Abstract
Context:
The presence of athletic trainers (ATs) in secondary schools to provide medical care is crucial, especially with the rise in sports participation and resulting high volume of injuries. Previous authors have investigated the level of AT services offered, but the differences in medical care offered between the public and private sectors have not been explored.
Objective:
To compare the level of AT services in public and private secondary schools.
Design:
Concurrent mixed-methods study.
Setting:
Public and private secondary schools in the United States.
Patients or Other Participants:
A total of 10 553 secondary schools responded to the survey (8509 public, 2044 private).
Main Outcome Measure(s):
School administrators responded to the survey via telephone or e-mail. Descriptive statistics depict national data. Open-ended questions were evaluated through content analysis.
Results:
A greater percentage of public secondary schools than private secondary schools hired ATs. Public secondary schools provided a higher percentage of full-time, part-time, and clinic AT services than private secondary schools. Only per diem AT services were more frequent in the private sector. Regardless of the extent of services, reasons for not employing an AT were similar between sectors. Common barriers were budget, school size, and lack of awareness of the role of an AT. Unique to the public sector, remote location was identified as a challenge faced by some administrators.
Conclusions:
Both public and private secondary schools lacked ATs, but higher percentages of total AT services and full-time services were available in the public sector. Despite differences in AT services, both settings provided a similar number of student-athletes with access to medical care. Barriers to hiring ATs were comparable between public and private secondary schools; however, remote location was a unique challenge for the public sector.
Key Words: sports, athletes, medical coverage
Key Points
The public secondary school setting provided more athletic trainer (AT) services than the private school setting.
Although AT services were lacking in both public and private secondary schools, the number of student-athletes in each sector with access to medical care was similar.
Barriers to employing ATs in public and private settings were budgetary constraints, school size, and lack of awareness of the AT's role. An additional barrier unique to the public sector was rural location.
The importance of having an athletic trainer (AT) on site to provide medical care to student-athletes at the secondary school level has been a topic of discussion for many years.1–4 The foundation for this conversation is, in part, the rise in athletic participation.5 As of 2013–2014, the number of student-athletes was approximately 7.8 million, having risen for the 25th consecutive year.5 In addition, the high volume of injuries6 and increase in sudden deaths in this setting,4,7 particularly in comparison with the collegiate setting, have drawn attention to the presence of ATs in secondary schools. The absence of an AT has often been reported in cases of death resulting from athletic participation,8–11 as noted in high-profile cases such as those of high school football student-athletes Max Gilpin from Kentucky8 and D.J. Searcy from Georgia.9 Gilpin collapsed after a series of “gassers” at football practice when the ambient temperature and heat index were 94°,8 and Searcy collapsed during a 3-a-day practice schedule during football camp.9 Both student-athletes lost their lives because of a lack of prevention strategies and inappropriate treatment of exertional heat stroke.8,9 Providing adequate medical care at the secondary school setting helps to mitigate the risk for long-term injury complications and sudden death in athletes.1–4,12,13
As injuries and deaths continue to occur in the secondary school setting, organizations such as the American Medical Association (AMA) and National Athletic Trainers' Association (NATA) continue to endorse and support the hiring of ATs to prevent unnecessary injuries and deaths related to sport participation and physical activity. On the basis of the AT's skill set, the organizations' recommendations also speak to the data suggesting that schools with an AT present have overall lower injury rates than those schools without an AT.14 Despite the recommendations of the AMA and NATA1–4,12,13 and the documented benefits of having an AT on site, many secondary schools do not provide AT services.1,15 The presence of ATs in secondary schools is on the rise, as indicated by 2 recent studies investigating AT services in the secondary school setting,16,17 but the services provided do not meet the recommendations of the AMA and NATA. These recommendations call for all secondary schools to provide a full-time, on-site AT for student-athletes.1,18 Although secondary school–aged student-athletes benefit from some medical care from ATs, full-time services in this setting remain deficient,16,17 particularly compared with the collegiate setting.
