Abstract
Background
Nipple-areola complex (NAC) reconstruction transforms a mound of soft tissue into a breast and often marks the final stage of breast reconstruction after mastectomy.
Methods
A systematic review and meta-analysis were conducted in accordance with the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines. Articles were classified based on the nipple reconstructive technique—either composite nipple sharing or local flap with nipple-sparing mastectomy (NSM) used as a control. A standardized “Satisfaction Score” (SS) for “nipple appearance” and “nipple sensation” was calculated for each technique. A Fisher’s exact test was used to compare the SS with local flap reconstruction with NSM.
Results
Twenty-three studies met the systematic review inclusion criteria. Nine NSM articles were identified with patient satisfaction data from 473 patients. The weighted average SS for NSM was 80.5%. Fourteen local flap technique articles were identified with satisfaction data from 984 patients and a weighted average SS of 73.9%. This was a statistically significant difference (P=0.0079). C-V and badge local flap techniques were associated with the highest SS, 92.6% and 90.5%, respectively. C-V and modified C-V flap technique was associated with a higher SS when compared to those using one or more other flap techniques (P=0.0001).
Conclusions
While patient satisfaction with nipple reconstruction is high regardless of technique, it is higher with NSM. When NSM is not an option, local flap reconstruction with a C-V or modified C-V flap may be associated with higher satisfaction than alternative local flap techniques.
Keywords: Mastectomy, breast reconstruction, nipple reconstruction, nipple-areola reconstruction, nipple-areola complex (NAC) reconstruction, preferred reporting items for systematic reviews and meta-analysis (PRISMA), meta-analysis
Introduction
Nipple-areola complex (NAC) reconstruction traditionally marks the final stage of breast reconstruction following mastectomy, making it an important component of the multidisciplinary approach to breast cancer. Many women endorse that the presence of a nipple following mastectomy improves body image and decreases the sense of mutilation that can accompany a mastectomy. Although preservation of a patient’s native nipple using a nipple-sparing mastectomy (NSM) technique may obviate this reconstructive step (1-8), it is sometimes not an option for patients from an oncologic perspective.
In the case of a unilateral mastectomy, composite nipple sharing can often provide a symmetric, satisfactory result (9,10). More often, however, local tissue rearrangement is used to create a nipple, followed by tattooing of the reconstructed nipple and the surrounding skin that is to become the areola. A variety of local flaps has been described in the literature (1,9-23).
Given that the benefit of breast and nipple reconstruction is aimed at psychosocial well-being rather than disease treatment, patient satisfaction is the most important outcome assessment measure. While separate studies exist that evaluate patient satisfaction with NSM and individual NAC reconstructive techniques, there is a lack of literature offering comparison between the level of satisfaction with the different methods of NAC reconstruction described and between NAC reconstruction and NSM among women undergoing mastectomy. This systematic review and meta-analysis sought to provide such comparisons.
Methods
This systematic review and meta-analysis was conducted in accordance with the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines (24).
Systematic review
A literature search was conducted using the U.S. National Library of Medicine (MEDLINE), PubMed and the Cochrane Database to identify relevant English (language) articles published between 1992 and March 2012. Keywords “nipple reconstruction” and “patient satisfaction” were used. Medical subject heading (MeSH) terms “nipples”, “reconstructive surgical procedures”, “satisfaction” and “sensation” were also exploded. Resulting article titles were examined for relevance, and duplicate title were excluded. A secondary search was conducted by evaluating references of all primary articles for any additional relevant studies. Article abstracts, and when necessary full text, were then reviewed for relevance. Exclusion criteria included technique papers, case reports and reviews. To facilitate comparison, only articles including quantitative measures of patient satisfaction were utilized. Articles were then classified based on nipple reconstructive technique—either composite nipple sharing or local flap reconstruction, with NSM used as a control. This article selection process is detailed in Figure 1.
Figure 1.
