Abstract
Health disparities persist despite ongoing efforts. Given the United States’ rapidly changing demography and socio-cultural diversity, a paradigm shift in behavioral medicine is needed to advance research and interventions focused on health equity. This paper introduces the Con-NECT Framework as a model to link the sciences of behavioral medicine and health equity with the goal of achieving equitable health and outcomes in the twenty-first century. We first evaluate the state of health equity efforts in behavioral medicine science and identify key opportunities to advance the field. We then discuss and present actionable recommendations related to ConNECT’s five broad and synergistic principles: (1) Integrating Context; (2) Fostering a Norm of Inclusion; (3) Ensuring Equitable Diffusion of Innovations; (4) Harnessing Communication Technology; and (5) Prioritizing Specialized Training. The framework holds significant promise for furthering health equity and ushering in a new and refreshing era of behavioral medicine science and practice.
Keywords: Health equity, Disparities, ConNECT framework, Behavioral science, Diversity, Dissemination
Introduction
Health disparities—also referred to as health inequities—have been well documented for over thirty years, particularly among racial/ethnic minority and socioeconomically disadvantaged populations (Heckler, 1986). Health disparities/inequities are reflected in avoidable differences between more and less advantaged social groups in terms of length of life; quality of life; rates of disease, disability, and death; severity of disease; and access to treatment. Efforts to reduce health disparities are not new; however, perspectives focused on health equity have emerged more recently (Kumanyika, 2016). Health equity is social justice in health; it is achieved when health disparities are eliminated (not merely reduced), indicating equitable opportunities to attain optimal health regardless of social position or socially-determined circumstance (Braveman et al., 2011; Whitehead & Dahlgren, 2006). In this paper, we encompass disparities and inequities under the umbrella of health equity and present a practical, complementary framework to advance health equity.
Health disparities persist and for many diseases and populations are registering disturbing increases (Williams, 2012) despite targeted efforts (Institute of Medicine, 2003, 2012) and ongoing research (Ashing et al., 2015; Best et al., 2015; Fleisher et al., 2016; Gwede et al., 2015; Lu et al., 2015; Meade et al., 2015; Sly et al., 2015). Recent reports document widening health inequities in overall life expectancy (Kochanek et al., 2015; Olshansky et al., 2012) and specific diseases such as a widening disparity in breast cancer mortality between African Americans1 and whites (DeSantis et al., 2016), increasing diabetes incidence among individuals with the lowest income and education levels (Beckles & Chou, 2013), and worsening burden of sexually transmitted infections and cancer among men who have sex with men (Centers for Disease Control and Prevention, 2015; Quinn et al., 2015). These increasing inequities suggest an urgent need for new and more targeted approaches to stop these, and other, disconcerting trends.
The rapidly transforming demography of the United States shows the nation’s racial/ethnic composition as shifting from predominantly non-Hispanic White to an increasing diversity of multiple ethnic groups. By 2044, projections indicate racial/ethnic minorities will comprise more than 50 % of the U.S. population (Colby & Ortman, 2014). Such dramatic demographic shifts will lead to unprecedented challenges and opportunities in behavioral medicine, given that the overwhelming majority of behavioral medicine research has been among non-Hispanic Whites and greater emphasis will need to be placed on addressing health issues of diverse populations. Concomitant with this need, increasing recognition that other marginalized social groups (in terms of sexual minority status, disability status, immigration status, language, or other social, education, or literacy characteristics) also suffer persistent health disparities (Dilley et al., 2010; Froehlich-Grobe et al., 2013; Operario et al., 2015; Smith, 2010) necessitates more targeted attention to the health of such groups to achieve health equity. As such, there is a pressing need to better understand the changing context of our nation by embracing diversity, promoting inclusivity, and designing, delivering and rapidly disseminating effective healthcare interventions for all segments of the population, including population subgroups (Kumanyika, 2012).
Health inequities are protracted and entrenched in complex interactions of social, cultural, behavioral, biological, and environmental factors. Behavioral interventions aimed at health equity must recognize these complex factors—especially given the evolving diversity of our country—to be appropriate, effective, and sustainable. Behavioral medicine can provide theoretical and methodological guidelines to inform translational research and influence practice and policy to foster health equity. However, twenty-first century behavioral medicine needs an expanded paradigm that meaningfully considers diversity and harnesses multidisciplinary and multisectoral expertise to optimally address health inequities in the U.S. and, in turn, help achieve health equity.
Our paper addresses this urgent need by presenting a framework that complements behavioral medicine science and provides actionable strategies for framing, measuring, and addressing health inequities. The Ethnic Minority and Multicultural Health Special Interest Group of the Society of Behavioral Medicine (SBM) is poised and purposed to examine and address health within medically understudied and underserved racial/ethnic minority populations through research, education, training, and mentoring and by developing proactive and directed efforts in behavioral medicine science. In this paper, we summarize and evaluate the current state of health equity efforts in behavioral medicine science (i.e., strategies implemented to help achieve health equity), identify opportunities to better integrate health equity science into behavioral medicine that are consonant with emerging trends, and propose future directions for behavioral research to foster health equity.
Health equity efforts in behavioral medicine science
Persistent health disparities suggest there is room to enhance health equity research, practice, and policy in behavioral medicine across the continuum of care (i.e., from prevention to survivorship, supportive and palliative care). Given the increasing diversity of the U.S., more consistent integration of the sciences of health equity and behavioral medicine is both timely and important. In this section, we discuss the current state of health equity efforts within behavioral medicine science and identify key challenges and opportunities for better integration.
Early health equity research, including behavioral research, largely focused on identifying and describing health inequities—defined then as differences in health and health outcomes based on socioeconomic status (SES) or groups defined by race/ethnicity (Braveman, 2006) with little attention afforded to groups defined in broader terms such as disability status, sexual orientation, or gender identity. Health equity research has evolved to increasingly focus on efforts to eliminate health inequities by making specific (i.e., targeted) intervention efforts to improve the health of individuals or groups who are economically or socially disadvantaged. Health disparities remain the metric by which we measure progress toward health equity (Braveman, 2014), so continued surveillance documenting disparate health remains essential. However, growing consensus (Dankwa-Mullan et al., 2010; Ruffin, 2010; Srinivasan & Williams, 2014) calls for research that can specifically inform the development of evidence-based solutions to achieve health equity.
Studies of how behavioral, cognitive, psychosocial, inter- and intra-personal factors and policies contribute to health behavior and associated inequities are prevalent in the literature. Research to date has yielded valuable scientific knowledge such as evidence on the burden of health disparities across populations, identification of determinants of disparities, and some evidence-based behavioral approaches to addressing inequities. Still, much research has centered on broad racial/ethnic categories. Within-group heterogeneity also must be considered (e.g., Latinos, Asians, Blacks), given the increasing recognition of within-group inequities (e.g., between immigrant versus U.S.-born groups with similar racial or ethnic heritage). A more comprehensive understanding of, and attention to, within-group health disparities can foster health equity by ensuring that health needs of subgroups within larger population categories are not neglected. (However, particularly in clinical encounters, care must be taken to appreciate individual differences as well as similarities so as not to stereotype persons.)
Similarly, a relatively small proportion of behavioral medicine studies have considered health inequities in terms of contextual and non-individual factors such as the physical and social environment, or mechanisms driving these associations (Pampel et al., 2010). In fact, early health equity efforts (albeit not framed as ‘health equity’) stemmed from studies that identified different health outcomes among different social classes, particularly as related to sanitation conditions (James, 2009). Understanding social influences on disparities in health outcomes is vital to achieving health equity because social conditions and inequities underpin disparities in health. Yet our operationalization of, and attention to, social influences on health inequities has evolved rather slowly. For example, although SES is a construct operationalized in terms of income, education, and occupation, rarely do behavioral medicine studies measure SES in terms of all three components. Additionally, standard measures of SES (either individual components or a composite) are not used across studies.
The emergence of targeted recruitment strategies (Alcaraz et al., 2011; Yancey et al., 2006), community-based participatory research (CBPR) (Israel et al., 2001), culturally-competent communication (Teal & Street, 2009), and measurement tools validated for use in specific vulnerable populations reflect increasing awareness and appreciation for new approaches to understanding and addressing health inequities. Still, health equity-focused approaches are inadequately woven into behavioral medicine science. Seemingly common in behavioral research is the use of traditional approaches rather than those that explicitly and adequately consider health equity. For example, attention to context (e.g., ‘worldview’) can enhance understanding of determinants of health disparities and therefore facilitate efforts to achieve health equity (Kleinman, 1978). Pasick et al. (2009) found that in contradistinction to tenets of behavioral theory, social context could influence behavior directly; the researchers analogized that behavioral theory without the consideration of culture and context would be like having a traditional compass on Mars.
