascular disease | 30 | (14) | 16 | (28) |
| Other vascular complications | 36 | (16) | 18 | (32) |
| Sepsis | 12 | (5.5) | 3 | (5.3) |
| Other readmissions | 45 | (21) | 12 | (21) |
| Unknown indication | 5 | (2.3) | 3 | (5.3) |
Predictors of unplanned readmission
Multivariable predictors of 30-day unplanned readmission are listed in Table V. Preoperative independent risk factors of any unplanned readmission in patients with CLI were diabetes (OR: 1.3, 95% CI: 1.01–1.6), congestive heart failure (OR: 1.6, 95% CI: 1.1–2.5), renal insufficiency (OR: 1.7, 95% CI: 1.3–2.2), and preoperative dialysis (OR: 1.4, 95% CI: 1.02–1.9). Intraoperatively, tibial angioplasty and/or stenting (OR: 1.3, 95% CI: 1.04–1.6) was also associated with an increased risk of unplanned readmission. Additional pre-discharge risk factors were in-hospital bleeding (OR: 1.9, 95% CI: 1.04–3.5) and unplanned return to the operating room (OR: 1.9, 95% CI: 1.1–3.5). Finally, discharge other than home was associated with unplanned readmission in CLI patients (OR: 1.5, 95% CI: 1.1–2.0).
Table VA.
Independent predictors of 30-day unplanned readmission following endovascular intervention in patients with CLI
| CLI | |||
|---|---|---|---|
|
| |||
| Variable | OR | 95% CI | P-value |
| Diabetes | 1.3 | 1.01–1.6 | .04 |
| Congestive heart failure | 1.6 | 1.1–2.5 | .03 |
| Renal insufficiency | 1.7 | 1.3–2.2 | <.001 |
| Preoperative dialysis | 1.4 | 1.02–1.9 | .04 |
| Tibial angioplasty/stenting | 1.3 | 1.04–1.6 | .02 |
| In-hospital bleeding | 1.9 | 1.04–3.5 | .04 |
| In-hospital unplanned return to the operation room | 1.9 | 1.1–3.5 | .03 |
| Discharge other than home | 1.5 | 1.1–2.0 | <.01 |
Adjusted for: age, gender, symptom status, race, history of ipsilateral revascularization, procedure time exceeding 140 min (75th percentile), length of stay longer than 4 days (75th percentile), inhospital surgical site infection or complication
Among patients with claudication, predictors of any unplanned readmission included dependent functional status (OR: 3.5, 95% CI: 1.4–8.7), smoking (OR: 1.6, 95% CI: 1.02–2.5), diabetes (OR: 1.5, 95% CI: 1.01–2.3), preoperative dialysis (OR: 3.6, 95% CI: 1.6–8.3), and procedure time exceeding 120 minutes (OR: 1.8, 95% CI: 1.1–2.7). Similar to patients with CLI, unplanned readmission in those with claudication was also independently associated with pre- discharge complications, such as in-hospital bleeding (OR: 2.9, 95% CI: 1.2–7.4) and in-hospital unplanned return to the operating room (OR: 3.4, 95% CI: 1.2–9.4).
Discussion
This study demonstrates that 30-day unplanned readmission after infrainguinal endovascular intervention is relatively common for CLI (1 in 6 patients) and claudication (1 in 15 patients). Also, mortality and morbidity after index admission were significantly worse in those readmitted. Adjusted analysis demonstrated that diabetes, congestive heart failure, renal insufficiency, preoperative dialysis, and tibial angioplasty and/or stenting were independent predictors of unplanned readmission in CLI patients. Other risk factors included postoperative adverse events, such as in-hospital bleeding, in-hospital unplanned return to the operating room, and discharge other than home. Among patients with claudication, risk factors for unplanned readmission were dependent functional status, smoking, diabetes, preoperative dialysis, and procedure time exceeding 120 minutes, as well as in-hospital factors, such as bleeding and unplanned return to the operating room.
Several other studies have evaluated readmission rates of endovascular procedures, although few of these stratified by symptom status and whether a readmission was planned or unplanned. An analysis between 2008–2010 of the Health Facts database, which records longitudinal patient data from over 480 contributing institutions throughout the U.S., found a readmission rate of 19% in 251 patients with CLI and 11% in 221 claudication patients undergoing endovascular intervention, whereas a single-institution study of 137 endovascular interventions, showed that 12% of CLI and 2.2% of claudication patients were readmitted.21,22 Our rates of 16% in patients with CLI and 6.5% in those with claudication fall well within these reported ranges. The variation may be partly attributable to differences in follow-up time, namely 30 days from discharge (both previous studies) rather than from the procedure, which was assessed in the current study. Our rates may be higher than those reported from Jackson et al.22 as NSQIP captures readmissions even at different institutions, therefore providing a more complete representation of all readmissions. While the 30-day time period is limited, we believe that it still represents a critical time period, especially in light of the short time between an endovascular procedure and typical discharge.
