Abstract
Hookah tobacco smoking (HTS) has been increasing, particularly among young adults and has similar health effects compared to cigarette smoking. The link between HTS and poly-tobacco use is well documented, but fewer show an association between HTS and alcohol use. It is essential to identify factors that increase the risk for or addictiveness and consequences of HTS, given its growing prevalence. This study examined whether the association between HTS and poly-tobacco use differed as a function of age and alcohol consumption within in a sample of 1,223 adult cigarette smokers. Approximately 20% of participants reported HTS. Compared to non-users, hookah users were more likely to be male, highly educated, and to report drug and alcohol use, binge drinking, and poly-tobacco use but were less likely to be heavy smokers (>10 cigarettes per day). Regression analyses predicting number of tobacco products used (excluding cigarettes and HTS) indicated a three-way interaction of HTS, frequency of alcohol use, and age such that the association between HTS and number of tobacco products used was strongest for younger respondents who consumed alcohol more frequently. As observed in previous studies, alcohol is an important risk factor in the relationship between HTS and poly-tobacco use, particularly among younger cigarette smokers. The links between alcohol, HTS, and poly-tobacco use should be considered when developing HTS education and prevention materials directed toward younger cigarette smokers. Findings provide information relevant to FDA’s interest in the addiction potential of HTS and its link to poly-tobacco use.
Keywords: hookah, shisha, alcohol, poly-tobacco use, young adults, binge drinking
Hookah tobacco smoking has been on the rise among men and women over the age of 18 over the last five years,1–3 and has become particularly popular among young adults.4 The increasing prevalence of HTS is concerning. HTS places users at risk for many of the same cancer-causing diseases as cigarette smokers, such as lung cancer and pulmonary and chronic obstructive pulmonary disorder5–11 and may be a catalyst to nicotine dependence, progression to regular tobacco and other health-risk behaviors correlated with increased cancer risk, including alcohol and marijuana use.12–22 HTS is associated with unique acute health effects such as carbon monoxide poisoning,23–26 and the spread of communicable diseases like herpes and tuberculosis.27 Failure to respond to the increasing HTS trend could contribute to morbidity and mortality in the U.S.
HTS has been consistently linked to the use of other tobacco products, including poly-tobacco use (≥ 2 tobacco products). For instance, cigarette smoking is commonly reported among hookah users.21,28–30 Among individuals 18 years and older, non-daily and daily smokers show a higher prevalence of lifetime HTS compared to the use of any other type of alternative tobacco product.31 A number of studies also document an association between alcohol use and HTS16,22,32,33 and between alcohol use and poly-tobacco use.34–36 The association between HTS and alcohol is concerning for several reasons: alcohol use has been shown to increase the likelihood of HTS initiation above and beyond other tobacco-related risk factors 18,37–40 and has been implicated in the use of a variety of other new and alternative tobacco products.22,34 Alcohol use is also robustly correlated with more severe nicotine dependence,41,42 lower desire to quit smoking,43 and poor tobacco cessation outcomes.44–46 Existing studies have found that many hookah users drink alcohol while engaging in HTS39,47 and concurrent alcohol use and HTS may enhance the subjective effects of HTS.39 However, not all studies have reported an association between HTS and alcohol use,48,49 suggesting further research is needed to tease apart “for whom” and “under what circumstances” alcohol is linked to HTS behavior. Understanding links between HTS and alcohol use is also important, given that the short- and long-term effects of new and alternative tobacco products, like HTS. are not well understood.
The majority of studies to date on HTS have focused on youth and young adult users, particularly college students,21,33,50,51 but not the full spectrum of tobacco users who may also be engaging in HTS. As a result, little is known about the HTS risk profiles in older age groups. While hookah use, and to some extent poly-tobacco use,34 are concentrated among youth and young adults, alcohol is robustly associated with tobacco use across the age spectrum.41,45,52,53 Taken together, these studies argue for inclusion of alcohol use as an important risk factor linking HTS to poly-tobacco use, but suggest there may also be different important age differences. This study examined the moderating effects of both age and alcohol use on the association between HTS and poly-tobacco use in a large sample of adult cigarette smokers.
