Abstract
Background and Purpose
While there is limited evidence supporting the use of soft tissue mobilization techniques for Subacromial Pain Syndrome (SAPS), synonymous with subacromial impingement syndrome, previous studies have reported successful outcomes using soft tissue mobilization as a treatment technique. The purpose of this case report is to document the results of Instrument‐Assisted Soft Tissue Mobilization (IASTM) for the treatment of SAPS.
Case Description
Diagnosis was reached based on the subject's history, tenderness to palpation, and four out of five positive tests in the diagnostic cluster. Treatment consisted of three visits where the IASTM technique was applied to the pectoral muscles as well as periscapular musculature followed by retesting pain‐free shoulder flexion active range of motion (AROM) and Numerical Pain Rating Scale (NPRS) during active shoulder flexion. Scapulothoracic mobilization and stretching were performed after AROM measurement.
Outcomes
The subject reported an NPRS of 0/10 and demonstrated improvements in pain free flexion AROM in each of the three treatment sessions post‐IASTM: 85 ° to 181 °, 110 ° to 171 °, and 163 ° to 174 ° with some carryover in pain reduction and pain free AROM to the next treatment. Through three treatments, DASH score improved by 17.34%, Penn Shoulder Score improved 29%, worst NPRS decreased from 4/10 to 0/10, and a GROC score of 6.
Discussion
IASTM may have a beneficial acute effect on pain free shoulder flexion. In conjunction with scapulothoracic mobilizations and stretching, IASTM may improve function, decrease pain, and improve patient satisfaction. While this technique will not ameliorate the underlying pathomechanics contributing to SAPS, it may serve as a valuable tool to restore ROM and decrease pain allowing the patient to reap the full benefits of a multi‐modal treatment approach.
Level of Evidence
5
Keywords: instrument assisted soft tissue mobilization, shoulder complex, subacromial impingement syndrome, subacromial pain syndrome
BACKGROUND AND PURPOSE
Subacromial Pain Syndrome (SAPS), an improved nomenclature for what was previously categorized as Subacromial Impingement Syndrome (SIS), may account for as much as 30% of patients presenting with shoulder complex pain and dysfunction, rendering it the most prevalent of the shoulder diagnoses.1,2 Dierks et al define SAPS as “all non‐traumatic, usually unilateral, shoulder problems that cause pain, localized around the acromion, often worsening during or subsequent to lifting of the arm.”1(p. 1) Clinical diagnoses falling under this umbrella term include bursitis, tendinosis calcarea, supraspinatus tendinopathy, partial tear of the rotator cuff, biceps tendinitis, and tendon cuff degeneration.1 Common examination findings associated with SAPS include abnormalities with scapular kinematics and posterior glenohumeral (GH) joint capsule tightness; both of which may contribute to altered joint kinematics such as decreased upward rotation and posterior tilting of the scapula.3
The effects of manual therapy (MT) as an intervention for SAPS have previously been investigated and yielded primarily low to moderate evidence supporting its efficacy as a treatment.4 In a meta‐analysis, Desjardins‐Charbonneau et al. reported with low to moderate levels of evidence that MT alone or in conjunction with other modalities may have a clinically important reduction in a patient's pain.4 Their review looked almost entirely at the effects of GH joint mobilization as well as thrust and non‐thrust mobilization of the cervical and thoracic spine on pain and range of motion in the shoulder complex. There has been limited and indirect research into the effects of soft tissue mobilization (STM) or Instrument Assisted STM (IASTM) as a primary treatment for SAPS, but these interventions have the potential to provide beneficial acute effects on pain, function, and patient satisfaction.5-8
Low levels of evidence support STM as a successful intervention for reducing pain5 and increasing range of motion (ROM) in the shoulder complex.6 Al Dajah et al demonstrated success in reducing pain, increasing GH external rotation at 45 º abduction, and overhead reach ROM with STM applied to the subscapuaris.5 Laudner et al used IASTM applied to the posterior cuff musculature of healthy college‐aged baseball players to significantly increase GH internal rotation and horizontal adduction ROM in one treatment.6 Tightness of the posterior cuff has been found to alter scapular kinematics and contribute to the cause of SAPS by displacing the scapula laterally.3 Surenkok et al experimented with the acute effects of scapulothoracic joint mobilizations and found improvements in shoulder ROM and scapular upward rotation.7 The authors of this study suggest that because the scapulothoracic joint is not a synovial joint but bound by muscle, that this intervention is successful in the dissolution of adhesions, realigning collagen, and increasing fiber glide.7 It is hypothesized that SAPS presenting with decreased upward scapular rotation without limitations in GH joint mobility, may be the result of soft tissue restrictions.3
Under the theory that IASTM has the ability to reduce scar tissue related restrictions, break up adhesions, and improve mobility,6,9-10 the intervention was applied to the pectoral, latissimus dorsi, peri‐scapular, and posterior cuff muscles. To further mobilize the soft tissue potentially restricting scapular movement, ST joint mobilizations were performed with the intention to increase ROM and improve function of the tissues stabilizing the ST joint.7 By extrapolating the findings from previous research studies,5-10 it is hypothesized that the proposed intervention will assist in normalizing scapulohumeral mobility and allow for the completion of therapeutic exercises to address the imbalances associated with SAPS. The purpose of this case report is to document the results of IASTM for the treatment of SAPS.
