Abstract
Reconstruction of the ruptured anterior cruciate ligament (ACL) does not always result in expected successful outcome. A satisfactory outcome depends not only on the tightness or strength of the graft but also on the quality of proprioceptive restoration. Mechanoreceptors of ACL are supposed to play considerable roles in the proprioceptive feedback system of knee. This study aimed to observe the condition and number of the surviving mechanoreceptors in the tibial remnant of ruptured ACL in human knees.
From April 2009 to January 2012, 60 patients with existing free tibial remnants who had undergone arthroscopic ACL reconstruction were enrolled and divided into 4 groups according to the time duration of injury to surgery (Group I: no more than 3 months; Group II: 3 to 6 months; Group III, 6 months to 1 year; Group IV: more than 1 year). Six normal ACL specimens were taken as controls. Specimens were obtained from ACL tibial remnant and stained by the immunohistochemical staining method. The type, size, and quantity of mechanoreceptors were observed under the light microscope. A total of 92 Ruffini-like corpuscles, 9 Pacini-like corpuscles, 5 unclassified neural endings, and free nerve endings were identified via immunohistochemical staining.
There were no significant differences in the number of mechanoreceptors in the 5 groups (P = 0.238). Some degenerative changes were observed in Group IV. The results suggest that the residual mechanoreceptors in the ruptured ACL exhibit long-term survival and showed no obvious signs of withering within 1 year.
Residual mechanoreceptors do exist in the tibial remnants of ruptured anterior cruciate ligament in human knees and identified clearly by using immunohistochemistry staining. No significant difference was found regarding quantitative variation of the residual mechanoreceptors about the injury duration.
Keywords: anterior cruciate ligament, mechanoreceptors, tibial remnants
1. Introduction
Anterior cruciate ligament (ACL) is considered as the passive static stabilizers of the joints against anterior tibial translation. The rupture of ACL contributes to the progressive functional instability and disability.[1] Since the ACL does not heal after rupture, reconstructive surgery is currently widely performed by using tendon autografts and allografts. Despite the restoration of mechanical stability after ACL reconstruction, some patients appear to poor joint position sense and proprioception function.[2,3] Therefore, successful outcome after ligament reconstruction may depend not only on the tightness or strength of the graft, but also on the quality of proprioceptive restoration.[4,5]
Since Schultz et al[6] first reported the existence of mechanoreceptors in human ACL, some related morphological studies have demonstrated a rich nerve supply and various types of sensory receptors in the ligament.[7–9] Freeman and Wyke[10] classified them into 4 types, including Ruffini ending, Pacinian corpuscle, Golgi tendon organ-like structure, and free nerve ending. Though the function and operational method of these intra-articular receptors have not been clearly confirmed, they were thought to contribute to the proprioception by detecting changes in tension, acceleration, direction of movement, and position of the knee joint.[11,12]
Many patients still have identifiable tissue remaining at the tibial insertion area after the ACL completely or partially ruptured, because most ACL tears occur at the femoral attachment.[13] Georgoulis et al[9] suggested that the presence of nerual mechanoreceptors in the tibial remnant as a possible source of reinnervation of the ACL autograft. Retention of the normal mechanoreceptors during reconstruction operation may accelerate the process of graft reinnervation and improve the recovery process.
If the ACL remnant could provide a source for graft reinnervation or preserve proprioceptive function to some extent, some closely related conditions should also be noticed, including the long existence of mechanoreceptors and proprioceptive nerve fibers in the ACL remnant, the reinnervation between sensory nerve endings and central system, and the regeneration of mechanoreceptors occurring in the remnant. However, the survival condition and functional condition of residual mechanoreceptors are still unclear. In the current study, a morphologic and quantitative evaluation of mechanoreceptors in the tibial remnants of complete-torn human ACL was performed by using group comparison according to the time from injury to surgery. This study aimed to observe the survival condition and the quantitative variation of mechanoreceptors in the tibial remnant of the ruptured ACL in human knees.
