Abstract
Introduction
Bacterial meningitis persists in being a substantial cause of high mortality and severe neurological morbidity, despite the advances in antimicrobial therapy. Accurate data has not been available regarding the epidemiology of bacterial meningitis particularly in developing countries, yet. Indeed, the present systematic review provides a comprehensive data analysis on the prevalence and epidemiology of bacterial meningitis in Iran.
Methods
We systematically reviewed articles from 1994 to 2015. The reports which contained the prevalence and etiology of acute bacterial meningitis by valid clinical and laboratory diagnosis were comprised in the present study.
Results
Our analysis indicated that Streptococcus pneumoniae (30% [I2 = 56% p < 0.01]), Haemophilus influenza type b (15% [I2 = 82.75% p < 0.001]), coagulase negative staphylococci (CoNS) (14% [I2 = 60.5% p < 0.06]), and Neisseria meningitidis (13% [I2 = 74.16% p < 0.001]) were the most common cause of acute bacterial meningitis among meningitis cases in Iran. Notably, high frequency rates of nosocomial meningitis pathogens were detected in the present analysis.
Conclusions
It was magnificently attained that the majority of cases for bacterial meningitis in Iran could be avertable by public immunization schemes and by preventive care to inhibit the broadening of hospital acquired pathogens.
Introduction
Infectious meningitis includes viral, bacterial, fungal, and parasitic meningitis which have been considered as severe and potentially fatal pathogens, caused 422,900 deaths and according to the statistic in 2010 approximately 2628,000 patients with disabling sequelae [1]. In the meantime, acute bacterial meningitis (ABM) has been perceived as a common life threatening infection, especially in neonates and infants [2]. Even though, the introduction of broad-spectrum of antibiotics have made bacterial meningitis curable; nonetheless, the mortality and morbidity rate of this life threatening pathogens remains ostensibly high. Whereas, endemic bacterial meningitis residues relatively an infrequent illness in developed countries, the probability of occurrence of endemic and epidemic bacterial meningitis in undeveloped countries accumulates as the major infection [3]. As a matter of fact, ABM continues to be a principal reason of death among neonates in developing countries. Apparently, it seems that this disease debris’s the fourth leading cause of disability in these parts of the globe [4, 5]. Diagnosis of ABM is based on the combination of typical clinical symptoms and the consequent of laboratory tests which indicates the inflammatory response in cerebrospinal fluid (CSF); indeed, demonstrates the specific causative bacterial agent (Gram’s stain, culture, antigen assay and molecular detection) [6]. Three major pathogens have been detected for manifestation of ABM which are listed as follows: Streptococcus pneumonia (pneumococcus), Haemophilus influenzae type b (Hib), and Neisseria meningitidis (meningococcus). Transparently, they have been responsible for 118.400, 83.000, and 75.000 deaths, respectively worldwide [7, 8]. According to the above evidence analysis, a wide range of bacteria can cause ABM. Limpidly, group B Streptococci (GBS) or Streptococcus agalactiae is one of the primary causes of neonatal bacterial meningitis in premature and term infants up to 3 months in many developing countries [9]. The other transpicuous deliberated bacterial strains which apparently could cause bacterial meningitis are Enterobacteriaceae spp., principally Escherichia coli K1 and Klebsiella pneumoniae that can be quite fatal. Moreover, Listeria monocytogenes has been rarely responsible for bacterial meningitis in newborns and infants, especially during zoonotic outbreaks [10, 11].
Translucently, It is essential to state that according to the previous repots, the prevalence and etiologies of ABM vary in each geographical area [12]. To the best of our knowledge, there is no sufficient data regarding the epidemiology of bacterial meningitis in Iran. Allegedly due to the lack of a routine vaccination program against meningeal pathogens; such as, pneumococci in Iran, ABM is considered as a public health hazard with high rate of morbidity, mortality, and tremendous cost burden for the health care providers [13]. Consequently, since there was no accurate estimate of the burden of ABM in Iran, the present systematic study was conducted to provide useful insights concerning the prevalence and epidemiology of the ABM in Iran. Systematic review and meta-analysis according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement were used (S1 Table) [14].
Materials and methods
Search strategies
From January 1, 1994 to May 1, 2015, the entire studies addressing meningitis infections in Iran were collected from world-wide databases including Medline (via PubMed), Web of Science, Embase, and Iranian national databases. Presumably, the search was carried out in both English and Farsi, distinctly and the research was restricted solely to original articles. The following search terms containing Medical Subject Headings (MESH) or keywords in text, title, or abstract were used with the help of Boolean operators (“and” or “or”): ‘‘bacterial”, ‘‘meningitis” and ‘‘Iran”. In addition to English articles, all relevant papers in national databases; included Scientific Information Database (www.sid.ir) and Magiran (www.Magiran.com), were utilized with similar search strategy and Farsi keywords. The reference and citation lists for the regain papers were searched by this phenomenal strategy and with any selected additional study.
