Abstract
Objective
Both impulsivity and sleep disturbance have been associated with heavy alcohol use among young adults; yet studies to date have not examined their interactive effects. The current study aimed to determine if adequate sleep moderates the association between impulsive personality traits and alcohol use among young adults.
Method
College students (N = 568) who had been mandated to alcohol treatment following violation of campus alcohol policy provided information regarding alcohol use and related consequences, impulsive personality traits (measured using the UPPS Impulsive Behavior Scale), and perception of sleep adequacy as part of a larger intervention trial.
Results
Higher urgency, lower premeditation, and higher sensation-seeking predicted greater levels of alcohol consumption, while higher urgency predicted more alcohol-related consequences. As hypothesized, there was a significant interaction between premeditation and sleep adequacy in the prediction of drinks per week; in contrast to hypotheses, however, premeditation was associated with drinking only among those reporting adequate (rather than inadequate) sleep. Specifically, the tendency to premeditate was associated with less drinking among those who reported adequate sleep and was not associated with drinking among those reporting inadequate sleep.
Conclusion
Sensation-seeking and urgency are associated with greater alcohol involvement among young adults, regardless of sleep adequacy. Conversely, the ability to plan ahead and anticipate the consequences of one’s behaviors (premeditation) is only protective against heavy drinking among individuals receiving adequate sleep. With replication, these findings may inform alcohol prevention and intervention efforts.
Keywords: mandated college students, drinking, premeditation, sensation-seeking, urgency
Both impulsivity (Ashenhurst, Harden, Corbin, & Fromme, 2015) and poor sleep health (DeMartini & Carey, 2009; DeMartini & Fucito, 2014; Kenney, Lac, LaBrie, Hummer, & Pham, 2013) have been associated with problematic alcohol use among young adults. However, the nature of the association between sleep and impulsivity and the combined impact of these factors on alcohol use is unclear. College students who engage in impulsive decision-making are more than twice as likely to report problematic versus non-problematic drinking (Murphy & Garavan, 2011). Because sleep deprivation has also been associated with impaired decision-making (Killgore, Balkin, & Wsensten, 2006; Schnyer, Zeithamova, & Williams, 2009; Venkatraman, Chuah, Huettel, & Chee, 2007), inadequate sleep may compound the negative effect of impulsivity on decision-making, leading to greater alcohol use and related consequences among individuals who tend to act impulsively.
Impulsivity and Alcohol Use
Impulsivity is well established as a predictor of alcohol involvement among emerging adults (Ashenhurst et al., 2015; Littlefield, Sher, & Steinley, 2010; Murphy & Garavan, 2011). Research in line with the personality-based conceptualization of impulsivity suggests that impulsivity is a multifaceted construct and the personality traits underlying this construct are differentially associated with alcohol use (Lynam & Miller, 2004; Lynam, Smith, Cyders, Fischer, & Whiteside, 2007; Magid & Colder, 2007; Miller, Flory, Lynam, & Leukefeld, 2003). Based on the findings of Whiteside and Lynam (2001), four personality traits that lead to impulsive behavior are urgency, defined as a tendency to behave rashly as a result of negative affect; lack of premeditation, or a failure to consider the consequences of one’s actions; lack of perseverance, an inability to persist beyond boredom or fatigue in fulfilling obligations; and sensation-seeking, a preference for stimulating and exciting activities associated with underarousal (Miller et al., 2003; Zuckerman, 1979).
When examining the relative contributions of these personality traits to drinking outcomes, high sensation-seeking and low premeditation seem to be the strongest predictors of drinking quantity, while high urgency is the strongest predictor of alcohol-related consequences (Kiselica, Echevarria, & Borders, 2015; Magid & Colder, 2007).1 This is consistent with latent class models, in which high sensation-seeking and low premeditation generally paralleled drinking trajectories of young adults from high school through college (Ashenhurst et al., 2015). Thus, it seems that high sensation-seeking, low premeditation, and high urgency may serve as particularly strong risk factors for heavy drinking and related consequences among young adults in college. Given the negative outcomes associated with heavy alcohol use among college students (Hingson, Zha, & Weitzman, 2009; Johnston, O'Malley, Bachman, Schulenberg, & Miech, 2015), research on behaviors that may exacerbate or minimize this risk is warranted.
Sleep and Alcohol Use
Poor sleep health also contributes to problematic alcohol use among adolescents and young adults. Conceptualizing ‘sleep health’ as a multidimensional pattern of sleep and wakefulness that promotes physical and mental well-being, Buysse (2014) suggests that sleep health may be characterized by (a) subjectively ‘good’ sleep quality (measured in this study as ‘sleep adequacy’), (b) an ability to maintain alert wakefulness during the day, (c) appropriate timing of sleep within the 24-hour day (e.g., consistent bedtimes), (d) easy and efficient sleep onset, and (e) developmentally appropriate sleep duration. Longitudinal and nationally representative studies have found robust associations between dimensions of poor sleep health and alcohol involvement in adolescents and young adults. Specifically, sleep duration has been associated with alcohol and other drug use, with some studies indicating that these associations occur in a dose-response manner (Sivertsen, Skogen, Jakobsen, & Hysin, 2015; Winsler, Deutsch, Vorona, Payne, & Szklo-Coxe, 2015; Wong, Robertson, & Dyson, 2015); delayed bedtimes and circadian rhythms have been associated with alcohol use and related problems (Hasler, Soehner, & Clark, 2015; Pasch, Latimer, Cance, Moe, & Lytle, 2012; Pieters, Van Der Vorst, Burk, Wiers, & Engels, 2010); daytime sleepiness has been associated with the age of onset of alcohol and other drug use (Wong, Brower, & Zucker, 2009); and difficulty initiating/maintaining sleep has been associated with the onset of alcohol use and related problems (Hasler et al., 2015; Wong, Brower, Fitzgerald, & Zucker, 2004; Wong et al., 2015). Of all these components of sleep health, however, sleep quality seems to play a particularly meaningful role in the occurrence of alcohol-related problems. Among college students, for example, poor sleep quality is a significant predictor of alcohol-related consequences, even after controlling for relevant variables such as drinking motives and poor mental health (Kenney, LaBrie, Hummer, & Pham, 2012; Kenney et al., 2013). Collectively, these data suggest that poor sleep health is a risk factor for heavy alcohol use and related problems among adolescents and young adults.
