Abstract
Background:
Choroidal detachment (CD) is often observed at an early period particularly after trabeculectomy and glaucoma drainage implant surgery. However, topical antiglaucoma eye drop-induced CD is a rare complication. Here, we report a case of topical bimatoprost-induced late-onset CD after trabeculectomy and review the literature.
Case report:
A 74-year-old man who suffered from primary open-angle glaucoma underwent his initial trabeculectomy with mitomycin-C in the right eye. Before the surgery, his intraocular pressure (IOP) was 20 to 22 mm Hg with bimatoprost 0.03%, dorzolamide 1%, and brimonidine 0.1% and his best corrected visual acuity (BCVA) was 0.9. The mean deviation in Humphrey Visual Field Analyzer (24–2 program) was −27.83 db. After successful trabeculectomy, IOPs were 11 to 16 mm Hg without any medication. Eight months after the surgery, we restarted bimatoprost to further reduce the IOP in the right eye, which was 15 mm Hg. At a hospital visit 2 months later, he complained of blurred vision that had persisted for the past 1 month; his IOP had decreased to 9 mm Hg. His BCVA was 0.04 and 3 quadrant CD was found. We discontinued bimatoprost and started him on betamethasone 0.1% 4 times per day. However, CD marginally changed after 1 week, with IOP at 7 mm Hg; thus, we performed scleral drainage for CD. After 3 weeks of drainage, CD completely disappeared. IOP increased to 16 mm Hg and BCVA was 0.7. However, 3 months after the drainage, IOP increased to 29 mm Hg, and needling revision was thus performed. After the surgery, IOP remained at 14 to 16 mm Hg without any glaucoma medication and CD recurrence. A review of the literature showed that various antiglaucoma medications induce CD, regardless of the preceding glaucoma surgery and that CD is usually resolved by withdrawing the medication and administering topical steroids. However, most previous studies have shown the recurrence of CD by rechallenging the same drug.
Conclusion:
In our case, topical bimatoprost induced late-onset CD after trabeculectomy. Early scleral drainage may be a good option to quickly resolve drug-induced CD and prevent its recurrence. Therefore, it must be kept in mind that various antiglaucoma medications induce CD.
Keywords: bimatoprost, choroidal detachment, glaucoma, late onset, trabeculectomy
1. Introduction
Choroidal detachment (CD) is often observed soon after trabeculectomy and glaucoma drainage implant surgery. The occurrence rate was reported as 11% to 19%[1,2] in trabeculectomy and 16%[2] in Baerveldt glaucoma implant. Late-onset CD is a rare complication in clinical settings; however, a case of late-onset spontaneous CD after trabeculectomy was previously reported.[3] Meanwhile, antiglaucoma eye drops itself cause CD with or without previous surgery.[4–14] However, the cause or treatment are yet to be established. If restarting the same medication reinduces CD, glaucoma treatment option will become limited. The present report describes late-onset CD after trabeculectomy with topical bimatoprost administration in a patient who experienced the usefulness of scleral drainage in immediately reducing CD and reviews the literature for exploring the mechanism and treatment for CD induced by antiglaucoma medications.