2. Methods
2.1. General data
This study was carried out at the Department of Arthroscopic Surgery, Shanghai Sixth People's Hospital, Shanghai, China, in collaboration with 2 junior and 1 senior pathologists from April 2009 to January 2012. The Ethics Committee of the Sixth People's Hospital Affiliated to Shanghai Jiao Tong University approved this study. Due to the number of mechanoreceptors may be affected by different types of remnant,[8,9] 60 patients (51 men, 9 women; age range 16–53 years) who were found having free tibial remnant, instead of remnant adhering to the posterior cruciate ligament (PCL) or femoral notch during arthroscopic ACL reconstruction were included in this study. Before the operation, written informed consent was obtained from each patient to remove the tibial remnant of ruptured ACL. The patients were divided into 4 groups according to the time from injury to surgery. Each group included 15 cases. The time duration between injury and surgery was no more than 3 months, 3 to 6 months, 6 months to 1 year, and more than 1 year, respectively, in Group I, II, III, and IV. As control, 6 normal ACL specimens were taken from healthy knee amputated at thigh level due to trauma. Exclusion criteria included previous knee surgery, history of other significant knee injury, and presence of associated PCL or collateral ligament injury.
2.2. Immunohistochemistry staining
During the ACL reconstruction, a piece of specimen about 5 mm wide, 7 mm long, and 5 mm in subsynovial depth was removed from the anteromedial side of the ACL tibial remnant, where the majority of receptors were proved to be located at with arthroscopic scissors and nuclei punch (Fig. 1).[14] The size of the specimen was kept constant by reference to the hook length of the arthroscopic probe. The unified standard was set for sampling. Specimens were fixed for 24 hours in 4% paraformaldeyde in phosphate buffer 0.1 M (pH 7.2) at 4°C, rinsed in phosphate buffer saline for 1 hour (PBS: 0.15 M NaCl in 0.01 M sodium phosphate buffer, pH 7.2), and then stored at 4°C in PBS containing 30% sucrose overnight. Then, they were successively mounted in OCT embedding medium and quickly frozen with liquid nitrogen for the later preparation of frozen sections. Series of 20 μm thick sections were cut with a cryostat and mounted on gelatin-coated glass slides. Each specimen was sectioned for 40 slices. They were dried and processed for immunohistochemistry staining. After blocking endogenous peroxidase activity (with 3% hydrogen peroxide), sections were incubated overnight at 4°C in a humid chamber to stain for demonstration of Anti-p75 Neurotrophin Receptor (p75, code 07–476, Millipore), Protein Gene Product (PGP 9.5, code AB5925, Millipore), or S-100 protein (S-100, code 18–0046, Invitrogen) immunoreactivity (IR) using PicTure 2-step method (Zymed). Each step was practiced according to the manual. DAB was used for chromogen. All of these primary antibodies have been used in several studies on mechanoreceptors previously with satisfying staining results. All serial sections were observed and evaluated by 2 junior pathologists under a light microscope (Leica DM4000) and then interpreted by a senior pathologist. The mechanoreceptors were morphologically classified by using Freeman and Wyke's criteria.[10] However, in this study the free nerve endings and other unclassified neural endings were not included since they function as the actual pain receptor and may interfere with the results.
Figure 1.