Method
Participants and Procedure
This is a secondary analysis of data that were combined from the screening measures of two NIH-funded studies (data collected from January 2014 to December 2015). The first study was a naturalistic assessment of the longitudinal smoking change outcomes of risky drinking adult smokers. The second was an administrative supplement to this project, designed to examine motivations for alcohol use and cigarette smoking in adult smokers with and without a history of risky drinking. Both studies included the same battery of questionnaires at baseline (described below). Eligibility for both studies was nearly identical and included: 1) 18–65 years old; 2) smoke > 10 cigarettes per day; and 3) desire to quit smoking in the next 6-months. Exclusion criteria were 1) suicidal, homicidal, or severe psychiatric disturbance; 2) substance dependence (excluding nicotine and caffeine); 3) current use of psychotropic medication; and 4) potential for severe alcohol withdrawal. Additionally, individuals eligible for the parent grant drank at risky levels [< 2 drinks a day for men; >1 for women and > 14 drinks per week for men; 7 for women, according to the guidelines of the National Institute on Alcoholism and Alcohol Abuse] and were excluded if they were pregnant or planning to become pregnant in the next 6 months. For the administrative supplement, a sampling method was employed to recruit 50% risky drinkers and 50% non-risky drinkers (consume at least 1 drink/week in the last 30 days but less than risky drinking levels). Participants included in the current analysis completed the screening for these studies but did not have to meet eligibility criteria, therefore not all participants who took the screening measure were risky drinkers. Participants in the parent grant were eligible to receive up to $178 for their participation over 6 months, and participants in the administrative supplement were eligible to receive up to $50 for completing two experimental sessions.
Participants were recruited from a large Northeastern US city via web or print advertisements, or through word-of-mouth. Advertisements asked for “smokers who are regular drinkers”. Participants were directed to complete an initial online screening survey or call a telephone number to determine eligibility; final eligibility was determined over the phone by a trained research assistant. A total of 1,405 individuals completed the screening questionnaires; 171 had missing other tobacco use data and 11 indicated smoking 0 cigarettes, so they were excluded from analyses. A final sample size of 1,223 adult (18+) cigarette smokers were included. a
Measures
Participants provided demographic information on age, race (White, African American, other), gender, education (<high school, high school graduate or GED, some college education or higher), and employment status (employed, unemployed, other).
Data were collected on number of drinks consumed per drinking episode (quantity) and number of days in a typical week alcohol was consumed (frequency). A binge drinking variable (yes/no) was computed from quantity/frequency measurements based on established measures (4+ drinks for women/5+ drinks for men).54,55 Participants were also queried “Have you used any drugs in the past 90 days?” (yes/no).
Use of other tobacco products, exclusive of cigarettes, was assessed by asking participants “Do you use any other tobacco products other than cigarettes?” with response options for e-cigarettes, cigars, little cigar/cigarillos, hookah, chew, and “other.” A variable capturing the total number of tobacco products was created by summing the number of ‘yes’ responses for each product (excluding hookah). For the parent grant, participants were asked if they smoked > 10 cigarettes per day (yes/no). However, for the administrative supplement study participants were asked how many cigarettes they smoke per day. Thus, to be consistent and examine cigarette smoking across both studies, participants were categorized into light smokers (≤10 cigarettes per day) versus heavy smokers (>10 cigarettes per day), consistent with the literature.56
Analyses
The prevalence and distributions of study variables were examined across hookah users and non-users. Following recommendations of Aiken and West,57 the moderating effects of age and alcohol use (separately for quantity, frequency, and binge drinking) on the association between HTS and number of non-cigarette tobacco products used were then examined. Continuous variables (alcohol quantity, alcohol frequency, and age) were z-transformed to reduce multi-collinearity and to account for scale invariance.57 Using HTS (0 = no) as the independent variable, and alcohol use (quantity, frequency, or binge drinking) and age as the moderators, regression equations were computed with relevant covariates entered in the first step, main effects in the second step, two-way interactions in the third step, and the three-way interaction (HTS x alcohol use x age) in the final step. For equations with significant interactions, regression coefficients for simple effects (one standard deviation above and below the mean of each moderator; e.g., low vs. high frequency drinking) were examined to determine whether they were significantly different than zero.57 Unstandardized betas are reported. Analyses were conducted using SPSS 22 58.
