Abstract
Objectives
To develop a simple prediction model for the pre-screening of Retinopathy of Prematurity (ROP) among preterm babies.
Methods
This was a prospective study. The test dataset (January 2007 until December 2010) was used to construct risk prediction models, and the validation dataset (January 2011 until March 2012) was used to validate the models developed from the test dataset. Two prediction models were produced using the test dataset based on logistic regression equations in which the development of ROP was used as the outcome.
Results
The sensitivity and specificity for model 1 [gestational age (GA), birth weight (BW), intraventricular haemorrhage (IVH) and respiratory distress syndrome (RDS)] was 82 % and 81.7%, respectively; for model 2, (GA and BW) the sensitivity and specificity were 80.5% and 80.3%, respectively.
Conclusion
Model 2 was preferable, as it only required two predictors (GA and BW). Our prediction model can be used for early detection of ROP to avoid poor outcomes.
Keywords: model, prematurity, prediction, risk, retinopathy
Introduction
Retinopathy of prematurity (ROP), formerly known as retrolental fibroplasia, was first described by Terry in 1942 (1). It is a disease confined to preterm infants and is a disorder of the immature retinal vasculature that can progress to tractional retinal detachment and complete blindness. In highly developed countries, it is estimated to be responsible for 3% to 11% of childhood blindness, and in moderately developed countries such as Malaysia and Brazil, it represents approximately 60% of childhood blindness (2). The incidence of ROP-induced-blindness in poorly developed regions such as Sub-Saharan Africa and Kenya is low due to the lack of facilities permitting the survival of pre-term babies. In highly developed countries, ROP is confined to infants with very low birth weight (VLBW) and gestational age (GA) ≤ 31 weeks (3), whereas the same cannot be said for moderately developed countries.
Screening of preterm babies for ROP is challenging. The increased survival of very immature babies results in a need to screen a large population of babies at risk of developing severe ROP, which is costly. In addition, a high degree of cooperation between neonatology and ophthalmology staff is required (4). In developing countries, there are additional difficulties due to the unequal distribution of the Neonatal Intensive Care Unit (NICU) facilities, lack of skilled ophthalmologists and lack of awareness among neonatologists (4).
Prediction models based on important risk factors aid in efficient screening of babies at high risk of developing ROP by reducing the number of babies unnecessarily examined and minimising the risk of misidentifying babies with ROP. Prediction models can also be cost effective and avoid the need for skilled ophthalmologists. Thus, the purpose of this research is to develop prediction models for the pre-screening of the at-risk population.
Methods
Our study was a prospective study involving preterm babies from a tertiary hospital in Sarawak, East Malaysia. All preterm babies managed in the neonatology ward and subsequently followed up in the eye clinic of Sarawak General Hospital (SGH) from January 2007 to March 2012 were included in our study. Data were collected and analysed in two time frames. Data for the development period (first dataset) were collected from January 2007 until December 2010, whereas data for the validation period (second dataset) were collected from January 2011 until March 2012.
The screening, treatment and follow-up of these babies were performed according to the Malaysian guidelines for the detection and treatment of ROP (5). Screening was carried out for infants with either birth weight (BW) less than 1 500 gram, GA less than 32 weeks or with an unstable clinical course who were at high risk (as determined by the paediatrician). The first examination was performed four weeks after birth. If there were no signs of ROP, screening was performed at two weeks interval. Infants with ROP were screened every week or more frequently depending on the severity. Screening was continued until the retina was completely vascularised, ROP had fully regressed, or ROP had progressed to a stage where treatment was indicated. Preterm infants born elsewhere, who missed follow-up or who were transferred to other hospitals, were excluded from our study.
As the main outcome was to develop a simple prediction model for ROP pre-screening of preterm babies, the primary clinical outcome was the incidence of any stage of ROP. The predictors were gestational age (GA), birth weight (BW), respiratory distress syndrome (RDS) and intraventricular haemorrhage (IVH).