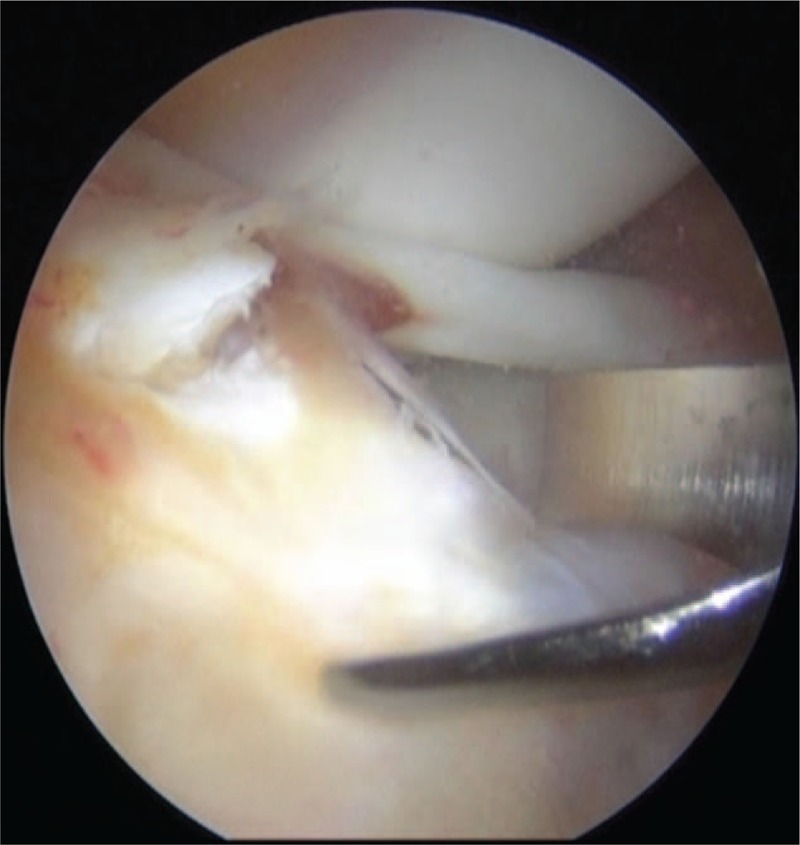
The specimen was removed from the anteromedial side of the ACL tibial remnant, with arthroscopic scissors and nuclei punch. ACL = anterior cruciate ligament.
2.3. Statistical analysis
Differences in the number of mechanoreceptors in each group were tested for statistical significance using the Kruskal–Wallis test. The Mann–Whitney U test was used to verify the statistical significance of differences in normal control group and Group IV. P-values < 0.05 were considered significant. Data analysis was done using SPSS for Windows version 17.0 (SPSS, Inc.).
3. Results
In total, 66 specimens (2640 slices) were examined. According to the Freeman and Wyke's criteria, besides 2 types of mechanoreceptors (92 Ruffini-like corpuscles, 9 Pacini-like corpuscles), 5 unclassified neural endings and free nerve endings were also observed under light microscopy (Fig. 2). No distinct Golgi organ-like corpuscles was identified.
Figure 2.
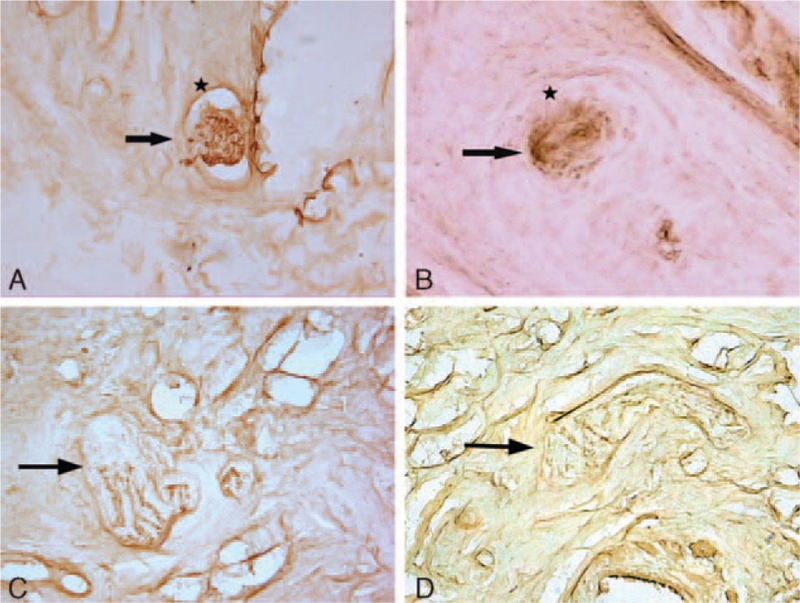
Histological appearance of Ruffini-like corpuscle (A), Pacini-like corpuscle (B), and unclassified neural ending (C and D). Ruffini-like endings are thinly encapsulated; terminal branches that coil and arborize within the corpuscles are displayed after staining for S-100. Pacini-like corpuscle contains a central axon (arrow) and a lamellated capsule, stained for p75. Unclassified neural endings are visualized by staining for PGP 9.5. Magnification,×100.