CASE DESCRIPTION: PATIENT HISTORY AND SYSTEMS REVIEW
A right hand dominant, 20 year‐old, male recreational weightlifter and barber by profession was referred to physical therapy by his primary care physician with a diagnosis of bilateral “sprain of the rotator cuff capsule”. The complaint originated about two weeks prior to his initial physical therapy (PT) evaluation with an onset of pain in bilateral shoulders approximately six hours after completing a shoulder workout targeting hypertrophy of the deltoid musculature. The subject reported introducing a new variation of the dumbbell lateral shoulder raise utilizing a range of 0 ° to about 110 ° abduction to his routine. The subject's symptoms in the right shoulder subsided within a few days of the initial irritation, but the left shoulder symptoms increased over the course of the following two weeks. The subject ceased all upper body weightlifting except for training biceps and triceps in a neutral shoulder position as advised by his primary care physician. He had no complaints of pain while carrying out his job related tasks as a barber. The subject denied the use of any medications at the time of the examination and was in good health as verified by his physician during his annual physical one week earlier.
At the time of PT evaluation, the subject denied any numbness, tingling, or burning sensations. He reported perceived weakness in elevating the left shoulder above 90 ° due to pain. Pain with shoulder elevation was reported as a 4/10 on the Numeric Pain Rating Scale (NPRS) (ICC=.63).11 Pain in a neutral shoulder position at rest was reported as 0/10 on the NPRS. The subject described any pressing motion, such as performed during the flat or incline bench press, or overhead exercises as the most provocative movements, but he also experienced symptoms with reaching overhead and putting on a shirt. He stated, “I am not able to bring my left hand up to my hair.” The subject's goals were to eliminate pain with weight lifting and overhead activities.
CLINICAL IMPRESSION #1
The subject experienced an insidious onset of shoulder pain after performing repetitions of shoulder abduction with a heavy load above 90 º. Differential diagnosis consisted of a deltoid strain, rotator cuff strain, rotator cuff tear, cervical radiculopathy and SAPS. Due to his style of weight training as well as profession of barbering, the likelihood of underlying muscle imbalances, postural faults, and flexibility impairments were probable. These suspected impairments led the authors in the direction of SAPS as the manifestation of the underlying deficits as well as rendering the subject a good candidate for treatments addressing soft tissue abnormalities.3 The examination included ruling out cervical radiculopathy as a possible cause followed by strength, flexibility, palpation, and special testing of the shoulder complex to further isolate the underlying causes as well as movement‐based diagnosis.