In sum, widespread recognition exists that health inequities stem from a complex interplay of multiple factors, which calls for new and nontraditional behavioral science approaches. Despite the promise of health equity-focused efforts that are underway, greater integration of these approaches is timely and critical for improving the health of our nation. We highlight in the upcoming sections several key and promising opportunities to facilitate progress toward this goal.
Opportunities for fostering health equity
To optimally foster health equity in the twenty-first century and level the playing field in behavioral medicine, we must maximize opportunities to more fully integrate health equity efforts into the fabric of behavioral medicine science. National research recommendations (National Institutes of Health, 2015) include bolstering applied research methods to identify practical and relevant strategies for achieving health equity. Additional opportunities exist for establishing more comprehensive understanding of a broader set of behavioral determinants to accelerate the development and implementation of health equity solutions. Further, more research is critically needed to elucidate how to intervene with vulnerable populations including identifying an array of evidence-based intervention strategies (e.g., interpersonal, systems, multilevel, community). Training and mentoring needs exist in these developing areas as well.
Additionally, there is a significant need to understand inequities beyond those framed in terms of race, ethnicity, and socioeconomic factors. For example, disparities suffered by sexual minority populations have only recently been considered for population-based surveillance (Dilley et al., 2010; Institute of Medicine, 2011). Within-group disparities (e.g., among Latino, Asian and Black subgroups, and among groups not defined in terms of race/ethnicity) are less often measured and therefore inadequately understood. These research opportunities hold substantial promise for identifying targeted, evidence-based, contextually-appropriate intervention strategies for distinct population subgroups. We conclude that a more focused and actionable paradigm that better integrates health equity efforts into behavioral medicine science is paramount and should highly build on burgeoning team science and transdisciplinary approaches.
Typically, health disparity and health equity tend to be studied by specialized groups or entities. Although this approach allows for the development of invaluable expertise and should continue, this knowledge needs to better and more quickly infuse other fields. We propose a bold approach where identifying and implanting health equity solutions is a consistent, cross-cutting, and vital theme for all special interest groups within SBM and other professional organizations, across all sectors of the National Institutes of Health (NIH), and throughout other agencies. This more unified approach is critically important to accelerate our advancement toward health equity.
The ConNECT Framework
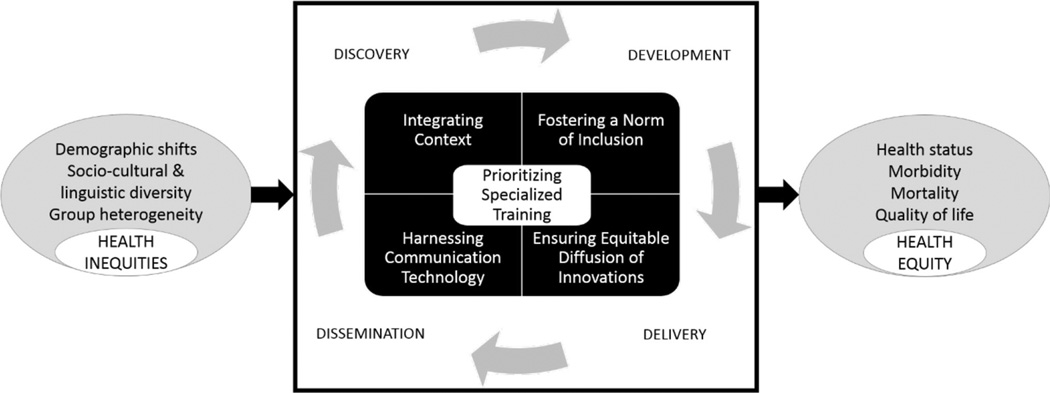
We propose the ConNECT Framework (Fig. 1) as an actionable model to (a) firmly link and ground the sciences of behavioral medicine and health equity; and (b) merge traditional/predominant behavioral medicine approaches with targeted strategies focused on marginalized subgroups to inform practice and policy to achieve health equity in the 21st century. ConNECT comprises five broad and synergistic health equity-focused principles:
Integrating CONtext: appreciate situational and interactive influences on health
Fostering a Norm of Inclusion: consistently engage and examine diverse groups
Ensuring Equitable Diffusion of Innovations: facilitate real-world benefit for all
Harnessing Communication Technology: optimize ecommunication for wide reach
Prioritizing Specialized Training: integrate education, training, and mentoring
Fig. 1.
The ConNECT Framework.
The framework’s principles are intended for use across the Translational Continuum, meaning from discovery (i.e., basic science) to dissemination (i.e., real-world application). Similarly, ConNECT principles are relevant at all stages of research and care delivery from prevention to palliative care/end-of-life. The framework considers the current state of health inequities; shifting demography; increasing cultural, literacy, and linguistic diversity; and between- and within-group heterogeneity that necessitate more inclusive and targeted approaches to eliminate inequities in health. Discussed below is each ConNECT principle in the context of behavioral medicine as well as the promise and application of each for achieving health equity. Table 1 provides examples of actionable recommendations that address gaps in current approaches and are specific to each principle as well as potential challenges and benefits.
Table 1.
Exemplar recommendations for application, potential benefits, and challenges of ConNECT Framework principles
| ConNECT principle | Current approaches and exemplar recommendations |
|---|---|
| Integrating Context | Current approach: predominant emphasis on individual-level determinants operating singularly with less attention to multilevel or synergistic influences |
| Consider: | |
| Targeting appropriate social and contextual determinants of health and causes of inequalities | |
| World view: culturally and socio-ecologically informed interventions that are culture-, place- and linguistic- based and population centered |
|
| Successful application: | |
| Is likely to foster greater acceptability, usability, efficacy, effectiveness and sustainability | |
| Challenge(s): | |
| Health inequities are fueled by complex multi-faceted factors that are difficult to address in one step or one study |
|
| Fostering a Norm of Inclusion | Current approach: intentional or unintentional exclusion of medically vulnerable and other marginalized groups in research |
| Consider: | |
| Maximizing diversity of participants/samples and appropriate representation in research to meaningfully reflect the burden of disease or inequities under study |
|
| Possible strategies may include over-sampling of certain groups (e.g., over-sampling Blacks/African Americans in a prostate cancer study, or in a study of diabetes, kidney disease or hypertension); and balancing representation by subgroups within a larger group (e.g., native-born vs. immigrant populations) |
|
| Successful application: | |
| Is likely to increase cultural, linguistic relevance and acceptability of findings or interventions | |
| Produces immediate understanding of diversity and possible early realization of benefits to diverse groups without delays related to future adaptations for subgroups |
|
| Challenge(s): | |
| Some groups are seen as ‘‘hard to reach’’ and may require greater resources afforded only by larger scale multi-center transdisciplinary collaborations, team science, partnerships, and community engagement |
|
| Similarly, some groups are not consistently recognized as medically vulnerable or underserved (e.g., due to sexual minority status) |
|
| Metrics for evaluating successful and meaningful inclusion still lacking | |
| Ensuring Equitable Diffusion of Innovations |
Current approach: emphasis on developing and disseminating evidence-based interventions for mainstream population and delayed translation/adaptation to other population groups |
| Consider: | |
| Community-based participatory research methods to partner with communities to plan for and design for dissemination from conceptualization to dissemination |
|
| Proactively use RE-AIM framework concurrently with the ConNECT Framework to as model for planning dissemination |
|
| Successful application: | |
| Helps identify barriers to dissemination and implementation, and facilitates crafting of solutions to promote early and broad dissemination efforts |
|
| Brings early benefits to broader communities without delay or waiting for adaptation processes | |
| Challenge(s): | |
| The prevailing paradigm calls for sequential approach that creates interventions for homogeneous groups then subsequently conducts adaptation for other groups if benefit is demonstrated |
|
| There is no consensus for delineating criteria for aggregating or disaggregating populations when developing initial interventions, i.e., when is a common intervention appropriate for diverse groups and when is it critical to desegregate populations or subgroups? |
|
| Establishing benefits and metrics for multisectoral stakeholders are required in community based dissemination |
|
| Harnessing Communication Technology |
Current approach: developing technology-based interventions for populations with moderate-to-high literacy and English proficiency |
| Consider: | |
| Leveraging the growing communication technologies such as smart phones and mobile health technologies that enhance reach and dissemination to achieve health equity |
|
| Increased reach through widespread (but intermittent) smartphone accessibility | |
| Apps and e-health or m-health interventions still need to be culturally-based and relevant; context, inclusion and reach are important considerations |
|
| Successful application: | |
| High speed Internet, apps, smartphones and certain social media platforms can build new connections to a broad range of communities and expand opportunities for greater reach |
|
| Increased engagement through interactivity increases awareness and opportunities to achieve health equity | |
| Challenge(s): | |
| The digital divide may reduce relevance of certain forms of communication (e.g., older and rural populations may lack smartphones, high speed Internet access, or Wi-Fi capabilities) |
|
| Prioritizing Specialized Training | Current approach: low integration of education, training, and mentoring to develop health equity expertise across sectors of behavioral medicine |
| Consider: | |
| Mentoring individuals from underrepresented groups and researchers committed to health equity to ensure broader transcultural relevance/competence and transdisciplinary expertise |
|
| Health equity and the socio-ecological framework as guiding principles for educating health care practitioners and researchers at all levels |
|
| Successful application: | |
| Effective mentoring can lead to greater diversity of leadership in major professional organizations and can facilitate advancement of health equity agenda |
|
| Improved outcomes and quality of care for populations and subgroups affected by inequities | |
| Challenge(s): | |
| Relatively few structured training programs exist focusing on dissemination and implementation and there is no consensus regarding relevant core competencies among professionals and for each participating sector |
Principle 1: integrating context
ConNECT’s first principle, integrating context, advocates greater emphasis on understanding social and contextual influences on health, which have been vastly understudied to date. Regulatory agencies recognize the value of considering determinants of health to inform workable and effective strategies, policies, and a comprehensive research agenda to improve population health and health equity (Institute of Medicine, 2006; Koh et al., 2011; National Institutes of Health, 2015). An important perspective for behavioral medicine is appreciating the importance of social determinants of health, which are structural economic and social conditions that influence the health of people and communities (Marmot et al., 2008). As examples, the impact of social structure on health inequities is exceedingly well documented in the literature, indicating that factors such as class and SES are clear and significant health determinants and need to be considered in both descriptive and intervention studies (Isaacs & Schroeder, 2004; Link & Phelan, 1995; Williams & Collins, 1995).
