Abstract
Foot ulcers account for 15% of comorbidities associated with diabetes. Presently, no device allows the status of foot ulcers to be continuously monitored when patients are not hospitalized. In this study, we describe a temperature and a pH sensor capable of monitoring diabetic foot and venous leg ulcers developed in the frame of the seventh framework program European Union project SWAN-iCare (smart wearable and autonomous negative pressure device for wound monitoring and therapy). Temperature is measured by exploiting the variations in the electrical resistance of a nanocomposite consisting of multiwalled carbon nanotubes and poly(styrene-b-(ethylene-co-butylene)-b-styrene). The pH sensor used a graphene oxide (GO) layer that changes its electrical potential when pH changes. The temperature sensor has a sensitivity of ~85 Ω/°C in the range 25°C–50°C and a high repeatability (maximum standard deviation of 0.1% over seven repeated measurements). For a GO concentration of 4 mg/mL, the pH sensor has a sensitivity of ~42 mV/pH and high linearity (R2=0.99).
Keywords: diabetic foot ulcer, wearable sensors, wound temperature, wound pH
Introduction
Diabetes is one of the most common diseases and its incidence is rapidly increasing. According to the 2015 edition of the IDF Diabetes Atlas, yearly published by the International Diabetes Federation, there are 415 million people worldwide with diabetes and this number is expected to grow up to 642 million in 2040, with an estimated 55% increase in 25 years.1 The diffusion of diabetes is not uniform in population. In the wealthiest countries, it mostly affects people >50 years of age, whereas it is more widespread among young people in middle-income countries.2
In 2015, ~5 million deaths of people could be ascribed to diabetes, mostly related to the comorbidities of the disease and its complications.1 Among the chronic complications of diabetes, the diabetic foot (DF), a chronic ulcerative condition, is the most prevalent and severe because it affects 25% of patients at least once in their life with a survival expectation less than that of many forms of cancer.3 DF ulcers are correlated to several risk factors, such as neuropathy (86% of cases), peripheral arterial disease (49% of cases), minor foot trauma, and foot deformity.4 The risk of amputation is not negligible; DF is the major cause of lower extremity amputations (LEAs) with a risk 20-fold higher than that of the general population and a limb amputated every 30 seconds.5
The healing rate of DF ulcers, defined as the rate of ulcers completely re-epithelized, stable for at least 2 weeks varies according to their pathogenesis,6 whereas the incidence is, depending on the reference population, 3%–5% for major amputations and 5%–40% for minor amputations. Another study reported that amputations range from 2.1 to 13.7 per 1,000.7–9 The association of ischemia with infection increases 300% the risk of LEAs in DF ulcer patients, whereas DF ulcers precede LEAs in >85% of the cases.10 The impact of such ulcers on the patients’ quality of life is high, as they impair both personal and work relationships, with heavy psychological consequences.11 In the United States, a substantial burden between $9 billion and $13 billion can be estimated for the health care system, summing the impact on private and public payers.12
Infection in DF ulcers is a major risk factor leading to amputation,10 and for this reason, the monitoring of the foot ulcers’ status may be of a great importance to ensure the effectiveness of therapies and the safety of patients. SWAN-iCare (smart wearable and autonomous negative pressure device for wound monitoring and therapy) is a large-scale integrating European project seventh framework program that tackles the challenge of developing wearable devices and sensors to monitor and manage foot and venous ulcers.13,14 The objective is to deliver a personalized therapy to patients whose ulcer status is remotely monitored so that a prompt action can be put in place in case of infection. The patient does not need to be hospitalized and can continue his/her normal life while a set of wearable sensors transmits the ulcer condition to a database accessible by clinicians. The sensors will monitor parameters such as transepidermal water loss of the perilesional skin, glucose, body temperature, skin and ulcer temperature, SpO2, levels of matrix metalloproteinases and bacteria, and the pH of the ulcer. There is a general consensus that there is a strong relationship between the ulcer temperature and the degradation of the ulcer status.15–19 In fact, an increase in the basal temperature can be a warning of the ulcer onset even 1 week before it starts.20 Besides temperature, an increase of pH at the wound can also be a sign of infection as it is related to the presence of bacteria that proliferate in the ulcer.15,21–25
High precision handheld infrared thermographic scanners and cameras can be used to measure ulcer temperature. However, these devices are expensive and measurements are limited to research purposes. Presently, no wearable device is available to continuously monitor the ulcer temperature. Similar consideration can be made for the measurement of pH as the market only offers handheld pH meters.
