Abstract
Introduction:
EMMS International and Emmanuel Hospital Association (EHA) implemented a pilot project, poverty reduction in India through palliative care (PRIPCare). A total of 129 interviews with patients and family enrolled in palliative care at three EHA hospitals (in Fatehpur, Lalitpur and Utraula) and staff discussions established that 66% of palliative care patients had lost livelihoods due to illness, 26% of patients' families had members who had lost livelihoods due to the illness, 98% of enrolled households had debts, 59% had loans for which they had sold assets, 69% of households took out debt after their family member fell ill, many patients do not know about government benefits and lack necessary documents, many village headmen require bribes to give people access to benefits, and many bereaved women and children lose everything. Palliative care enabled 85% of patients and families to spend less on medicines, 31% of patients received free medicines, all patients reduced use of out-patient departments (OPDs), 20% reduced use of inpatient departments (IPDs), and therefore spent less on travel, 8% of patients had started earning again due to improved health, members of 10% of families started earning again, and one hospital educated 171 village headmen and increased by 5% the number of patients and their families receiving government benefits. If only 0.7% of needy adults are receiving palliative care, these benefits could be delivered to 143 times more families, targeted effectively at poverty reduction. Palliative care has great scope to reduce that most desperate poverty in India caused by chronic illness.
Context:
This article concerns a study by the UK NGO EMMS International and Indian NGO EHA, to assess whether palliative care reduces household poverty.
Aims:
EHA staff had noticed that many patients spend a lot on ineffective treatment before joining palliative care, many families do not know their entitlement to government healthcare subsidies or government pensions, and many bereaved widows and children are disinherited. Convinced that palliative care can address these, EMMS and EHA implemented PRIPCare – a pilot project.
Settings and Design:
EHA began training staff for rural palliative care in north India in 2009, and started its first palliative care service at Harriet Benson Memorial Hospital, Lalitpur, Uttar Pradesh, in 2010, with home-based care backed by hospital out- and in-patient care. With EMMS support since 2012, EHA's palliative care service functions in eight hospitals in six states and Delhi.
Subjects and Methods:
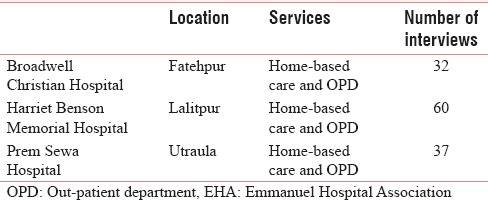
EMMS International provided the concept, commissioned the study and reviewed the report. EHA hired and guided a consultant, who piloted a questionnaire in EHA's Delhi Shalom Centre, and conducted 129 in-depth, one-to-one interviews in July and August 2015 with patients or close family members enrolled in the palliative care of three EHA rural hospitals, in Fatehpur, Lalitpur and Utraula. This represents 83% of patients in these hospitals, which in July 2015 was 79 patients in Lalitpur, 39 in Utraula, and 38 in Fatehpur. The questionnaire concerned illness, cost of treatment, use of government benefits, and family economic status. The consultant held focus group discussions with palliative care staff in these three hospitals.
Statistical Analysis:
An intern in EHA's Shalom Centre in Delhi entered data into Excel. The consultant analysed it using Excel.
Results:
Poverty of palliative care patients
18% of households enrolled for palliative care earn <Rs 5000/month
In 63% of households, the highest wage earner earns <Rs 5000/month
66% of palliative care patients had lost their livelihoods due to illness
26% of patients' families had members who had lost livelihoods due to the illness
Before palliative care, 80% of households paid for medicine, treatment, laboratory tests and travel to healthcare
98% of enrolled households have debts; 59% had sold assets to gain 0-interest loans
69% of households took out their debt after their family member fell ill
11% of enrolled households receive government benefits
49% of households have food cards or below poverty line cards
Many patients do not know their rights to government benefits
Many patients lack documents to enroll for government benefits
Many village headmen demand bribes to list people as eligible for benefits
Patients do not plan inheritance; many bereaved women and children lose everything.
