Summary:
Giant juvenile fibroadenomas are relatively rare, accounting for less than 1% fibroadenomas. Large breast tumors create significant asymmetry and provide unique reconstructive challenges after removal. In this case, we describe a 21-year-old female with delayed presentation of a giant fibroadenoma of the right breast. This represents an unusual presentation of benign breast disease requiring reduction of the skin envelope, extensive glandular resection, lower pole reconstruction, and free nipple grafting to achieve symmetry with the opposite breast. A novel modification of the Goldilocks mastectomy technique is described for partial breast reconstruction. Adaptation of the Goldilocks mastectomy technique provides adequate soft tissue for partial breast reconstruction. Using the lower pole deepithelialization breast skin flap provides autologous vascularized tissue to supplement volume loss after tumor and glandular excision. Benign breast disease can create significant breast deformities. Application and combination of the Goldilocks mastectomy technique allow for partial breast reconstruction without the need for an additional donor site or prosthetic devices.
Giant juvenile fibroadenomas are benign neoplasms that typically arise between the ages of 15 to 25 years. Less than 1% of all fibroadenomas arise in this age group. When larger than 5 cm, they are classified as giant fibroadenomas.1
The Goldilocks mastectomy has been previously described for mastectomy reconstruction in patients who do not wish to have autologous or alloplastic reconstruction. The name stems from the popular childhood character who desires the middle road when faced with decisions. Ideal candidates are patient with breast ptosis or macromastia. Rather than removing redundant skin during the mastectomy, the excess skin envelope is deepithelialized and used as vascularized tissue to supplement volume. Though modest in volume, it provides autologous tissue without the need for an additional donor site and avoids complications associated with prosthetic reconstruction.2
CASE REPORT
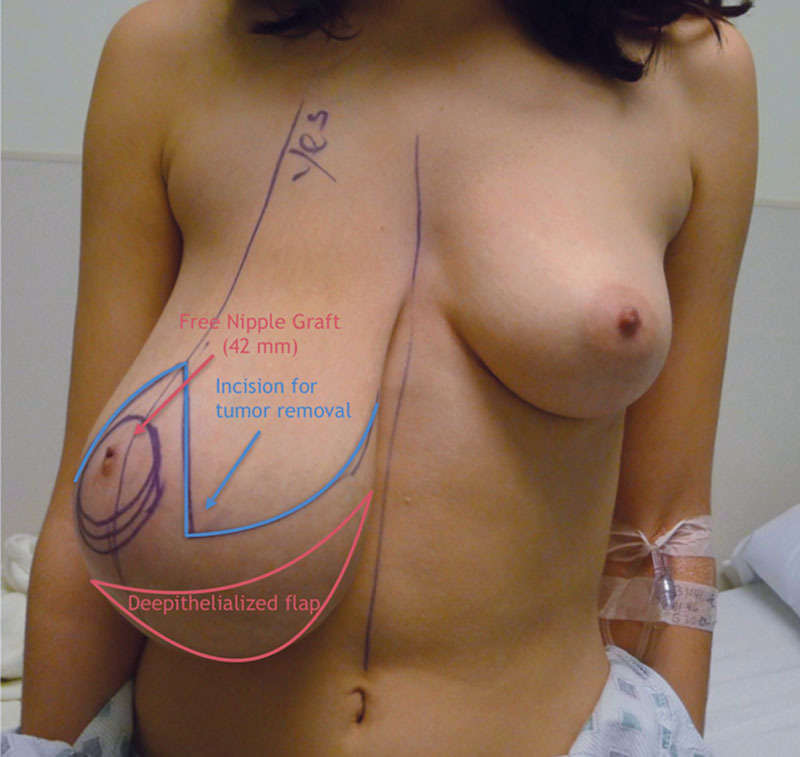
A 21-year-old, nulliparous female presented to her breast surgeon with a 5-year history of a slowly enlarging right breast mass. The mass was very large on presentation, causing the patient emotional distress. The contralateral breast had no physical findings or symptoms (Fig. 1). There was no history of trauma, previous breast surgery, or other comorbidities. Examination of the right breast showed a well-circumscribed, firm, and mobile mass. There was no axillary lymphadenopathy, nipple discharge, or overlying skin changes. Ultrasound revealed a hypoechoic, lobulated, septated lesion greater than 15 cm in diameter. Core needle biopsy demonstrated a fibroadenoma without atypia.