This study describes the technologies and principles of the temperature and pH sensors that are under development in the SWAN-iCare project. We report the sensing materials under investigation and their early performances for a future use to fabricate wearable sensors for monitoring DF ulcers.
Materials and methods
Temperature
A temperature-sensitive nanocomposite material was prepared consisting of a conducting phase of multiwalled carbon nanotubes (MWCNTs, Baytubes C150 P) dispersed in toluene within an insulating phase of a thermoplastic elastomer, poly(styrene-b-(ethylene-co-butylene)-b-styrene) (SEBS, Europrene Sol TH 212). In these kinds of materials, temperature variations lead to changes in the electrical resistance, so that they can be used to fabricate temperature sensors.26–29 A digital multimeter was used for log resistance values (Model 2700, Keithley) and a thermostatic bath (F 32, Julabo) as a reference temperature. A dispersion of MWCNTs–SEBS was obtained as reported in a study by Matzeu et al.26 A volume equal to 10 µL of the dispersion was drop casted onto a pair of gold electrodes (length of 7 mm) and let dry at room temperature to obtain a film (Figure 1). The electrodes were fabricated onto a Kapton® substrate (thickness of 50 µm; CAD Line, Pisa, Italy). Copper tracks were obtained by photolithography and electroplated with nickel and gold to fabricate the electrodes (thickness of copper 35 µm, nickel 3.0 µm, and gold 1.2 µm). The nanocomposite film was annealed at 145°C for 4 hours. This treatment decreases sensitivity but improves stability, that has been identified as a major problem in the previous study,30 resulting in more accurate measurements.31
Figure 1.
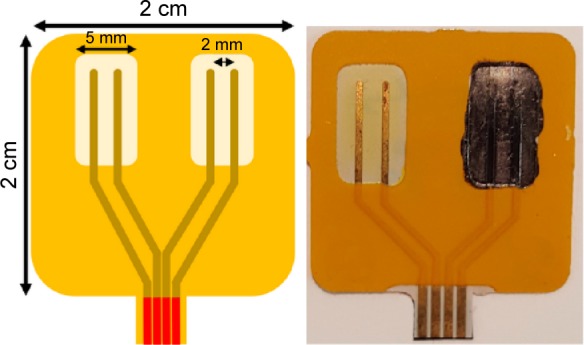
The temperature sensor.
Notes: Left: drawing of the Kapton substrate for the temperature sensor. Right: substrate with an electrode pair coated by a film of MWCNTs–SEBS.
Abbreviations: MWCNTs, multiwalled carbon nanotubes; SEBS, poly(styrene-b-(ethylene-co-butylene)-b-styrene).
pH
We exploited the potentiality of graphene oxide (GO, Graphenea) to measure pH because this material changes its potential in water solution when the pH changes.32 Figure 2 shows the substrate used for the tests. A GO layer coated the working electrode (WE) of a screen printed-board (C220BT, 33×10×0.5 mm, Dropsens). This board has gold counter electrode (CE) and WE (diameter 4 mm), whereas the reference electrode (RE) consists of Ag/AgCl. The electrical contacts are in silver. The pH was measured as the change of the open circuit potential between the WE and the RE (Palmsens3, Palmsens). Five microliters of a GO dispersion in water was deposited onto the WE and let dry at room temperature. The sensor was compared with a commercial pH meter (Basic 20 by Crison with Micro P glass electrode by XS Sensor) in Hank’s Balanced Salt Solutions (HBSS; Sigma-Aldrich). Different pH values were obtained adding NaOH and HCl solutions.