Sleep and Impulsivity
While both sleep and impulsivity have been linked to alcohol use, studies examining the association between sleep and impulsivity have been limited. In exploratory research, higher levels of urgency and lower levels of perseverance were correlated with greater sleep-related distress, whereas high sensation-seeking and low premeditation were unrelated to insomnia severity (Schmidt, Gay, & Van der Linden, 2008). However, these data were limited by the use of statistics that describe only bivariate associations between variables. Experimental studies examining associations between sleep and risk-taking, which may reflect impulsive behavior, are also non-conclusive. Twenty-three hours of sleep deprivation has been found to reduce risk-taking on the Balloon Analogue Risk Task (Acheson, Richards, & de Wit, 2007; Killgore, 2007), but approximately 50 hours of sleep deprivation increased risk-taking on the Iowa Gambling Task (Killgore et al., 2006). The relevance of findings from these behavioral impulsivity tasks to self-reported measures of impulsivity is unclear (Dick et al., 2010).
Although the link between sleep and impulsivity is poorly understood, growing evidence suggests there is an association between sleep and self-control (Meldrum, Barnes, & Hay, 2015; Pilcher, Callan, & Posey, 2015), which has been posited as a component of impulsivity (Costa & McCrae, 1992). In a recent study, one night of sleep loss was associated with a significant decrease in response inhibition on a Go/NoGo task, such that sleep-deprived participants had more difficulty inhibiting their responses to negative emotional stimuli than participants who had slept (Anderson & Platten, 2011). Thus, it seems acute sleep deprivation may have a negative effect on impulse control.
Current Study
The current study aimed to examine the associations between sleep, impulsivity, and alcohol use among young adults in college. Impulsive decision-making has been associated with heavy alcohol use (Murphy & Garavan, 2011), and sleep deprivation seems to impact one’s ability to make decisions (Killgore et al., 2006; Schnyer et al., 2009; Venkatraman et al., 2007). Therefore, we expected past-month sleep adequacy to moderate the association between impulsive personality traits and alcohol use, such that the association between facets of impulsivity and alcohol use would be strongest among those reporting inadequate sleep. Because high sensation-seeking and low premeditation have demonstrated the strongest associations with drinking quantity and high urgency has been most strongly associated with alcohol-related consequences (Kiselica et al., 2015), we hypothesized that sleep adequacy would moderate (a) the effects of sensation-seeking and premeditation on drinking quantity and (b) the effect of urgency on alcohol-related consequences.
Method
Participants and Procedure
Undergraduate students who had violated campus alcohol policy and had been mandated to alcohol treatment by the Office of Community Standards were recruited from a public university in the Northeast to participate in a larger intervention project (Carey et al., 2016). Violations ranged from drinking in the dormitory to ambulance transport to the emergency department. Mandated students had the option of participating in either the research project [involving a brief alcohol intervention (Carey et al., 2016) with email boosters] or the standard alcohol sanction. Participation in the research project involved several online survey assessments over the course of a year, but only data from the baseline assessment was used in this study. A total of 568 students (28% female, 84% White) with a mean age of 19.18 years (SD = 1.16) consented to participate. Participants were primarily freshmen (38%) and sophomores (35%), although juniors (18%) and seniors (9%) were also represented. All procedures were approved by the university’s Institutional Review Board.
Measures
Demographic information
Participants provided information regarding their age, gender, year in school, race/ethnicity, and fraternity/sorority affiliation.
Impulsivity
We used the 40-item version of the UPPS Impulsive Behavior Scale (Whiteside & Lynam, 2001) that has been validated with college students who drink alcohol (Magid & Colder, 2007). Participants rate their agreement with statements such as, “I like to stop and think things over before I do them,” on a scale from 0 (not at all) to four (very much). The four subscales of the UPPS include Urgency (10 items), Premeditation (10 items), Perseverance (8 items), and Sensation-Seeking (12 items). Individuals are characterized as high in impulsivity if they report high urgency and sensation-seeking scores and low premeditation and perseverance scores. These subscales demonstrated good internal consistencies in the current sample (α ranged from .81 to .86).
Sleep adequacy
Past-month subjective sleep adequacy was measured using the item, “How often do you think you get enough sleep?” (Wolfson & Carskadon, 1998). Participants also indicated the time they usually go to bed and wake up on weekdays and weekends. For descriptive purposes, responses to these items were used to calculate the average amount of sleep (across weekdays and weekends) that participants reported getting on a typical night in the past month. Subjective sleep adequacy, rather than average sleep time, was used as the predictor variable in regression models to account for wide variability in individuals’ sleep needs (Blunden & Galland, 2014; Carskadon & Short, 2014).