Many reasons explain why secondary schools fail to hire ATs, including cost, school size, and location.19 However, an aspect that has not been fully explored is the difference in AT services offered between the public and private sectors. Although the differences may be subtle,17,20 understanding the barriers that exist can potentially help to increase the number of ATs employed within these settings. Our purpose was to explore the differences between AT services provided within the secondary school setting based on whether the school was public or private. The following research questions guided our investigation:
-
1.
Were there differences between medical services provided at public and private secondary schools?
-
2.
Were there differences in barriers to hiring ATs between public and private secondary schools?
METHODS
We used a concurrent mixed-methods study to identify differences between AT services provided in private and public secondary schools.21 The design was founded on triangulation, which allowed us to better quantify AT services within the settings and understand the differences between the secondary school settings. The data collected and analyzed in the present paper were compiled in 2 investigations that shared identical procedures and instruments, with the only difference being the type of secondary school setting.
Data-Collection Procedures
The University of Connecticut Institutional Review Board deemed this study exempt from review because of the public nature of the data collected. Public and private secondary schools containing at least 1 of grades 9 to 12 in the United States with an interscholastic athletic program were included. Alternative, charter, magnet, preparatory, technical, and vocational schools were not included. Phone numbers were obtained from state high school athletic associations and the US Department of Education, and e-mails were used if the school or association provided this contact information.
The athletic director (AD), or principal if no AD was employed, of each school was contacted by phone and e-mail (when available) up to 4 times or until the questions were answered. Participant characteristics are shown in Table 1; 8509 public and 2044 private secondary schools responded to the survey. The AD or principal was questioned regarding medical care during interscholastic athletic activities and practices. The detailed interview procedures and job definitions are found in previously published research.16,17 Data collection took place from September 2011 through June 2014.
Table 1.
Participant Characteristics by Secondary School Sector
| School Sector |
Schools Identified, No. |
Schools Responding, No. |
Response Rate, % |
| Public | 14 951 | 8509 | 57 |
| Private | 5414 | 2044 | 38 |
Data Analysis and Credibility
We analyzed descriptive statistics for individual states, NATA districts, and nationwide data and reported these as means. All statistical analyses were performed in SPSS (version 20.0; IBM Corp, Armonk, NY). Qualitative data were analyzed using general inductive basic content-analysis procedures to examine trends in participants' responses. We selected this systematic approach to objectively describe and quantify our textual data because it allowed us to classify our findings as guided by our purpose. The 3 specific steps taken were (1) immersing ourselves in the data to become familiar with it and to make sense of what was collected, (2) organizing the data through an open-coding procedure to identify key themes and using headings to describe the content, and (3) grouping similar responses into categories, which through interpretation became overarching themes.22 Overarching themes addressed barriers to AT employment in the secondary school setting. Quotes were selected to represent each region of the United States.
The use of multiple-analyst and data-source triangulation helped us secure the credibility of the findings.23 Content analysis as described earlier was completed by 2 researchers. They reviewed the steps before engaging in the analyses and shared their findings before reporting them. Themes presented were based upon total agreement between the 2 researchers and majority response from the data. The use of both open- and closed-ended questions allowed us to triangulate the findings.
RESULTS
Quantitative Results
More than half of all public secondary schools (8509 of 14 951) and one-third of all private secondary schools (2044 of 5414) responded to the survey (Table 1). The level of medical care provided to secondary school student-athletes differed between the public and private sectors. The AT services available in these settings are compared in Table 2. Private secondary schools provided fewer AT services (58%) than did public secondary schools (70%). The percentage of student-athletes with access to AT services was comparable between the sectors. However, public schools offered more total AT services every afternoon: 37% of public schools had full-time services versus 28% of private schools. Part-time AT services in the public sector were 31% (2619 of 8509), 6% higher than in the private sector (25%; 501 of 2042). A similar difference was noted for services provided by a clinic. The only AT service type with a higher percentage in the private secondary school setting was per diem, but the difference was merely 2%.
Table 2.