2. Case report
A 74-year-old man with primary open-angle glaucoma was referred to our hospital because of glaucoma visual field progression. His intraocular pressure (IOP) was 20 to 22 mm Hg with bimatoprost 0.03%, dorzolamide 1%, and brimonidine 0.1%. His best corrected visual acuity (BCVA) was 0.9 in the right eye and 1.0 in the left eye. The mean deviation in the Humphrey Visual Field Analyzer (Carl Zeiss Meditec Inc., Dublin, CA) (24–2, SITA fast program) was −27.83 db in the right and −4.28 db in the left. Therefore, we performed trabeculectomy with mitomycin-C in the right eye. The surgical procedure is well-known and was performed at a temporal superior fornix conjunctival flap using mitomycin-C 0.04% for 4 minutes. After the successful trabeculectomy, IOP changed from 11 to 16 mm Hg for 8 months without any medication in the right eye. However, his glaucoma visual field defect was severe; therefore, we restarted bimatoprost in the right eye to further reduce IOP. After 2 months of restarting bimatoprost, he returned to our clinic for a routine examination. However, he complained of severe blurred vision in the right eye since a month. Slit lamp examination showed flat bleb formation at the temporal superior aspect of the right eye, with mild conjunctival hyperemia. The anterior chamber depth was normal and no inflammation was observed. However, mild Descemet membrane folds were observed in the cornea (Fig. 1). His BCVA in the right eye was 0.04 and IOP was 9 mm Hg. Fundus photography showed severe CD in 3 quadrants, especially in the temporal superior quadrant (Fig. 2A). No retinal detachment was observed. We suspected the cause of CD to be bimatoprost and, therefore, discontinued it. Additionally, betamethasone 0.1% 4 times per day was started in the right eye.
Figure 1.
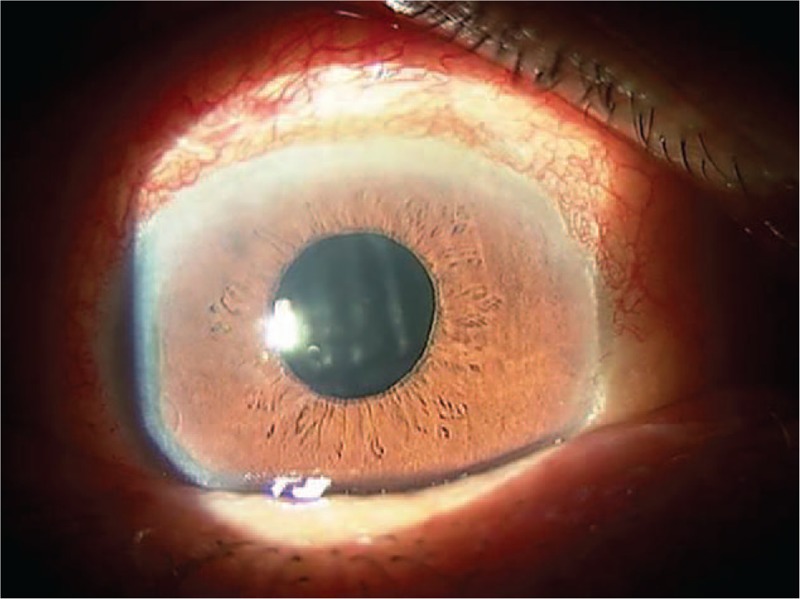
Ocular surface of the patient with CD at the first visit. The anterior chamber depth was normal and no inflammation was observed, but mild Descemet membrane folds and mild conjunctival hyperemia were observed. CD = choroidal detachment.