Poverty reduction through palliative care
85% of patients and families spent less monthly on medicine and travel after joining palliative care than before, due to symptom management, cheaper medicine, and home-based care
31% of patients received free medicines on the palliative care programme
All patients reduced the use of OPDs after joining palliative care. 20% reduced use of IPDs. Both contributed to lower travel expenditure
8% of palliative care patients started earning again due to improved health
Members of 10% of families started work again through palliative care respite
Staff tell families of benefits to which they are entitled and how to get them
One hospital palliative care team educated 171 Pradhans and increased by 5% the proportion of palliative care patients and families who receive government benefits
Early diagnosis plus immediate enrollment on palliative care contributes to greater household poverty prevention and reduction, and greater dignity
Palliative care's awareness-raising has increased the number of patients enrolling on palliative care. Expanded services could enroll people earlier in their illness, since 59% of patients were diagnosed over 2 years ago, but only 19% of patients had been on the palliative care programme for 2 years
Reduced use of OPD and IPD free up regular hospital services for others.
In India, approximately 645,441 children on any 1 day need palliative care, but only 0.7% of them receive it (ICPCN, EMMS, 2015). If only 0.7% of needy adults are receiving palliative care, then the benefits above could be delivered to 143 times more families, if targeted effectively at poverty reduction.
Conclusions:
Holistic palliative care can reduce the desperate poverty driven by life-limiting illness, and can do so systematically, on a large-scale, in-depth, especially if started early in the illness. Home-based care also frees up hospitals to serve more patients with treatable conditions.
Keywords: Bereaved families, Government benefits, Inheritance, Palliative care, Poverty reduction
INTRODUCTION
India is 135th of 187 countries in human wellbeing.[1] Most rural households are poor.[2] Staff of eight Emmanuel Hospital Association (EHA) hospitals providing palliative care noticed that: many patients have spent a lot on ineffective treatment; many families do not know about government benefits; many patients and families cannot work; many bereaved people are disinherited. 6 million people annually need palliative care,[3] but fewer than 1% of these obtain it; 36 million household members annually are thereby impoverished. 0.7% of children needing palliative care receive it.[4] Poverty reduction in India through palliative care (PRIPCare) studied EHA's palliative care programme's effects on poverty.
SUBJECTS AND METHODS
A questionnaire was developed as follows:
Three palliative care teams and EHA and EMMS International staff discussed how palliative care can reduce household poverty
Doctors in EHA central office developed a questionnaire to capture these aspects of poverty reduction
A consultant piloted the questionnaire with Shalom Delhi patients and helped to modify the questionnaire.
The questionnaire was administered and data were collected in three hospitals in Uttar Pradesh, as shown in Table 1.
Table 1.
EHA hospitals
The consultant administered the questionnaire through in-depth interviews with patients and their family members, with their written consent. The consultant also conducted focus group discussions with staff members. An intern in EHA's Shalom Centre in Delhi entered data into Excel. The consultant analysed the data using Excel.
RESULTS
Indicators of poverty
Nearly 18% of households earn <Rs 5000/month. 39% of households have debts which they will find difficult to repay. In 63% of households, the highest wage earner earns <Rs 5000/month. Families with chronically sick members often have to cut their monthly expenditure on food items.
Nearly 63% of households earned their income from casual work or begging. 0.8% are drivers, 1.5% are teachers, 5% are farmers, 12% are retailers, and 18% are regular labourers.
17% were female-headed households, with no adult male aged 16–59
19% of households live in one-room kacha houses (mud houses)
11% of households receive government benefits
49% of households have food ration cards or below poverty line (BPL) cards
58% of households own land and 47% have buffaloes or cows. Households owned assets as shown in Graph 1.
Graph 1.
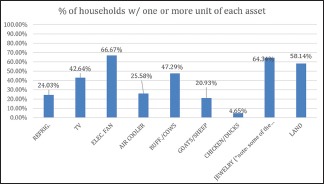
Household assets.
Costs associated with treatment before palliative care
Before joining palliative care, 71% of households had incurred costs of medicines, treatments and related laboratory costs, with monthly costs ranging from Rs 100 to Rs 500,000. 14% of households had spent between Rs 100,000 and Rs 500,000/month on medical costs. 18% of households had paid high costs of travel to healthcare, between Rs 5000 and Rs 50,000/month. Households had taken on debts or sold assets to meet these expenses: 39% of households had taken loans with interest, and 59% had taken loans without interest but had to sell assets to pay for this otherwise favourable loan. 69% of households had fallen into debt after their family member had fallen ill.