Alcohol use
Participants indicated the amount of alcohol they had consumed over the past month using the Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985). After being provided with standard drink definitions (12 oz. of beer, 5 oz. of 12% table wine, 12 oz. of wine cooler, or 1.25 oz. of 80-proof liquor), participants indicated how many standard drinks of beer, wine, and spirits they consumed on each day of a typical week in the past month. Responses were summed to calculate typical weekly drinking quantity (drinks per week). Participants also indicated how often in the past month they had engaged in heavy episodic drinking (4/5+ drinks on one occasion for women/men). These data are presented for descriptive purposes.
Alcohol-related consequences
Participants completed the Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler, Strong, & Read, (2005), which is a 24-item measure of alcohol-related consequences. Participants indicated (yes/no) if they had “felt very sick to my stomach or thrown up” or “woken up in an unexpected place” after drinking in the past month. Affirmative (yes) responses were summed to create the alcohol-related consequences outcome used in analyses. The BYAACQ has demonstrated strong psychometric properties (Kahler et al., 2005), and reliability in this sample was high (α = .84).
Data Screening & Analysis Plan
All analyses were conducted in SAS 9.4. Data were screened for missing values, outliers, normality, and multicollinearity prior to analysis. No imputation procedures were used for missing values. For count variables, outliers were trimmed at three times the interquartile range from the 75th percentile. After accounting for outliers in this way, skewness and kurtosis estimates were within the normal range. Based on previous research indicating that the impulsivity subscales measured in the UPPS may be significantly correlated (Coskunpinar et al., 2013; Kiselica et al., 2015), linear regression was used to test for multicollinearity between the UPPS subscales. Diagnostic statistics indicated high levels of tolerance (0.9) among subscales in the current sample, indicating that a substantial amount of variance in each UPPS subscale was unaccounted for by the other subscales.
Participants were categorized into ‘adequate’ or ‘inadequate’ sleep groups based on their responses to the sleep adequacy measure. A recent consensus statement issued by the American Academy of Sleep Medicine and the Sleep Research Society suggests that young adults need 8 to 9 hours of sleep per night (Watson et al., 2015). Collectively, participants reporting that they never or rarely get enough sleep averaged fewer than 8 hours of sleep per night (M = 7.84, SD = 1.10), while those reporting that they sometimes, usually, or always get enough sleep averaged greater than 8 hours of sleep per night (M = 8.38, SD = 0.97). Thus, participants were grouped as receiving ‘inadequate’ sleep if they reported never or rarely getting enough sleep and ‘adequate’ sleep if they reported sometimes, usually, or always getting enough sleep.
Hierarchical multiple regression analyses were used to test the hypothesized interactions between sleep group and impulsivity subscales on alcohol-related outcomes. Predictor variables were mean centered prior to regression analyses in order to aid in interpretation of interactions. In all models, participant age, gender, ethnicity, Greek status, average sleep time, and any UPPS subscale not already included in the analysis (Urgency, Premeditation, Perseverance, and/or Sensation-Seeking) were included as covariates; in the model predicting alcohol-related consequences, drinks per week was also included as a covariate (see Table 2). In the first model, interactions between sleep group and (a) sensation-seeking and (b) premeditation were modeled as simultaneous predictors of drinks per week. In the second model, the interaction between sleep group and urgency was modeled as a predictor of alcohol-related consequences. Each moderation analysis was conducted in two steps. First, sleep group and the UPPS subscale were regressed onto either drinks per week or alcohol-related consequences. Next, the interaction between sleep group and the UPPS subscale, as well as their respective main effects, were regressed onto the drinking outcome. Tests of simple slopes were conducted using procedures described by Aiken and colleagues (Aiken & West, 1991; Cohen, Cohen, West, & Aiken, 2003). High and low values were specified as one standard deviation above the mean and one standard deviation below the mean, respectively (see Table 1 for standard deviation values).
Table 2.
Main effects and interactions for drinking quantity and alcohol-related consequences.
| Drinks per Week | ||||||
| B | SE | β | t | p | Adj. R2 | |
| Step 1: Main Effects | .21 | |||||
| Age | 0.91 | 0.31 | .12 | 2.95 | .01 | |
| Female gender | −.4.82 | 0.80 | −.24 | −.5.99 | <.001 | |
| White race | 3.94 | 1.00 | .15 | 3.93 | <.001 | |
| Fraternity/sorority affiliation | 4.23 | 0.97 | .17 | 4.38 | <.001 | |
| Average sleep time | 0.25 | 0.36 | .03 | 0.69 | .49 | |
| Sensation-seeking | 0.09 | 0.04 | .09 | 2.09 | .04 | |
| Perseverance | 0.01 | 0.08 | .01 | 0.12 | .90 | |
| Urgency | 0.18 | 0.05 | .14 | 3.44 | <.001 | |
| Premeditation | −.0.22 | 0.06 | −.17 | −.3.83 | <.001 | |
| Sleep group | 0.29 | 0.93 | .01 | 0.31 | .76 | |
| Step 2: Interactions | .22 | |||||
| Sleep X Sensation-seeking | −.0.06 | 0.09 | −.06 | −.0.64 | .52 | |
| Sleep X Premeditation | −.0.25 | 0.12 | −.16 | −.2.05 | .04 | |
| Alcohol-Related Consequences | ||||||
| B | SE | β | t | p | Adj. R2 | |
| Step 1: Main Effects | .35 | |||||
| Age | −.0.02 | 0.13 | −.01 | −.0.17 | .87 | |
| Female gender | 1.57 | 0.35 | .17 | 4.51 | <.001 | |
| White race | −.0.54 | 0.43 | −.05 | −.1.27 | .20 | |
| Fraternity/sorority affiliation | 0.07 | 0.41 | .01 | 0.18 | .86 | |
| Average sleep time | −.0.13 | 0.15 | −.03 | −.0.85 | .40 | |
| Drinks per week | 0.21 | 0.02 | .45 | 11.2 | <.001 | |
| Sensation-seeking | 0.01 | 0.02 | .03 | 0.74 | .46 | |
| Perseverance | −.0.04 | 0.03 | −.05 | −.1.28 | .20 | |
| Urgency | 0.20 | 0.02 | .33 | 8.61 | <.001 | |
| Premeditation | 0.01 | 0.02 | .02 | 0.46 | .64 | |
| Sleep group | −.0.72 | 0.39 | −.07 | −.1.84 | .07 | |
| Step 2: Interactions | .35 | |||||
| Sleep X Urgency | −.0.07 | 0.05 | −.10 | −.1.37 | .17 | |
Table 1.