When comparing our results to studies conducted among patients undergoing infrainguinal bypass surgery, we found similar predictors of readmission.7–12 Only one other study, by Vogel et al., identified predictors of readmission following tibioperoneal angioplasty using the US Medicare database and showed that gangrene, chronic heart failure, chronic obstructive pulmonary disease, and renal failure were independent risk factors of 30-day unplanned readmission in CLI patients.16 The association between renal failure and higher risk of readmission has been demonstrated previously,2,9,12,15,21 and the present study further supports that end-stage renal disease correlates with worse outcomes, in particular a 1.4- and 3.6-fold increased risk of readmission in patients with CLI and claudication, respectively. While the study by Vogel et al. included over 13,000 patients, Medicare uses administrative discharge data for billing purposes, which limits the ability to appropriately capture comorbidities, functional status, and operative details. In contrast, NSQIP is not an administrative database but rather a clinical registry that uses clinical reviewers to evaluate operative and progress notes, and also gathers complete 30-day follow-up data through outpatient chart review and telephone follow-up.
There are important clinical implications to this study. Many preoperative risk factors are not directly modifiable; however, this study merely reinforces the importance of addressing chronic issues and optimizing co-existing conditions. Furthermore, attention should be focused on procedure-related and in-hospital complications as these are more modifiable and may provide opportunities to further lower readmission rates. Previous studies reported similar postoperative complications, such as bleeding and unplanned return to the operating room as risk factors,12,15 which may be attributed to anatomy- or procedure-specific difficulties. However, given their strong association with readmission, care should be taken to minimize blood loss and in the occurrence of complications, close monitoring and evaluation prior to discharge may be appropriate, such as duplex evaluation for pseudoaneurysm in the event of a groin hematoma. Consistent with findings of others,8,15,23–25 our data showed an association between readmission and discharge destination. This is likely related to more advanced comorbidities and worsening functional status, which may not be modifiable. However, advancements in communication between physicians at the hospital and healthcare professionals at skilled nursing facilities both at time of discharge and after may help to improve transition of care and patient outcomes.26 Caution is warranted in the use of invasive interventions in patients with claudication, especially tibial revascularization and procedures in those with a poor functional health status, given that these were associated with readmission. In addition, risk reduction guidelines or programs, such as smoking cessation, are associated with reduced postoperative complications and limb events,27,28 and likely improve outcomes of patients with claudication. Some have suggested withholding surgical treatment until the patient has stopped smoking, which is adopted by the Society of Vascular Surgery (SVS) Lower Extremity Guidelines Committee that recommends multidisciplinary smoking cessation efforts in those with claudication, repeatedly before interventions.29
In patients with CLI, the majority of hospital readmissions identified in this study were related to infection and wound complication, with 42% of all readmissions. Other studies have shown similar readmission rates due to infectious complications after infrainguinal revascularization, ranging from 38 to 55%.11,12,15,25 As wound complications are likely related to a number of patient factors, including diabetes, we believe this may account for some of the increased risk of wound complications. Additionally, open concurrent procedures may attribute to the increased risk and are likely to represent challenging anatomy or access site complications due to artery calcification, small vessel diameter, or previous interventions. Involvement of case managers for effective patient education and discharge instructions about potential complications may help further reduce postoperative readmissions.
Time to readmission is another consideration in lowering readmission rates. Merkow et al. reported that readmissions after surgical procedures appeared evenly dispersed over time with no particular peak following discharge.25 In our analysis, patients with CLI and claudication were readmitted at a median of 12 and 13 days, respectively. As addressed previously, early medical follow-up may be strategically timed.2 Capturing adverse events during early surveillance may allow for treatment in the outpatient setting, for example by nurse-conducted telephone calls 1-week post discharge or improved utilization of skilled nursing facilities. Moreover, identifying high-risk patients can help to prioritize patients who should be seen in clinic sooner after discharge.