Beyond examining social determinants such as class and SES, more research is needed that conceptualizes, measures, and elucidates contextual determinants, which reflect the more proximal, surrounding circumstances and environments in which individuals engage and are exposed to risk or protective factors (Diez-Roux, 1998; Kagawa-Singer et al., 2015; Link & Phelan, 1995). These include influences such as persons’ lived experiences, social context (e.g., social environments, relationships, and interactions), and cultural and literacy factors that influence health (Burke et al., 2009; Mogford et al., 2011; Shareck et al., 2016). In recent years, a growing cadre of scholars has encouraged researchers to examine health inequities through a lens of intersectionality, a perspective that emphasizes the examination of multiple dimensions of social status and life experiences (Bauer, 2014; Bowleg, 2012; Rogers & Kelly, 2011; Williams et al., 2012). The use of intersectional approaches in health seek to understand how multiple social identities (e.g., gender, race/ethnicity, SES, disability, sexual identity, sexual orientation) intersect to simultaneously influence exposure to risk factors, access to health resources, and intervention response (Williams et al., 2012). For example, a recent population-based study of sexual minority health employed an intersectional approach to examine how gender, racial, and sexual identities interacted to influence disparate exposure to behavioral risks and access to care (Hsieh & Ruther, 2016).
Intersectional perspectives seem especially promising for understanding and addressing health inequities because historically marginalized and oppressed groups often are not examined in relation to other groups but rather within their own contexts (Bowleg, 2012). Intersectionality inherently appreciates within-group heterogeneity and therefore can result in a deeper understanding of behaviors of marginalized groups. However, implementing these intersectional approaches will be challenging initially due to limited existing theories, methods, and measures (Bowleg, 2012). Nevertheless, behavioral scientists have remarkable opportunities to develop this important area of research in the coming decades in an effort to eliminate health inequities.
Another context-based area with considerable opportunity and applicability to health equity is multilevel in nature as well (Gorin et al., 2012). The socioecological framework (Bronfenbrenner & Morris, 2006) views health and adaptation of individuals as the result of dynamic interactions between systems and processes ranging from the proximal social context (e.g., family, workplace), the community, and the larger context (e.g., culture, sociopolitical, economic). The socioecological perspective is an accepted framework in behavioral medicine science generally, yet there remains the need for a comprehensive understanding and integration of socioecological approaches in health equity efforts. Greater attention to understanding and intervening at multiple levels of influence is warranted to optimally address health inequities. This may require, for example, consistently assessing factors at multiple levels of influence, considering distal and proximal influences on health, and employing more dynamic conceptual models that move beyond identifying singular determinants to identifying how multiple determinants operate synergistically to influence health (Diez-Roux, 2012).
Understanding and assessing contextual determinants of health is a necessary—albeit underdeveloped—area in our efforts to disentangle ethnic, epigenetic, cultural and socioecological elements (Bell & Lee, 2011; Edwards & Di Ruggiero, 2011). As current mounting evidence directs our attention to investigate and address the impact of cultural and socioecological determinants on health, we are challenged to develop comprehensive theoretical frameworks that reflect these multidimensional perspectives. This will be important to adequately understand how socioecological contexts and cultural processes impact health outcomes to guide implementation strategies with increased focus on achieving health equity without unnecessary delay. A fuller appreciation of cultural and socioecological contexts has significant implications for population research for informing health outcomes assessments, intervention studies, and implementation and dissemination science (Dean et al., 2013; Marmot et al., 2008). This is yet another important area that requires greater attention in behavioral medicine. Enhancing current theoretical frameworks or, if needed, developing new frameworks can accelerate our understanding of health inequities and how to effectively address them.
Integrating and acknowledging context in behavioral medicine research holds promise to advance health equity. For example, not all individuals from racial/ethnic minority or other socially marginalized groups are at high (individual) risk, have poor health, or engage in negative health behaviors. By examining contextual influences on health within these groups, we can learn why some subgroups fare well and others fare poorly despite similar demographic characteristics, health insurance coverage, living conditions, or other often-studied factors. Positive deviance (an asset-based problem-solving approach), for example, employs a similar perspective to understand why certain individuals in communities can identify and implement effective strategies in the face of otherwise challenging conditions (Marsh et al., 2004).
Principle 2: fostering a norm of inclusion
The second ConNECT principle calls for more intentionally-inclusive efforts in behavioral medicine research. Several models attempt to address the burden of disease at the individual level including shared decision making (Elwyn et al., 2012), precision medicine (Jameson & Longo, 2015), and personalized medicine (Chan & Ginsburg, 2011). We now have universal health care via the Patient Protection & Affordable Care Act, which potentially offers expanded coverage to all persons in the U.S. including patients from historically underserved groups (Shaw et al., 2014). In the advent of a diverse and newly-insured patient population and the increasing diversity of the U.S. population overall, our current models may be inadequate because few explicitly consider cultural, contextual, and socioecological factors. For example, while someone may now have access to healthcare, preventive strategies may be unimportant or unacceptable for a variety of reasons such as culture or literacy. For instance, a person may have inadvertently signed up for insurance with a very high deductible, thus making care unaffordable still. Behavioral medicine science can play a central role in contributing to the generation of knowledge in this area to augment existing and emerging models for 21st century health care.
The exclusion of diverse populations in basic and clinical research limits our ability to achieve health equity. For example, failure of racial/ethnic minority women to enroll in large numbers in clinical trials of cancer may leave unanswered important questions related to the racial disparity in cancer survival. In the clinical trial in which tamoxifen (Nolvadex) was found to reduce breast cancer by nearly 50 % in high-risk women, Black American, Asian American, Latino, and other groups together made up only about 4 percent of participants (Fisher et al., 1998). Recently, it was reported that the HPV vaccine did not offer equal preventive benefit for Black girls because the high-risk strains impacted by the HPV vaccine are not the same as those that infect White girls (Vidal et al., 2014). Another example is that paradoxically, despite high incidence of disability among people with diabetes, individuals with diabetes who have a disability are disproportionately excluded from diabetes research because co-occurrence of disability often disqualifies them from clinical trial participation (Moore, 2012). Persons with limited English proficiency often are similarly excluded from research participation (Glickman et al., 2011). Therefore, the extent to which therapeutic and intervention effectiveness are generalizable to these sizeable, medically vulnerable populations is unclear. Gaps in knowledge delay the applicability and, more importantly, the benefit of scientific discoveries to population groups who already experience disparate health status and outcomes. A commitment to and mindset of inclusion can help ensure that this trend ends in the coming decades.