Figure 2.
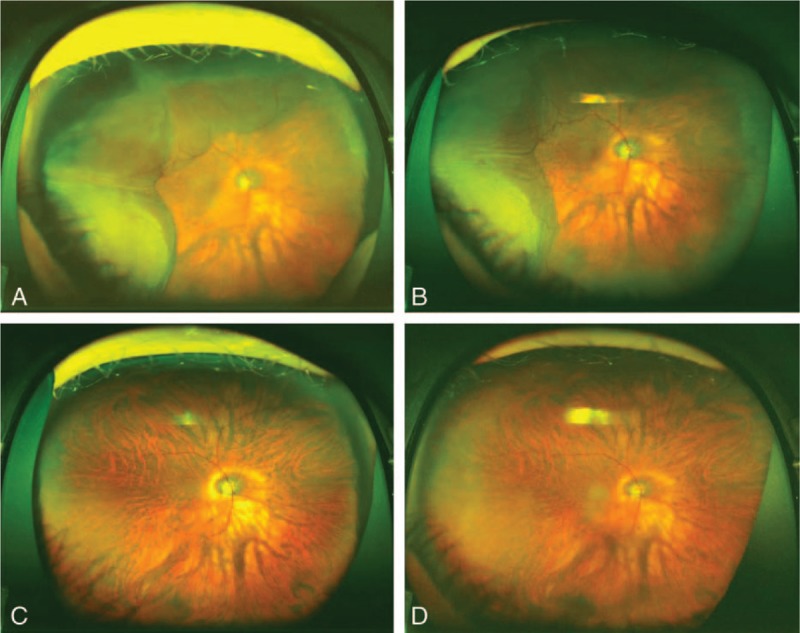
Time course of CD followed by retinal photographs obtained using Optos 200Tx (Optos PLC, Dunfermline, United Kingdom). (A) Three quadrants of CD were found after 2 months of topical bimatoprost. Patient's IOP was 9 mm Hg and BCVA was 0.04. (B) One week after discontinuing bimatoprost. CD was slightly decreased; however, IOP decreased to 7 mm Hg. The scleral drainage was performed after this. (C) Three weeks after the scleral drainage, CD completely disappeared. Patient's IOP increased to 16 mm Hg and BCVA recovered to 0.7. (D) Six months after needling revision, we did not find CD in the right eye, which had an IOP of 15 mm Hg. BCVA = best corrected visual acuity, CD = choroidal detachment, IOP = intraocular pressure.
After 1 week, CD slightly decreased but not with an IOP of 7 mm Hg (Fig. 2B). Therefore, we performed scleral drainage for CD at the temporal superior site. Three weeks after drainage, CD completely disappeared (Fig. 2C). His IOP increased to 16 mm Hg and BCVA was 0.7. Three months after drainage, his IOP increased to 29 mm Hg due to bleb failure; hence, we performed bleb needle revision with mitomycin-C 0.1 mL conjunctival injection. After the surgery, his IOP remained at 14 to 16 mm Hg without recurrence of CD for 6 months (Fig. 2D). At the last visit, his IOP in the right eye was 15 mm Hg and BCVA was 0.9. This case report was approved by the Research Ethics Committee of Saneikai Tsukazaki Hospital (Himeji, Japan).
3. Discussion
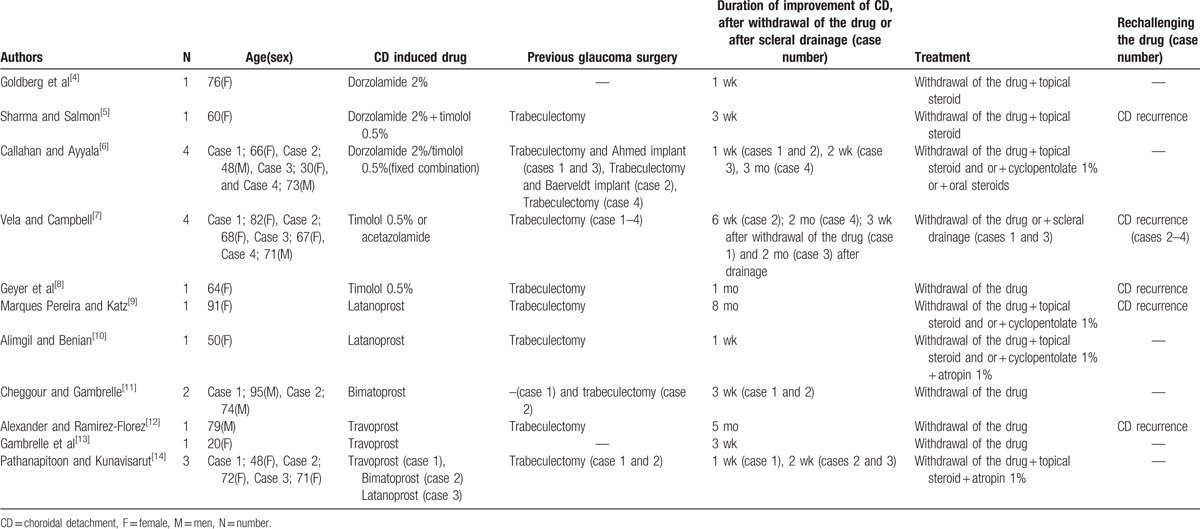
We report the case of a patient who developed late-onset CD induced by topical bimatoprost, wherein early scleral drainage was a good option to prevent CD recurrence. Previous studies[4–14] showed that topical antiglaucoma eye drops induce CD with or without previous glaucoma surgery. Drug-induced CDs were usually resolved by withdrawing the medication and administering topical steroids, sometimes with cyclopentolate or atropin (Table 1).
