Supplemental Digital Content is available in the text.
Summary:
Facial feminization surgery is a term to describe the surgical alteration of a masculine facial appearance to a more feminine appearance, which is most commonly performed for male-to-female transsexual individuals. To alter the midfacial relations, segmentalized osteotomies were performed in selected patients expanding on the established techniques for facial feminization surgery. All patients underwent a preoperative 3D computerized tomography scan and 3D photography before and after the surgery. The inclusion of the midface in surgery was determined based on the relative projection and angle of the zygomatic body compared with the supraorbital region (the supraorbital region was reduced in all patients). Patients were prospectively followed up by 3D surface photography and 3D computerized tomography scans. Rotation and advancement of the zygomatic region was found to be an effective way to further feminize the midfacial appearance in selected male-to-female transsexual patients. No major surgical complications occurred. Although somewhat technically challenging, we suggest that midface surgery should be considered for feminizing purposes in order for the patient to achieve a long-term favorable result compared with other alternative methods.
Gender dysphoria is defined as a marked incongruence between the assigned gender at birth and the experienced gender identity. Furthermore, there is a strong desire to alleviate this dysphoria by means of physical transition.1,2
Male-to-female (MtF) transgender individuals who have undergone transition early in their life generally do not have any challenges with their facial appearance as counter hormones against testosterone prevent the development of male facial structures. Initiation of transition after puberty allows for a persistent masculine appearance of the face and body.3 Facial feminization surgery (FFS) is a term to describe surgical alteration of a masculine facial appearance to a more feminine appearance most commonly performed for MtF transsexual individuals.4,5 The topic was recently reviewed by Morrison et al.6
A new recommendation for specialized care of patients with gender dysphoria was published by the Swedish National Board of Health and Welfare,7 which included FFS as a treatment modality in selected individuals. The first cohort of FFS patients was operated on at the Karolinska University Hospital starting in 2015. To alter the midfacial appearance, segmentalized osteotomies were performed. Although several well-established techniques exist for skeletal feminizations of the forehead and mandible, feminization of the midface has mostly been addressed using implants, fillers, or fat grafting.4,5,8 Although these approaches are technically less challenging, they do come with limitations of need for future revisions in the long run and a difficult-to-predict long-term result as the patient ages.
PATIENTS AND METHODS
Ten patients were recruited at the Stockholm Craniofacial Center between June and December 2015 as a first pilot cohort for FFS funded by public health in Sweden. Six were found suitable for midface surgery as determined by limited projection of the zygomatic body on computerized tomography (CT) scans. All patients underwent surgery to reduce the frontal bone and orbital rims as described by Capitán et al.8 In cases with a prominent mentum and/or mandibular lower border, these areas were treated as previously described.9 Based on 3D CT scans and 3D photography, patients with limited projection at the zygomatic and malar regions were offered bony surgery to augment these areas. A regular Le Fort III advancement would incorporate the nose and thus be unsuitable, as these patients do not wish to increase the projection of the nose nor alter the occlusive plane. Thus, a segmentalized osteotomy approach as pioneered by Hopper et al for children with Apert syndrome10 was used. Surgery was performed by a bicoronal incision to expose each zygomatic arch and the lateral orbital rims. An intraoral sulcus incision was performed for access to the maxilla, and a transconjunctival incision was used for access to the orbit. Osteotomies were performed at the zygomatic arch just inferior to the frontozygomatic suture (See figure, Supplemental Digital Content 1, which displays the coronal view, http://links.lww.com/PRSGO/A356). Using a piezoelectric saw the osteotomy at the frontozygomatic suture was connected to an osteotomy internal to the orbit continuously through the orbital floor past the maxillozygomatic suture (Fig. 1). From intraorally, the anterior wall of the maxilla was cut vertically, medially to the exit of the infraorbital nerve and horizontally superior to the alveolus. Finally, the posterior wall of the maxillary sinus and the posterior part of the zygomatic body were osteotomized to disconnect the whole segment on each side of the face (Fig. 1). The segments were repositioned guided by prebent (intraoperative) titanium microplates at the infraorbital rim so that the infraorbital margin and the zygomatic body were anteriorized 5 mm and the rotation of the zygoma was adjusted cranially by 3 mm. The prebent plates served to correct any asymmetry present and prevent introduction of any assymetries by nonperfect osteosynthesis. The plates were placed low on the infraorbital margin so as to be not easily palpable under the thin eyelid skin. Once the position was deemed satisfactory, osteosynthesis was performed at the zygomatic arch, lateral orbital rim, and lateral pillar of the maxilla (See figure, Supplemental Digital Content 2, which displays 3D CT scan of postoperative osteosynthesis, http://links.lww.com/PRSGO/A357). The maxillary or frontal mucoperiosteum was not removed. All entries were closed in layers by resorbable sutures. All patients could uneventfully be discharged after 1–3 days. One patient did need a lower eyelid correction performed as an outpatient procedure 2 months after the surgery. Apart from this and other expected postoperative effects such as temporary swelling, locally reduced sensibility, and pain, no other complications occurred. Patients were followed up for 11–17 months. A postoperative 3D CT scan was performed before discharge. No soft tissue surgery was performed and no surgery was done to the nose. Results were gathered using 3D photography surface scanning (Fig. 2). (See figure, Supplemental Digital Content 3, which displays the side view of patient (upper half of the figure) and an angled view of another patient (lower half of the figure), http://links.lww.com/PRSGO/A358.)