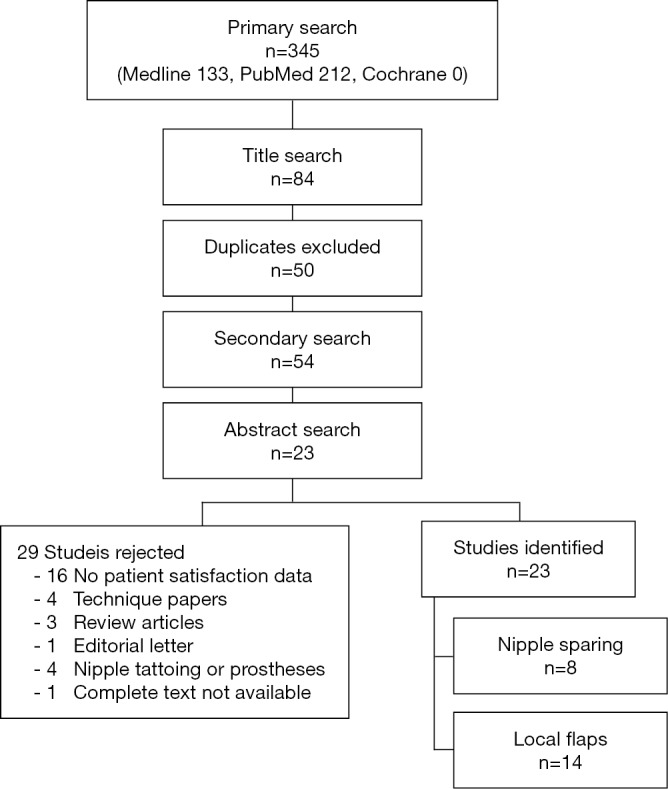
Relevant article identification process. One article contained patient satisfaction data for both nipple-sparing mastectomy (NSM) and local flap nipple reconstruction.
Quality of evidence
Each selected study was reviewed using the GRADE approach to assess the confidence in its estimate of effect. This included an assessment of the risk of bias and validity of the patient-report outcome measure used.
Data extraction and analysis
Given that a variety of aspects of patient satisfaction were evaluated with different measures used as a mark of satisfaction, a method of determining a standardized “Satisfaction Score” (SS) for the most commonly reported data points for each reconstructive method was used for the purpose of this review. A SS for both “nipple appearance” and “nipple sensation” was calculated for local flap reconstruction, as well as NSM as a control. No SS was calculated for composite nipple sharing as too few data points were identified.
The majority of studies used patient surveys with Likert scale response choices. The SS for such data was determined as the percentage of patients providing a satisfactory response as designated in the article text or decided by the reviewers. For example, many studies designated “satisfied” or “very satisfied” as survey responses indicating that the patient was satisfied. For studies utilizing a numerical scale where patients selected an integer on a scale of 1 to 5 or 1 to 10 to indicate their satisfaction, the percentage of patients providing numerical responses deemed to indicate satisfaction as described by the authors was used as the SS. In studies providing only an average numerical satisfaction value, that value was converted to a percentage by dividing by the total possible score. For example, an average satisfaction value of 3.5 on a scale of 1 to 5 translated to an SS of 70%. Similarly, for surveys asking patients to report their overall satisfaction as a percentage, the average percentage reported was used as the SS. The type of data used to determine the SS for each study is detailed in Tables 1,2. The overall SS for local flap reconstruction and NSM was determined by calculating an average SS weighted by the number of subjects in each study as shown in Tables 3,4.
Table 1. Summary of studies on patient satisfaction with nipple sparing mastectomy.
| Study | Subjects (response rate) | Follow-up | Surgical technique | Responses considered “satisfied” | Satisfaction (%) | Other results | |
|---|---|---|---|---|---|---|---|
| Nipple appearance | Nipple sensation | ||||||
| Didier et al. (1) | 159 (51.2) | Survey at 1 year | Subcutaneous NSM with intraoperative areolar ELIOT, implant reconstruction | Quite a bit, much, very much | 79 | 36 | 54% felt sexually attractive compared to 91% pre-operatively; 93% reported nipple preservation helped them cope with disease/consequences |
| Djohan et al. (2) | 78 (55.3) | 9–100 months, mean 50.4 | NSM, reconstruction with implant, DIEP, TRAM or other | Good, excellent | 72 | 10 | 66% satisfied with symmetry; 80% satisfied with color; 61% satisfied with position; 26% satisfied with arousal; 68% satisfied with texture |