Athletic Trainer (AT) Services in Private and Public Secondary School Sectors, % (No.)
| Variable |
Secondary School Sector |
Combined Total |
|
| Public |
Private |
||
| Total AT services | 70 (5930/8509) | 58 (1176/2044) | 67 (7106/10 553) |
| Full-time AT services | 37 (3145/8509) | 28 (574/2040) | 35 (3719/10 549) |
| Coverage every afternoon | 48 (4075/8509) | 40 (767/1901) | 47 (4842/10 410) |
| Athletes with access to AT services | 86 (2 394 284/2 787 595) | 84 (281 285/336 165) | 86 (2 675 569/3 123 760) |
Qualitative Results
Data analysis revealed 3 themes shared between public and private secondary schools: budgetary constraints, school size, and lack of awareness of the AT's role. Public schools had 1 additional theme: rural location. The percentage of secondary schools responding to each question is depicted in the Figure. Quotes supporting each theme are discussed in detail in the following sections.
Figure.
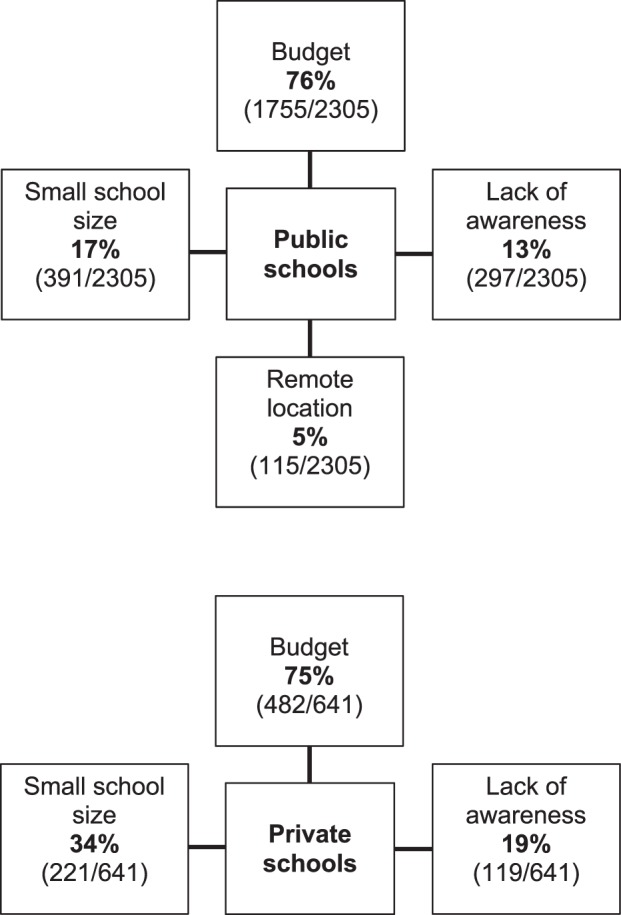
Percentages of secondary schools that provided reasons for not hiring an athletic trainer. Some schools provided more than 1 reason and appear in multiple categories. Personnel at a total of 2305 public and 641 private schools responded to the question. No need and other personnel viewed as appropriate medical providers were subthemes within the main theme of lack of awareness of the role of the athletic trainer, so those data were combined within the main theme.
Private and Public Secondary School Themes
Budgetary Constraints.
The ADs in both public and private schools indicated that lack of funding was their greatest barrier to hiring an AT. “We do not have the funding available for an athletic trainer,” said by an AD in a Michigan public school, was a common response. Similarly, a Georgia AD stated, “We're a private school so we don't have the funds,” and a Louisiana private school AD said his school “was not there yet financially.”
A related concern involved the lack of funding and support at the district administration level. For example, a Pennsylvania public school AD noted, “Our school district cut the position as a result of the financial crisis we are currently experiencing.” A public school Arizona AD remarked, “Our school and governing board will not advertise for an athletic trainer due to the budget.” Similarly, an Alabama private school AD mentioned that budget was the cause for “not [being] approved by the administration yet.”
Some public school ADs tried to solve budgetary constraints by seeking complimentary services, but there was “no health clinic around that offered free coverage” near the school in Louisiana. One Washington state public school offered “$4500 per season, but that's just not enough to get an athletic trainer to work here.” In the private sector, a Florida school wanted to rely on the community for free AT services; however, “the local colleges don't send [an AT] over.”