EXAMINATION
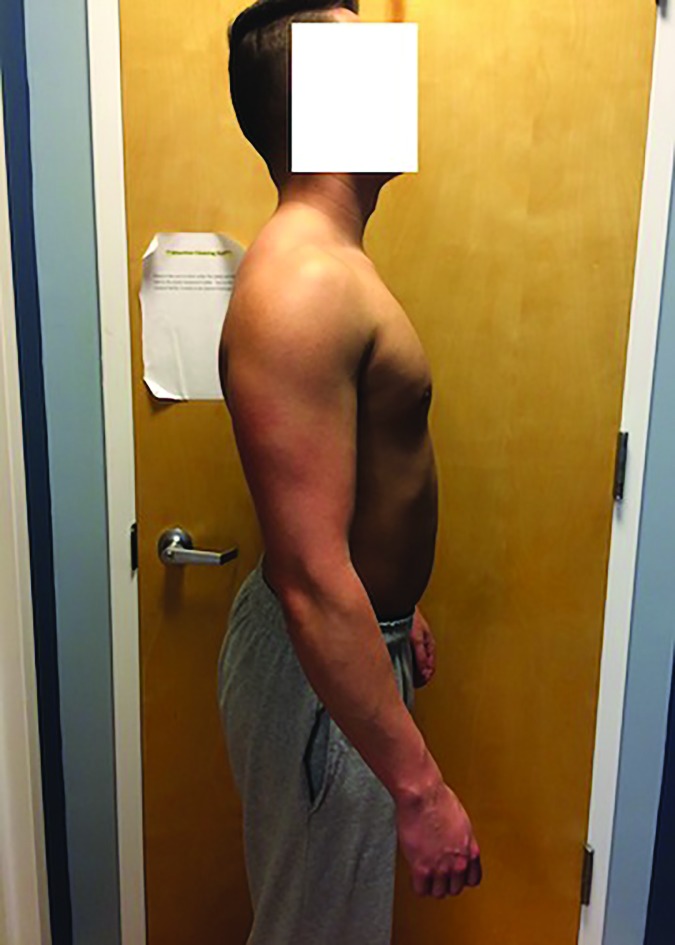
Observation of body structure and posture revealed forward shoulder posture, under‐developed left periscapular musculature compared to the right, elevated right shoulder compared to left, and an anterior pelvic tilt (Figures 1‐2). Cervical spine screening was unremarkable and provided no recreation of symptoms. Examination of the thoracic spine revealed hypomobility and tenderness with passive accessory intervertebral movements12-13 of the T1‐T7 vertebrae (κ=.13‐.82).13 Palpation of the left supraspinatus tendon insertion at the greater tubercle elicited pain consistent with the subject's symptoms. Inspection of the left upper trapezius displayed increased tone with concurrent scapular elevation. Active Range of Motion (AROM)14 testing recreated painful symptoms at 85 º left shoulder flexion although the subject was able to continue into 172 º flexion before initiating lumbar and lower thoracic lordotic compensation. Complete ROM testing results are listed in Table 1.
Figure 1.
Coronal View of Posture
Figure 2.
Posterior View of Posture
Table 1.
Shoulder Complex Range of Motion testing
| Movements | Ranges of Motion (Degrees) | |
|---|---|---|
| Right | Left | |
| Flexion | A=177 | A=172 |
| P=179 restricted by muscular endfeel |
P=178 restricted by muscular endfeel |
|
| Abduction | A=168 | A=180 |
| P=182 restricted by muscular endfeel |
P=189 normal muscular end feel |
|
| Apley's Scratch External Rotation | A=T2 | A=T3 |
| Apley's Scratch Internal Rotation | A = T8 | A = T4 |
| External rotation at 45 degrees abduction | P = 90 normal capsular endfeel |
P=97 normal capsular endfeel |
| Internal rotation at 45 degrees abduction | P=98 normal capsular endfeel |
P = 85 restricted by muscular endfeel |
A=AROM
P=PROM
Observation of scapulohumeral kinematics during shoulder flexion and abduction revealed movement system diagnoses of decreased upward rotation and posterior tilting of the scapula when compared to the asymptomatic side. Passive GH joint mobility testing exposed a restriction of the left posterior capsule and a slight restriction of the left inferior capsule. Passive flexion ROM of the shoulder complex was similar bilaterally and both exhibited a muscular end‐feel with overpressure. The subject demonstrated 5/5 and pain free manual muscle tests with gross muscle tests of the all shoulder musculature bilaterally except for experiencing pain during resisted external rotation of the left shoulder. All manual muscle testing was performed in the seated position as described by Kendall.15
Out of all special testing performed, as listed in Table 2, the subject tested positive for four out of five tests in the SIS cluster described by Michener et al (SN=.75, LR+=2.93).16 The subject tested positive for pectoral and latissimus tightness bilaterally.12 The scapular dyskinesis test (κw=.48‐.61)16 was performed with a 2.3 kg weight as described by McClure et al.17 Frontal plane assessment from the posterior showed no winging or aberrant movements but did reveal a decrease in upward rotation of the left scapula compared to the right.
Table 2.