Ruffini-like endings are thinly encapsulated. Globular corpuscles were measured approximately 50–150 μm. The parent axon broke up into smaller terminal branches with coil and arborize in the corpuscles (Fig. 2A). In this study, the dendritic intracapsular nerve fascicle was demonstrated via staining for all 3 kinds of antibodies (p75, PGP 9.5 and S-100) (Fig. 3). Especially, they were clearly visualized by showing specific IR after staining for PGP 9.5 and S-100. They were the most primary mechanoreceptors identified in the ACL remnant in this study.
Figure 3.
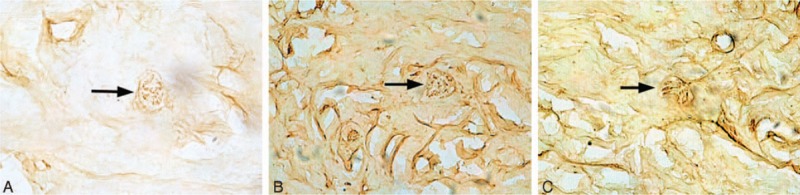
Ruffini-like corpuscles in the tibial remnants of the ruptured anterior cruciate ligament in human knees, stained for p75 (A), PGP 9.5 (B), and S-100 (C). Magnification,×100.
Pacini-like corpuscle exhibited a cylindrical structure in which a central axon was surrounded by an inner core with a thick, lamellated capsule showing intense p75 IR (Fig. 2B). The number of these corpuscles was obliviously less than that of Ruffini-like endings. Moreover, it was noted that their structures resembled micro-blood vessels and were apt to be interfered by the nonspecific staining during observation. Therefore, analysis of serial sections appears to be useful and essential for identifying mechanoreceptors.
Five morphologically unclassified neural endings could neither be clearly defined as Ruffini-like nor Pacini-like corpuscles. They exhibited variable features, including large size of approximately 150–400 μm, irregular shape, encapsulated, and unencapsulated varieties (Fig. 2C and D).
Unmyelinated free nerve endings were considered to be nociceptors that respond to inflammatory and pain stimuli. It also serves a local effector function by releasing neuropeptides. They were not included because it is difficult to distinguish from other nerve bundles.
The number of mechanoreceptors in each group is presented in Table 1. Mechanoreceptors were observed in all 5 groups. There were 33 mechanoreceptors in Group I, 23 in Group II, 24 in Group III, 13 in Group IV, and 13 in the normal control group, respectively. The mean number of mechanoreceptors was 2.20 ± 2.51, 1.53 ± 1.88, 1.60 ± 1.76, 0.87 ± 1.41, and 2.17 ± 0.41, respectively. The median number of mechanoreceptors was 2, 1, 1, 0, and 2, respectively. According to the results, no statistically significant differences were found among the number of mechanoreceptors identified in the 5 groups (P = 0.238). However, the difference in the number of mechanoreptors between the normal control group and Group IV was significant (P = 0.011).
Table 1.
The numbers of mechanoreceptors for each group.
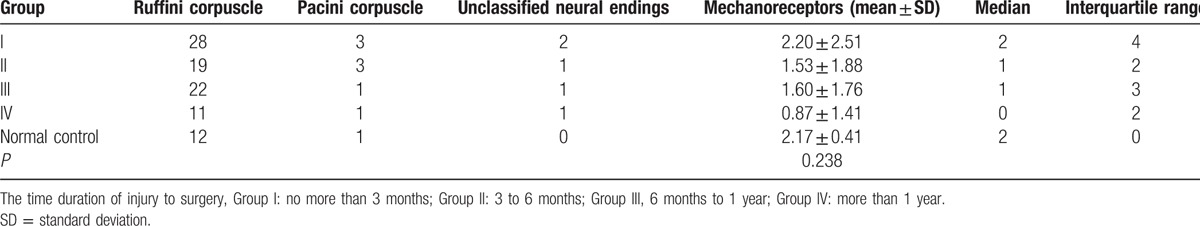
In morphological comparison, no obvious variation was observed regarding the size of the Ruffini-like endings among 5 groups. Some degenerative changes were observed in the specimens of Group IV (Fig. 4).
Figure 4.