Results
Differences between smokers reporting HTS and no HTS
Bivariate differences between adult smokers who were hookah users and non-users are shown in Table 1. Nearly 20% reported HTS. Those who reported HTS were predominantly male [χ2(1) = 4.50], highly educated [χ2(3) = 25.52], younger [F(1, 1220) = 185.03], used a greater number of other tobacco products (excluding cigarettes and hookah) [F(1, 1221) = 644.38], and were more likely to binge drink [χ2(1) = 5.10] and use drugs [χ2(1) = 39.05] (all p’s < .05). Compared to non-users, smokers reporting HTS were less likely to smoke heavily [χ2(1) = 22.00] and to be African American [χ2(2) = 7.72] (all p’s < .05). HTS was unrelated to alcohol quantity and frequency at the bivariate level.
Table 1.
Descriptive statistics and differences between adult cigarette smokers with and without HTS use on demographic, tobacco, and alcohol and drug use.
| HTS Use n = 231; 18.9% |
Non-HTS Use n = 992; 81.1% |
||||
|---|---|---|---|---|---|
|
| |||||
| n | % | n | % | p | |
| Gender | 0.03 | ||||
| Male | 141 | 61.0 | 529 | 53.3 | |
| Female | 90 | 39.0 | 463 | 46.7 | |
| Race | 0.02 | ||||
| African American | 132 | 57.4 | 624 | 63.1 | |
| White | 58 | 25.1 | 258 | 26.1 | |
| Other | 40 | 17.4 | 107 | 10.8 | |
| Education | 0.001 | ||||
| < HS diploma | 8 | 3.5 | 80 | 8.1 | |
| HS graduate/GED | 43 | 18.6 | 310 | 31.3 | |
| Some college | 118 | 51.1 | 373 | 37.6 | |
| College graduate or higher | 62 | 26.8 | 228 | 23.0 | |
| Employment status | 0.08 | ||||
| Employed | 122 | 52.8 | 450 | 45.4 | |
| Unemployed | 65 | 28.1 | 349 | 35.2 | |
| Other | 44 | 19.0 | 192 | 19.4 | |
| Heavy smoker (≥10 cigs/day) | 152 | 65.8 | 787 | 80.1 | 0.001 |
| Drug use (yes) | 95 | 42.0 | 216 | 21.8 | 0.001 |
| Binge drinking (yes) | 135 | 58.4 | 498 | 50.2 | 0.02 |
| Other non-hookah tobacco product use | 0.001 | ||||
| 0 products | 30 | 13.0 | 720 | 72.6 | |
| 1 product | 67 | 29.0 | 194 | 19.6 | |
| 2 products | 55 | 23.8 | 58 | 5.8 | |
| 3+ products | 79 | 34.2 | 20 | 2.0 | |
|
| |||||
| Mean | SD | Mean | SD | ||
|
| |||||
| Age | 27.16 | 7.26 | 39.38 | 13.19 | 0.001 |
| Alcohol frequency | 4.11 | 1.66 | 4.29 | 2.09 | 0.22 |
| Alcohol quantity | 5.31 | 3.88 | 5.54 | 5.12 | 0.52 |
Note. Data represent column percents. Totals may not equal 1,223 due to missing data. Other non-hookah tobacco use included e-cigarettes, cigars, little cigar/cigarillos, chew, and “other.”