| Mosahebi et al. (3) | 61 (93.0) | 8–109 months, mean 48 | NSM through mid-axillary incision, reconstruction with implant, implant + LD or DIEP | Satisfied, extremely satisfied | NA | NA | Satisfaction scores ranged 0.6 to 0.8 for all reconstruction types, with and without radiation (no significant difference); scores determined by comparing scores for reconstructed breast to contralateral or group average for unaffected breast in categories of satisfaction, comfort with brassiere and effect on sexual/social life |
| Munhoz et al. (4) | 18 (100.0) | 6–62 months, mean 29 | NSM with DCPI, BEIS reconstruction | Satisfied, very satisfied | 94.4 | NA | – |
| Nahabedian and Tsangaris (5) | 12 (100.0) | Survey at 6 months | Subcutaneous NSM, implant or flap reconstruction | Yes | 57.1 | 42.9 (present) | – |
| Sacchini et al. (6) | 110 (89.4) | 2–570.4 months, median 24.6 | NSM, implant or TRAM flap reconstruction | Score 7–10/10 | 90 | NA | Satisfaction 89%, 96% and 86% for implant, tissue expander and TRAM flap respectively; 94% satisfaction in prophylactic versus 87% in therapeutic |
| Ueda et al. (7) | 26 (79.0) | Median 16 months after chemotherapy and radiation | NSM, implant, LD, TRAM or DIEP reconstruction | Score out of 100% | NA | NA | Satisfaction scores using quality of life questionnaire for cancer patients treated with anticancer drugs: social activity 95%, physical aspects 88%, general condition 79%, bodily pain 76%, body image 73.5%, sexual aspects 60% |
| Yueh et al. (8) | 9 (90.0) | 2–89 months, mean 23 | NSM, implant or flap reconstruction | Satisfied, very satisfied | 66.7 | 80 (present) | 8.8/10 symmetry satisfaction score; 8.6/10 pigmentation satisfaction score |
NSM, nipple-sparing mastectomy; ELIOT, electron-beam radiotherapy; DIEP, deep inferior epigastric perforator flap; TRAM, transverse rectus abdominus muscle; LD, latissimus dorsi muscle; NA, not applicable; DCPI, double concentric periareolar incision; BEIS, biodimensional anatomical expander-implant system.
Table 2. Summary of studies on patient satisfaction with local flap nipple reconstruction.
| Study | Subjects (response rate) | Follow-up | Surgical technique | Responses considered “satisfied” | Satisfaction (%) | Other results | |
|---|---|---|---|---|---|---|---|
| Nipple appearance | Nipple sensation | ||||||
| Chen et al. (11) | 11 (100.0) | 12–27 months, mean 17 | Badge flap + tattooing on free or pedicled TRAM flap reconstruction | Score out of 100% | 90.5 | NA | Mean pigmentation score 8.5/10 |
| Cheng et al. (12) | 22 (88.0) | 6–36 months, mean 18 | Modified S dermal-fat flap + tattooing on free or pedicled TRAM, implant-only or LD + implant | Moderately pleased, very pleased | 86.4 | 13.6 | 50% satisfied with nipple projection; 90.9% satisfied with nipple symmetry; 54.5% satisfied with nipple size; 100% satisfied with nipple color; 100% would recommend the procedure |
| Costa and Ferreira (13) | 122 | Survey at 3 years | C-V flap + tattooing on double-pedicled TRAM or implant | Good, excellent | 92.6 | NA | 35% satisfaction in patients who underwent NAC reconstruction with skin graft from medial thigh |
| Didier et al. (1) | 92 (67.8) | Survey at 1 year | Unspecified | Quite a bit, much, very much | 43.0 | 20.0 | 72% felt sexually attractive compared to 98% pre-operatively; 34% found it difficult to look at themselves naked |
| El-Ali et al. (14) | 50 (100.0) | 6–36 months, mean 15.4 | Modified C-V flap + tattooing on LD, pedicled TRAM or implant | Good, very good | 80.0 | 28.0 (sensation present) | 82% satisfied with reconstructed NAC compared to opposite side; 82% reported body image improvement |