Descriptive statistics and zero-order correlations between variables (N = 568).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Female gender | -- | |||||||||||
| 2. | Age | −.05 | -- | ||||||||||
| 3. | White race | −.08 | .03 | -- | |||||||||
| 4. | Fraternity/sorority affiliation | −.04 | .03 | −.01 | -- | ||||||||
| 5. | Average sleep time | −.08 | −. 02 | −.01 | .05 | -- | |||||||
| 6. | Sleep adequacy | −.09 | .10 | .13 | −. 01 | .21 | -- | ||||||
| 7. | Urgency (UPPS) | −.03 | −.06 | −.01 | .01 | .05 | −.16 | -- | |||||
| 8. | Premeditation (UPPS) | .06 | −.05 | −.08 | −.03 | −.04 | .02 | −.23 | -- | ||||
| 9. | Perseverance (UPPS) | .08 | −.03 | .02 | −.08 | .08 | .13 | −.24 | .41 | -- | |||
| 10. | Sensation-seeking (UPPS) | −.13 | .07 | .10 | .01 | −.03 | .01 | .11 | −.12 | .25 | -- | ||
| 11. | Drinks per week | −.28 | .14 | .20 | .18 | .07 | .06 | .18 | −.24 | −. 11 | .18 | -- | |
| 12. | Alcohol-related consequences | .04 | .04 | .02 | .09 | .00 | −.14 | .42 | −.17 | −.17 | .08 | .43 | -- |
| N or mean | 40 | 19.2 | 475 | 94 | 8.27 | 2.2 | 12.6 | 23.12 | 20.9 | 29.6 | 12.5 | 5.4 | |
| % or SD | 71.7 | 1.2 | 83.6 | 16.5 | 1.02 | 0.9 | 9.3 | 7.0 | 5.5 | 7.0 | 9.2 | 4.3 |
Note. Bold print indicates p < .05. Bold italicized indicates p < .01. Bold italicized with underline indicates p < .001.
UPPS = UPPS Impulsive Behavior Scale.
Results
Descriptive Statistics
Descriptive statistics and zero-order correlations between variables are depicted in Table 1. Most participants reported ‘sometimes’ (38%) or ‘usually’ (37%) getting enough sleep in the past month, while fewer participants reported ‘never’ (2%), ‘rarely’ (18%), or ‘always’ (5%) getting enough sleep.2 Collectively, they reported moderate levels of sensation-seeking (M = 29.63, SD = 9.27, range = 0–48), premeditation (M = 23.12, SD = 6.95, range = 0–40), and perseverance (M = 20.91, SD = 5.48, range = 4–32) and relatively lower levels of urgency (M = 12.61, SD = 6.99, range = 0–34). On average, they reported consuming 12.49 (SD = 9.25) standard drinks over 2.42 (SD = 1.22) days in a typical week. The majority (88%) reported at least one (M = 4.16, SD = 3.77) heavy drinking episode in the past month. Zero-order correlations revealed significant positive associations between drinks consumed per week and (a) sensation-seeking and (b) urgency and significant negative associations between drinks consumed per week and (a) premeditation and (b) perseverance. Sleep adequacy was positively correlated with perseverance and negatively correlated with urgency and alcohol-related consequences; it was not significantly associated with other facets of impulsivity or drinks per week (see Table 1).
Main Effects
Complete data for all main effects and interactions are presented in Table 2. Higher sensation-seeking [B = .09, SE = .04, β = .09, t(529) = 2.09, p = .04], lower premeditation [B = −.22, SE = .06, β = −.17, t(529) = −3.83, p < .001], and higher urgency [B = .18, SE = .05, β = .14, t(529) = 3.44, p < .001] predicted more drinks per week. Perseverance [B = .01, SE = .08, β = .01, t(529) = .12, p = .90] and sleep group [B = .29, SE = .93, β = .01, t(529) = 0.31, p = .76] were not significantly associated with drinks per week.
In contrast to findings for drinks per week, higher urgency [B = 0.20, SE = .02, β = .33, t(528) = 8.61, p < .001] was the only significant predictor of alcohol-related consequences. Sleep group [B = −0.72, SE = .39, β = −.07, t(528) = −1.84, p = .07], sensation-seeking [B = 0.01, SE = .02, β = .03, t(528) = 0.74, p = .46], premeditation [B = 0.01, SE = .02, β = .02, t(528) = 0.46, p = .64], and perseverance [B = −0.04, SE = .03, β = −.05, t(528) = −1.28, p = .20] were not predictive of alcohol-related consequences.