Figure 2.
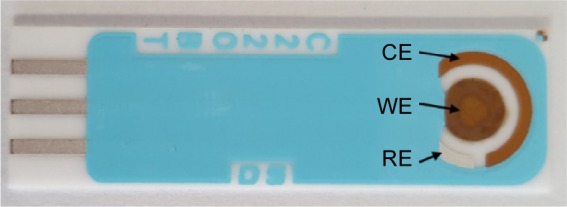
Screen-printed board used for the pH measurement.
Notes: The WE is coated with a graphene oxide layer. The RE is Ag/AgCl.
Abbreviations: CE, counter electrode; RE, reference electrode; WE, working electrode.
Results
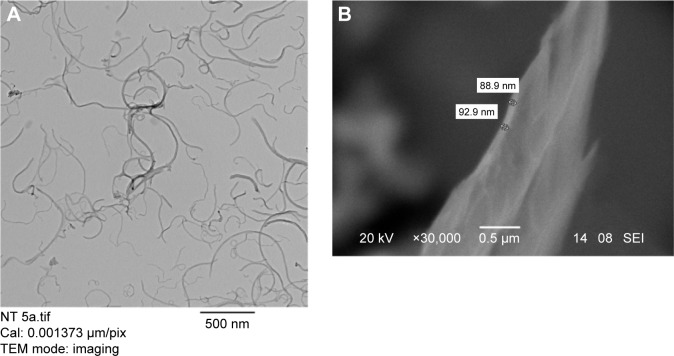
As SEBS is an insulating thermoplastic elastomer that expands or shrinks with temperature, this effect lead to changes in the topology of the MWCNT network. Temperature affected the electrical resistance of the film due to two main concurrent phenomena. In the first place, MWCNTs change their intrinsic resistance with temperature. Different behaviors were observed in different kinds of carbon nanotubes (eg, zigzag and armchair),33 but the MWCNTs showed a semiconductor behavior with a decrease of resistance at increasing temperatures. In the second place, the electrical resistance changed due to the different thermal expansion coefficients of the insulating phase (polymer matrix) and the conducting phase (MWCNTs), that led to a rearrangement of the topology of the network at different temperatures. SEBS shows a small but significant percentage of crystalline phase that melts just above room temperature,29 reinforcing the rubbery character of the material. The mobility of the MWCNTs is enhanced in a more “fluid” polymer matrix, and this makes it easier for individual nanotubes to connect each other leading to the decrease of the resistance that had been observed within different measurement cycles.26 The relative importance of this contribution has been strongly reduced by the annealing treatment and paying the price of a reduced sensitivity to improve the stability of the films and to obtain more reproducible measurements. Figure 3A shows the transmission electron microscopy (TEM) image (CM12, Philips) of MWCNTs–SEBS after a sonication of 5 minutes. SEBS is not visible during TEM analysis; however, Figure 3A allows the good dispersion of MWCNTs in SEBS to be confirmed.
Figure 3.
TEM and SEM images of MWCNTs-SEBS and graphene oxide, respectively.
Notes: (A) TEM image of a MWCNTs–SEBS composite after a 5-minute sonication. The MWCNTs are well dispersed (SEBS are not visible in TEM). (B) Scanning electron microscopy image of a graphene oxide layer.
Abbreviations: MWCNTs, multiwalled carbon nanotubes; SEBS, poly(styrene-b-(ethylene-co-butylene)-b-styrene); TEM, transmission electron microscopy; SEM, scanning electron microscope.