| Goh et al. (15) | 91 (100.0) | 1–86 months, mean 38.5* | Various flaps + tattooing on TRAM, DIEP, LD +/– implant or implant | Satisfactory, good, excellent | 88.0* | NA | 95% rated NAC position “about right”*; 87% rated NAC dimension “about right”*; 58% rated NAC projection “about right”* |
| Gullo et al. (16) | 161 | Survey at 1 year | Star flap enhanced by scar tissue° + tattooing on DIEP, TRAM or implant | Good (5–6.9/10), very good (³7/10) | 6.61/10 (SS =66.1%) | 4.11/10 (SS =41.1%) | Color satisfaction score of 6.36; position satisfaction score of 7.24; symmetry satisfaction score of 7.97 |
| Harcourt et al. (17) | 127 (51.4) | 3–84 months | Unspecified | Satisfied, very satisfied | 71.6 | 56.5 | 81.9% satisfied with nipple color; decision regret most strongly correlated with dissatisfaction and high depression score |
| Jabor et al. (18) | 43 (41.0) | ³6 months | Various flaps + immediate tattooing on TRAM, LD + implant or implant | Good, excellent | 64.0 | NA | No significant difference in NAC satisfaction with different breast mound or NAC types; factors most disliked in descending order: projection, color, size, texture, position; mean interval between mound and NAC reconstruction of 9.71 & 7.25 months in satisfied & unsatisfied patients, respectively (P=0.003) |
| Losken et al. (19) | 11 (“poor”) | 3–7 years, mean 5.3 | C-V flap + tattooing on TRAM flap | Score out of 100% | 81.0 | 26.0 | 42% satisfied with projection; 62% satisfied with pigmentation |
| Lossing et al. (20) | 21 (100.0) | 29–46 months, mean 36 | Modified S-flap + tattooing on lateral thoracodorsal flap | Score out of 10 | 8.2/10 (SS =82%) | 29.0 (sensation present) | Overall breast reconstruction satisfaction score of 8.9 |
| Otterburn et al. (22) | 199 | >1 year | C-V flap + tattooing on TRAM, implant or LD + implant | Score out of 5 | 3.8/5 (SS =76%) | 1.3/5 (SS =26%) | Color satisfaction score of 3.2/5; position satisfaction score of 4.2/5; projection satisfaction score of 3.3/5 |
| Valdatta et al. (23) | 29 (100.0) | Survey at 1 year | C-V flap + tattooing on | Score out of 10 | 6.65/10 (SS =66.5%) | 5.57/10 (SS =55.7%) | Color satisfaction score of 6.14; position satisfaction score of 7.85; projection satisfaction score of 6.28; symmetry satisfaction score of 7.42 |
*, data includes results for ten additional patients who underwent composite nipple sharing; ˚, primary procedure in 98 patients, secondary procedure for projection failure in 63 patients. TRAM, transverse rectus abdominus muscle; NA, not applicable; LD, latissimus dorsi muscle; NAC, nipple-areolar complex; DIEP, deep inferior epigastric perforator flap.
Table 3. Meta-analysis data for patient satisfaction with nipple sparing mastectomy.
| Variable | SS (%) | SE | Weight (%) | SS, 95% CI |
|---|---|---|---|---|
| Study | ||||
| Didier et al. (1) | 79.0 | 0.0323 | 41.2 | 0.79 (0.727, 0.853) |
| Djohan et al. (2) | 72.0 | 0.0508 | 20.2 | 0.72 (0.620, 0.820) |
| Munhoz et al. (4) | 94.4 | 0.0542 | 4.7 | 0.944 (0.838, 1.050) |
| Nahabedian and Tsangaris (5) | 57.1 | 0.1429 | 3.1 | 0.571 (0.359, 0.975) |
| Sacchini et al. (6) | 90.0 | 0.0286 | 28.5 | 0.90 (0.844, 0.956) |
| Ueda et al. (7) | NA | NA | NA | NA |
| Yueh et al. (8) | 66.7 | 0.1571 | 2.3 | 0.667 (0.359, 0.975) |
| Pooled estimate | 80.5 | – | 100.0 | 0.805 (0.765, 0.844) |
SS, satisfaction score; SE, standard error; CI, confidence interval; NA, not applicable.
Table 4. Meta-analysis data for patient satisfaction with local flap reconstruction.