Moderated Effects
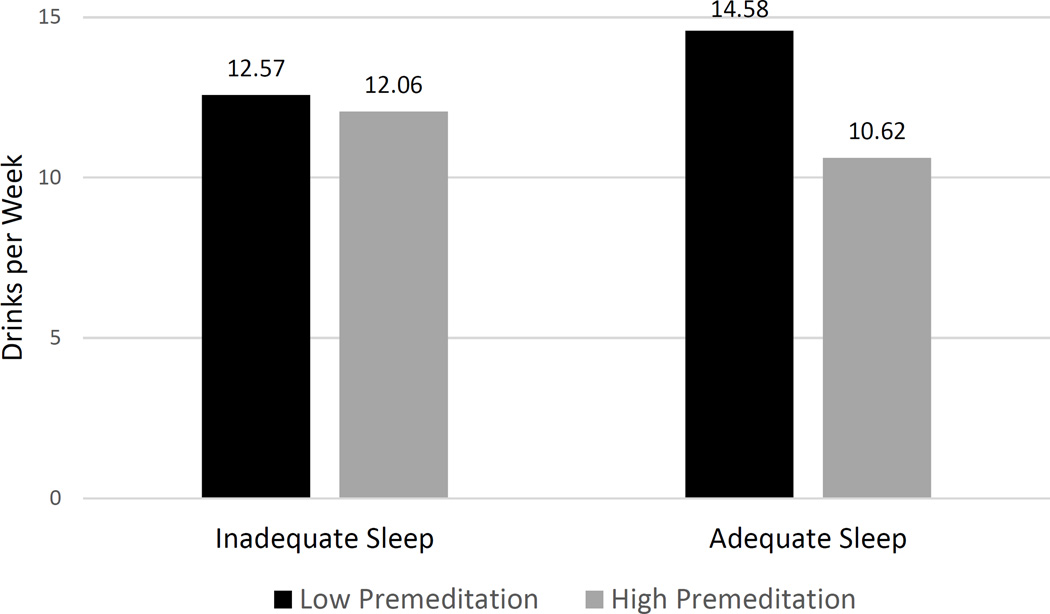
Analyses were conducted to determine if sleep group moderated (a) the effect of premeditation or sensation-seeking on drinks per week or (b) the effect of urgency on alcohol-related consequences. Tests of two-way interactions between sleep group and UPPS subscales revealed a significant interaction between sleep group and premeditation in the prediction of drinks per week [B = −0.25, SE = .12, β = −.16, t(529) = −2.05, p = .04]. Follow-up tests of simple slopes indicated that lower premeditation was associated with greater drinks per week among those in the adequate (B = −0.28, SE = .06, p < .001) but not the inadequate sleep group (B = .21, SE = .22, p = .34; see Figure 1). Sleep group did not significantly interact with sensation-seeking [B = −.06, SE = .09, β = −.06, t(529) = −0.64, p = .52] in the prediction of drinks per week. Similarly, there was not a significant interaction between sleep group and urgency [B = −.07, SE = .05, β = −.10, t(528) = −1.37, p = .17] in the prediction of alcohol-related consequences.
Figure 1.
Group differences in the premeditation by sleep group interaction on drinks per week.
Discussion
Published studies to date have not examined sleep as a moderator of the association between impulsive personality traits and alcohol use in young adults. In the current study, we replicated expected main effects of impulsivity on drinking outcomes and found partial support for our moderation hypothesis. Consistent with previous research (Kiselica et al., 2015), high sensation seeking, low premeditation, and high urgency predicted drinking quantity in this sample, and high urgency was the strongest predictor of alcohol-related consequences. Notably, sensation-seeking and urgency were associated with drinking and alcohol-related problems, respectively, independent of participants’ subjective experience of sleep adequacy; however, premeditation was associated with alcohol use only among those reporting adequate sleep.
In contrast to hypotheses, the association between premeditation and alcohol use was significant for those reporting adequate, rather than inadequate, sleep. Based on previous research (Schnyer et al., 2009), we expected inadequate sleep to exacerbate the association between low premeditation and alcohol use. Yet, among those reporting inadequate sleep, the tendency to think (or not think) carefully about one’s behaviors was not associated with alcohol use. For those reporting adequate sleep, however, the tendency to plan ahead and consider the consequences of one’s behaviors was associated with fewer drinks per week. For the UPPS facet of impulsivity defined as premeditation, the tendency to plan ahead may prevent an individual from drinking heavily because it prompts thoughtful consideration of the consequences of one’s behaviors (Magid & Colder, 2007). Our results suggest that these cognitive skills are only protective among individuals reporting adequate sleep; the ability to plan ahead no longer serves a protective function when one is sleep deprived.
Given that adequate sleep influenced drinking quantity only as a moderator of the association between premeditation and alcohol use (i.e., there was no main effect of sleep on drinking quantity), the mechanism by which adequate sleep exerts this effect is unclear. Both Cognitive-Motivational Theory (Finn, 2002) and dual process models (Wiers, Gladwin, Hofmann, Salemink, & Ridderinkhof, 2013) suggest that working memory capacity moderates the association between impulsive personality traits and behavioral regulation (in this case, alcohol use). Consistent with these models, the association between impulsivity and problematic alcohol use is strongest among those with poorer working memory capacity (Ellingson, Fleming, Verges, Bartholow, & Sher, 2014; Finn & Hall, 2004). Notably, sleep deprivation also has a negative impact on working memory capacity (Chee et al., 2006; Gohar et al., 2009). Thus, receiving adequate sleep may buffer the effects of poor working memory on alcohol use, leading to decreased alcohol use among those with the skills and cognitive resources necessary to consider the consequences of their drinking. Such findings would be consistent with the idea that sleep replenishes one’s capacity for self-control (Pilcher et al., 2015).