Time from diagnosis to enrolment in palliative care
59% of respondents had received their diagnosis over 2 years ago, as shown in Graph 2.
Graph 2.
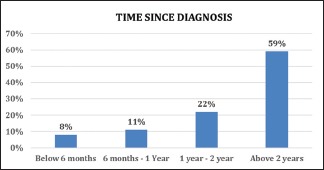
Time since diagnosis.
However, only 19% of respondents had joined palliative care over 2 years ago. From this, we deduce that many patients do not join a palliative care service soon after diagnosis, as shown in Graph 3.
Graph 3.
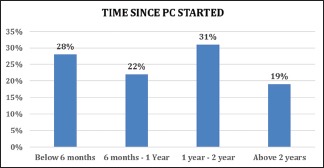
Time since palliative care started.
This is significant, because when patients enrol at a late stage, the palliative care team can deliver patient care, but time and the patient's health often do not permit a significant poverty reduction effect or a long time on the programme. Patients who have been on the palliative care programme for <6 months do not yet experience significant poverty reduction, while they stabilise their health, income, and expenditure. These patients are building up to poverty reduction, as their health improves, their family starts to experience respite, government benefits are sought, inheritance plans are made, and reduced expenditure on hospital visits and medicines starts to mean increased expenditure on paying off debts and improving nutrition. Patients who have been on the palliative care programme for between 6 months and 2 years receive the maximum benefit from the programme and the greatest poverty reduction for themselves and their families.
It is thus vital to enrol patients early in their illness. Ideally, patients are diagnosed early and are immediately enrolled on both treatment and palliative care, contributing to maximum health, dignity, and poverty prevention and reduction.
Key findings: The effects of palliative care on poverty in India
Inherent household poverty reduction in palliative care services
Palliative care's symptom management, provision of cheaper or free medicines and home-based care allowed 85% of patients and their families to spend less each month on medicines and travel to healthcare than before they joined the service
Palliative care's emphasis on home-based care means that patients and their families spent less on transport to hospital after than before enrolling for palliative care.
Household poverty reduction in holistic palliative care designed for India
In the three EHA programmes examined:
Awareness programmes are increasingly recruiting patients earlier than previously, thus increasing the poverty reduction effect on these families
Patients enrolling late are stabilised through donations of food
85% of households reduce expenditure on medicines, treatments and travel to healthcare after joining the home-based palliative care service [Figure 1]
31% of patients receive free medicines on the palliative care programme
More patients are aware of government benefit schemes to which they are entitled, and received help in enrolling
More government officials learned of the difficulty vulnerable people have in enrolling on government benefit schemes
More Pradhans granted palliative care patients and their families places on the list of BPL families, and in one hospital, 5% of patients were newly enrolled through the palliative care programme's interventions
Although 66% of patients had lost livelihoods due to illness, 8% of patients started earning again due to improvements in health through the palliative care service
Although 26% of families had members who had lost their source of livelihood, members of 10% of families started work again through palliative care support and respite
Palliative care staff are beginning to make themselves aware of inheritance laws and planning.
Figure 1.

Indian village.
Effects of palliative care on hospital services to its catchment population
Palliative care caused 36% of patients to reduce use of out-patient department (OPD) and 20% of patients to reduce use of in-patient department, and therefore allowed regular hospital services to provide their subsidised services to other vulnerable patients. (In fact, all patients reduced their use of OPD after joining the palliative care service, but not all reasons were directly attributable to the palliative care service; they included inability to afford OPD by this stage in their economic decline.)
What happens without access to holistic palliative care?