Table 1.
A review of the literature on drug-induced CDs.
CD induced by antiglaucoma eye drops is considered to occur because of 2 mechanisms: suppression of aqueous humor production (timolol, dorzolamide, and acetazolamide) and increased uveoscleral outflow (prostaglandin analogues such as latanoprost, bimatoprost, and travoprost) (Table). The mechanism of CD induced by the aqueous humor suppression group was suggested in detail by Vela.[7] The ciliary body is first damaged and/or sensitized by the long-term suppression of aqueous humor or filtering surgery. After retreatment with the drug, the sensitized ciliary body responds with a dramatic reduction in aqueous production causing hypotony.[7] On the other hand, the mechanism underlying CD induced by the increasing uveoscleral outflow group was the increase in the uveoscleral outflow of the aqueous humor via a reduction in the levels of collagen types I, III, and IV in the ciliary smooth muscles and adjacent sclera.[15] This hypothesis was also supported by Martínez-Belló et al,[16] who showed that 4 of 28 eyes with trabeculectomy showed persistent supraciliochoroidal effusion observed with ultrasound biomicroscopy for 6 months after trabeculectomy without CD. They suggested that observed supraciliochoroidal effusion may be produced by increased uveoscleral outflow resulting from iatrogenic cyclodialysis due to trabeculectomy technique with scleral spur excision, which removes the barrier between the anterior chamber and the suprachoroidal space.[16] We might excise the scleral spur in this case and topical bimatoprost further increased uveoscleral outflow, leading to CD.
Additionally, mitomycin-C use in trabeculectomy may have direct toxicity on the ciliary epithelium, thus resulting in aqueous hyposecretion.[17] Previous studies experienced the recurrence of CD by rechallenging the same drug.[5,7–9,11] Only Vela and Campbell[7] tried to resolve CD by scleral drainage in 2 of their patients, and 1 of the 2 cases during rechallenging timolol therapy did not develop CD. Interestingly, in 3 of 4 cases, the carbonic anhydrase inhibitors such as dorzolamide and acetazolamide did not induce CD but timolol induced CD,[7] despite the fact that timolol, dorzolamide, and acetazolamide have the same IOP reduction mechanism for suppressing aqueous humor production.
Time taken for CD resolution was observed to be 1 to 3 weeks,[4–6,10,11,13,14] but some studies have reported 5[12] and 8 months.[9] A long residual CD has the possibility to cause visual field defect or decreased visual acuity. In our case, the patient already had severe glaucoma visual field damage (mean deviation: −27.83 db). Therefore, we tried scleral drainage only for 1 week after discontinuing bimatoprost. As a result, the patient's visual acuity relatively recovered from 0.04 to 0.7 after 3 weeks of scleral drainage. Furthermore, the patient did not experience recurrence of CD after the bleb needling surgery.
4. Conclusion
We report a case of late-onset CD induced by topical bimatoprost after trabeculectomy. Early scleral drainage can be a good option to quickly resolve drug-induced CD and prevent its recurrence. Therefore, it should be kept in mind that various antiglaucoma medications induce CD.
Footnotes
Abbreviations: BCVA = best corrected visual acuity, CD = choroidal detachment, IOP = intraocular pressure.
The authors have no financial or proprietary interest in any product, method, or material described herein.
The authors have no financial disclosures and no conflicts of interest to declare.