Adequate sleep did not impact the association between sensation-seeking and alcohol use in the current study, suggesting that sensation-seeking acts independently of sleep adequacy in its influence on drinking quantity. This is somewhat consistent with previous research, in which sensation-seeking and sleep exert independent effects on delinquent behavior (Peach & Gaultney, 2013). The differential effect of adequate sleep on premeditation and sensation-seeking is also consistent with research indicating a decoupling of the premeditation/planning and sensation-seeking facets of impulsivity (Smith et al., 2007). Recent research suggests that substance abuse treatment enhances planning but not necessarily sensation-seeking among those with substance use disorders (Littlefield et al., 2015). Thus, sensation-seeking may represent a risk factor that is both less influenced by sleep adequacy and less amenable to change.
Urgency also had an independent effect on alcohol-related outcomes that was unaffected by sleep adequacy, suggesting that individuals who tend to act rashly in response to strong negative emotions drink more and experience more alcohol-related consequences regardless of adequate sleep. This finding is consistent with literature indicating that difficulty identifying and tolerating negative emotions is associated with alcohol-related problems among young adults (Emery, Simons, Clarke, & Gaher, 2014; Kaiser, Milich, Lynam, & Charnigo, 2012). However, it seems to contradict evidence that sleep influences emotion regulation among adolescents and young adults (Baum et al., 2014; Tavernier & Willoughby, 2015). It is plausible that the protective effect of sleep on emotion regulation is predicated on the individual’s ability to regulate their emotions when rested; specifically, individuals who tend to respond rashly to emotions may not have the skills (or may have limited skills) to control those emotions, regardless of how much or how well they slept.
The results of this study have implications for clinical assessment as well as alcohol prevention and intervention among young adults. First, the majority of participants reported that they only sometimes get enough sleep to feel well-rested. Given the negative consequences associated with chronic sleep restriction (Watson et al., 2015), health care providers are encouraged to assess regularly for subjective perceptions of sleep among young adults and intervene when appropriate. Second, the tendency to consider the consequences of one’s behavior was associated with less alcohol use, but only if individuals were receiving adequate sleep. This suggests that assessment of sleep may be important in alcohol-related treatment planning. Finally, because the associations between (a) sensation-seeking and alcohol use and (b) urgency and alcohol-related consequences persisted in spite of adequate sleep, alcohol interventions may benefit from treatment components targeting impulsive decision-making (Morrison, Madden, Odum, Friedel, & Twohig, 2014). Similarly, individuals who tend to respond abruptly to intense emotions may benefit from skills training interventions that focus on emotion regulation.
Interpretation of these results must be considered in the context of several limitations. First, because data were collected as part of larger research trial on college student drinking, only a single item representing sleep adequacy was available for the present analysis; therefore, findings should be replicated using a reliable measure of subjective sleep quality. Second, we used self-report measures of sleep adequacy and alcohol use. However, young adults’ self-reported estimates of sleep patterns (Wolfson et al., 2003) and alcohol use (Leffingwell et al., 2013) correspond with objective measures of each behavior, so it is unlikely that objective measures of the same constructs would produce meaningfully different results. Third, because predictor and outcome variables for this study were measured concurrently, we are unable to determine causality in these associations. Finally, participants were recruited from one campus, were predominantly White underclassmen, and were mandated to participate in an alcohol intervention after violating campus alcohol policy. Future replication of our findings in more diverse samples and with more reliable assessment measures is necessary to confirm these results.
Conclusion
The link between sleep and impulsivity – and the impact of this association on alcohol use among young adults – is poorly understood. Current findings suggest that sensation-seeking and urgency are associated with greater alcohol involvement among young adults, regardless of sleep adequacy. However, adequate sleep seems to enable individuals who tend to plan ahead to moderate their drinking. The interactive effects of sleep and impulsive personality traits on alcohol involvement suggest that both may be appropriate targets for interventions designed to decrease high-risk drinking among young adults.
Acknowledgments
This research was supported by grant numbers R01-AA012518 (PI: Kate B. Carey) and T32-AA007459 (PI: Peter Monti) from the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health. NIH had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Lack of perseverance has also been associated with drinking quantity in a recent meta-analytic review (Coskunpinar, Dir, & Cyders, 2013); however, this association has not replicated in studies specifically using the UPPS Impulsive Behavior Scale (Kiselica et al., 2015; Lynam & Miller, 2004; Magid & Colder, 2007; Miller et al., 2003). Because we used the UPPS Impulsive Behavior Scale in this study, we did not hypothesize a strong association between perseverance and alcohol use.
Because the majority of participants (n = 451, 80%) were included in the ‘adequate’ sleep group, we also ran analyses using weighted means. The pattern and significance of results were unchanged; therefore, unweighted data and results are presented here.