School Size.
Many ADs in both settings cited school size as a limiting factor: simply put, the school was not large enough to justify funding an AT position. “We are a small school” and “We're not big enough for an athletic trainer,” observed Virginia and Connecticut private school ADs, respectively. Public schools responded similarly to questions about a lack of an AT present at sporting events, citing “too low of an enrollment” in Montana and “[we] have a very small sports program” in Ohio.
“It is not common for a school of our size to have an athletic trainer” was mentioned by ADs in California, Oklahoma, and Washington, indicating that individuals at some small public schools and other low-enrollment schools felt that there was no expectation to have an AT. Some private school ADs acknowledged the need for ATs at larger institutions but did not see the need with a small student body. This was reflected by a Washington, DC, AD who stated, “I recognize a need for an athletic trainer as school size grows and the number of injuries increases,” and a Florida AD whose school was growing and “only had 2 sports for 2 years, so (now) getting an athletic trainer is the next step.” This attitude was also noted by a Utah public school AD who said his “school is only in our second year and is slowly growing so we do not see a need for an [athletic] trainer at this point since our participation numbers are so small.” Overall, both public and private sectors frequently identified school size as a barrier to hiring ATs in the secondary school setting.
Lack of Awareness of the Role of the AT.
A common theme in not hiring ATs involved the poor understanding of their role as medical professionals. In both the public and private sectors, ADs demonstrated this lack of awareness by responding that coaches and other individuals who were not medically certified (such as physical education teachers) served as medical providers or that there simply was no need for an AT at the school.
Other Personnel Viewed as Appropriate Medical Providers.
Many ADs thought that coaching education and first-aid and cardiopulmonary resuscitation training were suitable replacements for the skill set of an AT. A Texas public school AD said, “Many of the coaches have been trained and doing this for a long time so they provide medical coverage at games or when needed.” Similarly, a North Carolina AD commented, “We have a first responder who is basically an uncertified athletic trainer that is present at football games and practices,” and a California administrator believed, “Our paramedics and veteran coaches know how to tape if anything goes wrong, and the kids are sent to the doctors if they ever get a concussion.” In the private sector, an AD at a New York school replaced the AT position with a “gym teacher” and assumed the training was the same. This was also reflected by a Washington private school AD who said, “The full-time physical education teacher does a lot of work in the (athletic training) field.”
No Need.
Some ADs failed to understand the need for an AT or medical staff for student-athletes. This was illustrated by an Alaska AD who had “no need for that,” and a Missouri AD who explained, “We don't need one. We do not have football.” A Massachusetts private school AD responded to the question by saying, “That's a good question. What exactly do they do?” Furthermore, an Alabama private school AD suggested that an AT could be replaced by a “student insurance policy.” Such replies indicate that ADs may not see the need to hire ATs because they are unfamiliar with the skills, education, and services provided by these medical professionals.
Public Secondary School Theme: Rural Location
One barrier to providing AT services that was unique to public secondary schools was being in a “remote location,” as cited by an Arizona AD. Two Oregon ADs mentioned that reasons for not employing an AT were “lack of availability in a rural area” and that “the closest athletic trainer was 60 miles away.” In the northeastern United States, a public school AD from New York agreed with the previous statements and noted that they “would like to have one but we have no athletic trainers in the area… even if we tried to access them, the closest source is an hour away.” A similar reason was provided by a Virginia AD who described the rural town as a barrier, stating, “We are a very rural setting that doesn't provide a sports-minded community or resources for an athletic trainer.” These quotes suggest that ATs did not currently live in those areas and that ATs might not want to relocate to the community, creating a barrier for the schools. A similar problem was referenced by an Indiana AD who “could not find one [in the] rural area.” Multiple ADs in Alaska confirmed our overarching theme for public secondary schools by describing themselves as “bush schools in rural Alaska with no roads,” implying that an AT could not commute to their town to provide medical care. Despite this unique barrier expressed by the public schools, both the public and private sectors faced similar challenges to hiring an AT.