Figure 4 shows the calibration curve for an annealed nanocomposite MWCNTs–SEBS (20% w/w of MWCNTs) obtained over seven repeated measurement cycles, from minimum to maximum temperature and vice versa. The maximum standard deviation was 0.08°C in the interval °C. The sensitivity was ~85 Ω/°C, and the response time was 30 s/°C. The error calculated using this calibration curve was 0.3°C±0.2°C.
Figure 4.
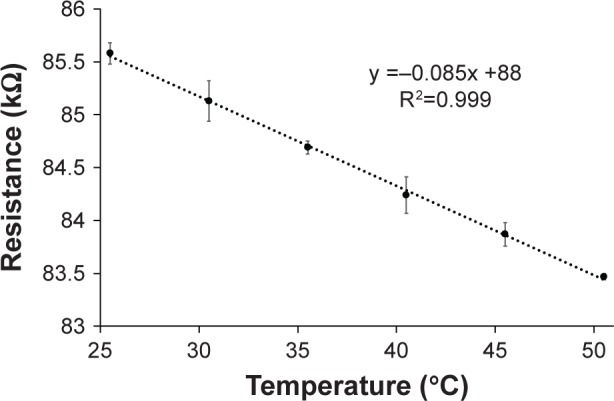
Calibration curve of a 20% w/w multiwalled carbon nanotubes–poly(styrene-b-(ethylene-co-butylene)-b-styrene) nanocomposite.
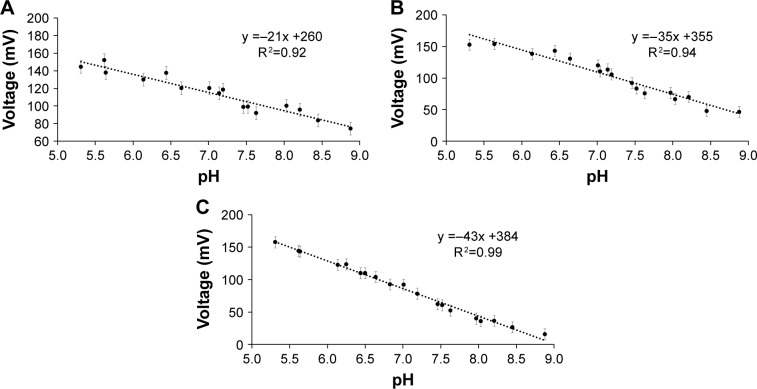
We tested three different GO concentrations to assess the sensitivity to pH. Figure 5 shows the calibration curves for different pH values at GO concentrations of 0.04, 0.4, and 4 mg/mL. Figure 3B shows the scanning electron microscope (SEM) image (XL30, Philips) of a GO film (thickness ~90 nm) for a concentration of 4 mg/mL. In a recent study,34 we reported as the sensor was able to record pH over 3 days in human plasma. The same sensor was used after 20 days from immersion in plasma for another 3-day measurement campaign and observed a difference of only 0.14±0.09 pH units compared with the commercial pH meter (Figure 6).
Figure 5.
Calibration curves for three GO pH sensors obtained at three different GO concentrations: (A) 0.04 mg/mL, (B) 0.4 mg/mL, and (C) 4 mg/mL.
Note: Sensitivity increases with increasing concentrations.
Abbreviation: GO, graphene oxide.
Figure 6.
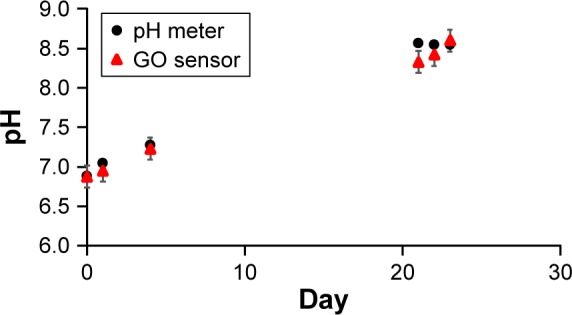
Test of the GO pH sensor in human plasma in comparison with a commercial pH meter.