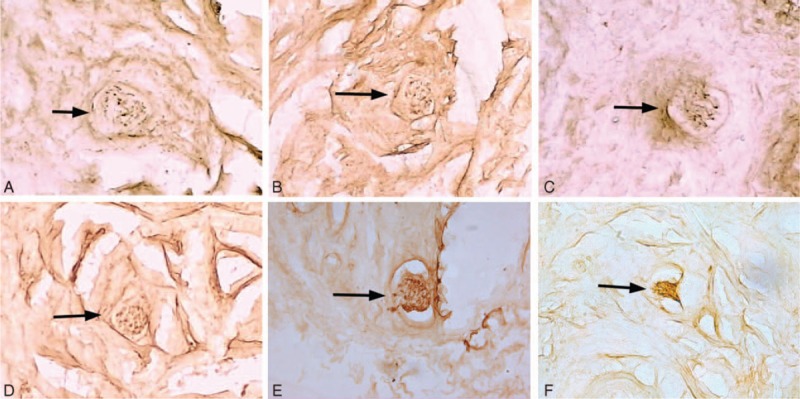
Ruffini-like endings identified in Group I (A), II (B), III (C), IV (D), normal control (E) and IV with degenerative and atrophic change (F), stained for S-100 (A, E, F), PGP 9.5 (B-D). Magnification,×100. (The time duration of injury to surgery, Group I: no more than 3 months; Group II: 3 to 6 months; Group III, 6 months to 1 year; Group IV: more than 1 year).
4. Discussion
Various mechanoreceptors in the ACL have been identified in animal and human experiments at present, they are supposed to play a considerable role in the proprioceptive feedback system of the knee.[14,15] Immunohistochemical techniques allow direct observation of the exact components of each mechanoreceptor including the capsule, the central axon, and the periaxonal cells, which have been proved much more sensitive for neural elements than conventional gold and silver chloride staining methods.[16] In the current study, an immunohistochemical method was utilized instead of conventional gold chloride method. Totally 92 Ruffini-like corpuscles, 9 Pacini-like corpuscles, 5 unclassified neural endings, and free nerve endings were identified in the specimens from the tibial remnant of the ruptured ACLs. The purpose of using 3 primary antibodies (p75, PGP 9.5, S-100) for IR is to find the best way to identify the mechanoreceptors in the human ACL. According to results during this experiment, it was indicated that Ruffini-like endings could be identified by IR with all 3 kinds of antibodies (p75, PGP 9.5 and S-100). However, the staining by PGP 9.5 and S-100 is much stronger, which is more capable to show structure of Ruffini-like endings, whereas the staining effect through p75 IR is better for the thick capsule of Pacini-like corpuscles. Golgi organ-like corpuscles could not be identified in this study. It is still controversial on the existence of Golgi organ-like corpuscles. Raunest et al[14] classified the Golgi organ-like corpuscle into a subtype of the Ruffini-type receptor. Schutte et al[17] considered Golgi corpuscle as a variant of Ruffini corpuscle. But in contrast to them, Lee et al[18] found many fusiform Golgi organ-like corpuscles in both the normal ACLs and the remnants by using neurofilament as the primary antibody. Thus, the detection method of Golgi organ-like corpuscle in the ACL remains to be improved and discussed.
A significant positive correlation was observed between the number of mechanoreceptors and the proprioceptive function of the knee joint.[11] When the ACL is ruptured, loss of innervation between mechanoreceptors and the posterior articular nerve (PAN) will occur, which may result in the functional instability of the knee.[19] Till now, no related study exactly showed the condition and number of the surviving mechanoreceptors in the tibial remnant of ruptured ACL in human knees.
This study investigated the quantitative variation of mechanoreceptors in the tibial remnants by means of group comparison and relatively larger sample size. The result has demonstrated that no statistically significant differences were found among 5 groups. It possibly means that no significant decrease or disappearing of the mechanoreceptors in the remnant could be observed instantly after the ACL ruptured. The main structural features of the residual mechanoreceptors can still be preserved for a long period. The injury duration-related changes in the morphological properties of the mechanoreceptors were also examined. No obvious variation was observed regarding the size of the Ruffini-like endings among 5 groups, but some degenerative changes could be observed in the specimens of patients who suffered the ACL injury more than 1 year. Therefore, the residual mechanoreceptors in a rupture ACL can survive within 1 year and show no obvious withering. Nevertheless, there was a trend toward decreasing and degeneration of mechanoreptors when the injury duration is more than 1 year. Although it may be interfered by the sample size and the power of test, statistically significant differences were found in the number of mechanoreptors in the normal control group and Group IV of this study.