Moderating effects of alcohol use and age on the association between HTS and number of other tobacco products
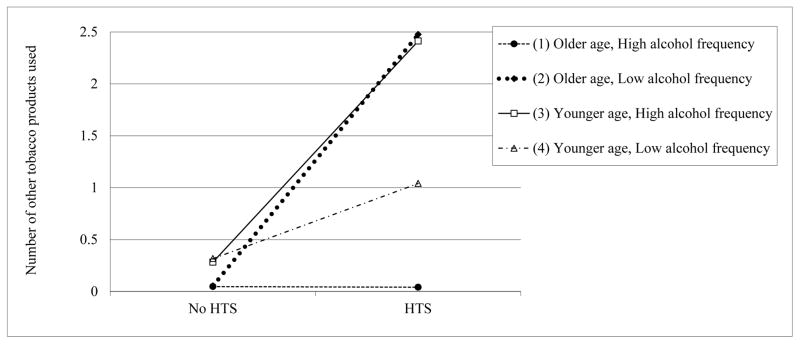
There was a significant HTS x alcohol use frequency x age interaction [F(12, 1181) = 61.17, p < 0.001, R2 = 0.38], after controlling for gender, race, heavy smoking, education, and drug use. Explication of the simple slopes revealed a positive association between HTS and other tobacco use, although the strength of the association between HTS and number of tobacco products used was strongest for those who were younger and who drank alcohol more frequently (b = 1.78, p < 0.001; see Figure 1). The weakest association between HTS and poly-tobacco use was found among older respondents who drank more frequently (b = 0.94, p < 0.001). That is, HTS was also positively associated with other tobacco use among older respondents who consumed alcohol more often, but the slope was not as steep.
Figure 1.
Moderating effects of alcohol use frequency and age on the association between HTS and number of other tobacco products used in adult cigarette smokers.
Note. Other non-hookah tobacco product use included e-cigarettes, cigars, little cigar/cigarillos, chew, and “other.”
There were no significant three-way interactions when alcohol quantity or binge drinking were examined as moderators in the model. There was a significant alcohol quantity x HTS interaction [F(8,1181) = 86.52, p < 0.001, R2 = 0.37], showing that the association between HTS and number of tobacco products used was stronger for those who drank greater quantities of alcohol (b = 1.61, p < 0.001), relative to those who drank less (b = 1.32, p < 0.001). No other two-way interactions or main effects emerged.
Discussion
Findings showed that HTS’s association to dual and poly-tobacco use were strongest among younger respondents who drank more often and more frequently. This is the first study examining alcohol use frequency and age as moderators of the relationship between HTS and poly-tobacco use among adult hookah users, rather than looking at main effect relationships of alcohol use or HTS to poly-tobacco use separately, as has been done in all prior research.49,59,60 Findings provide information relevant to the Food and Drug Administration’s (FDA) effort to understand the abuse liability of HTS and associations with other tobacco product use. Such information has the potential to inform FDA regulations of HTS products, including enhanced warning labels of the potential harms associated with HTS or age restrictions on HTS purchases (among others).
Compared to non-users, hookah users were more likely to be male, highly educated, to report drug and alcohol use, including binge drinking, and to consume a greater number of non-cigarette tobacco products. At the bivariate level, drinking frequency and quantity were unrelated to HTS. This is not consistent with other research showing an association between alcohol use and HTS 22,33,61, although the majority of these studies utilized college student samples or focused exclusively on young adults. Respondents in our study spanned the age continuum (20% 18–24; 32% 25–34; 18% 35–45; 31% 46+). Hookah users in our study were also less likely to endorse heavy smoking. This observation may be attributed to the fact that HTS is perceived to be less harmful than cigarette smoking. 33,62 Therefore, individuals may be more inclined to use hookah instead of cigarettes because they believe it is a less risky alternative. Additionally, there may have been a selection bias for those who completed the screening survey for this study because advertisements asked for regular drinkers.
Regression analyses showed that age and alcohol frequency significantly moderated the relationship between HTS and number of other tobacco products used, beyond the influence of several covariates. That is, dual users of cigarettes and hookah reported using a greater number of other tobacco products compared to cigarette smokers who did not use HTS, and this relationship was strongest among younger adults who reported drinking alcohol more often. Because alcohol has been shown to enhance the subjective effects of HTS (Soule et al., 2015), it is possible that hookah users who drink alcohol on a more frequent basis try other tobacco products to obtain similar subjective experiences. It may also be that, because alcohol reduces one’s inhibitions and restraint, those who are willing to try hookah may also use other products when they are intoxicated. The association between “real-time” drinking and number or types of tobacco products used should be examined in future research. These results suggest that the both age and how often one drinks alcohol are contributing factors to HTS and other tobacco use, rather than each factor alone.