Note: The GO sensor and the pH meter were always immersed in human plasma during the test.
Abbreviation: GO, graphene oxide.
Discussion
The temperature sensor showed a high linearity (R2=0.999) and sensitivity (~85 Ω/°C) between 25°C and 50°C. The annealing improved both the linearity and the repeatability, thus indicating a stabilization of the nanocomposite micro-domains. The size and shape of the Kapton substrate can be adapted to the dimension of the foot ulcer cavity for a smooth insertion. Before testing the sensor on patients, a protection coating should be applied onto the MWCNTs–SEBS nanocomposite. The role of the coating is twofold: it serves as a protection layer to avoid the nanocomposite to be damaged and to guarantee the biocompatibility in contact with the ulcer. For this purpose, a layer of Parylene C could be used because its biocompatibility is already established in the literature, although its effect on the shrinkage/expansion of the nanocomposite should be investigated.34,35
The pH sensor proved to be suitable for pH measurement during laboratory tests. When the concentration of GO was increased up to 4 mg/mL, the sensitivity (~43 mV/pH), linearity (R2=0.99), and repeatability (three measurements per pH value, ±0.2 pH units) improved. These results are sufficient for considering this sensor as a potential candidate for tests on patients. The GO biocompatibility of this sensor has not yet been assessed, but a study suggested that at concentration <20 µg/mL, the GO should not be cytotoxic.36
Conclusion
In this study, we described two temperature- and pH-sensitive materials that may be used to monitor chronic ulcers status over time. The Kapton board is suitable to be used for tests with patients and part of future work will be dedicated to design a Kapton board where both sensors can be fabricated.
The tests performed in laboratory showed promising results, but we are aware that these sensors still need to be clinically validated; however, some pivotal experiences with non-wearable temperature sensors on DF patients in a real clinical setting have already demonstrated how profitable such an information could be in terms of a better understanding of the clinical course of the disease, that encompass both chronic sub-clinical phases and acute phases that are mostly triggered by super-infection of chronic ulcers and of improving the clinical outcomes because of the timely modifications of local and systemic therapies.17–19
Therefore, the possibility of introducing wearable sensors, eventually embedded in dressings or bandaging, for a real-time monitoring of variables such as pH and temperature in DF-ulcerated patients could help clinicians in improving the quality of treatments for such a complex pathology, specially increasing the timeliness of intervention, that has been demonstrated to be directly correlated to its effectiveness, both in terms of reduction of LEAs and healing of the ulceration.37–39 Future work will be to perform a randomized controlled trial, including a sterilization process for the materials; to confirm this hypothesis; and to validate this new technology with clinical evidence.
Acknowledgments
This work was supported by EU-funded FP7 ICT-317894 SWAN-iCare project.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.International Diabetes Federation . IDF Diabetes Atlas. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Google Scholar]
- 2.Scully T. Diabetes in numbers. Nature. 2012;485(7398):S2–S3. doi: 10.1038/485s2a. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong DG, Wrobel J, Robbins JM. Guest editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J. 2007;4(4):286–287. doi: 10.1111/j.1742-481X.2007.00392.x. [DOI] [PubMed] [Google Scholar]
