Abstract
AIM
To determine the feasibility of introducing video recording (VR) of neonatal resuscitation (NR) in a perinatal centre.
METHODS
This was a prospective cohort quality improvement study on preterm infants and their caregivers. Based on evidence and experience of other centers using VR intervention, a contextually relevant implementation and evaluation strategy was designed in the planning phase. The components of intervention were pre-resuscitation team huddle, VR of NR and video debriefing (VD), all occurring on the same day. Various domains of feasibility and sustainability as well as feasibility criteria were predefined. Data for analysis was collected using quantitative and qualitative methods.
RESULTS
Seventy-one caregivers participated in VD of 14 NRs facilitated by six trained instructors. Ninety-one percent of caregivers perceived enhanced learning and patient safety and, 48 issues were identified related to policy, caregiver roles, and latent safety threats. Ninety percent of caregivers expressed their willingness to participate in VD activity and supported the idea of integrating it into a resuscitation team routine. Eighty-three percent and 50% of instructors expressed satisfaction with video review software and quality of audio VR. No issues about maintenance of infant or caregivers’ confidentiality and erasure of videos were reported. Criteria for feasibility were met (refusal rate of < 10%, VR performed on > 50% of occasions, and < 20% caregivers’ perceiving a negative impact on team performance). Necessary adaptations to enhance sustainability were identified.
CONCLUSION
VR of NR as a standard of care quality assurance activity to enhance caregivers’ learning and create opportunities that improve patient safety is feasible. Despite its complexity with inherent challenges in implementation, the intervention was acceptable, implementable, and potentially sustainable with adaptations.
Keywords: Video recording, Neonatal resuscitation, Delivery room, Feasibility, Perinatal centre
Core tip: Despite proven benefits video recording (VR) of neonatal resuscitation (NR) is not adopted by all perinatal centres. Major reasons include challenges in operationalization and sustainability. Understanding the enablers and mitigation strategies is crucial on making a decision on widespread adoption of VR of NR by hospitals. We conducted a feasibility analysis of introducing VR of NR in the delivery room. It was introduced as a standard of care quality assurance activity to enhance caregiver learning and address system issues that compromise patient safety. Our study results indicate that VR of NR was effective, acceptable, implementable, and potentially sustainable with adaptations.
INTRODUCTION
About 10% of newborns require assistance to begin breathing, and about 1% is critically ill and may need life-saving therapies such as ventilation, chest compression, and medications to support heart rate[1]. In perinatal centres, the goals of neonatal resuscitation (NR) program are to have a system in place to deliver effective, efficient and safe care during the neonatal transition or resuscitation at birth, and later while responding to cardiorespiratory events[2]. Relevant elements of care include policies that govern the provision of resuscitation services, availability of equipment and staff who are trained and competent to deliver consistent and reliable high-quality care[2]. Gaps in the delivery of high-quality care may arise out of team performance, adherence to best practices and presence of latent safety threats[3-5]. Poor or inconsistent team performance, in-turn could be secondary to the inevitability of having multiple teams with variable composition and lack of structured team training and reflective deliberate practice[6]. In this context, video debriefing (VD) of actual NR is believed to facilitate the acquisition, retention, and application of skills resulting in optimal team performance and outcomes[7]. Advantages of video recording (VR) include noninterference with resuscitation and collection of unalterable objective data[8]. Moreover, VR and VD of NR has been shown to facilitate individual learning, identify and address system issues leading to better team performance and patient safety[8-11]. Despite benefits and apparent feasibility, VR of actual NR is not adopted widely in all perinatal centres because it is a complex intervention[12] and its operationalization is challenging[9,13]. To date, there have been no reports of implementing VR of NR as a quality assurance standard of practice activity from a Canadian perinatal centre. We believed that testing the feasibility of this intervention on a small scale in the real world setting with contextual constraints would inform decisions on widespread adoption.