Inclusion and exclusion criteria
Apparently, the entire original articles presenting cross-sectional studies on the prevalence and etiology of ABM in patients with suspected meningitis in Iran were considered. Diagnosis of meningitis in the included studies were performed by abnormal CSF findings, including: increased polymorphonuclear leukocytes counts, protein concentration more than 100 mg/dl and hypoglycorrhachia, and CSF culture as the gold standard method for detecting and identifying meningeal isolates [15]. Evidently, numerous studies were excluded from the analysis because of the following reasons: articles which only focused on individual etiological agent for meningitis; article which only considered sub-acute or chronic meningitis, those which only considered individual groups of patients such as HIV positive or immunocompromised patients, surveys which contained other infectious meningitis besides bacterial infections; such as, viral, fungal, and those papers which did not utilize the mentioned methods above; furthermore, reviews and systematic review articles, case reports, and articles which were only available in abstract form were excluded.
Data extraction and definitions
Data were extracted using an extraction form independently and in duplicate by 2 investigators. The following data were extracted from the chosen articles: the first author’s name, the year of the study, the year of publication, the mean age, the location of the studies, the number of cases participated, the method of conducting surveys, the source of samples, sample size, and the prevalence of ABM. The studies identified by the search strategy and were reviewed for eligibility based on title and abstract by two authors. Differences in data extraction between investigators were resolved by consensus.
Quality assessment
Perspicuously, the quality assessment of inquiries were accompanied by two reviewers independently according to the Critical Appraisal Checklist recommended by the Joanna Briggs Institute [16]; moreover, the disagreements were resolved by consensus. The checklist composed of ten questions in which the reviewers answered the questions for the chosen studies based on an individual basis. The ‘Yes’ answer for each question got a point; indeed, the scores ranged from zero to ten. Apparently, the studies which obtained more than 60% were included in the present inquiry.
Meta-analysis
The statistical analysis was carried out by Stata (version13) software. The point estimates of the effect size, the prevalence of bacterial meningitis, and its 95% confidence interval (95% CI) were estimated peculiarly for each study. Random effects models were used to estimate pooled effect. In this regard, the heterogeneity among studies were tested by Cochran’s Q-statistic I2 squared and Galbraith graph. In order to estimate pooled effect, we utilized metaprop command rather than metan in Stata software. For installing, the command needs to be connected to the internet and then typing ssc install metaprop in Stata. We used ftt cimethod (score) or Freeman-Tukey transformation procedures for collecting binomial data. Contrary to metan command, Stata automatically omits studies which their proportion were 0 or 1, transparently, this method does not make the mentioned problem; eventually, plot confidence in forest intervals always were in the range of 0–1 [17–19]. The P-value, 0.05 was considered significant.
Results
Characteristics of included studies
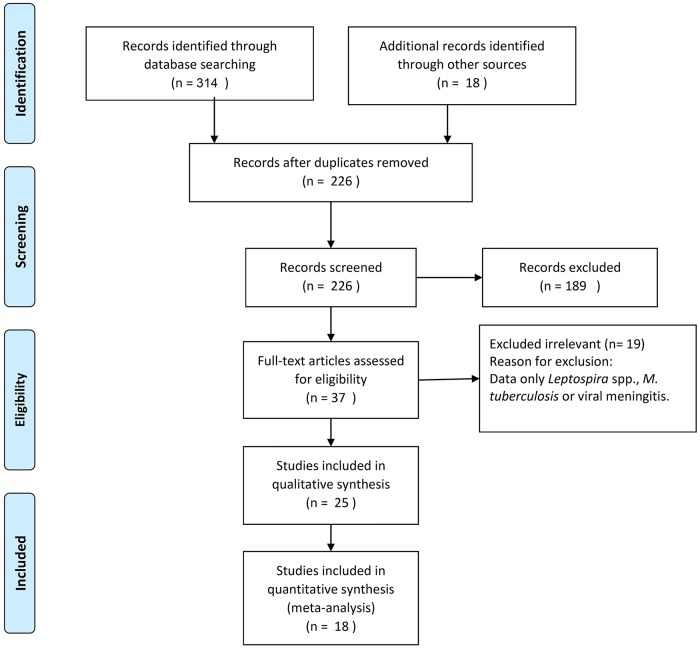
Translucently, a total of 314 reports were screened for the analysis of patients with ABM. Out of these studies 18 met the inclusion pellucid criteria (Fig 1). Characteristics of the selected articles are summarized in Table 1. In fact, 16 studies that were included in the analysis were in English and the rest were in Farsi. Overall, 1078 culture positive samples were analyzed in the included inquiries. Geographic location of the reports comprised east to west and north to south part of Iran; indeed, the majority of patients were coming from central part of Iran. The main diagnostic method in all included studies was the isolation and culture of the pathogen from CSF, or from blood and CSF. Moreover, in most of these studies, the plumb diagnosis was confirmed by additional techniques including serological and molecular assays.
Fig 1. Flow diagram of literature search and study selection.