Some authors thought that the regeneration and reinnervation of sensory nerve endings in the ligament graft may be correlated with the restoration of proprioceptive function. Several reports have suggested that reinnervation of mechanoreceptors occurs after reconstruction of the ACL.[12] Barrack et al[20] found that there was an increase in the mechanoreceptors of the ACL autograft after surgery in animal experiment. However, whether this process occurs in the human ACL graft is still unidentified. According to several previous studies,[9,18,21] the ACL remnant may provide a source for a faster reinnervation of the graft and a more favorable milieu for the restoration of proprioceptive function, but this should be in coherence with the corresponding conditions described above. Whether the mechanoreceptors and proprioceptive nerve fibers in the ACL remnant have a long-term survival plays a relatively more important role. In previous studies, it was reported that the mechanoreceptors in the remnants were identified even 3 years and 42 months after patients’ injures.[8,9] Denti et al[12] suggested that morphologically normal mechanoreceptors remained in the remnant of ACL just for 3 months after the injury and their number would gradually decrease after that time. However, the limitation of above studies is lack of a large-scale sample and successive observation.
Though results of this study showed difference to the above-mentioned studies, it is yet obvious that this study have advantages in utilizing an immunohistochemical method with multiple primary antibodies and successive observation with group comparison. Till now, no similar comparison has been performed for quantitative analysis of mechanoreceptors in human ACL. An study conducted by Zelena et al[22] on the ultrastructure of Pacinian corpuscles locating on the crural interosseous membrane in adult rats after transection of the right sciatic nerve showed that the denervated inner cores survived for a long period. However, they became atrophic 10 months after neurotomy. So they implied that the neurotrophic factor had little influence on the mature sensory terminals. Their result mostly agreed with this study.
There is some debate about the preserving the remnant of the ruptured ACL during reconstruction operation. The conventional surgical method involves debridement of the tibial remnant for facilitating visualization and operative procedure. At the present time, the remnant-preserving ACL reconstruction are drawing more and more attention because of some values in enhancing the revascularization and cellular proliferation of the graft, preserving proprioceptive function, facilitating the vascular ingrowth of the grafted ACL, and so on. According to the results of this study, it was believed that the residual mechanoreceptors have a long-term survival and strong viability after the ACL torn. The results raised the possibility that the ACL remnant provided a source for graft reinnervation and proprioceptive nerve fibers in growth which all may contribute to restoration of proprioceptive function and successful clinical outcome if it is preserved during ACL reconstruction.
Some potential limitations of this study required consideration. First, due to the restriction on clinical data collection, the patients were merely divided into 5 groups in the current study. Larger sample size and more detailed group comparison may be beneficial to improve the evidence level of this analysis. Second, the injury duration was determined according to the chief complaint of the patient, and this may be interfered by some subjective factors.
This study has shown that residual mechanoreceptors do exist in the tibial remnants of the ruptured anterior cruciate ligament in human knees and identified clearly by using immunohistochemistry staining. Ruffini-like corpuscles were the most primary mechanoreceptors in the ACL remnant. It was believed that the residual mechanoreceptors have a long-term survival and strong viability after the ACL torn. The remnant may provide a source for a faster reinnervation of the graft and a more favorable milieu for the restoration of proprioceptive function if it is preserved during ACL reconstruction. The ultrastructure changes of residual mechanoreceptors with different injury duration should be studied at the next stage. A comparison of the quality and quantity of mechanoreceptors in the reconstructed ACL with and without remnant preservation will be made in the future with clinical follow-ups.
Footnotes
Abbreviations: ACL = anterior cruciate ligament, IR = immunoreactivity, PAN = posterior articular nerve, PCL = posterior cruciate ligament.
LS and GX contributed equally to the study.
Funding: This study was supported by grants from the Graduate Innovation Fund of Shanghai Jiao Tong University Medical School (BXJ201139).