These examples clearly illustrate the need for a norm of inclusion in behavioral medicine. A diverse range of patient needs (e.g., culture, gender, SES, disability, sexual orientation, geography) should be included in best practices. In behavioral medicine research—specifically, clinical trials and cohort studies—researchers should normalize (e.g., proportional to extent of disease burden) the inclusion of diverse groups of participants to foster health equity in the future. We recognize this is often difficult for clinical researchers for a number of reasons: geographic and infrastructure impediments to equitable dissemination of clinical trials to underserved communities; referral patterns by providers who may not be adequately informed about availability of trials; and that many racial/ethnic minorities are distrusting of unique and experimental therapies (Schmotzer, 2012). In addition, some underserved and racial/ethnic populations face challenges with completing trials because of factors such as financial burden, lack of transportation and family responsibilities (Brown et al., 2000; Ford et al., 2008; Haring et al., 2016; Schmotzer, 2012; Sprague et al., 2013). Still, researchers must commit to making a deliberate change to including patients from diverse backgrounds to comprehensively understand their experiences of disease and treatment. A positive step in this direction is that a number of groups, such as the National Cancer Institute’s Community Oncology Research Program (now restructured under the NCORP enterprise), are making strides in creating meaningful partnerships among providers, cancer care investigators, and community organizations that care for diverse populations in health systems. NCORP centers highly on community engagement and awareness about the importance of equitable inclusion and dissemination of benefits to all populations (McCaskill-Stevens et al., 2013). Similarly, the NCI’s Geographical Management of Cancer Health Disparities Program (GMaP) comprises six regional networks for cancer health disparities research, training, and infrastructure (Wells et al., 2014).
Evidence suggests community-based participatory research (CBPR) methods hold promise for increasing inclusion of historically underrepresented and marginalized groups in behavioral medicine studies. CBPR-based strategies that have been successfully employed to recruit such groups include engaging lay community members to recruit participants, developing recruitment plans informed by local community advisory groups, recruiting via locally-relevant channels (e.g., radio, community-based venues), partnering with trusted local organizations and leaders to promote recruitment, and otherwise leveraging local social networks (Bryant et al., 2014; Greiner et al., 2014; Kreuter et al., 2012). Although the majority of published CBPR studies have been conducted with racial/ethnic minority and low-SES populations, emerging literature indicates CBPR methods can be similarly effective in recruiting participants from other underrepresented/marginalized groups such as sexual minority populations (Bryant et al., 2014; Rhodes et al., 2014), persons with disabilities (Nicolaidis et al., 2013), immigrants and refugees (Njeru et al., 2015), and individuals experiencing homelessness and co-occurring mental illness (Henwood et al., 2013). In a notable example underscoring the potential role of CBPR to foster inclusion, an evidential review of CBPR and smoking cessation interventions in marginalized communities found that studies with relatively low community involvement generally had challenges with participant recruitment (Andrews et al., 2012).
Fostering a norm of inclusion will not be without its challenges. Ubiquitous in the literature is the assertion that vulnerable populations are “hard to reach” and therefore not able to be enrolled in sizeable numbers in many research studies. However, this perspective implies that because different outreach strategies may be needed for different populations, it is essentially too difficult to be inclusive. To achieve health equity, this perspective must be recalibrated to one that makes diversity in research the norm. Suboptimal recruitment of diverse groups can no longer be an option. The U.S. government has taken steps to routinize the collection of data on sexual orientation and gender identity as standard demographic variables (Cahill et al., 2016). Additionally, the NIH has made positive strides towards inclusion by making the scientific justification for the inclusion or exclusion of women and racial/ethnic minorities a review criterion, rather than simply noting that such subgroups are present in the sample. Clear guidelines on acceptable levels of inclusion is an essential next step. Proactively partnering with researchers skilled in recruiting and retaining diverse samples, utilizing community-based partnerships to reach target populations, and employing culturally-salient evidence-based practices for recruitment are strategies that should be adopted widely to move us further along this positive trajectory of inclusion.
Principle 3: ensuring equitable diffusion of innovations
Equity in dissemination is the basis of ConNECT’s third principle. Multiple evidence-based interventions have been tested successfully in controlled settings with diverse populations, yet a significant gap remains in implementing these interventions in community and/or clinical practice settings (Napoles et al., 2013). The field of dissemination and implementation (D&I) science is designed to bridge the gap between research and practice, and is accomplished by attending to the first two ConNECT principles: context and inclusion. Dissemination is active spreading of evidence-based interventions to a specific audience, while implementation is the process of putting evidence-based interventions to use in a particular setting (Rabin et al., 2008).
D&I is an emerging area of science particularly suited to behavioral medicine research aimed at achieving health equity. D&I research and evaluation has challenges, however, especially as related to addressing health inequities (e.g., shared understanding among stakeholders, adequate resources). Sufficient pilot work, robust partnerships with communities and following strong D&I frameworks may help alleviate these barriers. Another critical challenge is distilling interventions to suit new settings and helping community members understand both the evidence base and necessary adaptations. The predominant convention is to complete efficacy interventions with mainstream populations first, then undertake cultural and linguistic adaptations for subgroups if successful (Kagawa-Singer et al., 2015). This sequential approach has its advantages but is clearly limiting in that it delays D&I by needing further adaptation to specific population subgroups. Another related and distinct barrier is the slow adaptation of interventions to meet diverse needs of unique subpopulations, especially those groups where homogeneity is often erroneously assumed, such as subgroups of Latinos, Asians and Blacks. As asserted by ConNECT’s second principle (Fostering a Norm of Inclusion), adequate inclusion of subgroups in meaningful numbers in original efficacy testing can only help in understanding health inequities and help move D&I forward more efficiently (Fleisher et al., 2016).
Inclusion of community perspectives in formative and developmental efforts before interventions are developed, tested, and finalized is important and can facilitate successful implementation. A variety of important perspectives of target communities and populations can also be captured in other paradigms and frameworks such as CBPR (Salimi et al., 2012), socioecological frameworks (Scholmerich & Kawachi, 2016), the Cultural Framework for Health (Kagawa-Singer et al., 2015), Persuasive Marketing (Jenkin et al., 2014), social marketing for systems change/community-based prevention marketing (Bryant et al., 2007) and the RE-AIM framework (Glasgow et al., 2003). However, ensuring D&I concepts are understood by communities is a critical aspect of D&I. Collaborating with stakeholders is an important step in the D&I process as the developers of the original intervention may not be aware of important cultural nuances that are needed to successfully adapt interventions that ultimately lead to more successful D&I.
Despite challenges, several models have been developed and tested to facilitate successful D&I. These include the aforementioned RE-AIM framework (Glasgow et al., 2003), which informs program development and evaluation, and the Evidence-Driven Community Health Improvement Process model, which incorporates RE-AIM into its evaluation (Layde et al., 2012). Incorporating model-based approaches at all phases of intervention development and testing could increase acceptability and facilitate dissemination as stakeholders would have contributed meaningful perspectives as collaborators from the early stages of the work (Phillips et al., 2014). Integration of context and inclusivity principles of the ConNECT Framework can help expedite and increase feasibility of D&I research. Perhaps the emphasis in traditional D&I research, which places the burden of uptake on communities, should shift focus to adapting interventions to particular settings and subgroups with heightened attention on community benefit (Atkins et al., 2016). These strategies have been successfully employed to reduce disparities in colorectal cancer screening in lower SES settings, among immigrant groups, among faith-based communities, and other multi-cultural settings (Berkowitz et al., 2015). Atkins and colleagues advocate for using ecological theory to reduce the gap between research and practice (Atkins et al., 2016).
Because D&I science remains a developing field of research, unanswered questions remain regarding the conduct of D&I in diverse settings and different population subgroups. To fill these gaps, the Centers for Disease Control has funded 10 Cancer Prevention and Control Research Networks across the U.S. to promote D&I. Supporting more of these types of programs can assist researchers and communities in bridging the gap between research and practice, thereby accelerating advancement toward health equity.
Principle 4: harnessing communication technology
ConNECT’s fourth principle recognizes the promise of utilizing communication technology in health equity efforts, which is integral and essential in addressing the first three principles of the ConNECT Framework: context, inclusion and equitable dissemination. The role of emerging technology in behavioral medicine has become commonplace with the development of web-based and mobile-enabled technology addressing a broad range of health related issues and conditions. In fact, interventions and approaches that are not technology based or enhanced are often viewed as less innovative and relevant due to the ubiquitous nature of communication technologies such as smartphones and other mobile devices.
Many terms (eHealth, mHealth) describe this growing field, while Connected Health has been used as a more expansive term. Connected Health is a model for healthcare delivery that uses technology to provide healthcare remotely with a goal to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care (Kvedar et al., 2014). The promise of Connected Health lies in the opportunity to reach broad (rural and urban) diverse audiences and contexts through widely available mobile devices and use of the expansive health related content available online. However, this promise has yet to be fully realized. Moreover, infrastructure issues add to the digital divide and equally important, few technology-based interventions are designed with appropriate contextual, cultural and linguistic approaches that facilitate the equitable utility and impact of these interventions across populations.