Table 1. Characteristics of studies included in the meta-analysis.
| Study | Published time | Enrollment time | Sampling area | Mean age | No. of culture positive |
|---|---|---|---|---|---|
| Attarpour et al. [30] | 2014 | 2012–2013 | Tehran | 61±40.2 months | 114 |
| Ataee et al. [31] | 2011 | 2005–2009 | Tehran | 16–70 years | 171 |
| Qurbanalizadegan et al. [32] | 2010 | 2002–2006 | Tehran | <5 years | 36 |
| Motamedifar et al. [33] | 2015 | 2011–2013 | Shiraz | 34±26 years | 225 |
| Yousefi et al. [34] | 2006 | 1998–2002 | Hamedan | <5 years | 146 |
| Abdinia et al. [35] | 2014 | 2003–2013 | Tabriz | 4.2 years | 107 |
| Zamani et al. [36] | 2005 | 1994–1999 | Tehran | 10–28 days | 15 |
| Ghotaslou et al. [37] | 2012 | 2008–2009 | Tabriz | 35±2 months | 11 |
| Heydarian et al. [38] | 2014 | 2005–2012 | Mashhad | 12.7 months | 5 |
| Ehsanipour et al. [39] | 2004 | 1997–2002 | Tehran | 28.5±18.3 months | 4 |
| Haghiashteiani et al. [40] | 2008 | 2001–2007 | Tehran | * | 121 |
| Khalessi et al. [41] | 2014 | 2008–2012 | Tehran | 8.41 days | 4 |
| Bagheri et al. [42] | 2015 | 2006–2012 | Mazandaran | 34.35±18.28 years | 14 |
| Alavi et al. [43] | 2010 | 2003–2007 | Ahvaz | 44.7 ± 26.7 years | 42 |
| Bahador et al. [44] | 2009 | 2003–2005 | Kerman | 15.2±5.2 years | 12 |
| Rezaei et al. [45] | 2013 | 2008–2009 | Tehran | 45.34±42.2 years | 11 |
| Aletayeb et al. [46] | 2010 | 1997–2007 | Ahwaz | 29 days | 31 |
| Mahmoudi et al. [47] | 2013 | 2009–2011 | Tehran | 10 years | 20 |
*Specimens collected from children hospital
The prevalence of bacteria
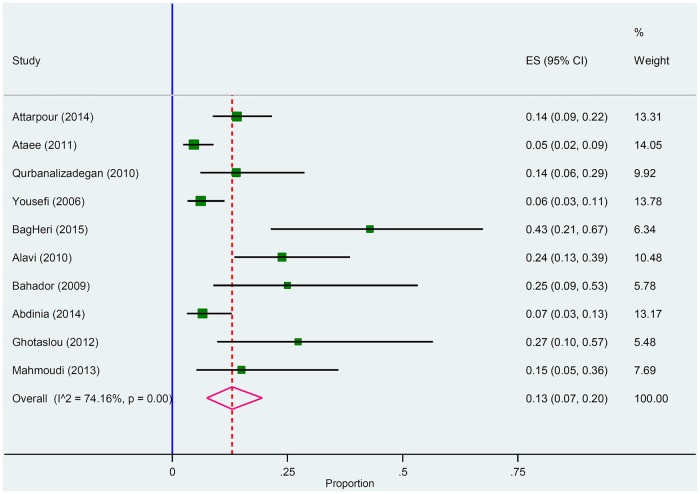
As shown in the Table 2, pneumococcus (30% [I2 = 56% p < 0.01]), Hib (15% [I2 = 82.75% p < 0.001]), CoNS (14% [I2 = 60.5% p < 0.06]), and meningococcus (13% [I2 = 74.16% p < 0.001]) were the most common cause of culture positive ABM.
Table 2. Meta-analysis of proportion of different bacteria in culture positive cases.
| Organism | Frequency of bacteria (%) | Confidence interval 95% | n/N | Heterogeneity Test, I2 (%) | Heterogeneity test, P value |
|---|---|---|---|---|---|
| S. pneumonia < 10 years old | 36 | 31–40 | 67/311 | 0.00 | 0.94 |
| S. pneumonia ≥10 years old | 20 | 13–27 | 182/507 | 32.23 | 0.19 |
| S. pneumonia Overall | 30 | 24–30 | 249/818 | 56 | 0.01 |
| H. influenzae | 15 | 8–22 | 118/876 | 82.75 | <0.001 |
| CoNS | 14 | 8–22 | 54/384 | 60.5 | 0.06 |
| N. meningitides | 13 | 7–20 | 70/673 | 74.16 | <0.001 |
| Klebsiella spp.< 1 month | 4 | 2–7 | 15/50 | 0.00 | 0.94 |
| Klebsiella spp.≥ 1 month | 28 | 11–48 | 17/316 | 36.72 | 0.21 |
| Klebsiella spp. Overall | 9 | 3–18 | 32/376 | 71.53 | <0.001 |
| E. coli | 8 | 6–11 | 57/936 | 20.75 | 0.26 |
| Others | 4 | 2–7 | 35/694 | 31.67 | 0.19 |
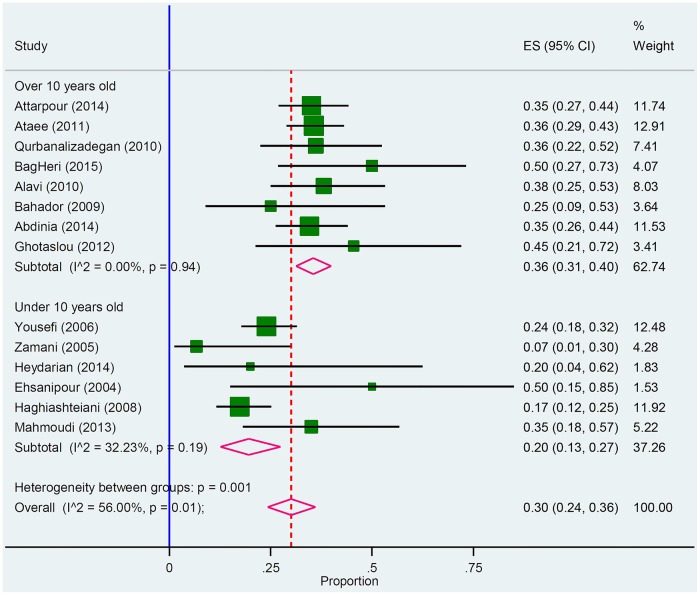
Streptococcus pneumonia
Distinctly, out of the 18 included studies; 14 studies met the inclusion criteria for Pneumococcus. As it was shown in Table 2 and Fig 2, Pneumococcus was responsible for 30% of ABM in Iran. Precisely, the review of the collected reports also manifested pneumococci was the most common causative agent for meningitis in 11 statistical analysis reports (61.11% of studies).
