Abstract
Rationale:
Thalamic pain is a distressing and treatment-resistant type of central post-stroke pain. Although stellate ganglion block is an established intervention used in pain management, its use in the treatment of thalamic pain has never been reported.
Patient concerns:
A 66-year-old woman presented with a 3-year history of severe intermittent lancinating pain on the right side of the face and the right hand. The pain started from the ulnar side of the right forearm after a mild ischemic stroke in bilateral basal ganglia and left thalamus. Weeks later, the pain extended to the dorsum of the finger tips and the whole palmar surface, becoming more severe. Meanwhile, there was also pain with similar characteristics emerging on her right face, resembling atypical trigeminal neuralgia.
Diagnoses:
Thalamic pain was diagnosed.
Interventions:
After refusing the further invasive treatment, she was suggested to try stellate ganglion block.
Outcomes:
After a 3-day period of pain free (numerical rating scale: 0) postoperatively, she reported moderate to good pain relief with a numerical rating scale of about 3 to 4 lasting 1 month after the first injection. Pain as well as the quality of life was markedly improved with less dose of analgesic agents.
Lessons:
Stellate ganglion block may be an optional treatment for thalamic pain.
Keywords: central post-stroke pain, pain management, stellate ganglion block, thalamic pain, thalamic stroke
1. Introduction
Thalamic pain, first described by Dejerine and Roussy in 1906,[1] is a distressing and treatment-resistant type of central post-stroke pain that may develop after thalamic stroke. Pharmacological treatment including antidepressants, anticonvulsants, and opioids had been used to control the pain. However, the treatment response is mostly moderate and the dosage is limited by side-effects. After failure of a combination of several drugs, neurosurgical approaches such as motor cortex stimulation and deep brain stimulation would be further adapted. However, these treatment modalities are of high-cost but without definite effectiveness.[2] Patients with thalamic pain are suffering from severely impaired quality of life as well as heavy economic burden. We present a case of multidrug-resistant thalamic pain successfully alleviated by stellate ganglion block, which is an established technique in pain management for a variety of conditions.[3]
2. Case Presentation
A 66-year-old woman presented with a 3-year history of severe intermittent lancinating pain on the right side of the face and the right hand. The pain started from the ulnar side of the right forearm after a mild ischemic stroke in bilateral basal ganglia and left thalamus. Weeks later, the pain extended to the dorsum of the finger tips and the whole palmar surface, becoming more severe. Meanwhile, there was also pain with similar characteristics emerging on her right face, resembling atypical trigeminal neuralgia. She was diagnosed with thalamic pain at another hospital and was treated with medication. By the time she came to our outpatient clinic, she had been on multiple oral analgesic agents treatment, including amitriptyline (50 mg, T.I.D.), pregabalin (50 mg T.I.D.), and gabapentin (0.3 g P.R.N.) for almost 2 years. However, the pain was not well controlled by then since the effect of the drugs had waned and there were some adverse effects such as nausea and tiredness. The distribution of pain remained in the same areas, and the intensity of pain, which was evaluated by the numerical rating scale, ranged from 7 to 10. The pain was occasionally aggravated by agitation. Both warm and cold perception of right hand and face were impaired. Neither other sensory abnormalities such as mechanical hyperalgesia or allodynia nor motor deficit was noted during the neurological examination. The Brief Pain Inventory (BPI) [4] showed general activity, normal work, and sleep were seriously affected. Anxiety and depression were suspicious with the score of 10 in Hospital Anxiety and Depression Scale (HADS)[8] (Table 1). Recent brain MRI demonstrated an old infarction focus in the left thalamus (Fig. 1). Her previous medical history included 18-year hypertension that was controlled on regular treatment and 17-year diabetes that was managed by insulin injection. After communicating with the patient and her family, invasive treatments such as motor cortex stimulation and deep brain stimulation were refused because of the economic factors. We eventually decided to perform stellate ganglion block after obtaining a written consent.
Table 1.
Preoperative and 11 months postoperative HADS and BPI scores.
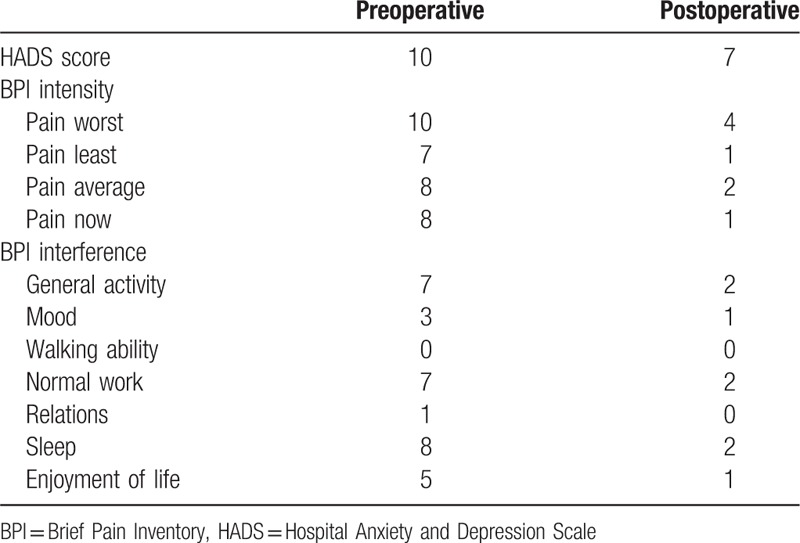
Figure 1.