Fig. 1.

Preoperative photograph of giant fibroadenoma of the right breast. Surgical markings include midline, inframammary fold, breast meridian, Wise pattern incision, and free nipple grafting.
Because of the size of her tumor, unilateral mammary hypertrophy, and marked asymmetry, a reconstructive approach would be used to address the redundant skin envelope, the inferior pole defect after excision, and abnormal nipple location. An inverted T incision with a Goldilocks type repair and a free nipple graft was designed after the excision of the giant fibroadenoma. Preoperative markings included the breast meridian, inframammary fold, and the inverted T pattern. A free nipple graft was necessary because the significant skin enveloped reduction after tumor excision would result in poor vascularity of the nipple areolar complex (NAC). The lower pole of the inverted T pattern would be deepithelialized for autoaugmentation (Fig. 2).
Fig. 2.
Schematic of preoperative plan for incisions, free nipple graft, and skin flaps.
The fibroadenoma was resected through the superior horizontal limb of the inverted T pattern. It was well circumscribed and encapsulated and did not invade the overlying skin or underlying chest wall. The tumor weight was 1.1 kg. The defect created by the fibroadenoma excision was located in the inferior pole of the breast. Metallic clips were left at the margins of the tumor to allow for postoperative radiographic observation. Frozen pathology revealed negative margins. However, if final pathology revealed positive margins, further discussion regarding observation versus mastectomy would have been necessary.
The NAC was delineated with a 42-mm cookie cutter, excised as a full thickness graft, and preserved in a saline soaked gauze. The inverted T pattern incisions were made with a 10 blade to the level of the dermis. The inferior skin flap was approximately 1 cm thick after tumor removal and was deepithelialized for autoaugmentation of the lower pole (Fig. 3). The deepithelialized skin flap was sutured superiorly, underneath the remaining native glandular tissue. The vertical component of the inverted T incision was confirmed to be 8 cm in length. The skin envelope was tailor tacked closed with staples, and the vertical component of the incision was placed at 12 cm lateral of the midline. The head of the operative table was raised to assess symmetry in both the sitting and supine positions. The nipple position was determined and marked in the sitting position. A 15-French drain was placed in the inferolateral breast, and the breast was closed in layers. The nipple location was marked with a 42-mm cookie cutter and deepithelialized. The free nipple graft was thinned to the dermal level and placed as a graft. It was sutured in place with a petroleum gauze bolster and 3-0 silk sutures.
Fig. 3.
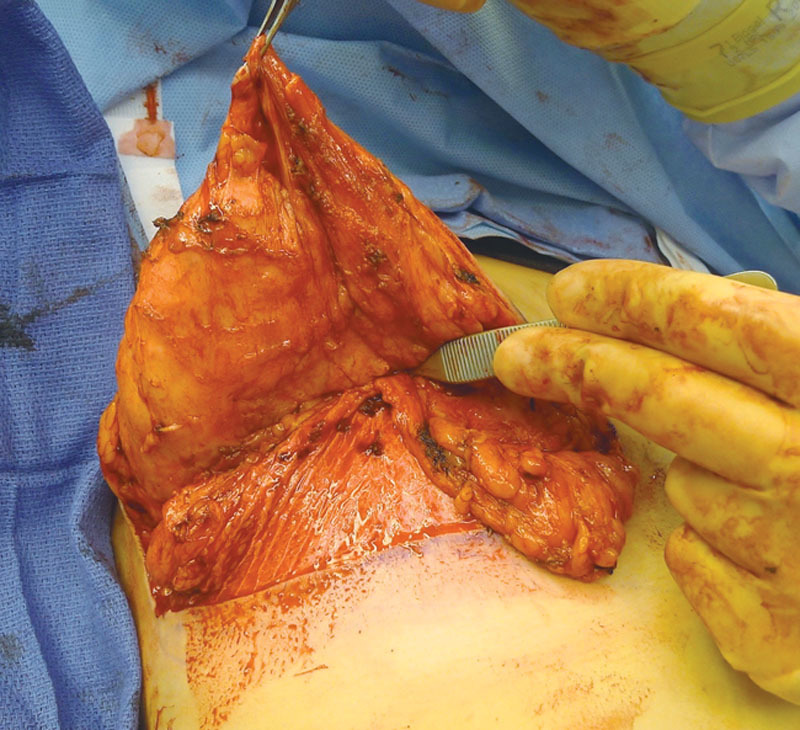
Intraoperative photograph after tumor removal and deepithelialization of inferior skin flap. The Goldilocks style flap was folded superiorly underneath the remaining gland to supplement volume.