Fig 2. Forest plot of the meta-analysis on proportion of S. pneumonia in culture positive cases.
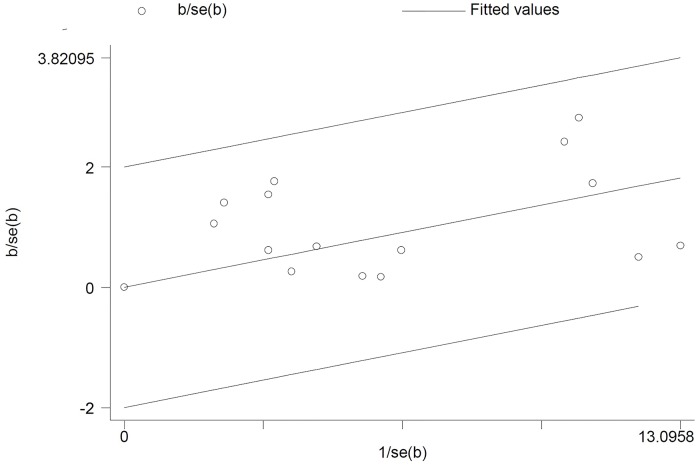
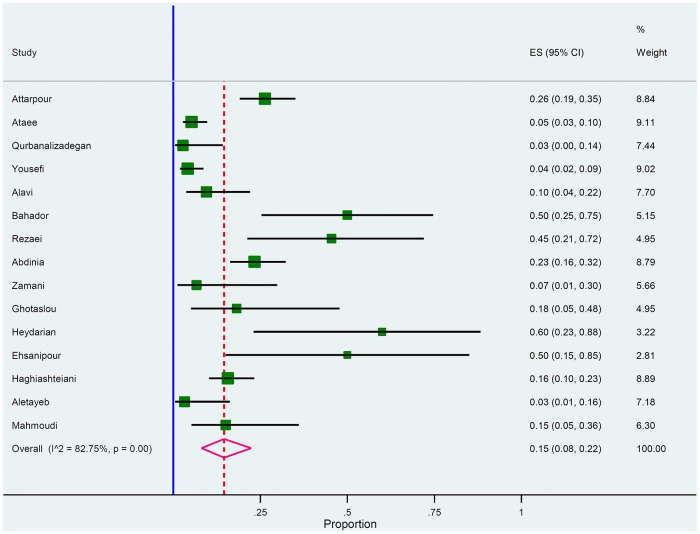
Haemophilus influenza
Articulately, out of the 18 included studies; 15 studies met the inclusion criteria for Hib (Fig 3). As it is presented in Galbraith plot in the Fig 4, the meta-analysis on H. influenza in culture positive meningitides; this graph shows heterogeneity among studies; in addition, all studies were in -2 to +2 z-score rang without any outlier point.
Fig 3. Galbrath plot of the meta-analysis on H. influenza in culture positive cases.
Fig 4. Forest plot of the meta-analysis on proportion of H. influenza in culture positive cases.
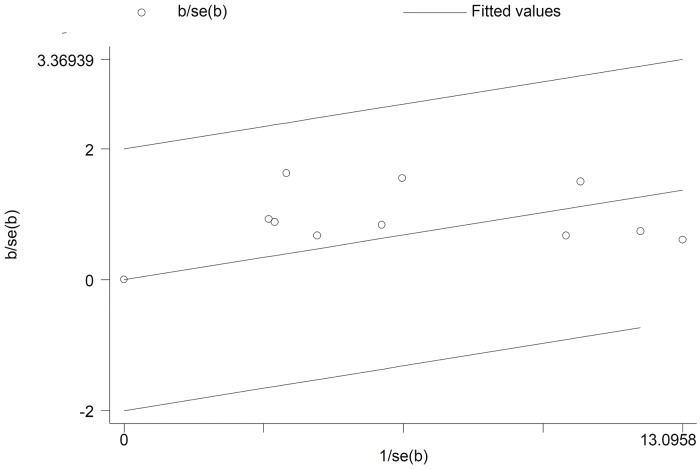
Neisseria meningitides
Of these 18 included studies; 10 studies met the inclusion criteria for N. meningitides (Fig 5). Galbrath plot of the meta-analysis on N. meningitides in culture positive meningitides showes heterogeneity among reports and all studies were in the range of -2 to +2 z-score without any outlier point (Fig 6).