The overwhelming majority of Americans have wireless phones, and almost two-thirds own a smartphone (Pew Research Center, 2015) with similar penetration among racial/ethnic and income groups. For those with low household incomes and levels of education, smartphones may be the only access point for online resources and services. According to the Pew Internet (2015), some 13 % of Americans with an annual household income of less than $30,000 are smartphone-dependent; in comparison, just 1 % of Americans from households earning more than $75,000 per year rely on their smartphones to a similar degree for online access (Pew Research Center, 2015). Similar findings across race/ethnicity show that 12 % of African Americans and 13 % of Latinos are smartphone-dependent, compared with only 4 % of Whites (Pew Research Center, 2015). While they might be dependent on their smartphones to get online, access is often intermittent due to a combination of financial stresses and technical constraints. For instance, according to a Pew Internet study (Pew Research Center, 2015), 30 % of smartphone-dependent Americans report they “frequently” reach the limit of their data plan and over half say that this happens to them at least occasionally. A recent report from the Joint Center (Turner-Lee et al., 2012) highlights the opportunities of mobile health while recognizing needed policy changes (e.g., universal access to mobile broadband, incentives for providers to use mobile enabled technologies with patients and promote consumer education) to ensure health equity. Although these emergent communication technologies hold great promise, researchers and policy makers need to understand these issues and identify strategies to reduce the ongoing digital divide.
Although access to online communication technologies is foundational for Connected Health, equally important is the culturally, contextually and linguistically relevant content of interventions. The National Assessment of Adult Literacy (White, 2003) found that 43 % of adults have either basic or below basic health literacy skills, and older people, non-whites, immigrants, non-high school graduates, and those with low SES have higher rates of limited health literacy. Data from the 2012 Program for the International Assessment of Adult Competencies indicate persistently low levels of adult literacy (U.S. Department of Education, 2013). Coupled with a record 61.8 million U.S. residents (native-born, legal immigrants, and undocumented immigrants) speaking a language other than English at home—an increase of 2.2 million from 2010 (Camarota & Zeigler, 2014)— the need for culturally and linguistic relevant online content and behavioral interventions is staggering. Some web sites have content in multiple languages (e.g., http://nnlm.gov/outreach/consumer/multi.html), but these sites are limited and more informational than supporting theory-guided behavioral interventions (Gibbons et al., 2011).
Within the emerging body of literature examining the impact of Connected Health interventions on health behaviors, there is a focus on interventions designed specifically for underserved populations. Published studies have focused on a range of communication approaches, populations and health issues. A systematic review of health technology use by underserved health consumers, included 125 papers representing 30 types of technology, 19 historically undeserved groups and 23 health issues (Montague & Perchonok, 2012). A key recommendation from this review highlights the need to develop and test culturally-tailored Connected Health interventions, including more research “to create a culturally informed approach to the design of health technology geared toward historically underserved populations” (Montague & Perchonok, 2012).
Connected Health provides a promising opportunity to increase health equity through broad dissemination of health information and interventions, especially through mobile devices to populations suffering health inequities. Designing these interventions requires community engagement and health communication partnerships with communities to ensure they are salient (Fleisher et al., 2013). These technologies themselves can encourage a more participatory approach with the community through social media and other crowdsourcing methods. However, the cautionary tale is that infrastructure issues to ensure equal access will require ongoing attention.
Principle 5: prioritizing specialized training
The fifth and final ConNECT principle underscores the need for targeted workforce development via education, training, and mentoring to improve health equity. The ConNECT Framework principles presented in previous sections point at core competencies for behavioral medicine researchers and practitioners as well as the need for specialized training to meaningfully advance efforts to achieve health equity in the U.S. (U.S. Department of Health and Human Services, 2013). Effectively addressing health inequities requires academic institutions and policy makers to consider health equity (Braveman et al., 2011) and the socioecological framework as guiding principles for educating health care practitioners and researchers. Health equity efforts that consider and integrate multiple levels of analyses require specialized—and often multidisciplinary— expertise. Specialized education appropriate for elucidating multiple influences on health should be integral to training the next generation of behavioral medicine professionals, such as prior efforts in elucidating the intersection between culture and literacy in cancer care (Meade, 2005).
Training on multiple influences on health and multilevel interventions (Taplin et al., 2012) also is relevant to D&I, which (as noted earlier) is vital to achieving health equity. For two decades, researchers have emphasized the promise of D&I science for ensuring effective healthcare innovations and research findings reach the majority of individuals and communities in need. Congruent with the socioecological framework, D&I research necessitates a multilevel approach that recognizes factors at the level of the individual, organization, community, and society that influence the adoption, implementation, and sustainability of interventions. D&I, including leveraging communication technology in D&I efforts, should be an essential component of the education and training provided to current and future behavioral medicine professionals. Unfortunately, despite growing support for the importance of D&I science for efforts to eliminate health inequities, relatively few structured training programs exist in this area and there is no consensus regarding relevant core competencies (Padek et al., 2015). Gonzales et al. (2012) recently proposed an interdisciplinary framework for D&I training and education that recognizes the importance of taking a socioecological perspective to guide the design and implementation of research and intervention efforts. Importantly, the ability to establish effective transdisciplinary research collaborations and partnerships is an essential element of D&I training and education. In other words, the ability to develop successful partnerships with researchers and practitioners and key stakeholders in the community is essential for D&I research and practice.
CBPR can be a useful framework for facilitating D&I efforts to promote health equity. CBPR involves “a systematic effort to incorporate community participation and decision making, local theories of etiology and change, and community practices into the research” (Wallerstein & Duran, 2006, p 313). Key principles of CBPR include colearning, capacity building, shared decision making, trust, mutual benefit to all of those involved, and a sustained commitment to eliminate health disparities (Wallerstein & Duran, 2006). As such, CBPR can facilitate the dissemination, implementation, and sustainability of evidence-based interventions aimed at reducing health inequities. A commitment to incorporating CBPR training into behavioral medicine training and mentoring is critical to foster health equity.
Lastly, specialized training also should encompass the diverse cultural, literacy and linguistic needs among populations suffering inequities in health. Cultural and linguistic competence (CLC) is a core competency for effective efforts to eliminate health inequities and provide high quality services for all individuals and communities (U.S. Department of Health and Human Services, 2013). However, achieving CLC requires gaining an understanding of context, cultural values, norms, practices and beliefs, historical, sociopolitical and institutional forces that influence the health of individuals and communities (Harrell & Bond, 2006)—important tenets consistent with the Con-NECT Framework. Effective communication, patient-centered care, and community-based practices are core elements of education and training that can propel current and future health care professionals and researchers to achieve CLC (U.S. Department of Health and Human Services, 2013).
Multilevel approaches, D&I efforts, CBPR strategies, and cultural and linguistic competency hold promise for fostering health equity and provide the foundation upon which the ConNECT Framework may be implemented. In particular, these topics should be integrated into undergraduate, graduate, doctoral and post-doctoral program and medical school trainings to ensure future generations of behavioral medicine scientists and practitioners acquire needed expertise in these areas. Furthermore, for established clinicians, scientists and practitioners, ConNECT could be disseminated through webinars and trainings at conferences and professional association meetings. Although significant efforts are being made to elucidate key competencies for health researchers and practitioners aiming to reduce health inequities, gaps remain in the degree to which those recommendations have been adopted by educational institutions and training programs (Awosogba et al., 2013). Training programs must include an element of mentoring as rarely can a scientist move from theoretical training to application without mentored support. As we move forward, it is essential to prioritize trainings that jointly deliver content in in these areas (rather than separate courses) as the new thrust in behavioral medicine to achieve health equity in the twenty-first century.
Discussion
Achieving health equity in behavioral medicine requires integration of established evidence-based frameworks, new paradigms that expand the contextual breadth and centrality of social-ecology and culture, and dedicated training. Hence, this paper proposes the ConNECT Framework that leverages the richness and deep salience of diversity and culture to optimize the effective delivery of interventions directed at the individual, community, and system levels to achieve health equity. Existing frameworks may lack specificity and could benefit from pragmatic, directed, and systematic attention to core elements that explicitly consider diversity, inclusivity, and equity. ConNECT offers a new lens through which researchers and practitioners can implement salient interventions from preventive to end-of-life care and from discovery to dissemination. Researchers should use this framework concurrently with other theoretical and conceptual models to consider contextual determinants, foster a norm of inclusion (i.e., design interventions with the broadest possible inclusion and representation that reflects the diversity of populations affected by health inequities), and advance equitable dissemination of beneficial interventions to all.
Two additional pillars of the ConNECT Framework include leveraging ever-growing communication technologies (to reduce digital divide) and specialized training in health equity essential for dissemination and advancement of clinical and public health practice and policy. We assert that all five elements of the framework are essential to advance health equity across the continuum of behavioral medicine research and practice. Although the salience and relevance of the pillars may vary with each setting, researchers and practitioners should thoughtfully consider all five in planning, implementation, and evaluation. Ultimately, we have proposed an approach that connects and helps operationalize steps vital to advancing health equity in research and practice and informing policy, with broad relevance across the continuum of care.