While we found higher readmissions rates in those patients with a longer hospital stay, no association was demonstrated in the adjusted analysis. Some may argue that keeping patients admitted for a few additional days may avert potential readmissions, although whether this reduces post discharge complications remains to be seen. Given that NSQIP follow-up ends at 30 days post intervention, a longer length of stay shortens post discharge follow-up and necessarily reduces the patient’s time at risk of readmission. Therefore, this study was unable to provide an accurate estimate in regard to the incidence of readmission when considering hospital stay duration, albeit short after endovascular intervention.
This study has several limitations that should be addressed. First, as NSQIP collects data through a clinical registry, it is subjected to data misclassification and limited by variable definitions. Second, confounding by indication may occur, since patients undergoing angioplasty were potentially unsuitable for open bypass surgery, despite adjustment for all reported baseline characteristics in the multivariable analysis. In addition, this study was unable to assess the lesion severity, extent of PAD, and the location of the puncture site or incision (e.g. groin, arm, lower leg), which will likely impact outcomes. Nonetheless, we believe that the Targeted Vascular module of NSQIP is a nationally representative and robust clinical registry that allows for reliable risk assessment in the 30-day postoperative period. As this study can only assess 30-day outcomes, further study is needed to identify the full implications of unplanned readmissions on a patient and national level. The SVS Vascular Quality Initiative registry provides more detailed variables, including closure device and ultrasound use, that may further explain associations found in this study.
Conclusions
This study demonstrates that unplanned readmission following endovascular intervention is relatively common and associated with increased morbidity and mortality. In both patients with CLI and claudication, risk factors for unplanned readmission include patient characteristics and procedure-related factors, as well as occurrence of in-hospital complications such as bleeding and unplanned return to the operating room. Many readmissions may not be avoidable, particularly in the CLI population, due to the extent of their comorbidities and socioeconomic status. However, this should not dissuade us from making efforts to optimize co-existing conditions, involve case managers to improve post discharge care and consider nurse-conducted phone calls to assess for potential complications that may be managed in an outpatient setting if identified early.
Supplementary Material
Table VB.
Independent predictors of 30-day unplanned readmission following endovascular intervention in patients with claudication
| Claudication | |||
|---|---|---|---|
|
| |||
| Variable | OR | 95% CI | P-value |
| Dependent functional status | 3.5 | 1.4–8.7 | <.01 |
| Smoking | 1.6 | 1.02–2.5 | .04 |
| Diabetes | 1.5 | 1.01–2.3 | .048 |
| Preoperative dialysis | 3.6 | 1.6–8.3 | <.01 |
| Procedure time exceeding 120 min (75th percentile) | 1.8 | 1.1–2.7 | .01 |
| In-hospital bleeding | 2.9 | 1.2–7.4 | .02 |
| In-hospital unplanned return to the operation room | 3.4 | 1.2–9.4 | .02 |
Adjusted for: age, gender
Acknowledgments
Supported by the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734.
Footnotes
This study was presented as a poster at the 2016 Vascular Annual Meeting of the Society for Vascular Surgery, National Harbor, MD, June 8-11, 2016.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wiseman JT, Guzman AM, Fernandes-Taylor S, Engelbert TL, Saunders RS, Kent KC. General and vascular surgery readmissions: a systematic review. J Am Coll Surg. 2014;219(3):552–69. e2. doi: 10.1016/j.jamcollsurg.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sellers MM, Merkow RP, Halverson A, Hinami K, Kelz RR, Bentrem DJ, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(3):420–427. doi: 10.1016/j.jamcollsurg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating whether changes in utilization of hospital outpatient services contributed to lower Medicare readmission rate. Medicare Medicaid Res Rev. 2014;4(1) doi: 10.5600/mmrr2014-004-01-b03. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 7.McPhee JT, Nguyen LL, Ho KJ, Ozaki CK, Conte MS, Belkin M. Risk prediction of 30-day readmission after infrainguinal bypass for critical limb ischemia. J Vasc Surg. 2013;57(6):1481–1488. doi: 10.1016/j.jvs.2012.11.074. [DOI] [PubMed] [Google Scholar]