Fig 5. Forest plot of the meta-analysis on proportion of N. meningitides in culture positive cases.
Fig 6. Galbrath plot of the meta-analysis on N. meningitides in culture positive cases.
Clinical and laboratory features
Overall, 43% (95% CI 30–57%) of neonate with CSF-culture positive were preterm (Table 3). Furthermore, 39% (95% CI 26–52) of the utter patients suffered from malnutrition. The clinical presentation of ABM was characterized by fever (71%, CI 37–69%), irritability (60%, 95% CI 52–69%), and seizures (33%, 95% CI 25–41%). In addition, more clinical features are shown in Table 4. It is mentionable that laboratory features in CSF-culture positive samples were characterized by increased CSF leukocytes counts (753.353 (cells/mm3), 95%CI 596.294–910.412), increased CSF protein (415.5 (mg/dl), 95% CI 86.5–744), decreased CSF glucose (30.46 (mg/dl), and 95% CI 25.17–35.74) (Table 3).
Table 3. Meta-analysis of proportion of clinical and laboratory features in culture positive meningitis.
| Clinical features | Proportion in culture positive meningitis (%) | Confidence interval 95% | n/N | Heterogeneity test, I2 (%) | Heterogeneity test, P value |
| Preterm (in neonate) | 43 | 30–57 | 29/66 | 18.77 | 0.29 |
| Malnutrition | 39 | 26–52 | 63/181 | 43.79 | 0.17 |
| Seizures | 33 | 25–41 | 104/320 | 35 | 0.17 |
| Irritability | 60 | 52–69 | 77/127 | 0.00 | <0.001 |
| Fever | 71 | 37–96 | 261/312 | 96.11 | <0.001 |
| Laboratory features | Prevalence in culture positive meningitis | n/N | Heterogeneity Test, I2 (%) | Heterogeneity test, P value | |
| Protein (mg/dl) | 415.5 | 86.5–744 | - | 99.4 | <0.001 |
| Glucose (mg/dl) | 30.46 | 25.17–35.74 | - | 36.58 | <0.001 |
| CSF leukocyte count (cells/mm3) | 753.353 | 596.294–910.412 | - | 0.07 | 0.793 |
Table 4. Clinical characteristics of patients with bacterial meningitis.
| Clinical presentation | |
|---|---|
| Decreased Moro Reflex | 20/5 (25%) |
| Icter | 2/20 (10%) |
| Hydrocephaly | 61/ 186 (32.8%) |
| Brain edema | 5/40 (12.5%) |
| Subdural Effusion | 5/40 (12.5%) |
| Lethargy | 51/157 (32.5%) |
| Nausea and vomiting | 179/268 (66.8%) |
| Headache | 85/ 253 (33.6%) |
| Leukocytosis | 109/146 (74.65%) |
| Died | 23/197 (11.6%) |
Discussion
Inclusively, the survey which was obtained from this investigation indicated that pneumococcus was the most common etiologic agent determined in patients with ABM in Iran and likewise, Hib, CoNS, and meningococcus were diagnosed respectively. Causative organisms for bacterial meningitis differ according to the population investigated, age of the participants, and geographic area in which the data were analyzed [20]. We considered the entire mentioned variables correlations with the prevalence of ABM causative agents in our analysis; nonetheless, the statistical significant variables like age solely were reported.
In the recent decade, pneumococcus has been considered as the main causative agent for bacterial meningitis in children less than 10 years old, in elder population, and in immunocompromised hosts in the United States as well as in European countries [21]. Indeed, the present study conducted a meta-analysis for the prevalence of pneumococcus meningitis in Iran. According to the statistical analysis, the prevalence of pneumococcus meningitis in children less than 10 years and individuals over 10 years old was 36% (95% CI; 31–40) and 20% (95% CI; 13–27) thereof. Peculiarly, there was a significant difference in the prevalence of these two sub-groups. The high prevalence rate of pneumococcal meningitis in Iran is alarming since the emergence of drug resistant strains; especially those are resistant to penicillin and third-generation cephalosporins. Penicillin resistance is an indicator of reduced susceptibility to other antibiotic agents, which could lead to treatment failures in patients with pneumococcal meningitis [22]. Moreover, the 7-valent pneumococcal conjugate vaccine (PCV-7) became commercially available; however, it is not as a mandatory prescribed vaccine in Iran and is only prescribed for high-risk individuals. Therefore, pneumococcal meningitis could have the potential to become a serious life threatening infection in this region.
According to the analysis retrieved, Hib (15%) was the second most common causative agent for bacterial meningitis in Iran. It is quite essential to mention that before the invention of the conjugate polysaccharide vaccine against Hib, this pathogen was the most incitement of meningitis world-wide. It is mentionable that as of now Hib meningitis is peculiarly rare in areas with routine Hib vaccination [23]. In Iran, based on the CDC reports, the rate of Hib meningitis was <15 per 100,000 in 2004 [24]. Moradi et al. predicted that vaccination against Hib in 2008 in the birth cohort in Iran could reduce from 385 meningitis cases to 62 cases [25]. Accordingly, there are facts that after 2014, the major achievement of the immunization programs occurred in Iran following the introduction of the DTPw-HB/Hib prevalent vaccine (containing diphtheria-tetanus-whole cell pertussis-hepatitis B/Hib); moreover, a significant reduction in the mortality and morbidity rate of Hib meningitis is predictable due to Hib meningitis in Iran. It should be noted that all the included studies in the present analysis were conducted before 2014.