Summary of Special Testing results for the shoulders
| Tests | R | L |
|---|---|---|
| Scapular Dyskinesia test with 3 lbs dumbbell17 | (‐) | (‐) decreased upward rotation |
| Hawkins/Kennedy sn=.6316 sp=.6316 |
(‐) | (+) |
| Neer test sn=.8116 sp=.5416 |
(‐) | (+) |
| Resisted external rotation Sn=.5616 Sp=.8716 |
(‐) | (+) |
| Empty can (Jobe) Sn=.5016 Sp=.8716 |
(‐) | (‐) |
| Painful Arc Sn=.7516 Sp = .6716 |
(‐) | (+) |
| Drop arm | (‐) | (‐) |
| Speed's Test sn = .38‐.6929 sp=.56‐.8329 |
(‐) | (‐) |
The subject completed the Disabilities of Arm, Shoulder, and Hand (DASH) questionnaire (ICC=.9)18 and the Penn Shoulder Score (PSS)(ICC=.94)19 outcome measures on the initial visit in order to track disability, limitations in sports activity, and patient satisfaction. These outcomes were chosen due to their established validity and known Minimal Clinically Important Difference (MCID) values.18-19 The subject scored a 19/100 on the DASH, 0/100 on the DASH work module, and a 100/100 on the DASH sports module. For the PSS, the subject scored 20/30 for pain (ICC=.88)19, 1/10 for satisfaction (ICC=.93)19, and 45/60 for function (ICC=.93)19 adding to a total score of 66/100 with 100 indicating high function, low pain, and high satisfaction with the function of the shoulder.19
CLINICAL IMPRESSION #2
After completing the physical examination, the subject's signs, symptoms, and movement system impairments were deemed consistent with SAPS. Several noteworthy findings included: decreased scapular upward rotation during shoulder elevation, tightness of the posterior GH joint capsule, forward shoulder posture, and decreased left periscapular muscle development compared to the right. These findings led to the hypothesis that the subject would benefit from IASTM and scapular mobilizations to address the movement system dysfunction of shoulder complex. Successful outcomes were considered as improved mobility without pain as well as improved PSS, DASH, Global Ratings of Change Scale (GROC), and NPRS scores.
INTERVENTION AND OUTCOMES
It has been proposed that IASTM instruments can be used as a diagnostic tool for identifying adhesions and abnormalities in tissues via changes in frequency of vibrations transmitted through the tool to the clinician.6,9,10,20 Silbaugh investigated the inter‐rater reliability of IASTM for detecting myofascial adhesions and reported a kappa coefficient of .344, suggesting low to moderate reliability.20 By utilizing the IASTM instrument over the respective muscle groups, soft tissue adhesions were detected by a change in the fluidity of the stroke of the IASTM instrument. Areas with a higher concentration of adhesions were identified by the sensation of traversing a roughened surface with the instrument, whereas tissue with fewer soft tissue restrictions allowed for a smoother glide of the tool against the subject's skin.
The subject was treated with IASTM, using the Edge Mobility Tool (The Edge Mobility System, Buffalo, NY), applied to the pectoral muscles and medial brachium with the subject in supine and the GH joint placed in 120 º abduction to place adequate tension on the selected tissues in the style of pectoral tightness test (Figure 3).12 The IASTM technique was performed for 20 seconds parallel to the muscle fibers followed by 20 seconds perpendicular to the muscle fibers with the instrument held at a 45 º angle to the skin.6 The Edge Mobility Tool was used beveled side contacting the skin. Pressure was applied lightly at first with a gradual increase due to the subject's initial sensitivity to the treatment. Pressure was increased with subject tolerance to maximal force due to evidence that heavy pressure elicits greater fibroblast proliferation than light or moderate pressure.21 The same IASTM protocol of 20 seconds parallel to the muscle fibers and 20 seconds perpendicular to the muscle fibers was applied to the posterior cuff musculature of the GH joint with the subject in prone and arms in 90 º abduction and internal rotation draped over the side of the plinth (Figure 4). While in the same position, the technique was applied to the periscapular musculature including the, trapezius, rhomboids, teres minor, teres major, and latissimus dorsi. (Figure 5)
Figure 3.
Supine positioning for IASTM to Pectoral Musculature
Figure 4.
Prone positioning for IASTM to the Posterior Cuff of the Shoulder
Figure 5.
Prone Positioning for IASTM to periscapular musculature
Post‐treatment measures included NPRS and pain free standing flexion AROM measured in degrees. Immediately following the intervention, the subject was instructed to stand and perform three repetitions of shoulder flexion and abduction. The subject reported 0/10 pain on the NPRS scale with both motions and 181 º pain free flexion AROM. The subject had no complaints of pain at end range flexion or abduction.