ROP was graded based on the International Classification of ROP (6,7). If ROP was present in both eyes, the eye with the more advanced disease was used for analysis. To develop the prediction model, the final ROP stage was used. The study was approved by the Malaysian Medical Research Ethics Committee (NMRR ID: 12532) and followed the tenets of the Declaration of Helsinki. Written informed consent for participation in the study was obtained from parents or guardians.
Statistical analysis
The aim of the study was to develop a simple prediction model to pre-screen ROP among preterm babies. Descriptive analyses, such as the mean and standard deviation, were used to clinically profile the babies using various characteristics, such as BW and GA. The frequencies and percentages were presented for categorical variables. A univariate analysis using Pearson’s chi-squared test was conducted to determine the predictors of ROP.
We designed two risk prediction models using the dataset from the development period based on the logistic regression equation with development of ROP as the outcome. We used four predictors that were significant in the univariate analysis for model 1 and two predictors that were significant in the multivariate analysis for model 2. We developed a binary logistic regression models to estimate the parameters and evaluate the statistical significance. All chosen predictors were simultaneously analysed (enter method). The logistic function for a single predictor is given by Z = βo + β1X1 + ɛ, where β is the coefficient, X is the predictor/variable and ɛ is the error term. To obtain the probability of the outcome of interest, the Z value is then transformed using the following link function: P [event] = ez/1 + ez, where ez is the exponential value of Z.
Using these two mathematical equations, we derived the optimal cut-off (probability) that identified babies with and without ROP using a sensitivity and specificity analysis. The optimal cut-offs were derived based on the highest values of sensitivity and specificity where the sensitivity value must be higher than the specificity value. We then used the same optimal cut-off from both models to validate the outcome based on the dataset in the validation period (second dataset). The prediction accuracy was evaluated based on the sensitivity, specificity, positive predictive and negative predictive values. All our analyses were carried out using SPSS version 19.0. (IBM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp.)
Results
This study involved 519 babies in the development period and 220 babies in the validation period. The mean (SD) BW of the babies in the development period was 1268.7 (SD 320.4) g and the mean (SD) GA was 29.6 (SD 2.4) weeks.
All four predictors (GA, BW, RDS, and IVH) were significant (P < 0.001) in the univariate analysis (Table 1). Thus, GA, BW, RDS, and IVH were good at predicting ROP in babies. After logistic regression, the most important adjusted risk factors were GA (OR: 1.406, 95% CI: 1.170 to1.689] and BW [OR: 1.004, 95% CI: 1.003 to1.006). We again tested these two variables using logistic regression with the enter method procedure and found that both were statistically significant (Table 2). We developed two models, and the equations of the predictive models were the following:
Table 1.
Univariate analysis for associated factors of ROP in preterm babies in a tertiary hospital in Sarawak
| Variables | No ROP n (%) | With ROP n (%) | P valuea |
|---|---|---|---|
| Gestational Age | < 0.001 | ||
| < 28 weeks | 109 (25.2) | 63 (76.8) | |
| 29 to 31 weeks | 218 (50.3) | 18 (22) | |
| > 31 weeks | 106 (24.5) | 1(1.2) | |
| Birth Weight | |||
| ELBW | 49 (11.3) | 56 (68.3) | < 0.001 |
| VLBW | 268 (62) | 23 (28) | |
| LBW | 115 (26.6) | 3 (3.7) | |
| Intraventricular Hemorrhage | < 0.001 | ||
| No | 334 (78.2) | 39 (49.4) | |
| Yes | 93 (21.8) | 40 (50.6) | |
| Respiratory Distress syndrome | < 0.001 | ||
| No | 180 (42.2) | 15 (19) | |
| Yes | 247 (57.8) | 64 (81) |
Chi-square test was applied
The total numbers were not the same with 519 in all tabulation due to missing values
Abbreviations: ELBW = Extremely Low Birth Weight; VLBW = Very Low Birth Weight; LBW = Low Birth Weight.
Table 2.