Notably, CoNS was the third most common cause of ABM according to our analysis which accounted for 14% (95% CI; 8–22) of the entire cases. Nosocomial bacterial meningitis poses a considerable public health hazard because of the growing emergence of multidrug resistant organisms (MDROs) and severely limited treatment options [26, 27]. As a matter of fact, the high incidence of nosocomial meningitis reported in Iran is alarming. It is essential to pay attention for controlling and preventing CNS infections by virtue of the opportunistic organisms. Now it's time to make the decision to improve the quality of infection control systems and practices in Iranian health centers according to international guidelines.
Meningococcus was considered as another common cause of ABM in Iran which accounts for 13% (95% CI; 7–20) of all cases. The only reported document regarding the meningococcal incidence rate in Iran was conformed in 2005, the search was done from 1996 until now, when the rate was 0.14 per 100 000 [28]. In 2000, meningococcal caused by the serogroup W-135 outbreak strain associated with the Hajj pilgrimage were reported in certain Middle Eastern and North Africa countries, including Iran [29]. Indeed, explicitly there is no sufficient data concerning the incidence rate of meningococcal meningitis in Iran. A polyvalent meningococcal vaccine, containing the purified polysaccharide capsules of group A, C, Y, and W-135 meningococci, is accessible in Iran. Nevertheless, the vaccine is not mandatory for the population, solely it is required for those who travel abroad (especially to Saudi Arabia for Hajj) and enlisted soldiers. Therefore, public immunization against meningococcus can reduce prevalence of ABM due to this pathogen.
Clinical features give the clue to the early diagnosis of ABM by a physician; therefore, there are various clinical symptoms which can be quite helpful in the diagnosis process. In the recent study, 71% (95% CI; 37–96) of ABM patient manifested sign and symptoms of fever with high heterogeneity (I2 = 96.11% p < 0.001). by using medications which are not prescribed by medical doctors for fever or other symptoms can head to heterogeneity and drug resistance consequences. The analysis showed that preterm 43% (95% CI; 30–57) had a distinct risk factor for neonate ABM. The other predominant finding in this study was showing the early screening techniques and the analysis of CSF for early screening of ABM (Tables 3 and 4). There was no significant relationship between alcoholism, splenectomy, immunosuppressive medication, and diabetes mellitus with culture positive patients. In future studies more inquiries are needed for other aspect of bacterial meningitis like the pattern of drug resistance, prevention, rapid, and novel detection methods because of the emergency of bacterial meningitis.
Conclusions
The current systematic review indicated that the most common causative agent of ABM could be vaccine-preventable pathogens in Iran. Further accurate and efficient data regarding the prevalence of the etiological agents for bacterial meningitis, especially after public immunization against Hib, can be exploited for an effective immunization schedules. Indeed, to reduce the incidence of nosocomial meningitis, prevention and control measures should be considered in accordance to the international standards in Iranian clinics and hospitals.
Supporting information
(DOC)
Acknowledgments
We would like to thank the “Clinical Research Development Center of Baqiyatallah hospital” for their kindly cooperation.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Portnoy A, Jit M, Lauer J, Blommaert A, Ozawa S, Stack M, et al. Estimating costs of care for meningitis infections in low- and middle-income countries. Vaccine. 2015;33 Suppl 1:A240–7. Epub 2015/04/29. [DOI] [PubMed] [Google Scholar]
- 2.Roine I, Peltola H, Fernandez J, Zavala I, Gonzalez Mata A, Gonzalez Ayala S, et al. Influence of admission findings on death and neurological outcome from childhood bacterial meningitis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2008;46(8):1248–52. Epub 2008/05/01. [DOI] [PubMed] [Google Scholar]
- 3.Kim KS. Pathogenesis of bacterial meningitis: from bacteraemia to neuronal injury. Nature reviews Neuroscience. 2003;4(5):376–85. Epub 2003/05/03. 10.1038/nrn1103 [DOI] [PubMed] [Google Scholar]
- 4.Kim KS. Acute bacterial meningitis in infants and children. The Lancet Infectious diseases. 2010;10(1):32–42. Epub 2010/02/05. 10.1016/S1473-3099(09)70306-8 [DOI] [PubMed] [Google Scholar]
- 5.Edmond K, Clark A, Korczak VS, Sanderson C, Griffiths UK, Rudan I. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. The Lancet Infectious diseases. 2010;10(5):317–28. Epub 2010/04/27. 10.1016/S1473-3099(10)70048-7 [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Debata PK, Ranjan A, Gaind R. The role and reliability of rapid bedside diagnostic test in early diagnosis and treatment of bacterial meningitis. Indian journal of pediatrics. 2015;82(4):311–4. Epub 2014/03/15. 10.1007/s12098-014-1357-z [DOI] [PubMed] [Google Scholar]