References
- [1].Jampel HD, Musch DC, Gillespie BW, et al. Collaborative Initial Glaucoma Treatment Study Group. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol 2005;140:16–22. [DOI] [PubMed] [Google Scholar]
- [2].Gedde SJ, Herndon LW, Brandt JD, et al. Surgical complications in the tube versus trabeculectomy study during the first year of follow-up. Am J Ophthalmol 2007;143:23–31. [DOI] [PubMed] [Google Scholar]
- [3].Burney EN, Quigley HA, Robin AL. Hypotony and choroidal detachment as late complications of trabeculectomy. Am J Ophthalmol 1987;103:685–8. [DOI] [PubMed] [Google Scholar]
- [4].Goldberg S, Gallily R, Bishara S, et al. Dorzolamide-induced choroidal detachment in a surgically untreated eye. Am J Ophthalmol 2004;138:285–6. [DOI] [PubMed] [Google Scholar]
- [5].Sharma T, Salmon JF. Hypotony and choroidal detachment as a complication of topical combined timolol and dorzolamide. J Ocul Pharmacol Ther 2007;23:202–5. [DOI] [PubMed] [Google Scholar]
- [6].Callahan C, Ayyala RS. Hypotony and choroidal effusion induced by topical timolol and dorzolamide in patients with previous glaucoma drainage device implantation. Ophthalmic Surg Lasers Imaging 2003;34:467–9. [PubMed] [Google Scholar]
- [7].Vela MA, Campbell DG. Hypotony and ciliochoroidal detachment following pharmacologic aqueous suppressant therapy in previously filtered patients. Ophthalmology 1985;92:50–7. [DOI] [PubMed] [Google Scholar]
- [8].Geyer O, Neudorfer M, Lazar M. Recurrent choroidal detachment following timolol therapy in previously filtered eye. Choroidal detachment post filtering surgery. Acta Ophthalmol (Copenh) 1992;70:702–3. [DOI] [PubMed] [Google Scholar]
- [9].Marques Pereira ML, Katz LJ. Choroidal detachment after the use of topical latanoprost. Am J Ophthalmol 2001;132:928–9. [DOI] [PubMed] [Google Scholar]
- [10].Alimgil ML, Benian O. Choroidal effusion and shallowing of the anterior chamber after adjunctive therapy with latanoprost in a trabeculectomized patient with angle closure glaucoma. Int Ophthalmol 2001;24:129–31. [DOI] [PubMed] [Google Scholar]
- [11].Cheggour M, Gambrelle J. Massive choroidal detachment secondary to topical use of bimatoprost: Report of two cases. J Fr Ophtalmol 2012;35:176–80. [DOI] [PubMed] [Google Scholar]
- [12].Alexander P, Ramirez-Florez S. Hypotony and choroidal detachment as a complication of travoprost after trabeculectomy surgery. Eye (Lond) 2008;22:736–7. [DOI] [PubMed] [Google Scholar]
- [13].Gambrelle J, Denis P, Kocaba V, et al. Uveal effusion induced by topical travoprost in a patient with Sturge-Weber-Krabbe syndrome. J Fr Ophtalmol 2008;31:e19. [PubMed] [Google Scholar]
- [14].Pathanapitoon K, Kunavisarut P. Choroidal detachment after topical prostaglandin analogs: case report. J Med Assoc Thai 2005;88:1134–6. [PubMed] [Google Scholar]
- [15].Sagara T, Gaton DD, Lindsey JD, et al. Topical prostaglandin F2alpha treatment reduces collagen types I, III, and IV in the monkey uveoscleral outflow pathway. Arch Ophthalmol 1999;117:794–880. [DOI] [PubMed] [Google Scholar]
- [16].Martínez-Belló C, Capeáns C, Sánchez-Salorio M. Ultrasound biomicroscopy in the diagnosis of supraciliochoroidal fluid after trabeculectomy. Am J Ophthalmol 1999;128:372–5. [DOI] [PubMed] [Google Scholar]
- [17].Mietz H. The toxicology of mitomycin C on the ciliary body. Curr Opin Ophthalmol 1996;7:72–9. [DOI] [PubMed] [Google Scholar]


