Abstract
Rationale:
Postliver transplant periampullary carcinoma is an extremely uncommon disease.
Patient concerns:
Cutaneous jaundice in a patient who had received a liver transplant 4 years earlier.
Diagnosis:
Periampullary carcinoma.
Interventions:
Radiofrequency ablation plus fully covered self-expanding metal stents (FCSEMS).
Outcomes:
The treatment of malignant neoplasm of the ampulla of Vater is the patient by radiofrequency ablation plus FCSEMS placement was successful. No complications occurred.
Lessons:
This is the first reported case of a liver transplant patient with inoperable periampullary carcinoma successfully treated by radiofrequency ablation plus FCSEMS placement. Our experience will be useful to other surgeons in managing similar patients in the future.
Keywords: endoscopic radiofrequency ablation, ERCP, liver transplantation, periampullary carcinoma, self-expandable metallic stent
1. Introduction
Periampullary tumors are uncommon neoplastic diseases that arise from the confluence of the common bile duct with the main pancreatic duct. Endoscopic endobilliary self-expandable metallic stent (SEMS) has been conventionally employed to manage malignant biliary obstruction not amenable to curative surgical resection.[1,2] However, stent placement merely alleviates biliary obstruction and stent blockage may ensue in greater than 50% of the cases within 6 to 8 months of SEMS placement.[3] Radiofrequency ablation combined with metallic stent has recently been reported for treating malignant biliary obstruction,[4–7] with a benign safety profile and a favorable benefit in survival.[8,9] However, there has been no report on the combined use of radiofrequency ablation and SEMS in carcinoma of the periampulla in postliver transplant recipients. We report our experience with 1 case of Vater ampulla carcinoma 4 years after liver transplant surgery who was managed by radiofrequency ablation with SEMS.
2. Case report
A 56-year-old male patient was admitted in April, 2014, because of skin jaundice for 1 week. The patient received orthotopic liver transplantation 4 years ago because of hepatitis B virus (HBV)-associated portal hypertension. He received postoperative immunosuppressive therapy and anti-HBV therapy. The postoperative function of the liver graft was normal. They patient provided written informed consent to the operation.
Physical examination did not show any abnormalities except jaundice. Total bilirubin at admission was 562.45 μmol/L (normal references, 0–17.1 μmol/L) and direct bilirubin 342.35 μmol/L (normal references, 0–6.8 μmol/L), alkaline phosphatase 314.3 U/L (normal references, 45–125 U/L), and CA-199 404.5 U/mL (normal references, 0 to 35 U/mL). Magnetic resonance cholangiopancreatography (MRCP) revealed a mass in the ampulla of the duodenum, and dilation of intrahepatic and extrahepatic biliary ducts and pancreatic ducts (Fig. 1A). Abdomen enhancement CT demonstrated thickening of the lower segment of the common bile duct, and the main portal vein trunk and branches were not visualized (Fig. 1B). The length of stricture in the bile duct was approximately 2.5 cm with more than 75% of the diameter of the biliary duct stenosed. Malignancy of the pancreatic duct was considered. Pathologic examination of the endoscopic biopsy specimens from the ampulla of Vater revealed advanced intraepithelial neoplastic changes and focal malignant changes (Fig. 2).
Figure 1.

(A) Magnetic resonance cholangiopancreatography (MRCP) reveals a mass in the ampulla of the duodenum of a 56-year-old male patient who developed Vater ampulla carcinoma 4 years after liver transplant surgery. (B) Abdomen enhancement CT demonstrates thickening of the lower segment of the common bile duct, and the main portal vein trunk and branches are not visualized. CT = computed tomography, MRCP = magnetic resonance cholangiopancreatography.
Figure 2.