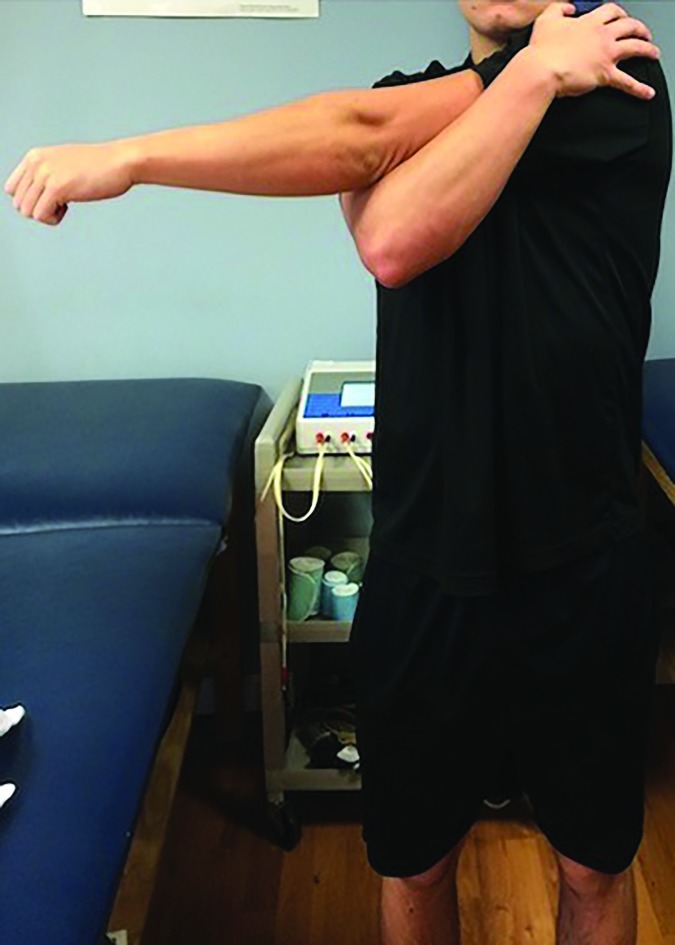
To further encourage proper scapulohumeral rhythm, 10 repetitions of grade III scapular mobilization were performed in all directions: superior, inferior, upward rotation, downward rotation, and distraction.3,7 Following scapular mobilization, 10 repetitions of manual resisted exercise from neutral to full flexion and back to neutral were performed to encourage muscle activation in the newly gained range of motion. Lastly, the subject was then given a cross body posterior capsule stretch (Figure 6)17 as well as a corner pectoral stretch (Figure 7)17 for three reptitions of 60 seconds22 for each exercise with the theory of introducing stretching to further improve tissue extensibility after targeting adhesions with IASTM and mobilizations.23 Upon completing these stretches, the subject was sent home with a home exercise plan consisting of these two stretches and instructed to do each stretch once a day for 3 repetitions of 60 seconds with the goal of maintaining the newly gained pain free ROM.
Figure 6.
Corner Pectoral Stretch
Figure 7.
Cross‐body Posterior Cuff Stretch
The subject returned to the clinic at three and five days post initial treatment. Upon arrival the subject completed the DASH, PSS, Global Rating of Change (GROC), and was tested for pain free flexion AROM as well as NPRS with shoulder flexion. The subject was then treated with the identical treatment protocol to the initial treatment consisting of IASTM, ST mobilizations, MRE's, and stretching. Pain free shoulder flexion AROM, as well as NPRS with shoulder flexion was measured after the IASTM treatment. The subject showed carryover improvement in pain free range of motion improving from 85 º at initial evaluation to 110 º at the beginning of the second treatment, then to 171 º upon arrival for the third session. After each IASTM treatment, the subject reported 0/10 NPRS and the perception of improved mobility as well as improvements in measured pain free flexion ROM. The subjects DASH score improved 17.34% as well as improving PSS score by 29 points, surpassing MCID's of 10.2% and 11.4 points respectively 18-19 (all outcomes are listed in Table 3). Improvements on the PSS indicate improved function, decreased pain, and improved satisfaction.19 After this treatment using manual therapy, the subject was prescribed a therapeutic exercise protocol consisting of progressive resisted exercises and neuromuscular re‐education of the scapular stabilizing musculature.24-25 The subject was educated on proper lifting mechanics and posture to return to a modified weight‐training program designed to not exacerbate symptoms.
Table 3.
