Abstract
A 45-year-old woman was admitted due to severe headache and neck stiffness. She had visited a local clinic for back pain and received a lumbar nerve root steroid injection 10 days before admission. Computed tomography and magnetic resonance imaging showed psoas abscess, pneumocephalus, and subdural hygroma. She was diagnosed with psoas abscess and meningitis. The abscess and external ventricle were drained, and antibiotics were administered. Unfortunately, the patient died on hospital day 19 due to diffuse leptomeningitis. Lumbar nerve root steroid injections are commonly used to control back pain. Vigilance to "red flag signs" and a rapid diagnosis can prevent lethal outcomes produced by rare and unexpected complications related to infection. Here, we report a case of fatal meningitis after infection of the cerebrospinal fluid following a lumbar nerve root steroid injection.
Keywords: Cerebrospinal fluid, Infection, Nerve root steroid injection, Psoas abscess
Lumbar nerve root block is a useful modality for evaluating pain due to disorders involving the lumbar spine or spinal nerves. Corticosteroids are widely used as nerve block agents due to their anti-inflammatory and possible analgesic actions, but large doses or prolonged administration can result in significant side effects. Lumbar nerve root steroid injections are commonly used to control back pain. This type of block can be performed with the patient in the prone or lateral position, under fluoroscopic guidance, to identify specific vertebral levels and reduce unintentional intrathecal or intravascular injection. Unfortunately, several complications, such as bleeding, inflammation, or infection, can occur after a nerve block. Spinal or epidural hematoma, meningitis, arachnoiditis, and an epidural abscess are rare but potentially devastating complications. Thus, careful attention and timely follow-up are needed to reduce the risk of complications during and after a nerve block.
Case Report
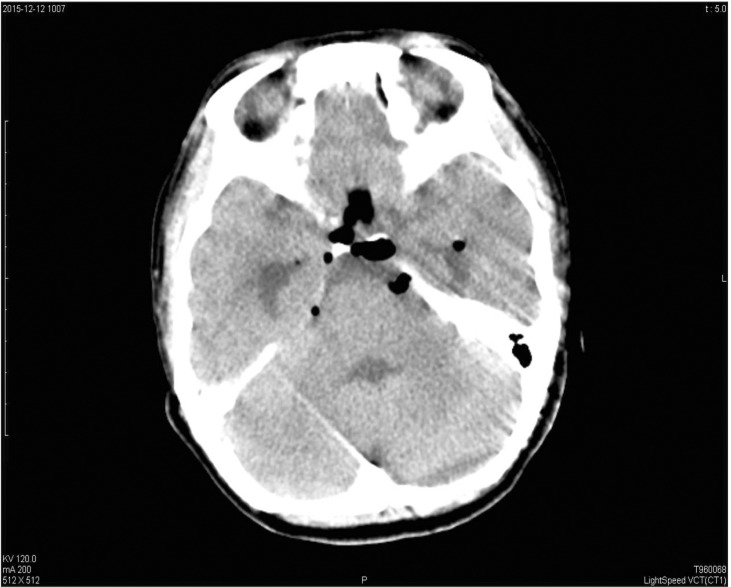
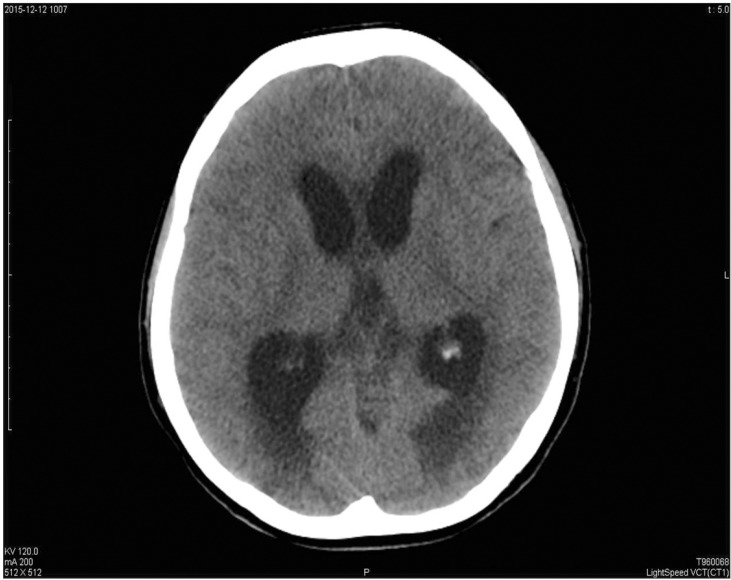
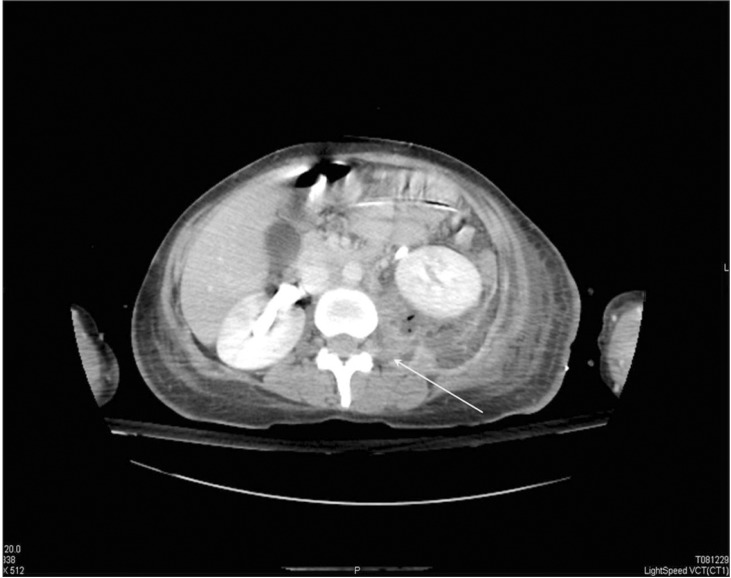
A 45-year-old female (height, 155 cm; weight, 48 kg) was admitted to our emergency department due to severe headache and irritability. She had visited a local clinic due to lower back pain radiating to the left thigh 10 days before visiting our hospital after 1,000 bows (kneeling to pray in a Buddhist temple) and received a lumbar nerve root steroid injection consisting of a mixture of 40 mg triamcinolone in 3 cc of 0.5% lidocaine on the left side at the L3–4 level, without screening for vertebral disorders by magnetic resonance imaging (MRI). The patient revisited the same clinic 7 and 2 days before admission to our hospital with newly developed neck stiffness and constant lower back pain, respectively, and was treated with a lumbar trigger point injection of 0.5% lidocaine and physical therapy. She showed no improvement and was transferred to our hospital due to severe headache that improved when lying down and worsened when sitting upright. On admission, she was alert but