References
- Acheson A, Richards JB, de Wit H. Effects of sleep deprivation on impulsive behaviors in men and women. Physiology & Behavior. 2007;91(5):579–587. doi: 10.1016/j.physbeh.2007.03.020. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- Anderson C, Platten CR. Sleep deprivation lowers inhibition and enhances impulsivity to negative stimuli. Behav Brain Res. 2011;217(2):463–466. doi: 10.1016/j.bbr.2010.09.020. [DOI] [PubMed] [Google Scholar]
- Ashenhurst JR, Harden KP, Corbin WR, Fromme K. Trajectories of binge drinking and personality change across emerging adulthood. Psychology of Addictive Behaviors. 2015 doi: 10.1037/adb0000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. Journal of Child Psychology and Psychiatry. 2014;55(2):180–190. doi: 10.1111/jcpp.12125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blunden S, Galland B. The complexities of defining optimal sleep: empirical and theoretical considerations with a special emphasis on children. Sleep Med Rev. 2014;18(5):371–378. doi: 10.1016/j.smrv.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Buysse DJ. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Walsh JL, Merrill JE, Lust SA, Kalichman SC, Carey MP. Using email boosters to maintain change after brief alcohol interventions for mandated college students: A randomized controlled trial. Manuscript in preparation. 2016 doi: 10.1037/ccp0000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Short MA. Measuring sleep need. Sleep Med Rev. 2014;18(5):369–370. doi: 10.1016/j.smrv.2014.06.007. [DOI] [PubMed] [Google Scholar]
- Chee MWL, Chuah LYM, Venkatraman V, Chan WY, Philip P, Dinges DF. Functional imaging of working memory following normal sleep and after 24 and 35h of sleep deprivation: Correlations of fronto-parietal activation with performance. NeuroImage. 2006;31:419–428. doi: 10.1016/j.neuroimage.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2003. [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research. 2013;37(9):1441–1450. doi: 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PTJ, McCrae RR. Revised NEO Personality Inventory Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- DeMartini KS, Carey KB. Correlates of AUDIT risk status for male and female college students. Journal of American College Health. 2009;58(3):233–239. doi: 10.1080/07448480903295342. [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Fucito LM. Variations in sleep characteristics and sleep-related impairment in at-risk college drinkers: A latent profile analysis. Health Psychology. 2014;33(10):1164–1173. doi: 10.1037/hea0000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Smith GT, Olausson P, Mitchell SH, Leeman RF, O'Malley SS, Sher K. Review: Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15(2):217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellingson JM, Fleming KA, Verges A, Bartholow BD, Sher KJ. Working memory as a moderator of impulsivity and alcohol involvement: Testing the cognitive-motivational theory of alcohol use with prospective and working memory updating data. Addictive Behaviors. 2014;39:1622–1631. doi: 10.1016/j.addbeh.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery NN, Simons JS, Clarke CJ, Gaher RM. Emotion differentiation and alcohol-related problems: The mediating role of urgency. Addictive Behaviors. 2014;39:1459–1463. doi: 10.1016/j.addbeh.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR. Motivation, working memory, and decision making: A cognitive-motivational theory of personality vulnerability to alcoholism. Behavioral and Cognitive Neuroscience Reviews. 2002;1(3):183–205. doi: 10.1177/1534582302001003001. [DOI] [PubMed] [Google Scholar]
- Finn PR, Hall J. Cognitive ability and risk for alcoholism: Short-term memory capacity and intelligence moderate personality risk for alcohol problems. Journal of Abnormal Psychology. 2004;113(4):569–581. doi: 10.1037/0021-843X.113.4.569. [DOI] [PubMed] [Google Scholar]
- Gohar A, Adams A, Gertner E, Sackett-Lundeen L, Heitz R, Engle R, Bijwadia J. Working memory capacity is decreased in sleep-deprived internal medicine residents. Journal of Clinical Sleep Medicine. 2009;5(3):191–197. [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Soehner AM, Clark DB. Sleep and circadian contributions to adolescent alcohol use disorder. Alcohol. 2015;49(4):377–387. doi: 10.1016/j.alcohol.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. Journal of Studies on Alcohol and Drugs. 2009;(Supp 16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2014: Volume 2, College students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2015. Retrieved from. [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward Efficient and Comprehensive Measurement of the Alcohol Problems Continuum in College Students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kaiser AJ, Milich R, Lynam DR, Charnigo RJ. Negative urgency, distress tolerance, and substance abuse among college students. Addictive Behaviors. 2012;37:1075–1083. doi: 10.1016/j.addbeh.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, LaBrie JW, Hummer JF, Pham AT. Global sleep quality as a moderator of alcohol consumption and consequences in college students. Addictive Behaviors. 2012;37(4):507–512. doi: 10.1016/j.addbeh.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Lac A, LaBrie JW, Hummer JF, Pham A. Mental health, sleep quality, drinking motives, and alcohol-related consequences: A path-analytic model. Journal of Studies on Alcohol and Drugs. 2013;74(6):841–851. doi: 10.15288/jsad.2013.74.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WDS. Effects of sleep deprivation and morningness-eveningness traits on risk-taking. Psychological Reports. 2007;100:613–626. doi: 10.2466/pr0.100.2.613-626. [DOI] [PubMed] [Google Scholar]