Outcome Measurements
| Initial Visit | Post‐IASTM intervention | Treatment 2 3‐day post initial visit | Post‐IASTM Intervention | Treatment 3 5‐day post initial visit | Post‐IASTM Intervention | |
|---|---|---|---|---|---|---|
| DASH MCID = 1017 |
19/100 | NA | 23/100 | NA | 1.7/100‡ | NA |
| DASH Work Module |
0/100 | NA | 0/100 | NA | 0/100 | NA |
| DASH Sports Module |
100/100 | NA | 87.5/100 | NA | 50/100 | NA |
| Penn Shoulder Score MCID = 11.418 |
66/100 | NA | 72/100 | NA | 95/100‡ | NA |
| Pain | 20/30 | NA | 24/30 | NA | 30/30 | NA |
| Satisfaction | 1/10 | NA | 2/10 | NA | 5/10 | NA |
| Function | 45/60 | NA | 46/60 | NA | 60/60 | NA |
| Pain Free Shoulder Flexion AROM (°) |
85 | 181 | 110 | 171 | 163 | 174 |
| NPRS with Shoulder Flexion28 |
4/10 | 0/10* | 2/10 | 0/10‡ | 0/10 | 0/10 |
| GROC | NA | Not Measured | 1 | Not Measured | 6 | Not Measured |
;met MCID
IASTM‐ Instrument Assisted Soft Tissue Mobilization
DASH‐ Disabilities of the Arm, Shoulder, and Hand questionnaire; Lower score indicates less disability
MCID‐ Minimal Clinically Important Difference
AROM‐ Active Range of Motion
NPRS‐ Numeric Pain Rating Scale
GROC‐ Global Ratings of Change scale
Penn Shoulder Score: High score indicates improved function
NA: Not Applicable
DISCUSSION
This case report describes the use of IASTM to augment the effects of scapular mobilization on SAPS. To date, much of the literature looking at manual therapy intervention for SAPS addresses the spine and GH joint itself, but minimal research has been carried out on the effects of soft tissue mobilizing of the surrounding structures.4-5,7,25-27 Patients with SAPS typically present with soft tissue restrictions limiting the mobility of the scapula.3 These restrictions may manifest in movement system dysfunction, or may be secondary to a learned misuse due to pain. Surenkok et al. looked at the acute effects of ST mobilization on shoulder ROM, scapular upward rotation, and Constant Shoulder Score.7 This study inspired the hypothesis that IASTM can supplement or even improve the effects of ST mobilization. Since the scapula is surrounded by soft tissue structures the mobilization may assist in increasing the extensibility of these tissues limiting motion.6 Laudner et al used IASTM to improve internal rotation and horizontal abduction ROM in college baseball players with the hypothesis that instruments are able to detect and effectively treat abnormalities in the soft tissue on a deeper level than the hands are capable of doing.6 Applying this same brief treatment to the muscles that surround the ST joint should have some of the same effects that are hypothesized with the proven STM. In a case report, Slaven and Mathers used ASTYM® technique, another form of IASTM in conjunction with thrust and non‐thrust joint mobilization techniques in the management of chronic ankle pain following a traumatic inversion ankle sprain.9 Their findings showed immediate increases in ankle mobility following the use of ASTYM treatment using the theory that the instrument assists in re‐aligning pathologically disorganized soft tissues back to their normal state.9 Sevier and Stegink‐Jansen also investigated the use of ASTYM for its effectiveness in treating lateral epicondyalgia vs. eccentric exercise.10 They found that subjects treated with ASTYM reported improved DASH scores and improved grip strength significantly compared to the improvements observed with eccentric exercise.10 It was hypothesized that this form of IASTM may regenerate and remodel soft tissues by creating a localized inflammatory response releasing cellular mediators and growth factors.9-10,20 Further research is needed to examine these claims. Regardless of hypothesized method of changes at the cellular level, the aforementioned studies have indicated acute and gradual benefits in soft tissue extensibility and normalization.2,9-10
IASTM alone proved to show immediate effects in pain free shoulder flexion AROM as shown in the pre‐ to post‐ intervention measures in Table 3. IASTM may reduce any soft tissue adhesions limiting scapular upward rotation, thus allowing greater shoulder complex range of motion without pain in the subacromial space. Pain free flexion AROM is a valuable measure for SAPS due to accounting for the subject's subjective input of where their pain begins on the spectrum of a validated objective measure of AROM. Improvements in pain free shoulder flexion and NPRS combined with improvements in other subjective outcome measures such as the PSS, DASH, and GROC can help deduce patient perceived improvement in function and ability. While the subject did show an increase in DASH score from the initial evaluation to the second visit, the change does not meet the MCID of 10.2. From the second to third visit, the subject improved by 24.34 points surpassing the MCID.