irritable. Bed rest and fluid therapy was prescribed as conservative treatment before a neurosurgeon considered meningitis combined with previously diagnosed pneumocephalus on a brain computed tomography (CT) scan. The treatment did not lead to improvement. Motor and sensory neurological signs and pupil reflexes were normal, except mild nuchal rigidity. She was diagnosed with systemic inflammatory response syndrome and neutrophilia, with a white cell count of 17,000/µl (reference range, 4,000–10,000/µl), a differential of 90.7% neutrophils and a C-reactive protein level of 12.92 mg/dl. A cerebrospinal fluid (CSF) tap detected a foul smelling pus-like CSF (Fig. 1) with an apyrexial body temperature of 36.0℃. Empirical antibiotics of 1 mg vancomycin, 1 g cefepime, and 500 mg metronidazole were given intravenously (IV). Brain CT scan indicated pneumocephalus, subdural hygroma, and meningitis (Fig. 2). A basal cistern tap was performed to treat the pneumocephalus, and conservative care was initiated. The patient progressed to stupor mental status with loss of the pupillary light reflex on hospital day 2 and was intubated with a ventilator under 5 µg/kg remifentanil and 5 mg midazolam IV sedation. An emergent right external ventricular drain (EVD) was inserted at an initial intracranial pressure (ICP) of 20 cmH2O to control progression of hydrocephalus (Fig. 3). However, EVD functioning was poor, so the neurosurgeon pulled the EVD and corrected the catheter position with a follow-up brain CT scan (Fig. 4) on hospital day 3. The CSF culture identified Streptococcus parasanguinis. The patient displayed some mental improvement, from stupor to drowsy status, on hospital day 4 but an attempt at weaning from the ventilator to a tracheal piece, and stopping the remifentanil and midazolam sedation, failed. An abdominal CT scan demonstrated a space-occupying lesion left of L3–4, which was suspected to be psoas abscess (Fig. 5). The neurosurgeon drained the retroperitoneal abscess while concurrently inserting a left EVD under general anesthesia on hospital day 5. The retroperitoneal abscess was drained again on hospital day 6. The original left EVD was removed due to lack of functioning and the right EVD was inserted to maintain ICP at 15 cmH2O. The abscess fluid culture revealed the presence of a few S. parasanguinis. The patient showed signs of improvement but responded irregularly to some simple verbal commands. She showed 4.5/4 mm pupil dilation with no light reflex on hospital day 9. No change in the EVD was detected and an attempt to change the EVD catheter failed due to brain swelling. The CT scan showed increased diffuse brain swelling, so the patient underwent a frontal and parietal bone craniectomy to decrease ICP. She became comatose, and her pupils dilated to 6.6 mm with no light reflex despite the decompressive craniectomy. The EVD catheter failed to drain the CSF and was removed on hospital day 13. Mean systolic blood pressure decreased to 50 mmHg with administration of dopamine. The patient died due to diffuse leptomeningitis on hospital day 19.