- 7.Teleb N, Pilishvili T, Van Beneden C, Ghoneim A, Amjad K, Mostafa A, et al. Bacterial meningitis surveillance in the Eastern Mediterranean region, 2005–2010: successes and challenges of a regional network. The Journal of pediatrics. 2013;163(1 Suppl):S25–31. Epub 2013/06/21. 10.1016/j.jpeds.2013.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England). 2012;380(9859):2095–128. Epub 2012/12/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saez-Llorens X, McCracken GH Jr. Antimicrobial and anti-inflammatory treatment of bacterial meningitis. Infectious disease clinics of North America. 1999;13(3):619–36, vii Epub 1999/09/02. [DOI] [PubMed] [Google Scholar]
- 10.Moreno MT, Vargas S, Poveda R, Saez-Llorens X. Neonatal sepsis and meningitis in a developing Latin American country. The Pediatric infectious disease journal. 1994;13(6):516–20. Epub 1994/06/01. [DOI] [PubMed] [Google Scholar]
- 11.Linnan MJ, Mascola L, Lou XD, Goulet V, May S, Salminen C, et al. Epidemic listeriosis associated with Mexican-style cheese. The New England journal of medicine. 1988;319(13):823–8. Epub 1988/09/29. 10.1056/NEJM198809293191303 [DOI] [PubMed] [Google Scholar]
- 12.Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev. 2010;23(3):467–92. Epub 2010/07/09. 10.1128/CMR.00070-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdinia B, Ahangarzadeh Rezaee M, Abdoli Oskouie S. Etiology and antimicrobial resistance patterns of acute bacterial meningitis in children: a 10-year referral hospital-based study in northwest iran. Iranian Red Crescent medical journal. 2014;16(7):e17616 Epub 2014/09/23. 10.5812/ircmj.17616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–9. [DOI] [PubMed] [Google Scholar]
- 15.VanDemark M. Acute bacterial meningitis: current review and treatment update. Critical care nursing clinics of North America. 2013;25(3):351–61. 10.1016/j.ccell.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 16.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews: Addressing questions of prevalence. International Journal of Health Policy & Management (IJHPM). 2014;3:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freeman MF, Tukey JW. Transformations related to the angular and the square root. The Annals of Mathematical Statistics. 1950:607–11. [Google Scholar]
- 18.Harris R, Bradburn M, Deeks J, Harbord R, Altman D, Sterne J. Metan: fixed-and random-effects meta-analysis. Stata journal. 2008;8(1):3. [Google Scholar]
- 19.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Archives of Public Health. 2014;72(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heckenberg SG, Brouwer MC, van de Beek D. Bacterial meningitis. Handbook of clinical neurology. 2014;121:1361–75. Epub 2013/12/25. 10.1016/B978-0-7020-4088-7.00093-6 [DOI] [PubMed] [Google Scholar]
- 21.Hoffman O, Weber RJ. Pathophysiology and treatment of bacterial meningitis. Therapeutic advances in neurological disorders. 2009;2(6):1–7. Epub 2010/12/25. 10.1177/1756285609337975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR. Advances in treatment of bacterial meningitis. Lancet (London, England). 2012;380(9854):1693–702. Epub 2012/11/13. [DOI] [PubMed] [Google Scholar]
- 23.Martin M, Casellas JM, Madhi SA, Urquhart TJ, Delport SD, Ferrero F, et al. Impact of haemophilus influenzae type b conjugate vaccine in South Africa and Argentina. The Pediatric infectious disease journal. 2004;23(9):842–7. Epub 2004/09/14. [DOI] [PubMed] [Google Scholar]
- 24.Feikin DR, Nelson CB, Watt JP, Mohsni E, Wenger JD, Levine OS. Rapid assessment tool for Haemophilus influenzae type b disease in developing countries. Emerging infectious diseases. 2004;10(7):1270–6. 10.3201/eid1007.030737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moradi-Lakeh M, Shakerian S, Esteghamati A. Immunization against Haemophilus Influenzae Type b in Iran; Cost-utility and Cost-benefit Analyses. International journal of preventive medicine. 2012;3(5):332–40. Epub 2012/06/19. [PMC free article] [PubMed] [Google Scholar]
- 26.Kim BN, Peleg AY, Lodise TP, Lipman J, Li J, Nation R, et al. Management of meningitis due to antibiotic-resistant Acinetobacter species. The Lancet Infectious diseases. 2009;9(4):245–55. Epub 2009/03/28. 10.1016/S1473-3099(09)70055-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler AT, Kourtis AP. Treatment of meningitis caused by methicillin-resistant Staphylococcus aureus with linezolid. Infection. 2007;35(4):271–4. Epub 2007/07/25. 10.1007/s15010-007-6211-z [DOI] [PubMed] [Google Scholar]