The five ConNECT principles are a critical new integrated perspective. Although not a sequential, stepwise paradigm, it is important to implement the model during all project phases. This model is intended to help unify existing behavioral theories and conceptual frameworks in behavioral medicine and health equity science, and its principles allow for precise and practical focus on health equity. Too often, in behavioral medicine and health care in general, health equity is not a deliberate or prospectively planned goal. ConNECT seeks to allow for better planning and integration of health equity in the processes of research and care delivery, rather than reinforcing the prevailing mindset of measuring health equity solely for surveillance. The goal here is to promulgate a new researcher mindset that brings these principles to the forefront in a consistent and sustainable manner.
Conclusions
This paper provides an important synthesis of challenges, opportunities, and recommendations for achieving health equity in behavioral medicine. Researchers, clinicians, and public health practitioners can begin to examine how their efforts might incorporate and integrate the principles espoused here. Important next steps for behavioral medicine are to operationally employ this paradigm and evaluate how addition of these principles helps to achieve health equity. The utility of this framework lies in its simplicity and ease of integration with existing frameworks and conceptual tools all familiar to behavioral medicine. ConNECT adds a unique and important focus on advancing health equity and ensuring that the benefit of science and clinical/public health practice reach all segments of society in a rapid and timely manner. Application of this paradigm during early stages of team-oriented research is likely to reduce delays often associated with the incremental and sequential process of developing targeted interventions for population subgroups. National goals to achieve health equity are well documented (Heckler, 1986; Institute of Medicine, 2006, 2012; Kumanyika, 2012) and the Con-NECT Framework offers a new, promising lens and practical instrument to progress toward these aims.
Footnotes
In this paper we focus on the four major minority population groups in the U.S. Diversity in country of origin, ethnicity, culture, language as well as health and disease outcomes exists among and within each of these broad ethnic minority groups. However, for broad inclusion: (1) African American/Blacks (Black) are peoples of African descent and include persons from the U.S., African, Europe, Latina American and the Caribbean; (2) Asians/Pacific Islanders (Asian) include groups with ancestral original in Asia and the Pacific Islands; (3) Latinos/Hispanics (Latino) are peoples with ancestral ties to Latin America, Mexico and the Caribbean; and (4) Native American/Alaskan Natives (NA/AN) refer to the descendants of original peoples in North America.
Compliance with ethical standards
Human and animal rights and Informed consent This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest Kassandra I. Alcaraz, Jamilia Sly, Kimlin Ashing, Linda Fleisher, Virginia Gil-Rivas, Sabrina Ford, Jean C. Yi, Qian Lu, Cathy D. Meade, Usha Menon, and Clement K. Gwede declare that they do not have any conflict of interest.
References
- Alcaraz KI, Weaver NL, Andresen EM, Christopher K, Kreuter MW. The Neighborhood Voice: Evaluating a mobile research vehicle for recruiting African Americans to participate in cancer control studies. Evaluation and the Health Professions. 2011;34:336–348. doi: 10.1177/0163278710395933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews JO, Newman SD, Heath J, Williams LB, Tingen MS. Community-based participatory research and smoking cessation interventions: A review of the evidence. Nursing Clinics of North America. 2012;47:81–96. doi: 10.1016/j.cnur.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashing KT, Lai L, Brown S, McDowell K, Carter D, Smith J, et al. Developing a treatment summary and survivorship care plan responsive to African-American breast cancer survivors. Psychooncology. 2015 doi: 10.1002/pon.3939. [DOI] [PubMed] [Google Scholar]
- Atkins MS, Rusch D, Mehta TG, Lakind D. Future directions for dissemination and implementation science: Aligning ecological theory and public health to close the research to practice gap. Journal of Clinical Child & Adolescent Psychology. 2016;45:215–226. doi: 10.1080/15374416.2015.1050724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awosogba T, Betancourt JR, Conyers FG, Estape ES, Francois F, Gard SJ, et al. Prioritizing health disparities in medical education to improve care. Annals of the New York Academy of Sciences. 2013;1287:17–30. doi: 10.1111/nyas.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer GR. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science and Medicine. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Beckles GL, Chou CF. Diabetes—United States, 2006 and 2010. MMWR Supplements. 2013;62:99–104. [PubMed] [Google Scholar]
- Bell J, Lee MM. Why place and race matter: Impacting health through a focus on race and place. Oakland, CA: PolicyLink; 2011. [Google Scholar]
- Berkowitz SA, Percac-Lima S, Ashburner JM, Chang Y, Zai AH, He W, et al. Building equity improvement into quality improvement: Reducing socioeconomic disparities in colorectal cancer screening as part of population health management. Journal of General Internal Medicine. 2015;30:942–949. doi: 10.1007/s11606-015-3227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best AL, Alcaraz KI, McQueen A, Cooper DL, Warren RC, Stein K. Examining the mediating role of cancer-related problems on spirituality and self-rated health among African American cancer survivors: A report from the American Cancer Society’s Studies of Cancer Survivors-II. Psychooncology. 2015;24:1051–1059. doi: 10.1002/pon.3720. [DOI] [PubMed] [Google Scholar]
- Bowleg L. The problem with the phrase women and minorities: Intersectionality—an important theoretical framework for public health. American Journal of Public Health. 2012;102:1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P. Health disparities and health equity: concepts and measurement. Annual Review of Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Braveman P. What are health disparities and health equity? We need to be clear. Public Health Reports. 2014;129:5–8. doi: 10.1177/00333549141291S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, Kumanyika S, Fielding J, Laveist T, Borrell LN, Manderscheid R, et al. Health disparities and health equity: The issue is justice. American Journal of Public Health. 2011;101:S149–S155. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, Morris PA. The bioecological model of human development. In: Damon W, Lerner RM, editors. Handbook of child psychology, Vol. 1: Theoretical models of human development. 6th. New York: Wiley; 2006. pp. 793–828. [Google Scholar]
- Brown DR, Fouad MN, Basen-Engquist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Annals of Epidemiology. 2000;10:S13–S21. doi: 10.1016/s1047-2797(00)00197-6. [DOI] [PubMed] [Google Scholar]
- Bryant CA, Brown KR, McDermott RJ, Forthofer MS, Bumpus EC, Calkins SA, et al. Community-based prevention marketing: Organizing a community for health behavior intervention. Health Promotion Practice. 2007;8:154–163. doi: 10.1177/1524839906290089. [DOI] [PubMed] [Google Scholar]
- Bryant L, Damarin AK, Marshall Z. Tobacco control recommendations identified by LGBT Atlantans in a community-based participatory research project. Progress in Community Health Partnerships. 2014;8:269–279. doi: 10.1353/cpr.2014.0041. [DOI] [PubMed] [Google Scholar]
- Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: rethinking behavioral theory. Health Education & Behavior. 2009;36:55s–70s. doi: 10.1177/1090198109335338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: A huge step forward for LGBT health. LGBT Health. 2016;3:100–102. doi: 10.1089/lgbt.2015.0136. [DOI] [PubMed] [Google Scholar]
- Camarota SA, Zeigler K. One in Five U.S. Residents Speaks Foreign Language at Home, Record 61.8 million. Washington, D.C: 2014. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2014. Atlanta: 2015. [Google Scholar]
- Chan IS, Ginsburg GS. Personalized medicine: Progress and promise. Annual Review of Genomics and Human Genetics. 2011;12:217–244. doi: 10.1146/annurev-genom-082410-101446. [DOI] [PubMed] [Google Scholar]
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. Population: 2014 to 2060. Washington, D.C: US Census Bureau; 2014. [Google Scholar]
- Dankwa-Mullan I, Rhee KB, Stoff DM, Pohlhaus JR, Sy FS, Stinson N., Jr Moving toward paradigm-shifting research in health disparities through translational, transformational, and transdisciplinary approaches. American Journal of Public Health. 2010;100:S19–S24. doi: 10.2105/AJPH.2009.189167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean HD, Williams KM, Fenton KA. From theory to action: Applying social determinants of health to public health practice. Public Health Reports. 2013;128:1–4. doi: 10.1177/00333549131286S301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: A Cancer Journal for Clinicians. 2016 doi: 10.3322/caac.21340. [DOI] [PubMed] [Google Scholar]
- Diez-Roux AV. Bringing context back into epidemiology: Variables and fallacies in multilevel analysis. American Journal of Public Health. 1998;88:216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV. Conceptual approaches to the study of health disparities. Annual Review of Public Health. 2012;33:41–58. doi: 10.1146/annurev-publhealth-031811-124534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. American Journal of Public Health. 2010;100:460–467. doi: 10.2105/AJPH.2007.130336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards N, Di Ruggiero E. Exploring which context matters in the study of health inequities and their mitigation. Scandinavian Journal of Public Health. 2011;39:43–49. doi: 10.1177/1403494810393558. [DOI] [PubMed] [Google Scholar]