Fig. 1. Initial yellowish turbid cerebrospinal fluid.
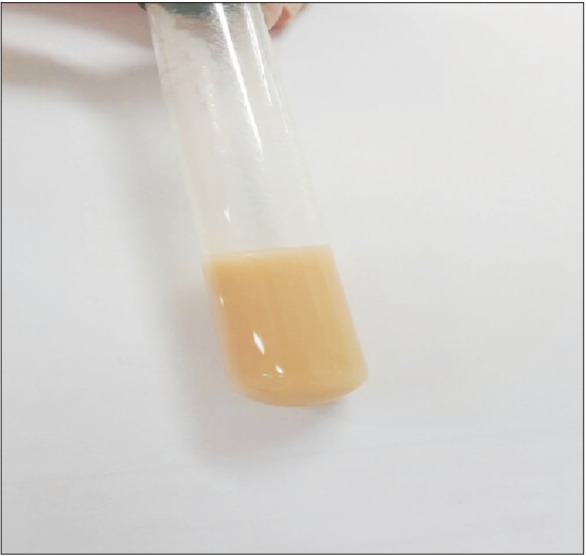
Fig. 2. Brain computed tomography (CT) scan taken 1 day before admission: pneumocephalus in the prepontine cistern. Subdural hygroma in the left cerebral subdural space.
Fig. 3. Yellowish turbid external ventricular drainage (EVD): an EVD tube was applied, which slightly decreased ventricular size.
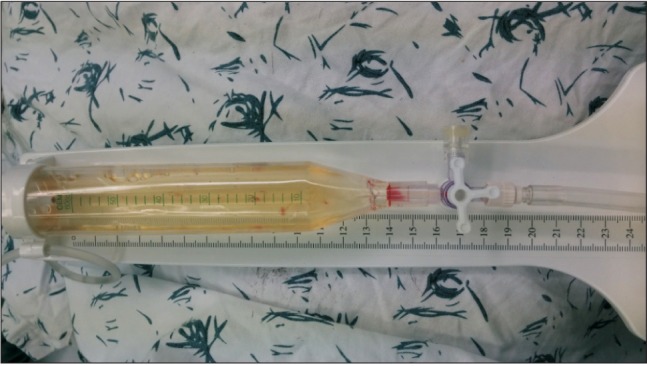
Fig. 4. Brain CT scan: subdural hygroma in the left cerebral space, and hydrocephalus highly suggestive of an infectious condition.
Fig. 5. Abdominal CT scan: extensive retroperitoneal and pararenal abscesses on the left side at the L3–4 level (> 25 cm length) (arrow).