The subject in this case had signs of mild scapular dyskinesia, which leads the authors to believe the causation of his symptoms was decreased scapular mobility due to soft tissue restrictions and not due to weakness of his scapular upward rotators. In cases where a patient has deficits in scapular stabilization strength and motor control, manual therapy intervention including this protocol of IASTM and ST mobilizations, can possibly be an effective precursor to proven therapeutic exercise/neuromuscular re‐education.24 Once proper mobility has been restored, it is expected that the patient will have an improved ability to perform exercises with proper mechanics. Without proper strength and neuromuscular control, the pure ability of the passive scapular mechanics may not transfer over to active movements.Marzetti et al looked at neurocognitive therapeutic exercise (NCTE) compared to traditional therapeutic exercise as treatment for SAPS.28 While both groups improved, the NCTE group showed greater improvements in DASH scores with results maintained over a 24‐week follow‐up period.28 In cases where soft tissue restrictions persists along with scapular dyskinesis a plan of care using IASTM followed by a NCTE protocol may be beneficial. SAPS typically has multiple impairments causing the end result of subacromial pain.3 The treatment of this syndrome could potentially benefit from interventions aimed at the underlying soft tissue, structural, and neuromuscular impairments to insure positive patient outcomes on a case‐by‐case basis. Soft tissue restriction can be a major impairment that can impede proper mechanics and hinder the patient's full potential in rehabilitation. Further investigation of using this IASTM intervention to enhance the effects of exercise is needed.
A number of limitations exist within this case report. While the subject did exhibit improvements under the afformentioned IASTM protocol, it is not possible to determine that the intervention solely was responsible for the patient's decrease in symptoms using case report methodology. The potential mechanisms of IASTM are discussed in this paper, but the possibility for neurologic, physiologic, and psychological contributory mechanisms were not taken into consideration. Further research into the mechanisms behind IASTM impacting multiple body systems is needed. Also, this case does not establish the long‐term impact of IASTM on SAPS. Further research is needed into the extent of the effects IASTM may exhibit on SAPS patients.
CONCLUSION
When combined with ST mobilizations and stretching, IASTM may be effective in acutely improving pain free flexion ROM, decreasing disability, improving function, decreasing pain, and improving patient satisfaction. While IASTM will not ameliorate all underlying pathomechanics contributing to SAPS, it may serve as a valuable tool to restore ROM and acutely decrease pain, thereby allowing the patient to reap the full benefits of a multi‐modal treatment approach.
REFERENCES
- 1.Diercks R Bron C Dorrestijn O, et al. Guideline for diagnosis and treatment of subacromial pain syndrome A multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthopaedica. 2014;85(3):314‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van der Windt D Koes B Boeke A Devillé W, et al. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract. 1996;46(410):519‐523. [PMC free article] [PubMed] [Google Scholar]
- 3.Ludewig PM Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desjardins‐Charbonneau A Roy J‐S Dionne CE, et al. The Efficacy of Manual Therapy for Rotator Cuff Tendinopathy: A Systematic Review and Meta‐analysis. J Orthop Sport Phys Ther. 2015;45(5):330‐50. [DOI] [PubMed] [Google Scholar]
- 5.Al Dajah SB. Soft tissue mobilization and PNF improve range of motion and minimize pain level in shoulder impingement. J Phys Ther Sci. 2014;26(11):1803‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laudner K Compton BD McLoda TA, et al. Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. Int J Sports Phys Ther. 2014;9(1):1‐7. [PMC free article] [PubMed] [Google Scholar]
- 7.Surenkok O Aytar A Baltaci G. Acute effects of scapular mobilization in shoulder dysfunction: a double‐blind randomized placebo‐controlled trial. J Sport Rehabil. 2009;18(4):493‐501. [DOI] [PubMed] [Google Scholar]