- 4.Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 2007;50(1):18–25. doi: 10.1007/s00125-006-0491-1. [DOI] [PubMed] [Google Scholar]
- 5.Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719–1724. doi: 10.1016/S0140-6736(05)67698-2. [DOI] [PubMed] [Google Scholar]
- 6.Yazdanpanah L, Nasiri M, Sara Adarvishi S. Literature review on the management of diabetic foot ulcer. World J Diabetes. 2015;6(1):37–53. doi: 10.4239/wjd.v6.i1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akhtar S, Schaper N, Apelqvist J, Jude E. A review of the Eurodiale studies: what lessons for diabetic foot care? Curr Diab Rep. 2011;11(4):302–309. doi: 10.1007/s11892-011-0195-x. [DOI] [PubMed] [Google Scholar]
- 8.Apelqvist J, Larsson J. What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes Metab Res Rev. 2000;16(Suppl 1):S75–S83. doi: 10.1002/1520-7560(200009/10)16:1+<::aid-dmrr139>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 9.Calhoun JH, Overgaard KA, Stevens CM, Dowling JP, Mader JT. Diabetic foot ulcers and infections: current concepts. Adv Skin Wound Care. 2002;15(1):31–42. doi: 10.1097/00129334-200201000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia. 2008;51(5):747–755. doi: 10.1007/s00125-008-0940-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siersma V, Thorsen H, Holstein PE, et al. Importance of factors determining the low health-related quality of life in people presenting with a diabetic foot ulcer: the Eurodiale study. Diabet Med. 2013;30(11):1382–1387. doi: 10.1111/dme.12254. [DOI] [PubMed] [Google Scholar]
- 12.Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37(3):651–658. doi: 10.2337/dc13-2176. [DOI] [PubMed] [Google Scholar]
- 13.Texier I, Xydis S, Soudris D, et al. SWAN-iCare project: towards smart wearable and autonomous negative pressure device for wound monitoring and therapy; 4th International Conference on wireless mobile communication and healthcare (Mobihealth); Athens, Greece. Nov 3–5, 2014; pp. 357–360. [Google Scholar]
- 14.Texier I, Marcoux P, Pham P, et al. SWAN-iCare: a smart wearable and autonomous negative pressure device for wound monitoring and therapy; IEEE 2013 International Conference on embedded computer systems: architectures, modelling, and simulation (SAMOS XIII); Samos, Greece. July 15–18, 2013; pp. 137–144. [Google Scholar]
- 15.Salvo P, Dini V, Di Francesco F, Romanelli M. The role of biomedical sensors in wound healing. Wound Med. 2015;8:15–18. [Google Scholar]
- 16.Lavery LA, Higgins KR, Lanctot DR, et al. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care. 2004;27(11):2642–2647. doi: 10.2337/diacare.27.11.2642. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, Lavery LA. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Am J Med. 2007;120(12):1042–1046. doi: 10.1016/j.amjmed.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 18.Dini D, Salvo P, Janowska A, Di Francesco F, Romanelli M. Correlation between wound temperature obtained with an infrared camera and clinical wound bed score in venous leg ulcers. Wounds. 2015;27(10):274–278. [PubMed] [Google Scholar]
- 19.Houghton VJ, Bower VM, Chant DC. Is an increase in skin temperature predictive of neuropathic foot ulceration in people with diabetes? A systematic review and meta-analysis. J Foot Ankle Res. 2013;6(1):31. doi: 10.1186/1757-1146-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roback K. An overview of temperature monitoring devices for early detection of diabetic foot disorders. Expert Rev Med Devices. 2010;7(5):711–718. doi: 10.1586/erd.10.35. [DOI] [PubMed] [Google Scholar]
- 21.Salvo P, Melai B, Bianchi S, et al. Non-invasive sensors for wound monitoring and therapy; Engineering in Medicine and Biology Society (EMBC), 37th Annual International Conference of the IEEE; Milan, Italy. 2015. [Google Scholar]