At the 1-week follow-up appointment, the nipple graft bolster was removed and had taken well. The 5-week follow-up revealed excellent breast symmetry and contour. The patient was ecstatic with her outcome (Fig. 4).
Fig. 4.

Five-week postoperative photo demonstrating a viable nipple graft and good contour and symmetry.
DISCUSSION
The Goldilocks mastectomy was initially described by Richardson and Ma2 as an alternative to conventional breast reconstruction in patients with macromastia or significant ptosis. In patients desiring mild to moderate volume reconstruction without implants and without an additional donor site, the Goldilocks mastectomy technique may be considered.
In the traditional Goldilocks mastectomy, the NAC is removed. A modification described by Krishnan et al3 demonstrates that this technique can be applied in the nipple-sparing mastectomy patient after explantation of a prosthetic device by deepithelializing redundant skin and imbrication.3,4 In this case, the nipple location on the affected breast was displaced inferiorly by the fibroadenoma. The primary objectives were tumor excision and confirmation of the diagnosis of a benign fibroadenoma. The vascularity of the NAC would be compromised by excision of the tumor. Thus, it was taking off as graft and placed in a symmetric.
In the setting of juvenile benign breast disease, a reliable long-term reconstruction is ideal. Several previous techniques have described using local fasciocutaneous flap after implant removal.5,6 This technique provides a low-cost reconstructive option that avoids the complications associated with prosthetic devices or the morbidity of a separate donor site.
SUMMARY
In the presented case, the giant fibroadenoma resection left a defect that was successfully reconstructed with deepithelialized skin flaps. To our knowledge, this is the first case in which the Goldilocks technique has been described for partial breast reconstruction in the setting of benign juvenile breast disease. The use of redundant breast skin flaps allows for moderate volume augmentation after deepithelialization. This reconstructive technique avoids the need for a separate donor site and does not interfere with future reconstructive options.
Footnotes
Disclosure: Dr. Nahabedian is a consultant for Lifecell, Allergan, and Convatec. Neither of the other authors has any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Sosin M, Pulcrano M, Feldman ED, et al. Giant juvenile fibroadenoma: a systematic review with diagnostic and treatment recommendations. Gland Surg. 2015;4:312–321. doi: 10.3978/j.issn.2227-684X.2015.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson H, Ma G. The Goldilocks mastectomy. Int J Surg. 2012;10:522–526. doi: 10.1016/j.ijsu.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Krishnan NM, Bamba R, Willey SC, et al. Explantation following nipple-sparing mastectomy: the Goldilocks approach to traditional breast reconstruction. Plast Reconstr Surg. 2015;135:795e–796e. doi: 10.1097/PRS.0000000000001130. [DOI] [PubMed] [Google Scholar]
- 4.Ogawa T. Goldilocks mastectomy for obese Japanese females with breast ptosis. Asian J Surg. 2015;38:232–235. doi: 10.1016/j.asjsur.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Gurunluoglu R, Sacak B, Arton J. Outcomes analysis of patients undergoing autoaugmentation after breast implant removal. Plast Reconstr Surg. 2013;132:304–315. doi: 10.1097/PRS.0b013e31829e7d9e. [DOI] [PubMed] [Google Scholar]
- 6.Losken A, Collins BA, Carlson GW. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy and fasciocutaneous flap in women with macromastia. Plast Reconstr Surg. 2010;126:731–738. doi: 10.1097/PRS.0b013e3181e3b38a. [DOI] [PubMed] [Google Scholar]