Discussion
Although a multidisciplinary approach is needed for effective pain management, nerve block with a locally injected steroid is commonly used to manage acute and chronic pain, as the steroid acts on the pain mechanism, and many pharmacological adjuvants can be used concurrently to enhance effectiveness. Lumbar nerve root steroid blocks are used to control pain in patients suffering from back and leg pain. While fluoroscopic iodine-based contrast guidance is traditionally used for these interventions, ultrasonography has been increasingly used recently. Fluoroscopy is usually performed to identify the exact location for the injection and to avoid injection into the vasculature or a dural puncture. Improvements in technology have led to better visualization and ease of use, and have decreased the incidence of potential adverse complications, such as injecting into the vasculature, pneumothorax, or injecting intraperitoneally. Unfortunately, some patients continue to experience complications associated with a nerve block, which can be lethal. Infectious complications of a lumbar nerve root block are rarely reported and are usually minor, but can be similar to those encountered after an epidural nerve block, such as an epidural abscess or pneumocephalus with meningitis [1,2]. Various guidelines are available to avoid infections, such as aseptic skin preparation, preventive antibiotics, and careful handling of instruments. However, a CSF infection can occur as a consequence of an unintentional dural puncture during a lumbar nerve steroid injection. Here, we present three key factors that determined the outcome in this case.
Direct seeding
A lumbar CT scan showed the infected psoas muscle, left of the L3–4 level with a fluid collecting in the abdomen. We suspected that the needle had accidentally punctured the dural space after passing the left psoas muscle abscess during the nerve root block procedure. The psoas abscess, which presumably developed prior to the procedure, could have contaminated the needle and allowed bacteria to migrate through the epidural space into the intrathecal space, resulting in a rapid progression of the CSF infection after 3 days. A post procedural-related infection, such as discitis, epidural abscess, spondylitis, or meningitis is rare, but is often associated with the patient's comorbidities [3,4]. In this case, the patient had not received any physical therapy or medical treatments before and had no systemic diseases, such as diabetes. Moreover, a CSF infection with S. parasanguinis, which is a Gram-positive bacterium and a member of the Streptococcus viridans group, is uncommon [5,6]. The patient's headache may have been caused by rapid brain movement resulting from meningeal irritation, which can be confused as a symptom of pneumocephalus or post-puncture dural headache (PDPH) resulting from CSF leakage [7,8]. Because a CSF infection can be concurrent with common complications, such as pneumocephalus or PDPH after nerve block, we suggest that a prompt and accurate differential diagnosis, based on the CSF infection and the red flag signs of meningitis, should be made as fast as possible.
Immunocompromised status
As the patient presented with neutrophilia without a fever, we also hypothesized that she was injected with steroid in an immunocompromised state. An incidental intrathecal steroid injection with bacterial contamination can suppress the immune system in the CSF space such that bacteria may grow rapidly. The CSF tap revealed yellow and turbid aspirates, and her symptoms progressed rapidly to severe meningitis. The patient constantly complained of severe headache but this was misinterpreted as a common benign symptom after the nerve block. Although a headache caused by meningitis resulting from a CSF infection is rare, clinicians must be aware of this possibility when making the differential diagnosis. In other words, when a patient shows atypical clinical symptoms that obscure the clinical diagnosis after a lumbar nerve root steroid injection, a prompt work-up and procedures to address the complications should be implemented [2]. Even if the CSF was not infected, a steroid injection in the presence of an iliopsoas muscle infection could aggravate a local infection to become systemic bacteremia. Delays in starting appropriate antimicrobial agents may also lead to considerable increases in morbidity [9]. Thus, we suggest that not only a prompt empirical antibiotic prescription, but also identifying the pathogen, is necessary when considering the immunosuppressed status of patients who have received steroid nerve blocks previously.
Possible etiology and diagnosis
A CSF infection may occur most frequently in the 24–48 hours after the procedure [10]. Noh and Heo [3] reported a CSF axis infection from an epidural abscess, and meningitis with initial signs of fever, 15 days after an epidural injection. Our patient complained of constant back pain with headache and neck pain within 3 days. Both fever and constantly progressing back pain are "red flag signs" that warrant a further evaluation of back pain [11]. In our case, headache could have been interpreted as a symptom of PDPH, which may have led the local clinic to miss the diagnosis after more than a week. The initial diagnosis of a CSF infection in both cases was extremely difficult. However, a CSF infection was possible after considering red flag signs that persisted after a lumbar nerve root block procedure, which could give rise to unintended complications in the context of the underdiagnosed patient's condition. Additionally, use of steroids for a nerve block in both of the aforementioned cases may have promoted the infection. The rapid progression of an infection to symptoms of meningitis, particularly neck stiffness, and the abscess that formed from the iliopsoas to the retroperitoneum, suggested the presence of a pre-existing iliopsoas abscess in the needle route. A direct needle infection normally would not cause such a quick and extensive CSF infection and iliopsoas abscess. The fact that the infectious conditions of the iliopsoas muscle abscess may have caused the initial back pain in this patient could have led to the under-diagnosis, and may be more common than expected [12]. This notion further supports our hypothesis of a preformed psoas abscess facilitating needle contamination. Patients who are at risk of infectious complications need to be referred to a general hospital as soon as possible, as a CSF infection and abscess after a lumbar nerve steroid injection for pain control could rapidly lead to septic conditions. Thus, our early suspicion and prompt referral for a diagnosis may have prevented a lethal outcome.