- 28.Ceyhan M, Anis S, Htun-Myint L, Pawinski R, Soriano-Gabarro M, Vyse A. Meningococcal disease in the Middle East and North Africa: an important public health consideration that requires further attention. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2012;16(8):e574–82. Epub 2012/06/01. [DOI] [PubMed] [Google Scholar]
- 29.Wilder-Smith A, Goh KT, Barkham T, Paton NI. Hajj-associated outbreak strain of Neisseria meningitidis serogroup W135: estimates of the attack rate in a defined population and the risk of invasive disease developing in carriers. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2003;36(6):679–83. Epub 2003/03/11. [DOI] [PubMed] [Google Scholar]
- 30.Attarpour-Yazdi MM, Ghamarian A, Mousaviehzadeh M, Davoudi N. Identification of the serotypes of bacterial meningitis agents; implication for vaccine usage. Iranian journal of microbiology. 2014;6(4):211 [PMC free article] [PubMed] [Google Scholar]
- 31.Ataee RA, Tavana AM, Izadi M, Hosseini SMJ, Ataee MH. Bacterial meningitis: a new risk factor. Journal of Research in Medical Sciences. 2011;16(2). [PMC free article] [PubMed] [Google Scholar]
- 32.Qurbanalizadegan M, Ranjbar R, Ataee R, Hajia M, Goodarzi Z, Farshad S, et al. Specific PCR assay for rapid and direct detection of Neisseria meningitidis in cerebrospinal fluid specimens. Iranian journal of public health. 2010;39(4):45 [PMC free article] [PubMed] [Google Scholar]
- 33.Motamedifar M, Ebrahim-Saraie HS, Mansury D, Nikokar I, Hashemizadeh Z. Prevalence of Etiological Agents and Antimicrobial Resistance Patterns of Bacterial Meningitis in Nemazee Hospital, Shiraz, Iran. Archives of Clinical Infectious Diseases. 2015;10(2). [Google Scholar]
- 34.Mashouf RY, Hashemi SH, Bijarchi M. Bacterial agents of meningitis in children and detection of their antibiotic resistance patterns in Hamadan, Western Iran. Pak J Biol Sci. 2006;9:1293–8. [Google Scholar]
- 35.Abdinia B, Rezaee MA, Oskouie SA. Etiology and antimicrobial resistance patterns of acute bacterial meningitis in children: a 10-year referral hospital-based study in northwest iran. Iranian Red Crescent Medical Journal. 2014;16(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.ZAMANI A, ZAMANI F. Cerebrospinal fluid findings in neonatal bacterial meningitis. Medical Journal of The Islamic Republic of Iran (MJIRI). 2005;19(3):241–5. [Google Scholar]
- 37.Ghotaslou R, Farajnia S, Yeganeh F, Abdoli-Oskouei S, Rezaee MA, Barzegar M. Detection of acute childhood meningitis by PCR, culture and agglutination tests in Tabriz, Iran. Acta Medica Iranica. 2012;50(3):192 [PubMed] [Google Scholar]
- 38.Heydarian F, Ashrafzadeh F, Rostazadeh A. Predicting factor s and prevalence of meningitis in patients with first seizure an d fever aged 6 to 18 months. Neurosciences. 2014;19(4):297–300. [PMC free article] [PubMed] [Google Scholar]
- 39.Ehsanipour F, Khodapanahandeh F, Aslani Z. The prevalence of meningitis in children with febrile seizure hospitalized at Hazrat Rasoul hospital (1997–2002). Razi Journal of Medical Sciences. 2005;11(44):907–11. [Google Scholar]
- 40.Haghiashteiani M, Mohammadi-Yeganeh S, Soroush S, Sadeghifard N, Sayadi S, Dabyri H, et al. Frequency and antimicrobial susceptibility of Haemophilus influenzae Type b isolated from children suspected to meningitis. Iranian J Publ Health. 2008;37(4):52–8. [Google Scholar]
- 41.Kalessi N, Afsarkhas L. Neonatal meningitis: risk factors, causes, and neurologic complications. Iranian journal of child neurology. 2014;8(4):46–50. [PMC free article] [PubMed] [Google Scholar]
- 42.Bagheri-Nesami M, Babamahmoodi F, Nikkhah A. Types, risk factors, clinical symptoms and diagnostic tests of acute adult meningitis in northern iran during 2006–2012. Journal of clinical and diagnostic research: JCDR. 2015;9(5):IC01 10.7860/JCDR/2015/11991.5936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alavi S, Moshiri N, Shokri S. Evaluation of epidemiological, clinical and laboratory findings of admitted patients with meningitis in Infectious Diseases Ward of Razi Hospital, Ahvaz. Jundishapur Scientific Medical Journal. 2010;9(3):222–31. [Google Scholar]
- 44.Amini M, Bahador M, Bahador M. Common cause and cerebrospinal fluid changes of acute bacterial meningitis. Iranian Journal of Pathology. 2009;4(2):75–9. [Google Scholar]
- 45.Rezaei M, Mamishi S, Mahmoudi S, Pourakbari B, Khotaei G, Daneshjou K, et al. Cerebrospinal fluid ferritin in children with viral and bacterial meningitis. Br J Biomed Sci. 2013;70(3):101–3. [DOI] [PubMed] [Google Scholar]
- 46.Aletayeb MH, Ahmad FS, Masood D. Eleven-year study of causes of neonatal bacterial meningitis in Ahvaz, Iran. Pediatr Int. 2010;52(3):463–6. 10.1111/j.1442-200X.2010.03107.x [DOI] [PubMed] [Google Scholar]
- 47.Mahmoudi S, Zandi H, Pourakbari B, Ashtiani MTH, Mamishi S. Acute bacterial meningitis among children admitted into an Iranian referral children's hospital. Jpn J Infect Dis. 2013;66(6):503–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.