- Killgore WDS, Balkin TJ, Wsensten NJ. Impaired decision making following 49 h of sleep deprivation. Journal of Sleep Research. 2006;15(1):7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- Kiselica AM, Echevarria JM, Borders A. The relative contributions of impulsivity facets to drinking outcomes. Addictive Disorders & Their Treatment. 2015;14(3):152–158. [Google Scholar]
- Leffingwell TR, Cooney NJ, Murphy JG, Luczak S, Rosen G, Dougherty DM, Barnett NP. Continuous objective monitoring of alcohol use: twenty-first century measurement using transdermal sensors. Alcoholism: Clinical and Experimental Research. 2013;37(1):16–22. doi: 10.1111/j.1530-0277.2012.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, Steinley D. Developmental trajectories of impulsivity and their association with alcohol use and related outcomes during emerging and young adulthood I. Alcoholism: Clinical & Experimental Research. 2010;34(8):1409–1416. doi: 10.1111/j.1530-0277.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Stevens AK, Cunningham S, Jones RE, King KM, Schumacher JA, Coffey SF. Stability and change in multi-method measures of impulsivity across residential addictions treatment. Addictive Behaviors. 2015;42:126–129. doi: 10.1016/j.addbeh.2014.11.002. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Miller JD. Personality pathways to impulsive behavior and their relations to deviance: Results from three samples. Journal of Quantitative Criminology. 2004;20:319–341. [Google Scholar]
- Lynam DR, Smith GT, Cyders MA, Fischer S, Whiteside SA. The UPPS-S: A multidimensional measure of risk for impulsive behavior. 2007 Unpublished technical report. [Google Scholar]
- Magid V, Colder CR. The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43:1927–1937. [Google Scholar]
- Meldrum RC, Barnes JC, Hay C. Sleep deprivation, low self-control, and delinquency: a test of the strength model of self-control. J Youth Adolesc. 2015;44(2):465–477. doi: 10.1007/s10964-013-0024-4. [DOI] [PubMed] [Google Scholar]
- Miller JD, Flory K, Lynam D, Leukefeld C. A test of the four-factor model of impulsivity-related traits. Personality and Individual Differences. 2003;34(8):1403–1418. [Google Scholar]
- Morrison KL, Madden GJ, Odum AL, Friedel JE, Twohig MP. Altering impulsive decision-making with an acceptance-based procedure. Behavior Therapy. 2014;45:630–639. doi: 10.1016/j.beth.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy P, Garavan H. Cognitive predictors of problem drinking and AUDIT scores among college students. Drug and Alcohol Dependence. 2011;115:94–100. doi: 10.1016/j.drugalcdep.2010.10.011. [DOI] [PubMed] [Google Scholar]
- Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. Journal of Youth and Adolescence. 2012;41:1184–1196. doi: 10.1007/s10964-012-9784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peach HD, Gaultney JF. Sleep, impulse control, and sensation-seeking predict delinquent behavior in adolescents, emerging adults, and adults. Journal of Adolescent Health. 2013;53:293–299. doi: 10.1016/j.jadohealth.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Pieters S, Van Der Vorst H, Burk WJ, Wiers RW, Engels RCME. Puberty-dependent sleep regulation and alcohol use in early adolescents. Alcoholism: Clinical and Experimental Research. 2010;34(9):1512–1518. doi: 10.1111/j.1530-0277.2010.01235.x. [DOI] [PubMed] [Google Scholar]
- Pilcher JJ, Callan C, Posey JL. Sleep deprivation affects reactivity to positive but not negative stimuli. J Psychosom Res. 2015 doi: 10.1016/j.jpsychores.2015.05.003. [DOI] [PubMed] [Google Scholar]
- Schmidt RE, Gay P, Van der Linden M. Facets of impulsivity are differentially linked to insomnia: Evidence from an exploratory study. Behavioral Sleep Medicine. 2008;6:178–192. doi: 10.1080/15402000802162570. [DOI] [PubMed] [Google Scholar]
- Schnyer DM, Zeithamova D, Williams V. Decision-making under conditions of sleep deprivation: Cognitive and neural consequences. Military Psychology. 2009;21(Suppl 1):S36–S45. [Google Scholar]
- Sivertsen B, Skogen JC, Jakobsen R, Hysin M. Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug and Alcohol Dependence. 2015;149:180–186. doi: 10.1016/j.drugalcdep.2015.01.045. [DOI] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14(2):155–170. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- Tavernier R, Willoughby T. A longitudinal examination of the bidirectional association between sleep problems and social ties at university: the mediating role of emotion regulation. J Youth Adolesc. 2015;44(2):317–330. doi: 10.1007/s10964-014-0107-x. [DOI] [PubMed] [Google Scholar]
- Venkatraman V, Chuah YML, Huettel SA, Chee MWL. Sleep deprivation elevates expectation of gains and attenuates response to losses following risky decisions. Sleep: Journal of Sleep and Sleep Disorders Research. 2007;30(5):603–609. doi: 10.1093/sleep/30.5.603. [DOI] [PubMed] [Google Scholar]
- Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Tasali E. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Wiers RW, Gladwin TE, Hofmann W, Salemink E, Ridderinkhof KR. Cognitive bias modification and cognitive control training in addiction and related psychopathology: Mechanisms, clinical perspectives, and ways forward. Clinical Psychological Science. 2013;1(2):192–212. [Google Scholar]
- Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M. Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. doi: 10.1007/s10964-014-0170-3. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69(4):875–887. [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey for adolescents. Sleep: Journal of Sleep and Sleep Disorders Research. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism: Clinical and Experimental Research. 2004;28(4):578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use, and behavioral problems in adolescence. Sleep Medicine. 2009;10(7):787–796. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcoholism: Clinical and Experimental Research. 2015;39(2):355–362. doi: 10.1111/acer.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. Sensation seeking: Beyond the optimal level of arousal. Hillsdale, NJ: Erlbaum; 1979. [Google Scholar]