The authors report no conflicts of interest.
References
- [1].McDaniel WJ, Jr, Dameron TB., Jr The untreated anterior cruciate ligament rupture. Clin Orthop Rel Res 1983;158–63. [PubMed] [Google Scholar]
- [2].Fremerey RW, Lobenhoffer P, Zeichen J, et al. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Brit 2000;82:801–6. [DOI] [PubMed] [Google Scholar]
- [3].MacDonald PB, Hedden D, Pacin O, et al. Proprioception in anterior cruciate ligament-deficient and reconstructed knees. Am J Sports Med 1996;24:774–8. [DOI] [PubMed] [Google Scholar]
- [4].Beard DJ, Kyberd PJ, Fergusson CM, et al. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Brit 1993;75:311–5. [DOI] [PubMed] [Google Scholar]
- [5].Ochi M, Iwasa J, Uchio Y, et al. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Brit 1999;81:902–6. [DOI] [PubMed] [Google Scholar]
- [6].Schultz RA, Miller DC, Kerr CS, et al. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am 1984;66:1072–6. [PubMed] [Google Scholar]
- [7].Aydog ST, Korkusuz P, Doral MN, et al. Decrease in the numbers of mechanoreceptors in rabbit ACL: the effects of ageing. Knee Surg Sports Traumatol Arthrosc 2006;14:325–9. [DOI] [PubMed] [Google Scholar]
- [8].Dhillon MS, Bali K, Vasistha RK. Immunohistological evaluation of proprioceptive potential of the residual stump of injured anterior cruciate ligaments (ACL). Int Orthop 2010;34:737–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc 2001;9:364–8. [DOI] [PubMed] [Google Scholar]
- [10].Freeman MA, Wyke B. Articular contributions to limb muscle reflexes. The effects of partial neurectomy of the knee-joint on postural reflexes. Brit J Surg 1966;53:61–8. [DOI] [PubMed] [Google Scholar]
- [11].Adachi N, Ochi M, Uchio Y, et al. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand 2002;73:330–4. [DOI] [PubMed] [Google Scholar]
- [12].Denti M, Monteleone M, Berardi A, et al. Anterior cruciate ligament mechanoreceptors. Histologic studies on lesions and reconstruction. Clin Orthop Relat Res 1994;29–32. [PubMed] [Google Scholar]
- [13].Crain EH, Fithian DC, Paxton EW, et al. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy 2005;21:19–24. [DOI] [PubMed] [Google Scholar]
- [14].Raunest J, Sager M, Burgener E. Proprioception of the cruciate ligaments: receptor mapping in an animal model. Arch Orthop Trauma Surg 1998;118:159–63. [DOI] [PubMed] [Google Scholar]
- [15].Tsuda E, Okamura Y, Otsuka H, et al. Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. Am J Sports Med 2001;29:83–7. [DOI] [PubMed] [Google Scholar]
- [16].Del Valle ME, Harwin SF, Maestro A, et al. Immunohistochemical analysis of mechanoreceptors in the human posterior cruciate ligament: a demonstration of its proprioceptive role and clinical relevance. J Arthroplasty 1998;13:916–22. [DOI] [PubMed] [Google Scholar]
- [17].Schutte MJ, Dabezies EJ, Zimny ML, et al. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am 1987;69:243–7. [PubMed] [Google Scholar]
- [18].Lee BI, Min KD, Choi HS, et al. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc 2009;17:1095–101. [DOI] [PubMed] [Google Scholar]
- [19].Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med 1982;10:329–35. [DOI] [PubMed] [Google Scholar]
- [20].Barrack RL, Lund PJ, Munn BG, et al. Evidence of reinnervation of free patellar tendon autograft used for anterior cruciate ligament reconstruction. Am J Sports Med 1997;25:196–202. [DOI] [PubMed] [Google Scholar]
- [21].Junkin DM, Jr, Johnson DL. ACL tibial remnant, to save or not? Orthopedics 2008;31:154–9. [DOI] [PubMed] [Google Scholar]
- [22].Zelena J. Survival of Pacinian corpuscles after denervation in adult rats. Cell Tissue Res 1982;224:673–83. [DOI] [PubMed] [Google Scholar]