| Variable | SS (%) | SE | Weight (%) | SS, 95% CI |
|---|---|---|---|---|
| Study | ||||
| Chen et al. (11) | 90.5 | 0.0884 | 1.12 | 0.905 (0.817, 0.994) |
| Cheng et al. (12) | 86.4 | 0.0730 | 2.24 | 0.864 (0.791, 0.937) |
| Costa and Ferreira (13) | 92.6 | 0.0237 | 12.40 | 0.926 (0.902, 0.950) |
| Didier et al. (1) | 43.0 | 0.0516 | 9.35 | 0.430 (0.378, 0.482) |
| El-Ali et al. (14) | 80.0 | 0.0565 | 5.08 | 0.800 (0.743, 0.857) |
| Goh et al. (15) | 88.0 | 0.0340 | 9.25 | 0.880 (0.856, 0.914) |
| Gullo et al. (16) | 66.1 | 0.0373 | 16.36 | 0.661 (0.624, 0.698) |
| Harcourt et al. (17) | 71.6 | 0.0400 | 12.91 | 0.716 (0.676, 0.756) |
| Jabor et al. (18) | 64.0 | 0.0731 | 4.37 | 0.640 (0.567, 0.713) |
| Losken et al. (19) | 81.0 | 0.1182 | 1.12 | 0.810 (0.692, 0.928) |
| Lossing et al. (20) | 82.0 | 0.0838 | 2.13 | 0.820 (0.736, 0.904) |
| Oliveira et al. (21) | 80.0 | 0.1788 | 0.51 | 0.800 (0.621, 0.979) |
| Otterburn et al. (22) | 76.0 | 0.0302 | 20.22 | 0.760 (0.730, 0.790) |
| Valdatta et al. (23) | 66.5 | 0.0876 | 2.95 | 0.665 (0.577, 0.753) |
| Pooled estimate | 73.9 | – | 100.00 | 0.739 (0.725, 0.753) |
SS, satisfaction score; SE, standard error; CI, confidence interval; NA, not applicable.
Data analysis also included a Fisher’s exact test to determine if there was a statistically significant difference between the SS with local flap reconstruction compared to that with NSM, as well as between the individual local flap reconstruction techniques compared to all other flap techniques combined.
Results
Data extraction and analysis
Initial primary search identified 345 articles with four additional articles found in the secondary search of the references from relevant articles. Of these, a total of 23 studies met the systematic review inclusion criteria, all containing patient satisfaction data. For use as a control, eight articles examining satisfaction with nipple-sparing mastectomies on 473 patients were included. Two articles evaluating the use of composite nipple sharing in 91 patients were identified. Fourteen studies contained satisfaction data from 984 patients undergoing nipple reconstruction with various local skin flaps.
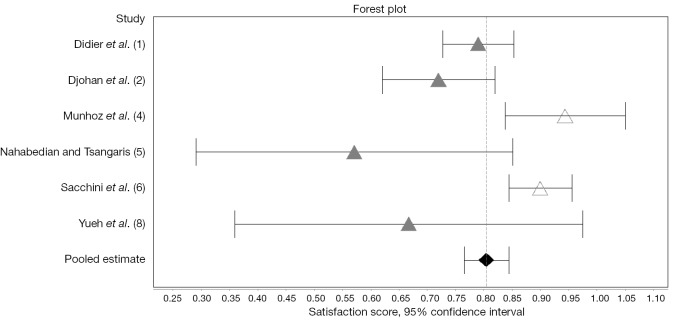
For each included article, the number of subjects, length of follow-up, surgical technique and patient satisfaction data was determined and recorded in Tables 1,2,5. Table 1 reflects data from patients undergoing NSM with various methods of reconstruction including both immediate and staged implants, as well as pedicled and free autologous flaps. Of the nine NSM articles identified, six contained patient satisfaction data for nipple appearance from 386 patients. The weighted average SS was 80.5% (95% CI, 0.765–0.844) as calculated in Table 3 and shown in Figure 2. Only two studies included satisfaction data for nipple sensation from 237 patients, which yielded a weighted average SS of 27.4%.
Table 5. Summary of studies on patient satisfaction with composite nipple sharing.
| Study | Subjects (response rate) | Follow-up | Responses considered “satisfied” | Satisfaction (%) | Other results | |
|---|---|---|---|---|---|---|
| Nipple appearance | Nipple sensation | |||||
| Spear et al. (9) | 34 (57.6) | 0–16 years | Satisfied, very satisfied | 92 | NA | 88% satisfied with naturalness of nipple; 92% satisfied with color; 85% satisfied with projection; 63% reported minimal or no decrease in donor nipple sensation; 63% reported role of donor nipple in femininity/sexuality was slightly decreased or unchanged; 80% probably or definitely would undergo procedure again |
| Zenn and Garofalo (10) | 57 (65.0) | 2–69 months, mean 33 | Reasonable to same as before (3–5/5) | NA | 35 | 91%, 93% & 87% satisfied with color, shape & size, respectively; 96% reported donor nipple appeared “not bad” or better; 87% with donor nipple sensation present; 87% with residual donor nipple erectile function; 87% would undergo procedure again |
NA, not applicable.
Figure 2.
Forest plot showing satisfaction scores with nipple-sparing mastectomy (NSM) (1,2,4-6,8).