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: A model for clinical practice. Journal of General Internal Medicine. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. Journal of the National Cancer Institute. 1998;90:1371–1388. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- Fleisher L, Bass SB, Gonzales E, Davis S, Slamon R, Jibaja-Weiss M, Gibbons M. Best practices in culturally appropriate health education approaches. In: Kinsey P, Louden DM, editors. Ethnicity, health, and well-being—An African American Perspective. Lincoln: Lincoln University Press; 2013. [Google Scholar]
- Fleisher L, Davis SN, Gross L, Bagden L, Zakrzewski D, Gonzalez E, et al. Lessons learned from implementing a prostate cancer risk assessment program for underserved high-risk men in the community: The Prostate REACH Project. Journal of Cancer Education. 2016;31:191–197. doi: 10.1007/s13187-015-0854-8. [DOI] [PubMed] [Google Scholar]
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- Froehlich-Grobe K, Lee J, Washburn RA. Disparities in obesity and related conditions among Americans with disabilities. American Journal of Preventive Medicine. 2013;45:83–90. doi: 10.1016/j.amepre.2013.02.021. [DOI] [PubMed] [Google Scholar]
- Gibbons MC, Fleisher L, Slamon RE, Bass S, Kandadai V, Beck JR. Exploring the potential of Web 2.0 to address health disparities. Journal of Health Communications. 2011;16(Suppl 1):77–89. doi: 10.1080/10810730.2011.596916. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health. 2003;93:1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glickman SW, Ndubuizu A, Weinfurt KP, Hamilton CD, Glickman LT, Schulman KA, et al. Perspective: The case for research justice: Inclusion of patients with limited English proficiency in clinical research. Academic Medicine. 2011;86:389–393. doi: 10.1097/ACM.0b013e318208289a. [DOI] [PubMed] [Google Scholar]
- Gonzales R, Handley MA, Ackerman S, O’Sullivan PS. A framework for training health professionals in implementation and dissemination science. Academic Medicine. 2012;87:271–278. doi: 10.1097/ACM.0b013e3182449d33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin SS, Badr H, Krebs P, Prabhu Das I. Multilevel interventions and racial/ethnic health disparities. Journal of the National Cancer Institute Monographs. 2012;2012:100–111. doi: 10.1093/jncimonographs/lgs015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greiner KA, Friedman DB, Adams SA, Gwede CK, Cupertino P, Engelman KK, et al. Effective recruitment strategies and community-based participatory research: Community networks program centers’ recruitment in cancer prevention studies. Cancer Epidemiology, Biomarkers and Prevention. 2014;23:416–423. doi: 10.1158/1055-9965.EPI-13-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwede CK, Koskan AM, Quinn GP, Davis SN, Ealey J, Abdulla R, et al. Patients’ perceptions of colorectal cancer screening tests and preparatory education in federally qualified health centers. Journal of Cancer Education. 2015;30:294–300. doi: 10.1007/s13187-014-0733-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haring RC, Henry WA, Hudson M, Rodriguez EM, Taualii M. Views on clinical trial recruitment, biospecimen collection, and cancer research: Population science from landscapes of the Haudenosaunee (People of the Longhouse) Journal of Cancer Education. 2016 doi: 10.1007/s13187-016-1067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP, Bond MA. Listening to diversity stories: Principles for practice in community research and action. American Journal of Community Psychology. 2006;37:365–376. doi: 10.1007/s10464-006-9042-7. [DOI] [PubMed] [Google Scholar]
- Heckler MM. Report of the secretary’s task force on black and minority health. Morbidity and Mortality Weekly Report. 1986;35:109–112. [PubMed] [Google Scholar]
- Henwood BF, Stanhope V, Brawer R, Weinstein LC, Lawson J, Stwords E, et al. Addressing chronic disease within supportive housing programs. Progress in Community Health Partnerships. 2013;7:67–75. doi: 10.1353/cpr.2013.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh N, Ruther M. Sexual minority health and health risk factors: Intersection effects of gender, race, and sexual identity. American Journal of Preventive Medicine. 2016;50:746–755. doi: 10.1016/j.amepre.2015.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press (US); 2003. [PubMed] [Google Scholar]
- Institute of Medicine. The National Academies Collection: Reports funded by National Institutes of Health. In: Hernandez LM, Blazer DG, editors. Genes, behavior, and the social environment: Moving beyond the nature/nurture debate. Washington, DC: National Academies Press (US); 2006. [PubMed] [Google Scholar]
- Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press (US); 2011. The National Academies Collection: Reports funded by National Institutes of Health. [PubMed] [Google Scholar]
- Institute of Medicine. How far have we come in reducing health disparities? Progress since 2000: Workshop summary. Washington, DC: National Academies Press (US); 2012. The National Academies Collection: Reports funded by National Institutes of Health. [PubMed] [Google Scholar]
- Isaacs SL, Schroeder SA. Class—the ignored determinant of the nation’s health. New England Journal of Medicine. 2004;351:1137–1142. doi: 10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Education for Health (Abingdon) 2001;14:182–197. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]
- James SA. Epidemiologic research on health disparities: Some thoughts on history and current developments. Epidemiologic Reviews. 2009;31:1–6. doi: 10.1093/epirev/mxp010. [DOI] [PubMed] [Google Scholar]
- Jameson JL, Longo DL. Precision medicine–personalized, problematic, and promising. New England Journal of Medicine. 2015;372:2229–2234. doi: 10.1056/NEJMsb1503104. [DOI] [PubMed] [Google Scholar]
- Jenkin G, Madhvani N, Signal L, Bowers S. A systematic review of persuasive marketing techniques to promote food to children on television. Obesity Reviews. 2014;15:281–293. doi: 10.1111/obr.12141. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Dressler WW, George SM, Elwood WN with the assistance of a specially appointed expert panel. The cultural framework for health: An integrative approach for research and program design and evaluation. Bethesda: 2015. [Google Scholar]
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science and Medicine. 1978;12:85–95. doi: 10.1016/0160-7987(78)90014-5. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Anderson RN, Arias E. Leading causes of death contributing to decrease in life expectancy gap between black and white populations: United States, 1999–2013. NCHS Data Brief. 2015;218:1–8. [PubMed] [Google Scholar]
- Koh HK, Piotrowski JJ, Kumanyika S, Fielding JE. Healthy people: A 2020 vision for the social determinants approach. Health Education & Behavior. 2011;38:551–557. doi: 10.1177/1090198111428646. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Kegler MC, Joseph KT, Redwood YA, Hooker M. The impact of implementing selected CBPR strategies to address disparities in urban Atlanta: A retrospective case study. Health Education Research. 2012;27:729–741. doi: 10.1093/her/cys053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumanyika S. Health disparities research in global perspective: New insights and new directions. Annual Review of Public Health. 2012;33:1–5. doi: 10.1146/annurev-publhealth-112911-155504. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK. Health equity is the issue we have been waiting for. Journal of Public Health Management and Practice. 2016;22(Suppl 1):S8–S10. doi: 10.1097/PHH.0000000000000363. [DOI] [PubMed] [Google Scholar]
- Kvedar J, Coye MJ, Everett W. Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Affairs (Millwood) 2014;33:194–199. doi: 10.1377/hlthaff.2013.0992. [DOI] [PubMed] [Google Scholar]
- Layde PM, Christiansen AL, Peterson DJ, Guse CE, Maurana CA, Brandenburg T. A model to translate evidence-based interventions into community practice. American Journal of Public Health. 2012;102:617–624. doi: 10.2105/AJPH.2011.300468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, Spec No. 1995;35:80–94. [PubMed] [Google Scholar]
- Lu Q, Yeung NC, You J, Dai J. Using expressive writing to explore thoughts and beliefs about cancer and treatment among Chinese American immigrant breast cancer survivors. Psychooncology. 2015 doi: 10.1002/pon.3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ. 2004;329:1177–1179. doi: 10.1136/bmj.329.7475.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaskill-Stevens W, Lyss AP, Good M, Marsland T, Lilenbaum R. The NCI Community Oncology Research Program: What every clinician needs to know. American Society of Clinical Oncology Educational Book. 2013 doi: 10.14694/EdBook_AM.2013.33.e84. [DOI] [PubMed] [Google Scholar]
- Meade CD. Cancer, culture and literacy: Critical next steps in improving care for diverse populations. Cancer Control. 2005;12:4–5. doi: 10.1177/1073274805012004S01. [DOI] [PubMed] [Google Scholar]
- Meade CD, Rodriguez EM, Arevalo M, Luque JS, Harris N, San Miguel G, et al. Introducing biospecimen science to communities: Tools from two cities. Progress in Community Health Partnerships. 2015;9:51–59. doi: 10.1353/cpr.2015.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogford E, Gould L, Devoght A. Teaching critical health literacy in the US as a means to action on the social determinants of health. Health Promotion International. 2011;26:4–13. doi: 10.1093/heapro/daq049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montague E, Perchonok J. Health and wellness technology use by historically underserved health consumers: systematic review. J Med Internet Res. 2012;14:e78. doi: 10.2196/jmir.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SM. Scientific reasons for including persons with disabilities in clinical and translational diabetes research. Journal of Diabetes Science and Technology. 2012;6:236–241. doi: 10.1177/193229681200600204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napoles AM, Santoyo-Olsson J, Stewart AL. Methods for translating evidence-based behavioral interventions for health-disparity communities. Preventing Chronic Disease. 2013;10:E193. doi: 10.5888/pcd10.130133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. NIH-wide strategic plan fiscal years 2016–2020. 2015 Retrieved from https://www.nih.gov/sites/default/files/about-nih/strategic-plan-fy2016-2020-508.pdf.