Results from logistic regression for Model 1 and Model 2
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| B | OR | 95% CI | B | OR | 95% CI | |
| Constant | 11.436 | 12.791 | ||||
| Gestational age | −0.312 | 0.732 | 0.605, 0.886* | −0.341 | 0.711 | 0.592,0.854** |
| Birth weight | −0.004 | 0.996 | 0.994, 0.997** | −0.004 | 0.996 | 0.994,0.997** |
| RDS | 0.629 | 1.876 | 0.884, 3.980 | |||
| IVH | 0.541 | 1.717 | 0.921, 3.201 | |||
significant at less than 0.05.
significant at less than 0.001.
Model 1: Include all variables that were significant at univariate analysis and standardized coefficient were derived from logistic regression using enter method.
Model 2: Include variables(Gestational age and birth weight) that were significant at multivariate analysis and standardized coefficient were derived from logistic regression using enter method.
Model 1 was derived from four predictors, and model 2 was derived without RDS and IVH. Z is the logit value where Z is a continuous variable centred on 0. To obtain the probability of the outcome of interest, the Z value is then transformed using the following link function:
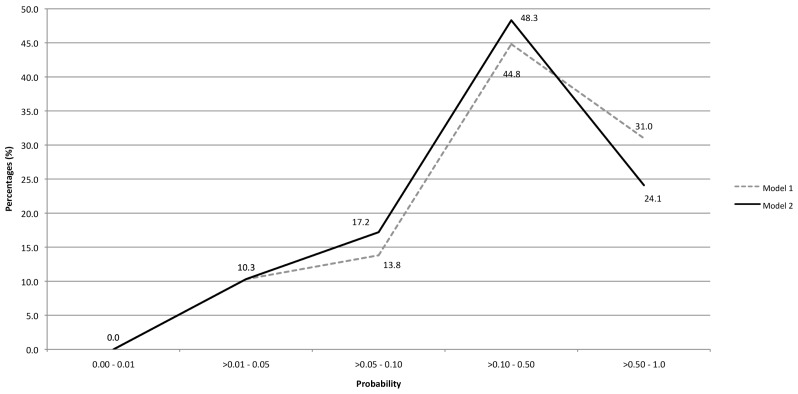
P [event] = ez/1 + ez. This probability value ranges from 0 to 1. The distributions of the probability for both models are presented in figure 1.
Figure 1.
The percentage of patients presented with ROP between model 1 and model 2.
For model accuracy, the sensitivity and specificity of model 1 was higher than model 2 (Table 3). However, there was only a slight difference between these two models. Based on the validation period, the sensitivity and specificity of model 1 were 72.4% and 82.3% (from optimal cut-off of 0.159), while the values for model 2 were 65.5% and 81.9% (from an optimal cut-off of 0.173). Although model 1 was slightly better, the accuracy was comparable to model 2 (Table 4 and Figure 1). The minimum cut-off value for screening preterm babies who are at higher risk of developing any ROP for both models was 0.01. Preterm infants with a probability of less than 0.01 did not develop ROP in our study (Figure 1).
Table 3.
Result of Sensitivity and Specificity analysis for Model 1 and Model 2
| Model | Optimal cut off | ROC | 95%CI | Sensitivity | Specificity |
|---|---|---|---|---|---|
| 1 | 0.159 | 0.89 | 0.84, 0.94 | 82.0% | 81.7% |
| 2 | 0.173 | 0.87 | 0.83, 0.92 | 80.5% | 80.3% |
Model 1: All significant predictors from univariable analyses were analysed using multivariable (enter method).
Model 2: Two significant predictors from multivariable (enter method) were analysed again using multivariable (enter method).
Table 4.
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of validation result
| Model 1 | Model 2 | |
|---|---|---|
| Sensitivity | 72.4% | 65.5% |
| Specificity | 82.3% | 81.9% |
| PPV | 39.6% | 36.5% |
| NPV | 94.9% | 93.7% |
Minimum probability to cover all patients with ROP from validation data is at least 0.01 for both models.