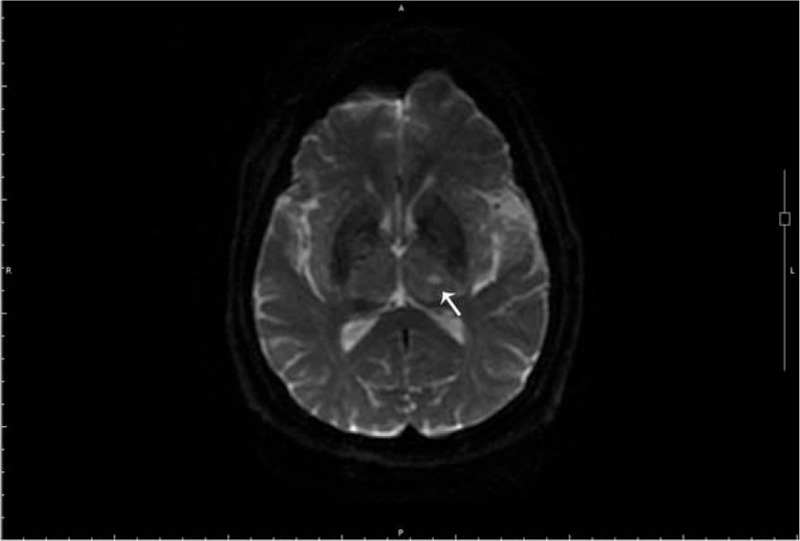
Brain MRI-DWI shows an old infarction focus in the left thalamus (white arrow). MRI-DWI = magnetic resonance image diffusion weighted imaging.
After a 3-day period of pain free (numerical rating scale: 0) postoperatively, she reported moderate to good pain relief with a numerical rating scale of about 3 to 4 lasting 1 month after the first injection. Similar injections were repeated twice (1 and 3 months later, respectively) and there was an increase in the duration of almost pain-free (numerical rating scale: 0–2) period lasting over half a year. Presently, she continues to take amitriptyline (50 mg Q.D.) and takes other analgesic agents on an occasional basis instead of regular use. The pain as well as the quality of life has been marked improved according to the results of reassessment of the BPI and HADS after 11 months. (Table 1)
3. Discussion
As one type of central post-stroke pain, thalamic pain is both a clinical challenge and a scientific mystery.[5] The pain is often intolerable and uncontrollable, and the underlying mechanisms remain unclear. The thalamus is a key relay station for the transmission of nociceptive information to the cerebral cortex. However, thalamus stroke is not always associated with pain development, and variables such as patient age, sex, and laterality of thalamic lesion have no predictive value.[2] Paralleled to the elusive pathological mechanisms, effects of the multiple available treatments were limit. Currently, no evidence-based therapeutic algorithm for thalamic pain has been proposed and the treatment modalities are still in exploration.
Stellate ganglion block is a selective sympathetic block that affects ipsilateral head, neck, upper extremity, and the upper part of the thorax. Its indications are wide, ranging from Raynaud disease, hot flashes to a series of pain conditions such as complex regional pain syndrome, atypical facial pain, and upper extremity pain.[7] Although the mechanisms underlying the effect of stellate ganglion block on various pathologies is not completely understood, it is conceivable and plausible that wide indication implies wide ranges of mechanisms as sympathetic nervous system is interconnected throughout the whole body.
Our report demonstrates that patient with thalamic pain could benefit from stellate ganglion block. With less medication administrated, the pain scores had been decreased and the quality of life had been improved. According to our knowledge, application of stellate ganglion block on thalamic pain has never been reported. It is worth noting that in this patient, the pain symptom could be occasionally aggravated by agitation, which may be associated with the activation of sympathetic nervous system. Although the relationship among the pain, psychological factors, and autonomic nerve system remains unclear, the sympathetic-related brain regions dominating both sensory and psychological activities had been identified in a previous research,[6] which may also provide an explanation for modulating the contralateral thalamic (central) pathway by ipsilateral sympathetic block. Therefore, it could be inferred that this intriguing feature may be responsible for the efficacy of stellate ganglion block. In that light, this case presented may provide a clinical clue to exploring a sensory-emotional-autonomic network involved in the nervous system.
4. Conclusions
Although the mechanisms of this effect are not clear, stellate ganglion block may be an optional treatment for thalamic pain, especially when the pain is associated with autonomic alteration such as emotional changes. Further studies are needed to define its potential role in the treatment of thalamic pain.
Footnotes
Abbreviations: BPI = Brief Pain Inventory, HADS = Hospital Anxiety and Depression Scale.
The authors report no conflicts of interest.
The study was approved by Xinhua Hospital Medical Ethics committee. The patient had consented to submission of this case report to the journal.
References
- [1].Dejerine J, Roussy G. Le syndrome thalamique. Rev Neurol (Paris) 1906;14:521–32. [Google Scholar]
- [2].Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet Neurol 2009;8:857–68. [DOI] [PubMed] [Google Scholar]
- [3].Kumar N, Thapa D, Gombar S, et al. Analgesic efficacy of pre-operative stellate ganglion block on postoperative pain relief: a randomised controlled trial. Anaesthesia 2014;69: 954-660. [DOI] [PubMed] [Google Scholar]
- [4].Tan G, Jensen MP, Thornby JI, et al. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 2004;5:133–7. [DOI] [PubMed] [Google Scholar]
- [5].Vartiainen N, Perchet C, Magnin M, et al. Thalamic pain: anatomical and physiological indices of prediction. Brain 2016;139(pt 3):708–22. [DOI] [PubMed] [Google Scholar]
- [6].Westerhaus MJ, Loewy AD. Central representation of the sympathetic nervous system in the cerebral cortex. Brain Res 2001;903:117–27. [DOI] [PubMed] [Google Scholar]
- [7].Woo A, Tharakan L, Vargulescu R. Stellate ganglion block for painful congenital venous malformation of the arm. Pain Pract 2015;15:E65–8. [DOI] [PubMed] [Google Scholar]
- [8].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]