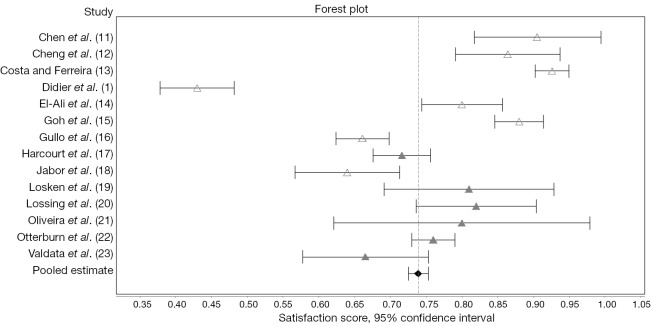
The data from articles evaluating the use of local skin flap reconstruction is shown in Table 2. The most commonly used local flap techniques included C-V, S, star, skate and badge flaps, with or without modification. All 14 included studies contained data for calculation of an SS for nipple appearance; the weighted average SS was 73.9% (95% CI, 0.725–0.753) as calculated in Table 4 and shown in Figure 3. Seven of the articles provided nipple sensation satisfaction data with a weighted average SS of 35.9%. The studies with the highest reported SS for appearance were those which used the C-V and badge local flap techniques with a SS of 92.6% and 90.5%, respectively.
Figure 3.
Forest plot showing satisfaction scores with local flap nipple reconstruction (1,11-23).
A Fisher’s exact test comparing patient satisfaction with local flap reconstruction compared to NSM had a P value of 0.0079. A significant difference in SS (P=0.0001) was also seen in studies which utilized only a C-V or modified C-V flap technique compared to those using one or more other flap techniques.
Only one of the two nipple sharing studies provided results for each nipple appearance and nipple sensitivity (Table 5). For this reason, no SS was calculated for either category.
Quality of evidence
Using the GRADE approach, the studies were evaluated for the confidence in their estimate of effect. As no widely-accepted, validated questionnaire for nipple reconstruction satisfaction exists, the validity of patient-reported outcome measures utilized cannot be established. All 23 included studies were performed retrospectively and relied on patient questionnaire responses, making them inherently prone to response bias. The eight studies with response rates less than 80% were considered to be at higher risk of bias due to low response rates. There were also four studies which did not disclose a response rate. A lower confidence was also attributed to studies of smaller size. In reviewing the collection of studies as a whole, a great deal of publication bias is likely also present due to the reluctance to report low patient satisfaction results.
Discussion
Breast reconstruction has become a fundamental component of the multidisciplinary approach toward the treatment of women with breast cancer, making the plastic surgeon an integral part of this treatment team. The breast is an important component of the female identity. Following mastectomy, women report that undergoing reconstruction helps them to feel as though they have overcome the disease, to cope with their feelings regarding the loss of their breast and to improve their body image (25).
Previous studies assessing patient satisfaction with various methods of breast reconstruction have established that the presence of a nipple, whether native or reconstructed, positively impacts overall patient satisfaction with the breast. Posited explanations include the creation of a finished looking breast, an increased sense of attractiveness, a feeling of a more normal appearance and improvement in symmetry in cases of unilateral reconstruction (18,26-29).
Given that both breast mound and nipple reconstruction play a psychosocial, rather than a disease-modification role, patient satisfaction and health-related quality of life (HR-QoL) improvement are the most important outcomes of interest. Assessment of these outcome measures, however, is subjective and difficult to evaluate. It relies on the use of patient surveys and questionnaires which introduce response and self-selection bias. In a systematic review such as this, further difficulty exists due to the lack of consistency in the manner in which “satisfaction” is measured, both in the aspects of the reconstruction evaluated and the quantification of the responses. The ability to draw conclusions based on the statistical results of this review is extremely limited by the created SS. While we feel this was the best available method to allow comparison between the included studies, it was clearly less than ideal.
The utilization of standardized patient-reported outcome measures like the BREAST-Q provides a way to quantify patient satisfaction and HR-QoL outcomes (29). Currently, this type of validated outcome measure does not exist specifically for nipple reconstruction, but it would be beneficial in providing surgeons a tool to assess their own outcomes and facilitate comparison between the many different local flap techniques. It would also allow for more consistency when assessing multiple different studies or conducting multi-center studies.
Despite the imperfect comparative analysis technique utilized due to the limitations of the available publications, a significantly higher patient SS was seen with use of the C-V or modified C-V flap. Reasons authors cited for favoring this flap included its ease, consistency, reliability and lack of donor site morbidity (14,19,22,23). With the high satisfaction seen regardless of technique, however, factors such as surgeon preference and experience should be considered when choosing a nipple reconstruction technique.