DISCUSSION
A comparison of AT services provided in the public and private secondary school settings revealed differences in the types and extent of medical care. Overall, the public sector offered a greater percentage of total AT services. Public secondary schools also employed more full-time ATs than private secondary schools. Only per diem AT services were more available in the private sector compared with the public sector. It is interesting that although different levels of medical care were supplied, a similar percentage of student-athletes had access to AT services in both the public and private sectors. This means that even with fewer full-time ATs in the private secondary school setting, a similar number of student-athletes were reached. Our finding that larger private secondary schools were more likely to provide AT services supports this statement. At the same time, larger schools with more student-athletes offered AT services, but student-athletes at smaller schools were not receiving adequate medical care. Even though the percentage of schools making AT services available has increased, 30% of public schools and 42% of private schools did not employ an AT. The reasons why these schools have not provided AT services warrant further investigation.
The AT services offered at public and private secondary school settings were comparable. School administrators acknowledged similar barriers for hiring ATs. Undoubtedly, budget was the most substantial problem, as illustrated in the Figure, as 76% of public and 75% of private secondary schools did not employ an AT. Thus, despite differences in funding sources for the public and private sectors, budget remained a concern across the board. In addition to monetary concerns, school size was another common barrier between settings but appeared to be a much larger hurdle for private secondary schools to overcome. According to the 2011–2012 National Center for Education Statistics Schools and Staffing Survey,24 a majority of public schools enrolled approximately 200 to 750 students per school, whereas most private schools enrolled fewer than 100 students. Therefore, on average, public schools were at least twice the size of private schools, which supports our finding that this barrier was identified by more school administrators working in the private sector. Also, Pryor et al16 reported an average of 919 students per school in the public sector, whereas private secondary schools averaged 313 students.17
The third barrier shared by both sectors was a lack of awareness, specifically of the role an AT serves in the secondary school setting. Although relatively similar in occurrence at the public (13%) and private (19%) sectors, the lack of awareness posed a substantial problem in itself. Evidence of this lack of awareness was clear when ADs relied on other personnel to provide coverage and medical care for student-athletes. School administrators and ADs, those often involved in the hiring process, relied on coaches, nurses, physicians, interns, chiropractors, physical therapists, and emergency medical technicians as medical care providers for student-athletes during practices and competitions. This may indicate that the individuals in charge of hiring do not know ATs exist or are unsure of the services they can provide to secondary school student-athletes. Similarly, other ADs demonstrated a lack of awareness of the role an AT plays in the secondary school setting by stating the school had no need for one. As the number of student-athletes participating in sports increases,5 it is of utmost importance to provide proper on-site medical care by employing an AT,4 especially in the secondary school setting. In addition to preventing, assessing, and treating injuries, ATs manage emergency situations, eliminate unnecessary physician visits, and supply immediate care to reduce the short- and long-term consequences from injuries athletes sustain in sport.4 The lack of need expressed by ADs in this study calls for increased efforts to educate this population on the role ATs play in this setting, as well as the education and skills required to become a certified AT.
Overall, a majority of private and public secondary schools experienced the same challenges in providing AT services. However, a unique barrier identified by school administrators at public secondary schools was a rural location. Participants working in a remote location indicated they had a difficult time finding ATs to fill those positions or that finding an AT to commute to the school from a hospital or clinic and provide medical care was a challenge. Some ADs also believed that ATs did not want to relocate to a smaller, remote community to work at a secondary school.
Practical Implications
Although barriers were identified in the hiring of ATs, various strategies can be explored and used to overcome these obstacles (Table 3). When administrators allocate money to their athletic program during the budgeting process, appropriate funds should also be included to employ an AT. If funds are not available for appropriate medical care, the school should reconsider offering an athletic program until this is feasible, as student-athletes are at increased risk for injury and even death in the absence of an on-site AT.12,13 Student-athlete safety should be a top priority, and this alone justifies the need to find ways to budget efficiently. One difference in budget management between the public and private secondary school settings is the party responsible for allocating money. In the public sector, the school board determines the budget.20 However, in the private sector, depending on school structure, the dean or principal may be responsible for the budget.