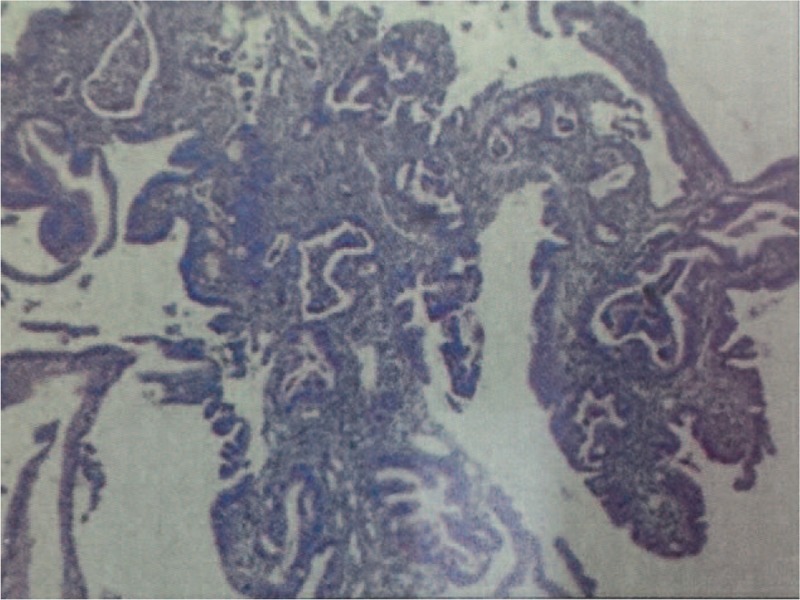
Pathological examination of endoscopic biopsy specimens from the ampulla of Vater reveals advanced intraepithelial neoplastic changes and focal malignant changes while post-transplantation lymphoid proliferative disease is not present. H&E staining; ×100. H&E = hematoxylin and eosin.
ERCP was done to determine location and length of the lesion and a draining nasobilliary tube was placed. At day 3 post-nasobilliary tube placement, total bilirubin stood at 204.11 μmol/L, direct bilirubin 96.80 μmol/L, and alkaline phosphatase 293.1U/L. The nasobilliary tube was then removed and a guidewire was placed via endoscopic biliary catheterization. The stricture was dilated with an 8.5 F dilator, and then the radiofrequency ablation catheter (Habib EndoHPB, EMCISION, UK) was advanced under the guidance of the guidewire. After the tumor was precisely located under visual guidance, ablation was initiated (power 10 W; ablation time 120 seconds; ablation temperature 60°C).[4] Postablation imaging showed dilation of the biliary stricture and the radiofrequency ablation electrode was withdrawn from the biliary tract and then advanced to the carcinoma in the periampulla and a second ablation was carried out (Fig. 3) followed by placement of fully covered self-expanding metal stents (FCSEMS) (Boston Scientific Corporation). The patient suffered no complications and was discharged at postoperative day 19. At 10 months of follow-up, total bilirubin stood at 34.21 μmol/L, direct bilirubin 20.15 μmol/L and alkaline phosphatase 95.30 U/L, and CA-199 was 73.67 U/L (Table 1). Endoscopic retrograde cholangiao-pancreatography (ERCP) showed that the common bile duct was patent, and the dilated segment of the bile duct did not show stenosis following radiofrequency ablation (Fig. 4A). No tumor invasion within the stent was observed (Fig. 4B).
Figure 3.

Radiofrequency ablation of the ampulla in the duedenoum (periampullary carcinoma).
Table 1.
Biochemical changes before and after radiofrequency ablation therapy.
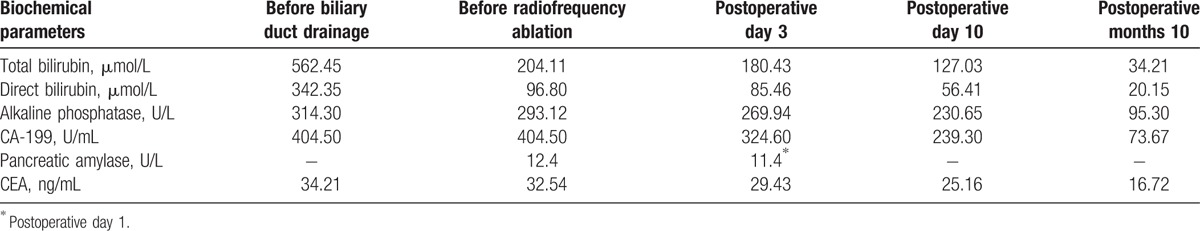
Figure 4.