Discussion
ROP has been linked to several risk factors. These factors can be maternal (complications of pregnancy or use of beta-blockers) and foetal (sepsis, intraventricular haemorrhage, respiratory distress syndrome, hypercarbia, recurrent apnoea, vitamin E deficiency, indomethacin treatment for patent ductus arteriosus, light, blood transfusions, use of erythropoietin and the type of neonatal unit). As ROP affects only the immature retinal vessels and does not develop after retinal vascularization is complete, the major risk factor is the degree of prematurity, which is measured by either BW or GA. The incidence and severity of ROP were inversely related to BW and GA [8–9]. Of the two, BW is considered the more powerful predictor (10). In our study, BW and GA were also significant predictors of ROP.
The first epidemic of ROP began in 1940 and was due to the high unrestricted and unmonitored use of supplemental oxygen, which was brought to an end a decade later by oxygen restriction. It also led to the discovery that oxygen supplementation was a risk factor for the development of ROP, which was confirmed by Campell (11). Both hypoxia and hyperoxia may be associated with ROP. Although 70 years has passed since the first reported case of ROP, we still do not know the safe limits of supplemental oxygen in clinical practice. Current evidence suggests that ROP is linked to the duration of oxygen supplementation rather than the concentration. Intraventricular haemorrhage caused by rupture of the immature thin walled sub-ependymal vessels due to cerebral hypoperfusion is associated with very immature infants. Intraventricular haemorrhage as a significant risk factor for ROP has been reported by some studies (12). In our study, IVH and RDS showed significance only in the univariate analysis and thus, were less important in predicting ROP in our study. Similar results have been reported in other studies (13–14).
Our prediction model is derived from the logistic regression equation. To strengthen the stability of the two models, we validated the cut-off derived from the test dataset and confirmed it with the validation dataset. In our study, the first model was best at identifying babies with and without ROP at a cut-off value of 0.159. However, the second model with a cut-off value of 0.173 was slightly better than the first model in predicting ROP as it required only two variables (GA and BW). In addition, a cut-off value of 0.01 for both models can be used for screening high risk babies. The low positive predictive value and high negative predictive value might be caused by the relatively low prevalence of the disease. Although this prediction approach is easy, cheap and fast, the accuracy of these two models need to be validated from time to time to ensure consistency.
There were some limitations in our study. The focus of this study was to establish a prediction model for ROP, and only the four most significant variables were involved (GA, BW, RDS, and IVH) in predicting ROP. These four variables were widely accepted as risk factors for ROP in previous studies. Thus, other predictors, such as demographic profile, were not discussed in this paper. The authors have a sufficient sample size to conduct a multivariate analysis for the first (GA, BW, RDS, and IVH) and the second models (GA and BW). The coefficients were derived from the development model with a sample size of more than 500 samples. For the development model, the minimum analysis set was 506 out of 519 (97.5%). A previous study found that analyses that were conducted from samples of more than 500 had similar statistics to the parameters in the population (15). Thus, the coefficients that were derived from the analysis were considerably reliable and valid. Most notably, our prediction models were based on data from a single centre. External validation is required to improve the accuracy of these prediction models.
Conclusion
The two equation models that we developed are equally good and are sensitive in predicting the future incidence of ROP among babies. Model two is preferable because it only uses two predictors and these variables are easy and fast to capture. Although it is well known that BW and GA are the best predictors of ROP, our study has developed an effective and simple method to screen or predict preterm babies at risk of developing ROP based on these two variables.
Acknowledgement
We would like to thank the Director General of Health, Malaysia for the permission to publish this paper and all the medical officers, staff nurses and specialist of the eye department and the Pediatric department who helped us in this study. Besides that, we would like to extend our appreciation to Mr Hon Yoon Khee for his assistance to do language proof for this manuscript.
Footnotes
Conflicts of Interest
None.
Funds
None.