- 8.Harshbarger ND Eppelheimer BL Valovich McLeod TC, et al. The effectiveness of shoulder stretching and joint mobilizations on posterior shoulder tightness. J Sport Rehabil. 2013;22(4):313‐9. [DOI] [PubMed] [Google Scholar]
- 9.Slaven EJ Mathers J. Management of chronic ankle pain using joint mobilization and ASTYM® treatment: a case report. J Man Manip Ther. 2011;19(2):108‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sevier TL Stegink‐Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: A randomized controlled clinical trial. PeerJ [Internet]. 2015. [Cited May 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spadoni GF Stratford PW Solomon PE, et al. The evaluation of change in pain intensity: a comparison of the P4 and single‐item numeric pain rating scales. J Orthop Sports Phys Ther. 2004;34(4):187‐93. [DOI] [PubMed] [Google Scholar]
- 12.Magee DJ. Orthopedic Physical Assessment. St. Louis, MO: Saunders Elsevier; 2008: 318‐20, 503‐5. [Google Scholar]
- 13.Childs JD Cleland JA Elliott JM, et al. Neck Pain. J Orthop Sport Phys Ther. 2008;38(9):A1‐34. [DOI] [PubMed] [Google Scholar]
- 14.Norkin CC White DJ. Measurement Of Joint Motion: a Guide to Goniometry. Philadelphia: F.A. Davis; 1995: 57‐89. [Google Scholar]
- 15.Kendall FP McCreary EK Provance, et al. Muscles Testing And Function With Posture And Pain. 5th ed. Baltimore: Lippincott Williams and Wilkins; 2005. P. 314‐33. [Google Scholar]
- 16.Michener LA Walsworth MK Doukas WC, et al. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90(11):1898‐903. [DOI] [PubMed] [Google Scholar]
- 17.Tate AR McClure P Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 2: Validity. J Athl Train. 2009;44(2):165‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roy JS Macdermid JC Woodhouse LJ. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Care Res. 2009;61(5):623‐32. [DOI] [PubMed] [Google Scholar]
- 19.Leggin BG Michener LA Shaffer MA, et al. The Penn Shoulder Score: Reliability and Validity. J Orthop Sport Phys Ther. 2006;36:138‐51. [DOI] [PubMed] [Google Scholar]
- 20.Silbaugh K. Validity of Instrument Assisted Soft Tissue Mobilization for Detecting Myofascial Adhesions through Secondary Diagnostic Ultrasound Analysis [thesis]. Terre Haute, Indiana: Indiana State University; 2013. [Google Scholar]
- 21.Gehlsen GM Ganion LR Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31(4):531‐5. [DOI] [PubMed] [Google Scholar]
- 22.Freitas SR Vaz JR Bruno PM, et al. Stretching effects: High‐intensity & moderate‐duration vs. low‐intensity & long‐duration. Int J Sports Med. 2016; 37:239‐44. [DOI] [PubMed] [Google Scholar]
- 23.Cools AM Borms D Castelein B, et al. Evidence‐based rehabilitation of athletes with glenohumeral instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):382‐9. [DOI] [PubMed] [Google Scholar]
- 24.Abdulla SY Southerst D Côté P et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulderϿ. A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man Ther. 2015;20(5):646‐56. [DOI] [PubMed] [Google Scholar]
- 25.Tate AR McClure PW Young IA, et al. Comprehensive impairment‐based exercise and manual therapy intervention for patients with subacromial impingement syndrome: A case series. J Orthop Sport Phys Ther. 2010;40(8):474‐93. [DOI] [PubMed] [Google Scholar]
- 26.Heredia‐Rizo AM López‐Hervás A Herrera‐Monge P, et al. Shoulder functionality after manual therapy in subjects with shoulder impingement syndrome: A case series. J Bodyw Mov Ther. 2013;17(2):212‐8. [DOI] [PubMed] [Google Scholar]
- 27.Camargo PR Alburquerque‐Sendín F Avila MA, et al. Effects of stretching and strengthening exercises with and without manual therapy on scapular kinematics, function, and pain in individuals with shoulder impingement: A randomized controlled trial. J Orthop Sports Phys Ther. 2015;58(12):1‐34. [DOI] [PubMed] [Google Scholar]
- 28.Marzetti E Rabini A Piccinini G, et al. Neurocognitive therapeutic exercise improves pain and function in patients with shoulder impingement syndrome: A single‐blind randomized controlled clinical trial. Eur J Phys Rehabil Med. 2014;50(3):255‐64. [PubMed] [Google Scholar]
- 29.Hegedus EJ Goode A Campbell S, et al. Physical examination tests of the shoulder: A systematic review with meta‐analysis of individual tests. Br J Sports Med. 2007;42(2):80‐92. [DOI] [PubMed] [Google Scholar]
- 30.Michener LA Snyder AR Leggin BG. Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J Sport Rehabil. 2011;20:115‐28. [DOI] [PubMed] [Google Scholar]