- 8.Damrauer SM, Gaffey AC, DeBord Smith A, Fairman RM, Nguyen LL. Comparison of risk factors for length of stay and readmission following lower extremity bypass surgery. J Vasc Surg. 2015;62(5):1192–200. e1. doi: 10.1016/j.jvs.2015.06.213. [DOI] [PubMed] [Google Scholar]
- 9.McPhee JT, Barshes NR, Ho KJ, Madenci A, Ozaki CK, Nguyen LL, et al. Predictive factors of 30-day unplanned readmission after lower extremity bypass. J Vasc Surg. 2013;57(4):955–962. doi: 10.1016/j.jvs.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 10.Aziz F, Lehman EB, Reed AB. Unplanned return to operating room after lower extremity arterial bypass is an independent predictor for hospital readmission. J Vasc Surg. 2016;63(3):678–687. e2. doi: 10.1016/j.jvs.2015.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Najafian A, Selvarajah S, Schneider EB, Malas MB, Ehlert BA, Orion KC, et al. Thirty-day readmission after lower extremity bypass in diabetic patients. J Surg Res. 2016;200(1):356–364. doi: 10.1016/j.jss.2015.06.061. [DOI] [PubMed] [Google Scholar]
- 12.Zhang JQ, Curran T, McCallum JC, Wang L, Wyers MC, Hamdan AD, et al. Risk factors for readmission after lower extremity bypass in the American College of Surgeons National Surgery Quality Improvement Program. J Vasc Surg. 2014;59(5):1331–1339. doi: 10.1016/j.jvs.2013.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal S, Sud K, Shishehbor MH. Nationwide Trends of Hospital Admission and Outcomes Among Critical Limb Ischemia Patients During 2003–2011. J Am Coll Cardiol. 2016 doi: 10.1016/j.jacc.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 14.Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009;50(1):54–60. doi: 10.1016/j.jvs.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 15.Davenport DL, Zwischenberger BA, Xenos ES. Analysis of 30-day readmission after aortoiliac and infrainguinal revascularization using the American College of Surgeons National Surgical Quality Improvement Program data set. J Vasc Surg. 2014;60(5):1266–1274. doi: 10.1016/j.jvs.2014.05.051. [DOI] [PubMed] [Google Scholar]
- 16.Vogel TR, Dombrovskiy VY, Carson JL, Graham AM. In-hospital and 30-day outcomes after tibioperoneal interventions in the US Medicare population with critical limb ischemia. J Vasc Surg. 2011;54(1):109–115. doi: 10.1016/j.jvs.2010.12.055. [DOI] [PubMed] [Google Scholar]
- 17.Shiloach M, Frencher SK, Jr, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6–16. doi: 10.1016/j.jamcollsurg.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 18.Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228(4):491–507. doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251–267. doi: 10.1016/j.yasu.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3 doi: 10.1186/1751-0473-3-17. 17-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vogel TR, Kruse RL. Risk factors for readmission after lower extremity procedures for peripheral artery disease. J Vasc Surg. 2013;58(1):90–7. e1–4. doi: 10.1016/j.jvs.2012.12.031. [DOI] [PubMed] [Google Scholar]
- 22.Jackson BM, Nathan DP, Doctor L, Wang GJ, Woo EY, Fairman RM. Low rehospitalization rate for vascular surgery patients. J Vasc Surg. 2011;54(3):767–772. doi: 10.1016/j.jvs.2011.03.255. [DOI] [PubMed] [Google Scholar]
- 23.Engelbert TL, Fernandes-Taylor S, Gupta PK, Kent KC, Matsumura J. Clinical characteristics associated with readmission among patients undergoing vascular surgery. J Vasc Surg. 2014;59(5):1349–1355. doi: 10.1016/j.jvs.2013.10.103. [DOI] [PubMed] [Google Scholar]
- 24.Curran T, Zhang JQ, Lo RC, Fokkema M, McCallum JC, Buck DB, et al. Risk factors and indications for readmission after lower extremity amputation in the American College of Surgeons National Surgical Quality Improvement Program. J Vasc Surg. 2014;60(5):1315–1324. doi: 10.1016/j.jvs.2014.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313(5):483–495. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 26.Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14 doi: 10.1186/1472-6963-14-423. 423-6963-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hussain MA, Al-Omran M, Mamdani M, Eisenberg N, Premji A, Saldanha L, et al. Efficacy of a Guideline-Recommended Risk-Reduction Program to Improve Cardiovascular and Limb Outcomes in Patients With Peripheral Arterial Disease. JAMA Surg. 2016 doi: 10.1001/jamasurg.2016.0415. [DOI] [PubMed] [Google Scholar]
- 28.Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med. 2011;124(2):144–154. e8. doi: 10.1016/j.amjmed.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 29.Society for Vascular Surgery Lower Extremity Guidelines Writing Group. Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015;61(3 Suppl):2S–41S. doi: 10.1016/j.jvs.2014.12.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.