Authors’ Contributions
Conception and design, provision of study materials or patient: MP
Analysis and interpretation of the data: MAB
Drafting of the article, critical revision of the article for the important intellectual content, final approval of the article: MP, MAB, MAS. CMS, CLG, TAK
References
- 1.Terry TL. Extreme prematurity and fibroblastic overgrowth of persistent vascular sheath behind each crystalline lens I. Preliminary report. American Journal of Ophthalmology. 1942;25:203–204. doi: 10.1016/S0002-9394(42)92088-9. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, Zin A International NO-ROP Group. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115(5):518–525. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 3.Quinn GE. What do we do about ROP in larger birth weight babies? British Journal of Ophthalmology. 2002;86:1072–1073. doi: 10.1136/bjo.86.10.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haines L, Fielder AR, Scrivener R, Wilkinson AR. Royal College of Paediatrics and Child Health, the Royal College of Ophthalmologists and British Association of Perinatal Medicine Retinopathy of prematurity in the UK I: the organisation of services for screening and treatment. Eye. 2002;16(1):33–38. doi: 10.1038/sj.eye.6700030. [DOI] [PubMed] [Google Scholar]
- 5.Clinical Practice. Guidelines for Retinopathy of Prematurity. [Accessed February13, 2012]. Available at http://www.acadmed.org.my/view_file.cfm?fileid=259.
- 6.The Committee for the Classification of Retinopathy of Prematurity. An international classification of Retinopathy of Prematurity. Archives of Ophthalmology. 1984;102(8):1130–1134. doi: 10.1001/archopht.1984.01040030908011. [DOI] [PubMed] [Google Scholar]
- 7.The International Committee for the Classification of the Late Stages of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. II. The classification of retinal detachment. Archives of Ophthalmology. 1987;105(7):906–912. doi: 10.1001/archopht.1987.01060070041024. [DOI] [PubMed] [Google Scholar]
- 8.Yang CY, Lien R, Yang PH, Chu SM, Hsu JF, Fu RH, Chiang MC. Analysis of incidence and risk factors of retinopathy of prematurity among very-low-birth-weight infants in North Taiwan. Pediatrics and Neonatology. 2011;52(6):321–326. doi: 10.1016/j.pedneo.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Ebrahim M, Ahmad RS, Mohammad M. Incidence and risk factors of retinopathy of prematurity in Babol, North of Iran. Ophthalmic Epidemiology. 2010;17(3):166–170. doi: 10.3109/09286581003734860. [DOI] [PubMed] [Google Scholar]
- 10.Mccolm JR, Fleck BW. Retinopathy of prematurity: causation. Seminars in Neonatology. 2001;6(6):453–460. doi: 10.1053/siny.2001.0079. [DOI] [PubMed] [Google Scholar]
- 11.Campbell K. Intensive oxygen therapy as a possible cause for retrolental fibroplasias. A clinical approach. Medical Journal of Australia. 1951;2:48–50. Journal code: 0400714. L-ISSN: 0025-729X. [PubMed] [Google Scholar]
- 12.Brown DR, Biglan AW, Stretavsky MM. Retinopathy of prematurity: the relationship with intraventricular hemorrhage and bronchopulmonary dysplasia. Journal of Pediatric Ophthalmology and Strabismus. 1990;27(5):268–271. doi: 10.3928/0191-3913-19900901-13. [DOI] [PubMed] [Google Scholar]
- 13.Holmström G, Broberger U, Thomassen P. Neonatal risk factors for retinopathy of prematurity--a population-based study. Acta Ophthalmologica Scandinavica. 1998;76(2):204–207. doi: 10.1034/j.1600-0420.1998.760216.x. [DOI] [PubMed] [Google Scholar]
- 14.Zhu L, Shi WJ, Zhang SL, Yu LP, Yao MZ, Shi YY, Zeng XQ, Wang SN, Chen DM, Lin ZL, Ruan FQ, Huang QW, Qian Y, Chen C. Evaluation of risk factors for retinopathy of prematurity. Zhonghua Yi Xue Za Zhi. 2011;91(25):1749–1752. [PubMed] [Google Scholar]
- 15.Bujang MA, Ghani PA, Zolkepali NA, Selvarajah S, Haniff J. A comparison between convenience sampling versus systematic sampling in getting the true parameter in a population: explore from a clinical database: the Audit Diabetes Control Management (ADCM) registry in 2009. Proceedings of the International Conference Statistics Sciences Business Engineering. 2009;2012:15. doi: 10.1109/ICSSBE.2012.6396615. [DOI] [Google Scholar]