As the oncologic safety of nipple-sparring mastectomy continues to be better understood and accepted, more and more patients will likely be able to keep their native nipples. There will, however, always be cases in which resection of the NAC is necessary, making ever-relevant the quest for an ideal nipple reconstruction technique that provides a realistic, well-projected nipple with a high patient satisfaction rate.
Conclusions
Patient satisfaction with nipple reconstruction is high, regardless of the technique used. Although patient satisfaction with breast reconstruction has previously been demonstrated to be higher with nipple reconstruction compared to foregoing nipple reconstruction, patient satisfaction is significantly higher among those who undergo NSM than those who require nipple reconstruction with one of a variety of popular local flap techniques. When safe from an oncologic perspective, NSM should be performed when possible. When NSM is not an option, local flap reconstruction with C-V or modified C-V flap may be associated with higher satisfaction than alternative local flap techniques.
Acknowledgements
None.
Footnotes
Conflicts of Interest: Dr. Nahabedian is a speaker/consultant for LifeCell, Sientra, and Allergan. Dr. Satteson and Dr. Brown have no conflicts of interest to declare.
References
- 1.Didier F, Radice D, Gandini S, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat 2009;118:623-33. 10.1007/s10549-008-0238-4 [DOI] [PubMed] [Google Scholar]
- 2.Djohan R, Gage E, Gatherwright J, et al. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg 2010;125:818-29. 10.1097/PRS.0b013e3181ccdaa4 [DOI] [PubMed] [Google Scholar]
- 3.Mosahebi A, Ramakrishnan V, Gittos M, et al. Aesthetic outcome of different techniques of reconstruction following nipple-areola-preserving envelope mastectomy with immediate reconstruction. Plast Reconstr Surg 2007;119:796-803. 10.1097/01.prs.0000251999.52374.09 [DOI] [PubMed] [Google Scholar]
- 4.Munhoz AM, Aldrighi C, Montag E, et al. Optimizing the nipple-areola sparing mastectomy with double concentric periareolar incision and biodimensional expander-implant reconstruction: aesthetic and technical refinements. Breast 2009;18:356-67. 10.1016/j.breast.2009.09.008 [DOI] [PubMed] [Google Scholar]
- 5.Nahabedian MY, Tsangaris TN. Breast reconstruction following subcutaneous mastectomy for cancer: a critical appraisal of the nipple-areola complex. Plast Reconstr Surg 2006;117:1083-90. 10.1097/01.prs.0000202103.78284.97 [DOI] [PubMed] [Google Scholar]
- 6.Sacchini V, Pinotti JA, Barros AC, et al. Nipple-sparing mastectomy for breast cancer and risk reduction: oncologic or technical problem? J Am Coll Surg 2006;203:704-14. 10.1016/j.jamcollsurg.2006.07.015 [DOI] [PubMed] [Google Scholar]
- 7.Ueda S, Tamaki Y, Yano K, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery 2008;143:414-25. 10.1016/j.surg.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 8.Yueh JH, Houlihan MJ, Slavin SA, et al. Nipple-sparing mastectomy: evaluation of patient satisfaction, aesthetic results, and sensation. Ann Plast Surg 2009;62:586-90. 10.1097/SAP.0b013e31819fb1ac [DOI] [PubMed] [Google Scholar]
- 9.Spear SL, Schaffner AD, Jespersen MR, et al. Donor-site morbidity and patient satisfaction using a composite nipple graft for unilateral nipple reconstruction in the radiated and nonradiated breast. Plast Reconstr Surg 2011;127:1437-46. 10.1097/PRS.0b013e318208d107 [DOI] [PubMed] [Google Scholar]
- 10.Zenn MR, Garofalo JA. Unilateral nipple reconstruction with nipple sharing: time for a second look. Plast Reconstr Surg 2009;123:1648-53. 10.1097/PRS.0b013e3181a3f2f9 [DOI] [PubMed] [Google Scholar]
- 11.Chen SG, Chiu TF, Su WF, et al. Nipple-areola complex reconstruction using badge flap and intradermal tattooing. Br J Surg 2005;92:435-7. 10.1002/bjs.4885 [DOI] [PubMed] [Google Scholar]