This study had several limitations. The sample included self-reported regular cigarette smokers who responded to an advertisement asking for “regular drinkers”, rather than a general population of hookah users. While these sample characteristics may limit generalizability, cigarette and alcohol use are common among hookah users and thus findings nonetheless have public health implications. Furthermore, respondents in the sample were not drinking heavily or even daily. Second, due to data collection methods, cigarette smoking frequency was assessed dichotomously, not as a continuous factor. Although hookah users were lighter smokers, consistent with the research, it is unknown if this finding would be different if smoking was measured continuously. Further, because data were assessed via a brief screener, specific types of drug classes used were not assessed. Lastly, alternative tobacco use was also analyzed dichotomously, so the current analyses do not account for differences in frequency of alternative tobacco use.
This study fills an important gap in the literature by examining the influence of both age and alcohol use on the relationship between HTS and poly-tobacco use in a diverse adult sample of smokers across a broad age continuum. Most prior studies of HTS and alcohol use have included college students only or small convenience samples21,33,48,50,60,63; few have explored these associations in larger urban samples with a wide age range. As HTS increases in popularity in the US and outpaces cigarette smoking among younger users, it is essential to continue to investigate potential factors that increase the risks associated with HTS. HTS exposes individuals to many of the same toxicants found in cigarette smoke in higher concentrations64,65 and places users at risk for many of the same diseases as cigarette smokers66–69 including nicotine dependence, lung cancer, and respiratory illness.67–69 The results of this study identify a need to use rigorous prospective designs to investigate the short- and long-term harms of the combination of alcohol, HTS, and poly-tobacco use public health interventions focused on enhanced awareness of HTS health effects that target young adults and youth who may be at risk for HTS and poly-tobacco use. Without knowledge of the factors associated with HTS, which could be targeted in health interventions, HTS will continue to pose health risks and increase in prevalence in the foreseeable future.
Highlights.
To examine effects of alcohol use and age on the association between hookah and poly-tobacco use in adult cigarette smokers
Poly-tobacco use is common among adult smokers who use hookah
The link between hookah and poly-tobacco use was strongest in younger respondents who drank more often
Acknowledgments
FUNDING: This work was supported by grants R03CA 175870-01A1 and R03CA 175870-01A1S.
Role of Funding Sources
This work was supported by grants R03CA 175870-01A1 and R03CA 175870-01A1S.
Footnotes
It is possible that some participants may have completed the screening questionnaire for both studies. We were unable to detect duplicates.
Contributors
Amy Cohn and Sarah Ehlke designed the study and wrote the protocol, and conducted analyses. Amy Cohn, Sarah Ehlke, Eric Soule, and Caroline Cobb conducted literature searches, provided summaries of previous research studies, and assisted with conceptualization and writing of the current study findings. Author Cohn wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript
Conflict of Interest
Authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Grinberg A, Goodwin RD. Prevalence and correlates of hookah use: a nationally representative sample of US adults ages 18–40 years old. The American journal of drug and alcohol abuse. 2016:1–10. doi: 10.3109/00952990.2016.1167214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith JR, Edland SD, Novotny TE, et al. Increasing hookah use in California. American journal of public health. 2011;101(10):1876–1879. doi: 10.2105/AJPH.2011.300196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salloum RG, Thrasher JF, Kates FR, Maziak W. Water pipe tobacco smoking in the United States: findings from the National Adult Tobacco Survey. Preventive medicine. 2015;71:88–93. doi: 10.1016/j.ypmed.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson A, Williams V, Rath J, Villanti AC, Vallone D. The next generation of users: prevalence and longitudinal patterns of tobacco use among US young adults. American journal of public health. 