Our case demonstrates a rapid CSF infection and meningitis following a lumbar nerve root steroid injection. Although local clinics have limited facilities, a patient's infection status must be established before risking an invasive procedure, such as an epidural or root block, because the complications can be fatal. Pain clinicians must also recognize red flag signs as an emergency, which should prompt checking for an infectious complication. Despite all aseptic efforts, clinicians must remain vigilant against CSF infection following a lumbar nerve root steroid injection. Although laboratory work-ups, CT, and MRI are helpful tools, the most successful approach to an infectious complication remains suspicion by the pain clinician.
References
- 1.Kim DH, Kim DC, Lee JR, Han YJ, Choe H. Epidural abscess after epidural block for pain management: a report of 3 cases. J Korean Pain Soc. 2003;16:286–290. [Google Scholar]
- 2.Ahn S, Ko YS, Lim KS. Ventricular pneumocephalus with meningitis after lumbar nerve root block. Case Rep Emerg Med. 2013;2013:640185. doi: 10.1155/2013/640185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noh SH, Heo DH. Whole cerebrospinal axis infection after lumbar epidural injection: a case report. Eur Spine J. 2015;24(Suppl 4):S525–S528. doi: 10.1007/s00586-014-3667-2. [DOI] [PubMed] [Google Scholar]
- 4.Donner B, Tryba M, Strumpf M, Dertwinkel R. Dangers and complications in pain therapy with epidural and intrathecal catheters. Schmerz. 1995;9:219–234. doi: 10.1007/BF02529443. [DOI] [PubMed] [Google Scholar]
- 5.Vicente JJ, Galardi-Castilla M, Escalante R, Sastre L. Structural and functional studies of a family of Dictyostelium discoideum developmentally regulated, prestalk genes coding for small proteins. BMC Microbiol. 2008;8:1. doi: 10.1186/1471-2180-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bochud PY, Eggiman P, Calandra T, Van Melle G, Saghafi L, Francioli P. Bacteremia due to viridans streptococcus in neutropenic patients with cancer: clinical spectrum and risk factors. Clin Infect Dis. 1994;18:25–31. doi: 10.1093/clinids/18.1.25. [DOI] [PubMed] [Google Scholar]
- 7.Kim YD, Lee JH, Cheong YK. Pneumocephalus in a patient with no cerebrospinal fluid leakage after lumbar epidural block. Korean J Pain. 2012;25:262–266. doi: 10.3344/kjp.2012.25.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee BH. Pneumocephalus after inadvertent dural puncture during epidural block: a case report. Korean J Anesthesiol. 1997;33:997–1000. [Google Scholar]
- 9.Arun R, Al-Nammari SS, Mehdian SM. Multilevel vertebral osteomyelitis and facet joint infection following epidural catheterisation. Acta Orthop Belg. 2007;73:665–669. [PubMed] [Google Scholar]
- 10.Graves M. Cerebrospinal fluid infections. The Cerebrospinal Fluid. Boston: Springer; 1989. pp. 143–165. [Google Scholar]
- 11.Kim DH. Minimally invasive percutaneous spinal techniques. Toronto: Elsevier Health Sciences; 2010. pp. 1–28. [Google Scholar]
- 12.Garner JP, Meiring PD, Ravi K, Gupta R. Psoas abscess - not as rare as we think? Colorectal Dis. 2007;9:269–274. doi: 10.1111/j.1463-1318.2006.01135.x. [DOI] [PubMed] [Google Scholar]