- 12.Cheng MS, Ho CM, Cheung WY, et al. Nipple-areola reconstruction in autologous breast reconstruction: Chinese patients' perspective. Ann Plast Surg 2004;53:328-33. 10.1097/01.sap.0000137247.53249.a1 [DOI] [PubMed] [Google Scholar]
- 13.Costa MP, Ferreira MC. Aesthetic quality of the nipple-areola complex in breast reconstruction with a new local graft technique. Aesthetic Plast Surg 2009;33:774-9. 10.1007/s00266-009-9387-z [DOI] [PubMed] [Google Scholar]
- 14.El-Ali K, Dalal M, Kat CC. Modified C-V flap for nipple reconstruction: our results in 50 patients. J Plast Reconstr Aesthet Surg 2009;62:991-6. 10.1016/j.bjps.2007.12.059 [DOI] [PubMed] [Google Scholar]
- 15.Goh SC, Martin NA, Pandya AN, et al. Patient satisfaction following nipple-areolar complex reconstruction and tattooing. J Plast Reconstr Aesthet Surg 2011;64:360-3. 10.1016/j.bjps.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 16.Gullo P, Buccheri EM, Pozzi M, et al. Nipple reconstruction using a star flap enhanced by scar tissue: the Regina Elena Cancer Institute experience. Aesthetic Plast Surg 2011;35:731-7. 10.1007/s00266-011-9677-0 [DOI] [PubMed] [Google Scholar]
- 17.Harcourt D, Russell C, Hughes J, et al. Patient satisfaction in relation to nipple reconstruction: the importance of information provision. J Plast Reconstr Aesthet Surg 2011;64:494-9. 10.1016/j.bjps.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 18.Jabor MA, Shayani P, Collins DR, et al. Nipple-areola reconstruction: satisfaction and clinical determinants. Plast Reconstr Surg 2002;110:457-63; discussion 464-5. 10.1097/00006534-200208000-00013 [DOI] [PubMed] [Google Scholar]
- 19.Losken A, Mackay GJ, Bostwick J. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg 2001;108:361-9. 10.1097/00006534-200108000-00013 [DOI] [PubMed] [Google Scholar]
- 20.Lossing C, Brongo S, Holmström H. Nipple reconstruction with a modified S-flap technique. Scand J Plast Reconstr Surg Hand Surg 1998;32:275-9. 10.1080/02844319850158606 [DOI] [PubMed] [Google Scholar]
- 21.Oliveira M, Nunes D, Beolchi M, et al. Circular local skin flap. A new approach to areola reconstruction. Acta Cir Bras 2007;22:322-6. 10.1590/S0102-86502007000400015 [DOI] [PubMed] [Google Scholar]
- 22.Otterburn DM, Sikora KE, Losken A. An outcome evaluation following postmastectomy nipple reconstruction using the C-V flap technique. Ann Plast Surg 2010;64:574-8. [DOI] [PubMed] [Google Scholar]
- 23.Valdatta L, Montemurro P, Tamborini F, et al. Our experience of nipple reconstruction using the C-V flap technique: 1 year evaluation. J Plast Reconstr Aesthet Surg 2009;62:1293-8. 10.1016/j.bjps.2008.03.064 [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Telzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Filiberti A, Tamburini M, Murru L, et al. Psychologic effects and esthetic results of breast reconstruction after mastectomy. Tumori 1986;72:585-8. [DOI] [PubMed] [Google Scholar]
- 26.Guyomard V, Leinster S, Wilkinson M. Systematic review of studies of patients’ satisfaction with breast reconstruction after mastectomy. Breast 2007;16:547-67. 10.1016/j.breast.2007.04.004 [DOI] [PubMed] [Google Scholar]
- 27.Ramon Y, Ullmann Y, Moscona R, et al. Aesthetic results and patient satisfaction with immediate breast reconstruction using tissue expansion: a follow-up study. Plast Reconstr Surg 1997;99:686-91. 10.1097/00006534-199703000-00013 [DOI] [PubMed] [Google Scholar]
- 28.Shaikh-Naidu N, Preminger BA, Rogers K, et al. Determinants of aesthetic satisfaction following TRAM and implant breast reconstruction. Ann Plast Surg 2004;52:465-70; discussion 470. 10.1097/01.sap.0000123901.06133.b7 [DOI] [PubMed] [Google Scholar]
- 29.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast Reconst Surg 2009;124:345-53. 10.1097/PRS.0b013e3181aee807 [DOI] [PubMed] [Google Scholar]