2014;104(8):1429–1436. doi: 10.2105/AJPH.2013.301802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. International Journal of Epidemiology. 2010;39(3):834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 6.Khabour OF, Alzoubi KH, Bani-Ahmad M, Dodin A, Eissenberg T, Shihadeh A. Acute exposure to waterpipe tobacco smoke induces changes in the oxidative and inflammatory markers in mouse lung. Inhalation toxicology. 2012;24(10):667–675. doi: 10.3109/08958378.2012.710918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro cytotoxicity and mutagenicity of mainstream waterpipe smoke and its functional consequences on alveolar type II derived cells. Toxicology letters. 2012;211(3):220–231. doi: 10.1016/j.toxlet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro effects of waterpipe smoke condensate on endothelial cell function: a potential risk factor for vascular disease. Toxicology letters. 2013;219(2):133–142. doi: 10.1016/j.toxlet.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aoun J, Saleh N, Waked M, Salamé J, Salameh P. Lung cancer correlates in Lebanese adults: A pilot case–control study. Journal of epidemiology and global health. 2013;3(4):235–244. doi: 10.1016/j.jegh.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta D, Boffetta P, Gaborieau V, Jindal S. Risk factors of lung cancer in Chandigarh, India. Indian Journal of Medical Research. 2001;113:142. [PubMed] [Google Scholar]
- 11.Koul PA, Hajni MR, Sheikh MA, et al. Hookah smoking and lung cancer in the Kashmir valley of the Indian subcontinent. Asian Pac J Cancer Prev. 2011;12(2):519–524. [PubMed] [Google Scholar]
- 12.Griffiths MA, Ford EW. Hookah smoking: behaviors and beliefs among young consumers in the United States. Soc Work Public Health. 2014 Jan 1;29(1):17–26. doi: 10.1080/19371918.2011.619443. [DOI] [PubMed] [Google Scholar]
- 13.Auf RA, Radwan GN, Loffredo CA, El Setouhy M, Israel E, Mohamed MK. Assessment of tobacco dependence in waterpipe smokers in Egypt. Int J Tuberc Lung Dis January. 2012;16(1):132–137. doi: 10.5588/ijtld.11.0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neergaard J, Singh P, Job J, Montgomery S. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine Tob Res October. 2007;9(10):987–994. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res February. 2011;13(2):78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sterling KL, Mermelstein R. Examining hookah smoking among a cohort of adolescent ever smokers. Nicotine Tob Res December. 2011;13(12):1202–1209. doi: 10.1093/ntr/ntr146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berg CJ, Schauer GL, Asfour OA, Thomas AN, Ahluwalia JS. Psychosocial Factors and Health-Risk Behaviors Associated with Hookah use among College Students. J Addict Res Ther. 2011 Oct 10;(Suppl 2) doi: 10.4172/2155-6105.S2-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fielder RL, Carey KB, Carey MP. Predictors of initiation of hookah tobacco smoking: a one-year prospective study of first-year college women. Psychol Addict Behav December. 2012;26(4):963–968. doi: 10.1037/a0028344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fielder RL, Carey KB, Carey MP. Hookah, cigarette, and marijuana use: a prospective study of smoking behaviors among first-year college women. Addict Behav November. 2013;38(11):2729–2735. doi: 10.1016/j.addbeh.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011 May 5;115(1–2):131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarrett T, Blosnich J, Tworek C, Horn K. Hookah use among U.S. college students: results from the National College Health Assessment II. Nicotine Tob Res. 2012 Oct;14(10):1145–1153. doi: 10.1093/ntr/nts003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohn A, Villanti A, Richardson A, et al. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addictive behaviors. 2015;48:79–88. doi: 10.1016/j.addbeh.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Ashurst JV, Urquhart M, Cook MD. Carbon monoxide poisoning secondary to hookah smoking. The Journal of the American Osteopathic Association. 2012;112(10):686–688. [PubMed] [Google Scholar]
- 24.Clarke SF, Stephens C, Farhan M, et al. Multiple patients with carbon monoxide toxicity from water-pipe smoking. Prehospital and disaster medicine. 2012;27(06):612–614. doi: 10.1017/S1049023X12001227. [DOI] [PubMed] [Google Scholar]