Families with low income succumb to poverty immediately when hit with a life-limiting illness like cancer. Without reliable advice, they do not know whether proposed fee-paying treatment may work, they may not be directed to the best value appropriate treatment which can be delivered simultaneously with palliative care, and they may be unaware that instead only palliative care is the best option. They are left with no savings, sell assets, and incur heavy debts
Due to late enrolment in the palliative care service, 39% of patient households have unpayable debts, and many cut their monthly expenditure on food
Patients believe many myths about their illness and its treatment
Many patients are unaware of government schemes to subsidize healthcare, such as Rashtriya Swasthya Bima Yojana and BPL cards
Many patients and families do not know about other government benefits such as widows', old age, and disability pensions. Patients have limited access to these benefits due to the lack of documentation
Village Pradhans often do not approve patients wishing to enrol for these benefits or undergoing their annual renewal of registration for them
Enrolments and renewals for government benefits are too cumbersome for these vulnerable patients and their families, who quickly lose heart, if not given help to enrol
Patients do not undertake inheritance planning, and their family, especially women and children, can lose everything since widows and daughters by custom do not inherit property from their husband or father.
Case study
Seema, aged 24 and injured since childhood, was given a sewing machine and regular dry rations through the palliative care programme. Team members then got her a tricycle from the social welfare department for commuting. Now Seema is an independent woman earning a decent livelihood for her mother and herself, through sewing. Recently, she was awarded a “pucca” house under a government housing scheme. Soon she will have a disability pension. The palliative care programme's multidisciplinary approach to networking reduced her poverty [Figure 2].
Figure 2.

Case study.
DISCUSSION AND CONCLUSION
Chronic illness causes poverty worldwide. In the USA, cancer is more prevalent among poor people.[5] The 2014 Global Atlas of Palliative Care at the End of Life finds that palliative care is cheaper for families and health-care services than alternatives.[6] Moreover, government expenditure on health is extremely inadequate in almost all low- and middle-income countries. Patients in these countries rely heavily on out-of-pocket financing for basic healthcare, resulting in a high prevalence of catastrophic payments and a large poverty impact of these payments.[7]
In India, where 1% of the population suffers from chronic or terminal illness, patients stop working, families prioritise care over income, and households increase expenditure on treatments and cures. As households fall into greater poverty, they sell assets, take out unsustainable debt, and the situation spirals out of their control. The poorest households are particularly affected, as their illiteracy and lack of influence make it most difficult for them to gain access to government benefits.
Palliative care in India has an inherent potential to reduce household poverty, including through reducing households' expenditure on medical care, assisting patients and their family members to receive government benefits, and enabling some family members and patients to work again. EHA's palliative care services are achieving these poverty reduction impacts even before EHA has developed them for poverty reduction. With the development and refinement of these services, more patients and family members could enrol in palliative care, and earlier. More households would spend less money on inappropriate treatments and hospital visits and medicines, would make these savings earlier, would enrol for all government benefits, would earn more again, would save more money over the course of the illness, and would organise inheritance to benefit women and girls. Severe illness devastates poor households' income and expenditure, driving them into hopeless poverty. Holistic palliative care has vast potential to limit all these effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Funded by EMMS International.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
EMMS International thanks Dr. Jane Bates for her pioneering work in developing the concept of palliative care for poverty reduction, which she is researching with EMMS in Malawi, in a project funded by the UK's Department for International Development and The True Colours Trust.
REFERENCES
- 1.UNDP. Human Development Report 2014, Sustaining Human Progress. 2014 [Google Scholar]
- 2.Indian Government, Socio-Economic and Caste Census Rural India. 2011 [Google Scholar]
- 3.Khosla D, Patel FD, Sharma SC. Palliative care in India: Current progress and future needs. Indian J Palliat Care. 2012;18:149–54. doi: 10.4103/0973-1075.105683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Children's Palliative Care Network, Assessment of Need for Children's Palliative Care in India and Globally. Edinburgh: Commissioned and Published by EMMS International; 2015. [Google Scholar]
- 5.Wilkes G, Freeman H, Prout M. Cancer and poverty: Breaking the cycle. Semin Oncol Nurs. 1994;10:79–88. doi: 10.1016/s0749-2081(05)80061-0. [DOI] [PubMed] [Google Scholar]
- 6.Global Atlas of Palliative Care at the End of Life. London: Worldwide Palliative Care Alliance; 2014. Worldwide Palliative Care Alliance. [Google Scholar]
- 7.Kumar SK. Kerala, India: A regional community-based palliative care model. J Pain Symptom Manage. 2007;33:623–7. doi: 10.1016/j.jpainsymman.2007.02.005. [DOI] [PubMed] [Google Scholar]