Table 3.
Strategies for Addressing Barriers to Hiring Athletic Trainers
| Barrier |
Strategies |
| Budget | Pay to play |
| Fundraise | |
| Raise taxes (public schools) | |
| Raise tuition (private schools) | |
| Small school | Cooperative teams with surrounding towns |
| Share coverage | |
| Lack of awareness of athletic trainer's role | Educate medical community |
| Remote location | Bring athletic trainer to area with job |
Private secondary schools are responsible for creating their own funding through tuition, grants, and fundraisers.20 The “pay-to-play” concept is a strategy that many schools are already using to increase the athletic budget and might be considered by other private and public secondary schools. This money could be put toward an AT's salary, as well as medical equipment and supplies. For either sector, employing an AT may help to cut other costs, such as insurance premiums, because risk and liability are reduced with appropriate medical care. If the budget remains a challenge despite incorporation of the suggested strategies, another option is to partner with a physical therapy or rehabilitation clinic that provides schools with an AT free of charge if patient referrals are directed back to that clinic. A possibility specific to the private sector as a means of increasing the budget is to increase tuition. Private schools generate their own revenue, so this could be the easiest way to maximize resources. Furthermore, some private schools require students to play a sport to attend, so raising tuition to provide proper medical care is something parents and guardians would likely support.
Lack of awareness of the AT's role is a barrier that is more difficult to address, as it is not something the school can change by itself. However, this can be solved if the athletic training community promotes the profession throughout secondary schools across the country. Much attention has focused on educating school administrators and school boards. Targeting smaller populations, regional schools, and the medical community may also increase awareness in secondary school personnel. Because ADs and school administrators use the services of nurses, emergency medical technicians, physicians, and others for student-athlete care, educating these individuals that ATs are the most appropriate health care professionals to provide medical care to student-athletes would be beneficial. For example, if an AD asks a nurse to supply medical services at a sporting event, the nurse who is familiar with the role of the AT can tell the AD that an AT should provide medical care in that setting as he or she is not the most qualified person to perform that duty. Offering this information to appropriate individuals could act as a catalyst for change and a means of promoting the AT profession.
Many administrators reported school size as an obstacle to overcome in justifying the hiring of an AT. Although it falls short of best practices, one option is to share AT services with other smaller schools in the area. Optimal medical care is provided by the employment of a full-time AT; however, if a school cannot afford to employ an AT, collaborating with other local schools to share AT services may be a possibility. Another strategy both private and public sectors could use is cooperative programs, whereby student-athletes from various schools in surrounding towns collectively form 1 athletic program. This type of structure brings in money from many different sources and may assist in maximizing the budget. Although this is a much larger barrier in the private than in the public secondary school setting, these strategies can be used by schools in both sectors experiencing challenges due to school size.
The barrier unique to the public sector was being located in a remote area. Schools located in these areas reported that there simply were no ATs available to employ. It is crucial to have an AT on site, especially in remote locations where emergency response times are longer. Grossman et al25 investigated differences in prehospital care between urban and rural areas and found the mean emergency response time for urban locations was 7.0 minutes, compared with 13.6 minutes in rural locations. In addition to response time, scene time and transport time were also longer for rural areas. Once at the scene of the incident, traveling to the hospital took 9 minutes longer in rural than urban locations.25 A more shocking finding that offers the best justification for ATs in remote areas is that victims in rural settings are at more than 7 times the risk of death than their urban counterparts if the emergency response exceeds 30 minutes.25 Employing on-site ATs in these remote schools ensures immediate medical attention and care: life-preserving skills such as cardiopulmonary resuscitation and automated external defibrillator (AED) application can be performed by a medical professional until emergency services arrive. From the time of collapse, an AED should be applied in less than 3 to 5 minutes26; an arrival time of 13.6 minutes for emergency services is far outside the optimal window for survival. This is of greatest concern for schools that do not have an AT or an AED on site. A strategy to address this barrier is bringing an AT to the area for a job instead of looking for an AT already living there. An individual would be more likely to relocate or move to a new area knowing that he or she is guaranteed a job. Also, increasing the salary at schools in a remote location might enhance the attractiveness of living in a less populated area. A special consideration is the state of Alaska, where medical care in any form is limited, making this a unique circumstance. For such regions, although having an AT available is the best practice, it is imperative that an easily accessible AED be available at all practice and competition locations. Additional strategies for employing ATs in remote locations warrant investigation.