- 25.La Fauci G, Weiser G, Steiner IP, Shavit I. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. Cjem. 2012;14(01):57–59. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 26.Ozkan S, Ozturk T, Ozmen Y, Durukan P. Syncope associated with carbon monoxide poisoning due to narghile smoking. Case reports in emergency medicine. 2013 doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Association AL. Hookah smoking: a growing threat to public health issue brief. Smokefree Communities Project. 2011 [Google Scholar]
- 28.Barnett TE, Smith T, He Y, et al. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health. 2013;13:302. doi: 10.1186/1471-2458-13-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee YO, Bahreinifar S, Ling PM. Understanding tobacco-related attitudes among college and noncollege young adult hookah and cigarette users. J Am Coll Health. 2014;62(1):10–18. doi: 10.1080/07448481.2013.842171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Primack BA, Shensa A, Kim KH, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res January. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMillen R, Maduka J, Winickoff J. Use of emerging tobacco products in the United States. Journal of environmental and public health. 2012 doi: 10.1155/2012/989474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Czoli CD. Bidi and hookah use among Canadian youth: findings from the 2010 Canadian Youth Smoking Survey. Preventing chronic disease. 2013:10. doi: 10.5888/pcd10.120290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heinz AJ, Giedgowd GE, Crane NA, et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addictive behaviors. 2013;38(11):2751–2760. doi: 10.1016/j.addbeh.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 34.Fix BV, O’Connor RJ, Vogl L, et al. Patterns and correlates of polytobacco use in the United States over a decade: NSDUH 2002–2011. Addictive behaviors. 2014;39(4):768–781. doi: 10.1016/j.addbeh.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Grucza RA, Bierut LJ. Youth tobacco use type and associations with substance use disorders. Addiction. 2014;109(8):1371–1380. doi: 10.1111/add.12567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bombard JM, Pederson LL, Koval JJ, O’Hegarty M. How are lifetime polytobacco users different than current cigarette-only users? Results from a Canadian young adult population. Addictive behaviors. 2009;34(12):1069–1072. doi: 10.1016/j.addbeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Fielder RL, Carey KB, Carey MP. Prevalence, frequency, and initiation of hookah tobacco smoking among first-year female college students: a one-year longitudinal study. Addictive behaviors. 2012;37(2):221–224. doi: 10.1016/j.addbeh.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shepardson RL, Hustad JT. Hookah tobacco smoking during the transition to college: prevalence of other substance use and predictors of initiation. Nicotine & Tobacco Research. 2015 doi: 10.1093/ntr/ntv170. ntv170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soule EK, Barnett TE, Curbow BA, Moorhouse MD, Weiler RM. Hookah and Alcohol Use among Young Adult Hookah Smokers: A Mixed Methods Study. American journal of health behavior. 2015;39(5):665–673. doi: 10.5993/AJHB.39.5.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in US young adults. American journal of preventive medicine. 2015;48(6):742–746. doi: 10.1016/j.amepre.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 41.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the united states: Results from the national epidemiologic survey on alcohol and relatedconditions. Archives of general psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 42.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of general psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 43.Cargill BR, Emmons KM, Kahler CW, Brown RA. Relationship among alcohol use, depression, smoking behavior, and motivation to quit smoking with hospitalized smokers. Psychology of addictive behaviors. 2001;15(3):272. [PubMed] [Google Scholar]
- 44.Kahler CW, Borland R, Hyland A, McKee SA, Thompson ME, Cummings KM. Alcohol consumption and quitting smoking in the International Tobacco Control (ITC) Four Country Survey. Drug and alcohol dependence. 2009;100(3):214–220. doi: 10.1016/j.drugalcdep.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kahler CW, Spillane NS, Metrik J. Alcohol use and initial smoking lapses among heavy drinkers in smoking cessation treatment. Nicotine & Tobacco Research. 2010;12(7):781–785. doi: 10.1093/ntr/ntq083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hughes JR, Kalman D. Do smokers with alcohol problems have more difficulty quitting? Drug and Alcohol Dependence. 2006;82(2):91–102. doi: 10.1016/j.drugalcdep.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 47.Soule E, Barnett T, Curbow B. Keeping the night going: the role of hookah bars in evening drinking behaviours. Public health. 2012;126(12):1078–1081. doi: 10.1016/j.puhe.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 48.Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug and alcohol dependence. 2011;115(1):131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dugas EN, O’Loughlin EK, Low NC, Wellman RJ, O’Loughlin JL. Sustained waterpipe use in young adults. Nicotine & Tobacco Research. 2013 doi: 10.1093/ntr/ntt215. ntt215. [DOI] [PubMed] [Google Scholar]