Fig. 1.

Model of the craniofacial skeleton. Right side, Midface osteotomies and anterior repositioning of the zygomatic/malar complex. Dotted lines denote areas of osteotomies. Left side, Dotted lines denote areas of upper face feminization of the frontal bone and orbit.
Fig. 2.
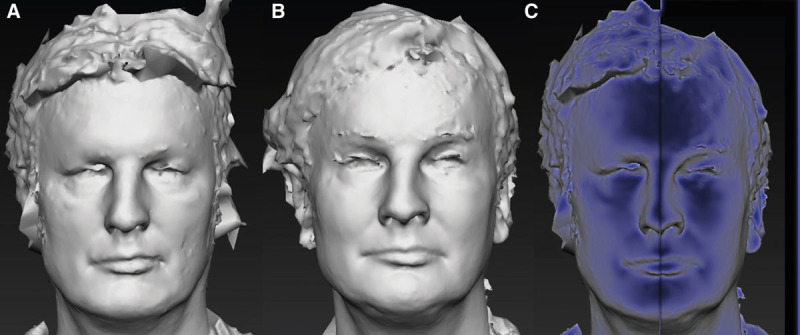
A, Preoperative 3D photography surface scan. Note the flatness of the malar region in this patient. B, Postoperative 3D photography surface scan. C, Pixel intensity illustration of preoperative 3D photography surface scan (left half) and postoperative 3D photography surface scan (right half). Note the intensity shift toward the malar and infraorbital areas of the face postoperatively.
Ethical approval: 2015/2225-31.
DISCUSSION
The relative projection of separate areas of the craniofacial skeleton largely determines the appearance of the facial framework. We would argue that relations rather than absolute measurements within the craniofacial skeleton are probably the key aspects to determine for any reconstruction, although data on normal relations in humans are not reliably available as of yet. For feminization of the upper face the objective was to reduce the supraorbital and frontal sinus protrusion and to create a straighter slope of the frontal bone. The upper and lateral portions of the orbital rims should be less pronounced than in the typical male.4,8,9 In patients with insufficient projection of the midface, reduction of the frontal and supraorbital areas may not fully result in a feminized appearance because the relative position is not posterior enough compared with the zygomatic projections. Our decision to perform bony work in the midface rather than using implants, fillers, or lipofilling was mainly because the patient representation involved in the Swedish National Board of Health and Welfare directive have stressed their wish to have a permanent gender transition as an effect of any procedure. Patients in this group will optimally be treated by surgical means once to then live on in their desired gender without follow-up or need for future revisions in the long run. Because of thinning of the soft tissues, reduced tone of facial musculature, and the effects of gravity with aging, there is often a need for revision of previously augmented areas or repositioning of implants to achieve an appearance adequate for the patient’s age. In contrast, the repositioned skeleton will undergo the same aging as the remainder of the facial skeleton, and it is hoped that repeated procedures will not be needed, at least for feminizing purposes. Long-term follow-up of these patients will help determine if this is indeed a correct proposition.
CONCLUSION
We present a novel method for feminization of the midface in MtF transgender patients. Although the surgery is rather complex compared with other alternatives, it will reasonably lead to long-term predictive results and a favorable appearance as the patient ages.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Dhejne C, Lichtenstein P, Boman M, et al. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One. 2011;6:e16885. doi: 10.1371/journal.pone.0016885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhejne C, Van Vlerken R, Heylens G, et al. Mental health and gender dysphoria: a review of the literature. Int Rev Psychiatry. 2016;28:44–57. doi: 10.3109/09540261.2015.1115753. [DOI] [PubMed] [Google Scholar]
- 3.van de Grift TC, Cohen-Kettenis PT, Steensma TD, et al. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016;45:575–585. doi: 10.1007/s10508-015-0614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ousterhout DK. Feminization of the forehead: contour changing to improve female aesthetics. Plast Reconstr Surg. 1987;79:701–713. doi: 10.1097/00006534-198705000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Altman K. Facial feminization surgery: current state of the art. Int J Oral Maxillofac Surg. 2012;41:885–894. doi: 10.1016/j.ijom.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 6.Morrison SD, Vyas KS, Motakef S, et al. Facial feminization: systematic review of the literature. Plast Reconstr Surg. 2016;137:1759–1770. doi: 10.1097/PRS.0000000000002171. [DOI] [PubMed] [Google Scholar]
- 7.Socialstyrelsen. God Vård av Vuxna Med Könsdysfori. Stockholm, Sweden: Socialstyrelsen; 2015. [Google Scholar]
- 8.Capitán L, Simon D, Kaye K, et al. Facial feminization surgery: the forehead. Surgical techniques and analysis of results. Plast Reconstr Surg. 2014;134:609–619. doi: 10.1097/PRS.0000000000000545. [DOI] [PubMed] [Google Scholar]
- 9.Becking AG, Tuinzing DB, Hage JJ, et al. Transgender feminization of the facial skeleton. Clin Plast Surg. 2007;34:557–564. doi: 10.1016/j.cps.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Hopper RA, Kapadia H, Morton T. Normalizing facial ratios in apert syndrome patients with Le Fort II midface distraction and simultaneous zygomatic repositioning. Plast Reconstr Surg. 2013;132:129–140. doi: 10.1097/PRS.0b013e318290fa8a. [DOI] [PubMed] [Google Scholar]