Limitations and Future Directions
The biggest limitation to our study was that full-time and part-time employment were not operationally defined (ie, hours per week), so the AT's level of employment was based solely on the AD's knowledge of employment status. Perceptions of AT employment may have differed among participants. Although we strongly believe that both sectors were adequately represented, another limitation is that the response rates were only 38% and 57% for private and public schools, respectively. Because administrators from every school did not participate in the study, the actual percentages of AT services may differ, potentially altering the relationship between these services in private and public sectors.
Answers to questions that currently remain unanswered can help us to understand the next steps that should be taken for the profession. Both public and private schools relied on medical personnel other than ATs to cover practices and games, but the reason for this remains unknown. Learning why school administrators and ADs continue to favor the services of nurses, emergency medical technicians, physicians, etc, over ATs will allow us to educate these personnel about the role of ATs as medical professionals qualified to care for student-athletes.
Remote location was a stated barrier in the public but not the private setting, so a future direction would be to question private school ADs in rural areas as to how they were able to advocate for and hire an AT. This information could assist remotely located public schools that identified this barrier as a challenge. It would be interesting to follow up with schools that did not employ ATs and assess the level of change that has occurred since the study took place. Another approach would be to follow up with the ADs who employed ATs and gain a better understanding of the steps taken to secure that position. This could assist the schools without ATs in making strides toward providing AT services.
CONCLUSIONS
Both public and private secondary schools lacked ATs, but the former provided more AT services than the latter. Although public schools supplied more full-time services than did private schools, the number of student-athletes with access to some extent of medical care was comparable. The barriers to hiring ATs were similar for both settings, with budget being the largest obstacle to overcome. School size and lack of awareness of the AT's role were also common barriers. Unique to the public sector, schools located in remote areas had difficulty employing ATs. Even though barriers existed to employing ATs in secondary schools, a variety of strategies can be explored and used to provide appropriate medical care to student-athletes.
ACKNOWLEDGMENTS
The National Athletic Trainers' Association provided partial funding for this study.
REFERENCES
- 1. Lyznicki JM, Riggs JA, Champion HC. . Certified athletic trainers in secondary schools: report of the Council on Scientific Affairs, American Medical Association. J Athl Train. 1999; 34 3: 272– 276. [PMC free article] [PubMed] [Google Scholar]
- 2. Council on Sports Medicine and Fitness. Tackling in youth football. Pediatrics. 2015; 136 5: E1419– E1430. [DOI] [PubMed] [Google Scholar]
- 3. Robinson B. . The value of the secondary school athletic trainer. National Federation of State High School Associations Web site. https://www.nfhs.org/articles/the-value-of-the-secondary-school-athletic-trainer/. Published March 2015. Accessed July 27, 2016. [Google Scholar]
- 4. Athletic trainers fill a necessary niche in secondary schools. National Athletic Trainers' Association Web site. www.nata.org/NR031209. Accessed August 8, 2015. [Google Scholar]
- 5. High school participation increases for 25th consecutive year. National Federation of State High School Associations Web site. http://www.nfhs.org/articles/high-school-participation-increases-for-25th-consecutive-year/. Published October 2014. Accessed July 27, 2016. [Google Scholar]
- 6. Rechel JA, Yard EE, Comstock RD. . An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2 008; 43 2: 197– 204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mueller FO, Kucera KL, Cox LM. . Catastrophic sports injury research—thirtieth annual report: fall 1982–spring 2012. University of North Carolina at Chapel Hill Web site. http://nccsir.unc.edu/files/2014/06/NCCSIR-30th-Annual-All-Sport-Report-1982_2012.pdf. Accessed July 27, 2016. [Google Scholar]