- 22.Salvo P, Smajda R, Dini V, et al. A D-optimal design to model the performances of dressings and devices for negative pressure wound therapy. J Tissue Viability. 2016;25(2):83–90. doi: 10.1016/j.jtv.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 23.McArdle C, Lagan K, Spence S, McDowell D. Diabetic foot ulcer wound fluid: the effects of pH on DFU bacteria and infection. J Foot Ankle Res. 2015;8(Suppl 1):A8. [Google Scholar]
- 24.Nagoba BS, Suryawanshi NM, Wadher B, Selkar S. Acidic environment and wound healing: a review. Wounds. 2015;27(1):5–11. [Google Scholar]
- 25.Martinez-De Jesus FR, Ramos-De la Medina A, Remes-troche JM, et al. Efficacy and safety of neutral pH superoxidised solution in severe diabetic foot infections. Int Wound J. 2007;4(4):353–362. doi: 10.1111/j.1742-481X.2007.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matzeu G, Pucci A, Savi S, Romanelli M, Di Francesco F. A temperature sensor based on a MWCNT/SEBS nanocomposite. Sensor Actuat A-Phys. 2012;178:94–99. [Google Scholar]
- 27.Giuliani A, Placidi M, Di Francesco F, Pucci A. A new polystyrene-based ionomer-MWCNT nanocomposite for wearable skin temperature sensors. React Funct Polym. 2014;76:57–62. [Google Scholar]
- 28.Biver T, Criscitiello F, Di Francesco F, Minichino M, Swager TM, Pucci A. Perylene bisimide/MWCNTs water dispersions for miniaturized temperature sensors. RSC Adv. 2015;5:65023–65029. [Google Scholar]
- 29.Holden G, Legge CR, Quirk RP, Schroeder HE, editors. Thermoplastic Elastomers: A Comprehensive Review. 2nd ed. Munich, Germany: Hanser & Hanser/Gardner; 1996. [Google Scholar]
- 30.Calisi N, Giuliani A, Alderighi M, et al. Factors affecting the dispersion of MWCNTs in electrically conducting SEBS nanocomposites. Eur Polym J. 2013;49(6):1471–1478. [Google Scholar]
- 31.Shih CJ, Lin S, Sharma R, Strano MS, Blankschtein D. Understanding the pH-dependent behavior of graphene oxide aqueous solutions: a comparative experimental and molecular dynamics simulation study. Langmuir. 2012;28(1):235–241. doi: 10.1021/la203607w. [DOI] [PubMed] [Google Scholar]
- 32.Baughman RH, Zakhidov AA, de Heer WA. Carbon nanotubes – the route toward applications. Science. 2002;297(5582):787–792. doi: 10.1126/science.1060928. [DOI] [PubMed] [Google Scholar]
- 33.Melai B, Salvo P, Calisi N, et al. A graphene oxide pH sensor for wound monitoring; 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); Orlando, USA. August 16–20, 2016; pp. 1898–1901. [DOI] [PubMed] [Google Scholar]
- 34.Chang TY, Yadav VG, De Leo S, et al. Cell and protein compatibility of parylene-C surfaces. Langmuir. 2007;23(23):11718–11725. doi: 10.1021/la7017049. [DOI] [PubMed] [Google Scholar]
- 35.Hsu JM, Rieth L, Normann RA, Tathireddy P, Solzbacher F. Encapsulation of an integrated neural interface device with Parylene C. IEEE Trans Biomed Eng. 2009;56(1):23–29. doi: 10.1109/TBME.2008.2002155. [DOI] [PubMed] [Google Scholar]
- 36.Wang K, Ruan J, Song H, et al. Biocompatibility of graphene oxide. Nanoscale Res Lett. 2011;6(1):1–8. doi: 10.1007/s11671-010-9751-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mills JL, Beckett WC, Taylor SM. The diabetic foot: consequences of delayed treatment and referral. South Med J. 1991;84(8):970–974. [PubMed] [Google Scholar]
- 38.Chantelau E. The perils of procrastination: effects of early vs delayed detection and treatment of incipient Charcot fracture. Diabet Med. 2005;22(12):1707–1712. doi: 10.1111/j.1464-5491.2005.01677.x. [DOI] [PubMed] [Google Scholar]
- 39.Faglia E, Clerici G, Caminiti M, Quarantiello A, Gino M, Morabito A. The role of early surgical debridement and revascularization in patients with diabetes and deep foot space abscess: retrospective review of 106 patients with diabetes. J Foot Ankle Surg. 2006;45(4):220–226. doi: 10.1053/j.jfas.2006.04.002. [DOI] [PubMed] [Google Scholar]