- 50.Primack BA, Shensa A, Kim KH, et al. Waterpipe smoking among US university students. Nicotine & Tobacco Research. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Enofe N, Berg CJ, Nehl EJ. Alternative tobacco use among college students: who is at highest risk? American journal of health behavior. 2014;38(2):180. doi: 10.5993/AJHB.38.2.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Falk DE, Yi H, Hiller-Sturmhöfel S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders. Alcohol Res Health. 2006;29(3):162–171. [PMC free article] [PubMed] [Google Scholar]
- 53.Kahler CW, Strong DR, Papandonatos GD, et al. Cigarette smoking and the lifetime alcohol involvement continuum. Drug and alcohol dependence. 2008;93(1):111–120. doi: 10.1016/j.drugalcdep.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wechsler H, Austin SB. Binge drinking: the five/four measure. Journal of studies on alcohol. 1998;59(1):122–124. doi: 10.15288/jsa.1998.59.122. [DOI] [PubMed] [Google Scholar]
- 55.Wechsler H, Nelson TF. Binge drinking and the American college students: What’s five drinks? Psychology of Addictive Behaviors. 2001;15(4):287. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- 56.Choi WS, Okuyemi KS, Kaur H, Ahluwalia JS. Comparison of smoking relapse curves among African-American smokers. Addictive behaviors. 2004;29(8):1679–1683. doi: 10.1016/j.addbeh.2004.02.060. [DOI] [PubMed] [Google Scholar]
- 57.Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- 58.SPSS I. Algorithms. Chicago: IBM SPSS Inc; 2013. IBM SPSS statistics 22. [Google Scholar]
- 59.Braun RE, Glassman T, Wohlwend J, Whewell A, Reindl DM. Hookah use among college students from a Midwest University. Journal of community health. 2012;37(2):294–298. doi: 10.1007/s10900-011-9444-9. [DOI] [PubMed] [Google Scholar]
- 60.Lipkus IM, Reboussin BA, Wolfson M, Sutfin EL. Assessing and predicting susceptibility to waterpipe tobacco use among college students. Nicotine & Tobacco Research. 2015;17(9):1120–1125. doi: 10.1093/ntr/ntu336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sterling KL, Mermelstein R. Examining hookah smoking among a cohort of adolescent ever smokers. Nicotine & Tobacco Research. 2011;13(12):1202–1209. doi: 10.1093/ntr/ntr146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: predictors and characteristics among current hookah users. Tobacco induced diseases. 2009;5(1):1. doi: 10.1186/1617-9625-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sutfin EL, Song EY, Reboussin BA, Wolfson M. What are young adults smoking in their hookahs? A latent class analysis of substances smoked. Addictive behaviors. 2014;39(7):1191–1196. doi: 10.1016/j.addbeh.2014.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol January. 2003;41(1):143–152. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 65.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol May. 2005;43(5):655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 66.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol June. 2010;39(3):834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 67.Khabour OF, Alzoubi KH, Bani-Ahmad M, Dodin A, Eissenberg T, Shihadeh A. Acute exposure to waterpipe tobacco smoke induces changes in the oxidative and inflammatory markers in mouse lung. Inhal Toxicol August. 2012;24(10):667–675. doi: 10.3109/08958378.2012.710918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro cytotoxicity and mutagenicity of mainstream waterpipe smoke and its functional consequences on alveolar type II derived cells. Toxicol Lett. 2012 Jun 6;211(3):220–231. doi: 10.1016/j.toxlet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro effects of waterpipe smoke condensate on endothelial cell function: a potential risk factor for vascular disease. Toxicol Lett. 2013 May 5;219(2):133–142. doi: 10.1016/j.toxlet.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]