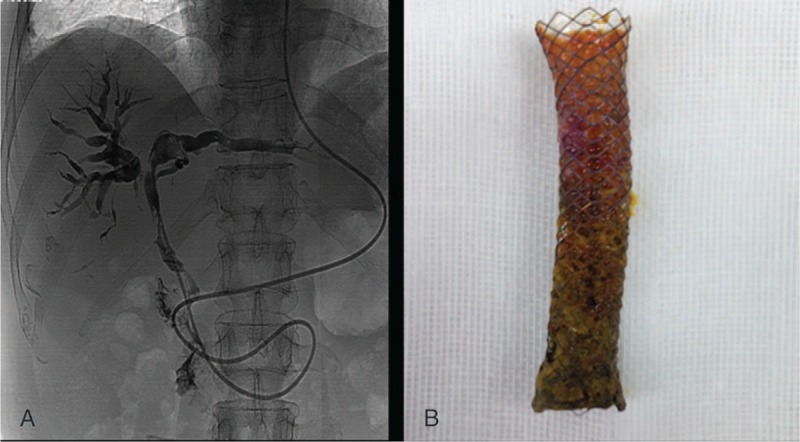
(A) Imaging of the biliary tract at10 months postoperatively. (B) Removed FCSEMS at 10 months postoperatively. FCSEMS = fully covered self-expanding metal stents.
3. Discussion
We report the successful treatment of a patient with malignant neoplasm of the ampulla of Vater by radiofrequency ablation plus stent placement. For biliary malignancies not amenable to curative surgical resection, stent has been commonly used for alleviating obstructive jaundice. However, tumor regrowth often causes stent blockage; thus, inhibiting tumor growth and prolonging stent patency are critical in management of biliary malignancies. Recently, radiofrequency ablation has been used to treat biliary malignancies.[10–13]
The number of living patients with liver transplant has increased over the recent years given improvement in survival and emergence of gastrointestinal tumors has been reported recently.[10,11] We searched PubMed, and Chinese databases Wangfang and CNKI for literature on emergent neoplasms postliver transplant. Between January, 1993, and June, 2012, 47 papers were published on emergent neoplasms postliver transplant. Among 27,301 liver transplant recipients, gastrointestinal tract tumors were found in 208 cases with an incidence rate of 0.76%, including 1 case of biliary tract carcinoma, 16 cases of pancreatic cancer, and 3 cases of periampullary cancer. Our patient developed periampullary cancer 4 years after liver transplant with involvement of the portal vein. Because the tumor was inoperable, we treated the patient with radiofrequency ablation in combination with FCSEMS placement. The patient saw marked improvement in biochemical markers including CA-199 and rapid decline in jaundice. Though the condition of the patient remained satisfactory at 10 months of follow-up, the longer term outcome of the treatment awaits further evaluation. Endoscopic ultrasound remains a valuable diagnostic modality in the diagnosis of periampullary tumor. Unfortunately, the endoscopic ultrasound examination was not performed in our patient as it was not available at our hospital.
Radiofrequency ablation can remove tumor tissues and achieve reduction in tumor volume in patients with inoperable biliary tract cancer, with demonstrable survival benefit.[5] Moreover, endobilliary radiofrequency ablation prolongs patency of FCSEMS, thus avoiding the suffering from and the cost of repeated endoscopic therapies and changes of stents. Reduction in tumor volume allows placement of larger stents, which facilitates better draining and prolongs patency. This is particularly beneficial for patients with severe stricture of the bile duct that precludes the use of larger stents. For these patients, endobilliary radiofrequency ablation provides a second chance for stenting, thus avoiding complications of percutaneous transhepatic cholangial drainage.
Endobilliary radiofrequency ablation may cause thermal injury-associated fistula, hemorrhaged , and pancreatitis.[11,14] It is critical that the radiofrequency ablation electrode be properly positioned in the bile duct and the area to be ablated fall within the stenosed segment of the bile duct. In addition, the electrode should not come into contact with the stent. The electrode should be kept immobile for 1 minute at the end of ablation to facilitate biliary tract remodeling. In case of bleeding, hemostasis can be achieved by compression with balloon or FCSEMS.[15] No bile duct fistula as a result of radiofrequency ablation has been reported so far and our patient also did not develop bile duct fistula. Bile duct fistula might ensue as a result of that the ablation power is too high or the ablation time is too long.[16] Currently, it is considered safe when radiofrequency ablation is performed at a power of 5 to 10 W for 90 s to 120 s. On the other hand, pancreatitis most commonly occurs when the lower segment of the bile duct is ablated. Thermal conduction may cause injury in the pancreas, leading to blockage of the pancreatic duct. Pancreatitis may be managed with conventional antibiotic therapy and preventive measures such as stent placement may also be taken.