- Nicolaidis C, Raymaker D, McDonald K, Dern S, Boisclair WC, Ashkenazy E, et al. Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. Journal of General Internal Medicine. 2013;28:761–769. doi: 10.1007/s11606-012-2262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njeru JW, Patten CA, Hanza MM, Brockman TA, Ridgeway JL, Weis JA, Wieland ML. Stories for change: Development of a diabetes digital storytelling intervention for refugees and immigrants to minnesota using qualitative methods. BMC Public Health. 2015;15:1311. doi: 10.1186/s12889-015-2628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs (Millwood) 2012;31:1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- Operario D, Gamarel KE, Grin BM, Lee JH, Kahler CW, Marshall BD, et al. Sexual minority health disparities in adult men and women in the United States: National Health and Nutrition Examination Survey, 2001–2010. American Journal of Public Health. 2015;105:e27–e34. doi: 10.2105/AJPH.2015.302762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padek M, Colditz G, Dobbins M, Koscielniak N, Proctor EK, Sales AE, et al. Developing educational competencies for dissemination and implementation research training programs: An exploratory analysis using card sorts. Implementation Science. 2015;10:114. doi: 10.1186/s13012-015-0304-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasick RJ, Burke NJ, Barker JC, Joseph G, Bird JA, Otero-Sabogal R, et al. Behavioral theory in a diverse society: Like a compass on Mars. Health Education & Behavior. 2009;36:11s–35s. doi: 10.1177/1090198109338917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Internet. Americans’ Internet Access: 2000–2015. 2015 [Google Scholar]
- Pew Research Center. U.S. Smartphone Use in 2015. 2015 [Google Scholar]
- Phillips SM, Alfano CM, Perna FM, Glasgow RE. Accelerating translation of physical activity and cancer survivorship research into practice: Recommendations for a more integrated and collaborative approach. Cancer Epidemiology, Biomarkers and Prevention. 2014;23:687–699. doi: 10.1158/1055-9965.EPI-13-1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, Schabath MB. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA: A Cancer Journal for Clinicians. 2015;65(5):384–400. doi: 10.3322/caac.21288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. Journal of Public Health Management and Practice. 2008;14:117–123. doi: 10.1097/01.PHH.0000311888.06252.bb. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Alonzo J, Mann L, Downs M, Siman FM, Andrade M, et al. Novel approaches to HIV prevention and sexual health promotion among Guatemalan gay and bisexual men, MSM, and transgender persons. AIDS Education and Prevention. 2014;26:345–361. doi: 10.1521/aeap.2014.26.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J, Kelly UA. Feminist intersectionality: Bringing social justice to health disparities research. Nursing Ethics. 2011;18:397–407. doi: 10.1177/0969733011398094. [DOI] [PubMed] [Google Scholar]
- Ruffin J. The science of eliminating health disparities: Embracing a new paradigm. American Journal of Public Health. 2010;100:S8–S9. doi: 10.2105/AJPH.2010.191957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salimi Y, Shahandeh K, Malekafzali H, Loori N, Kheiltash A, Jamshidi E, et al. Is community-based participatory research (CBPR) Useful? A systematic review on papers in a decade. International Journal of Preventive Medicine. 2012;3:386–393. [PMC free article] [PubMed] [Google Scholar]
- Schmotzer GL. Barriers and facilitators to participation of minorities in clinical trials. Ethnicity and Disease. 2012;22:226–230. [PubMed] [Google Scholar]
- Scholmerich VL, Kawachi I. Translating the socioecological perspective into multilevel interventions: Gaps between theory and practice. Health Education & Behavior. 2016;43:17–20. doi: 10.1177/1090198115605309. [DOI] [PubMed] [Google Scholar]
- Shareck M, Kestens Y, Vallee J, Datta G, Frohlich KL. The added value of accounting for activity space when examining the association between tobacco retailer availability and smoking among young adults. Tobacco Control. 2016;25:406–412. doi: 10.1136/tobaccocontrol-2014-052194. [DOI] [PubMed] [Google Scholar]
- Shaw FE, Asomugha CN, Conway PH, Rein AS. The Patient Protection and Affordable Care Act: opportunities for prevention and public health. Lancet. 2014;384:75–82. doi: 10.1016/S0140-6736(14)60259-2. [DOI] [PubMed] [Google Scholar]
- Sly J, Jandorf L, Erwin DO. Who’s missing? Predictors of attrition following participation in culturally targeted educational breast and cervical cancer outreach programs for latinas. Journal of Health Communications. 2015;20:851–858. doi: 10.1080/10810730.2015.1018596. [DOI] [PubMed] [Google Scholar]
- Smith DL. Health care disparities for persons with limited English proficiency: Relationships from the 2006 Medical Expenditure Panel Survey (MEPS) Journal of Health Disaprities Research and Practice. 2010;3:57–67. [Google Scholar]
- Sprague D, Russo J, LaVallie DL, Buchwald D. Barriers to cancer clinical trial participation among American Indian and Alaska Native tribal college students. The Journal of Rural Health. 2013;29:55–60. doi: 10.1111/j.1748-0361.2012.00432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan S, Williams SD. Transitioning from health disparities to a health equity research agenda: The time is now. Public Health Reports. 2014;129:71–76. doi: 10.1177/00333549141291S213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taplin SH, Anhang Price R, Edwards HM, Foster MK, Breslau ES, Chollette V, et al. Introduction: Understanding and influencing multilevel factors across the cancer care continuum. Journal of the National Cancer Institute Monographs. 2012;2012:2–10. doi: 10.1093/jncimonographs/lgs008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teal CR, Street RL. Critical elements of culturally competent communication in the medical encounter: A review and model. Social Science and Medicine. 2009;68:533–543. doi: 10.1016/j.socscimed.2008.10.015. [DOI] [PubMed] [Google Scholar]
- Turner-Lee N, Smedley BD, Miller J. Minorities, mobile broadband and the management of chronic diseases. Washington, DC: Joint Center for Political and Economic Studies; 2012. [Google Scholar]
- U.S. Department of Education. Literacy, Numeracy, and Problem Solving in Technology-Rich Environments Among U.S. Adults. Washington, DC: 2013. [Google Scholar]
- U.S. Department of Health and Human Services. The National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care. 2013 Retrieved from https://www.thinkculturalhealth.hhs.gov/pdfs/EnhancedCLASStandardsBlueprint.pdf.
- Vidal AC, Smith JS, Valea F, Bentley R, Gradison M, Yarnall KS, et al. HPV genotypes and cervical intraepithelial neoplasia in a multiethnic cohort in the south-eastern USA. Cancer Causes and Control. 2014;25:1055–1062. doi: 10.1007/s10552-014-0406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promotion Practice. 2006;7:312–323. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- Wells KJ, Lima DS, Meade CD, Munoz-Antonia T, Scarinci I, McGuire A, et al. Assessing needs and assets for building a regional network infrastructure to reduce cancer related health disparities. Evaluation and Program Planning. 2014;44:14–25. doi: 10.1016/j.evalprogplan.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S. In: The 2003 National Assessment of Adult Literacy (NAAL) (NCES 2003-495r) U.S. Department of Education, editor. Washington, DC: 2003. [Google Scholar]
- Whitehead M, Dahlgren G. Levelling Up (Part 1): A Discussion paper on concepts and principles for tackling social inequities in health. Denmark: 2006. [Google Scholar]
- Williams DR. Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior. 2012;53:279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: Patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- Williams DR, Kontos EZ, Viswanath K, Haas JS, Lathan CS, MacConaill LE, et al. Integrating multiple social statuses in health disparities research: The case of lung cancer. Health Services Research. 2012;47:1255–1277. doi: 10.1111/j.1475-6773.2012.01404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]