- 8. American football coach cleared in death of teenager Max Gilpin. The Telegraph. September 2009. http://www.telegraph.co.uk/sport/othersports/americanfootball/6205261/American-football-coach-cleared-in-death-of-teenager-Max-Gilpin.html. Accessed July 27, 2016. [Google Scholar]
- 9. Parents of dead high school football stars suing. CBS This Morning Web site. http://www.cbsnews.com/news/parents-of-dead-high-school-football-stars-suing/. Published July 2012. Accessed July 27, 2016. [Google Scholar]
- 10. Slefo G. . Mother of boy who died on basketball court sues Riverside High School. Chicago Sun-Times. April 30, 2015. http://chicago.suntimes.com/news/7/71/566897/mother-boy-died-basketball-court-sues-riverside-high-school. Accessed July 27, 2016. [Google Scholar]
- 11. Kahler K, Greene G. . The game's tragic toll. MMQB Web site. http://mmqb.si.com/mmqb/2015/11/24/high-school-football-deaths-2015. Published November 2015. Accessed July 27, 2016. [Google Scholar]
- 12. Casa DJ, Almquist J, Anderson SA, et al. . The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: best-practices recommendations. J Athl Train. 2013; 48 4: 546– 553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Casa DJ, Guskiewicz KM, Anderson SA, et al. . National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012; 47 1: 96– 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. High schools with athletic trainers have more diagnosed concussions, fewer overall injuries. American Academy of Pediatrics Web site. https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/High-Schools-with-Athletic-Trainers-have-More-Diagnosed-Concussions-Fewer-Overall-Injuries.aspx. Published October 2012. Accessed July 27, 2016. [Google Scholar]
- 15. DeWitt TL, Unruh SA, Seshadri S. . The level of medical services and secondary school-aged athletes. J Athl Train. 2012; 47 1: 91– 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pryor RR, Casa DJ, Vandermark LW, et al. . Athletic training services in public secondary schools: a benchmark study. J Athl Train. 2015; 50 2: 156– 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pike AM, Pryor RR, Mazerolle SM, Stearns RL, Casa DJ. . Athletic trainer services in US private secondary schools. J Athl Train. 2016; 51 9: 717– 726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Full-time, on-site athletic trainer coverage for secondary school athletic programs. National Athletic Trainers' Association Web site. http://www.nata.org/sites/default/files/secondaryschool.pdf. Accessed July 27, 2016. [Google Scholar]
- 19. Mazerolle SM, Raso SR, Pagnotta KD, Stearns RL, Casa DJ. . Athletic directors' barriers to hiring athletic trainers in high schools. J Athl Train. 2015; 50 10: 1059– 1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Private versus public. Great Kids Web site. http://www.greatschools.org/find-a-school/defining-your-ideal/59-private-vs-public-schools.gs. Accessed July 27, 2016. [Google Scholar]
- 21. Creswell JW, . Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Los Angeles, CA: SAGE Publications; 2011. [Google Scholar]
- 22. Elo S, Kyngas H. . The qualitative content analysis process. J Adv Nurs. 2008; 62 1: 107– 115. [DOI] [PubMed] [Google Scholar]
- 23. Pitney WA, Parker J. . Qualitative Research in Physical Activity and the Health Professions. Champaign, IL: Human Kinetics; 2009. [Google Scholar]
- 24. Characteristics of public and private elementary and secondary schools in the United States: results from the 2011–12 schools and staffing survey. National Center for Education Statistics Web site. http://nces.ed.gov/pubs2013/2013312.pdf. Accessed July 27, 2016. [Google Scholar]
- 25. Grossman DC, Kim A, Macdonald SC, Klein P, Copass MK, Maier RV. . Urban-rural differences in prehospital care of major trauma. J Trauma. 1997; 42 4: 723– 729. [DOI] [PubMed] [Google Scholar]
- 26. Drezner JA, Courson RW, Roberts WO, et al. . Inter-Association Task Force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. Prehosp Emerg Care. 2007; 11 3: 253– 271. [DOI] [PubMed] [Google Scholar]