In conclusion, we report the first case of a liver transplant patient with inoperable periampullary carcinoma who was successfully managed by radiofrequency ablation plus FCSEMS placement. Postliver transplant periampullary carcinoma is extremely uncommon and our experience will be useful to other surgeons in managing similar patients in the future.
Footnotes
Abbreviations: ERCP = endoscopic retrograde cholangiao-pancreatography, FCSEMS = fully covered self-expanding metal stents, HBV = hepatitis B virus, SEMS = self-expandable metallic stent.
Funding: This study was supported by National high technology research and development plan (No. 2012AA021001), Tianjin science and technology plan (key) project (No. 14ZCZDSY00019) and Tianjin Health Bureau project (12KG103).
The authors have no conflicts of interest to disclose.
References
- [1].Andersen JR, Sorensen SM, Kruse A, et al. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut 1989;30:1132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Shepherd HA, Royle G, Ross AP, et al. Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Brit J Surg 1988;75:1166–8. [DOI] [PubMed] [Google Scholar]
- [3].Loew BJ, Howell DA, Sanders MK, et al. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: final results of an international multicenter, randomized, controlled trial. Gastrointest Endosc 2009;70:445–53. [DOI] [PubMed] [Google Scholar]
- [4].Alis H, Sengoz C, Gonenc M, et al. Endobiliary radiofrequency ablation for malignant biliary obstruction. Hepatobiliary Pancreat Dis Int 2013;12:423–7. [DOI] [PubMed] [Google Scholar]
- [5].Kallis Y, Phillips N, Steel A, et al. Analysis of endoscopic radiofrequency ablation of biliary malignant strictures in pancreatic cancer suggests potential survival benefit. Dig Dis Sci 2015;60:3449–55. [DOI] [PubMed] [Google Scholar]
- [6].Mizandari M, Pai M, Xi F, et al. Percutaneous intraductal radiofrequency ablation is a safe treatment for malignant biliary obstruction: feasibility and early results. Cardiovasc Intervent Radiol 2013;36:814–9. [DOI] [PubMed] [Google Scholar]
- [7].Rustagi T, Jamidar PA. Intraductal radiofrequency ablation for management of malignant biliary obstruction. Dig Dis Sci 2014;59:2635–41. [DOI] [PubMed] [Google Scholar]
- [8].Mukund A, Arora A, Rajesh S, et al. Endobiliary radiofrequency ablation for reopening of occluded biliary stents: a promising technique. J Vasc Interv Radiol 2013;24:142–4. [DOI] [PubMed] [Google Scholar]
- [9].Wadsworth CA, Westaby D, Khan SA. Endoscopic radiofrequency ablation for cholangiocarcinoma. Curr Opin Gastroenterol 2013;29:305–11. [DOI] [PubMed] [Google Scholar]
- [10].Yang LC, Shi HY, Huang JW, et al. Biliary stenting for unresectable cholangiocarcinoma: a population-based study of long-term outcomes and hospital costs in Taiwan. Kaohsiung J Med Sci 2015;31:370–6. [DOI] [PubMed] [Google Scholar]
- [11].Steel AW, Postgate AJ, Khorsandi S, et al. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc 2011;73:149–53. [DOI] [PubMed] [Google Scholar]
- [12].Figueroa-Barojas P, Bakhru MR, Habib NA, et al. Safety and efficacy of radiofrequency ablation in the management of unresectable bile duct and pancreatic cancer: a novel palliation technique. J Oncol 2013;2013:910897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Fu Y, Yang W, Wu JY, et al. Intrahepatic biliary injuries associated with radiofrequency ablation of hepatic malignancies. Chin Med J 2011;124:1957–63. [PubMed] [Google Scholar]
- [14].Tiong L, Maddern GJ. Systematic review and meta-analysis of survival and disease recurrence after radiofrequency ablation for hepatocellular carcinoma. Brit J Surg 2011;98:1210–24. [DOI] [PubMed] [Google Scholar]
- [15].Itoi T, Yasuda I, Doi S, et al. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy 2011;43:369–72. [DOI] [PubMed] [Google Scholar]
- [16].Zacharoulis D, Lazoura O, Sioka E, et al. Habib EndoHPB: a novel endobiliary radiofrequency ablation device. An experimental study. J Invest Sur 2013;26:6–10. [DOI] [PubMed] [Google Scholar]