Objective
Conduct a feasibility analysis of introducing VR of NR in the delivery room, as a standard of care quality assurance activity to enhance caregiver learning and create opportunities that improve patient safety.
MATERIALS AND METHODS
This was a prospective cohort quality improvement (QI) study. All inborn preterm infants delivered at less than 33 wk of gestation from November 2013 to January 2014, as well as resuscitation team members, were included.
Setting
Approximately 225 infants of less than 33 wk gestation are born every year at McMaster University Medical Centre hospital. The L and D suite has eight delivery rooms (DR), two operating rooms (OR-A and OR-B) and three obstetric ICU beds. A 47-bedded level 3 regional NICU is located adjacent to L and D suite. All infants are delivered and resuscitated in the same room. Following resuscitation, all babies were transferred to a dedicated stabilization room adjacent to the delivery suite, before finally being transferred to NICU. A fellow, nurse, respiratory therapist and a nurse practitioner attended all births. A neonatologist participated in the resuscitation and stabilization of infants born at less than 26 wk. of gestation or when indicated for higher gestational age.
Planning of the intervention
In 2010, a large QI project aimed at improving practices during resuscitation in preterm infants was introduced in our center. Video recording of actual neonatal resuscitation as a quality assurance activity (NRQAA) was a project nested within the larger project. The QI team composed of two physicians, nurse practitioner and a nurse was formed to oversee the implementation of this project. We implemented NRQAA program in four phases.
Phase I (January 2010-July 2012): The QI sub-team initially did a literature review to understand the requirements (equipment, personnel, standard procedures), critical success factors and challenges in the implementation of VR of NR[4,7-11,13-15]. We obtained input from leads of two other centers with experience in the VR of NR. Following that, we developed the first draft of the NRQAA program and presented to nurses, physicians, respiratory therapists, nurse practitioners and managers on separate occasions. Concerns about workload, workflow and seeking approvals from multiple stakeholders were gathered. Concurrently, we reviewed policies, procedures, and guidelines, at the department, hospital, provincial (state) and national level before seeking approvals from all stakeholders. We contacted representatives of above organizations/authorities as necessary to facilitate approvals. A standardized operating manual providing complete details of the intended program, necessary approvals, and implementation process was prepared. Finally, we obtained approval of hospital’s quality of care and patient safety committee, represented by all stakeholders. Following approval, installation of camera, web server and necessary hardware and software happened in consultation with engineering, information and communication technology, infection control and obstetric teams. Finally testing and fine-tuning of audio VR, review of software, storage and erasure of videos were completed (Table 1).
Table 1.
Overview of video recording of actual neonatal resuscitation as a quality assurance activity program and contextual details
| Overarching goal | Enhance the likelihood of caregivers’ delivering effective, safe and high quality NR care |
| Specific goal | Feasibility of introducing NRQAA program as a standard of care activity in a tertiary perinatal centre |
| Method of implementation Assessment of readiness | Quality assurance activity. Not introduced as a research study or a teaching activity Although NRP certification of all caregivers, in-situ unadvertised mock code (2008), high fidelity simulation using SimnewB (2010) were occurring in the unit, training in team behaviors, crisis resource management and error prevention had not happened |
| Training in team behaviors and exposure to VR | Interprofessional workshop in team behaviors, crisis resource management and error prevention (October 2011-January 2012), orientation of all new resuscitation team members and learners to team behaviors (January 2011 onwards), use of VD during mock resuscitations and training sessions (July 2011 onwards) were introduced. Pre resuscitation briefing of all anticipated high risk deliveries were introduced as a routine (September 2011). Team composition, configuration during resuscitation, member roles, anticipation of worst-case scenario and care planning were to be discussed by the neonatal fellow in briefing meetings. An expectation to complete the resuscitation and stabilization within 60 min of life was communicated to all members. T piece resuscitator for CPAP and PPV, Oxygen administration based on pulse oximetry reading and targeting saturation value appropriate for minute of life, and prophylactic CPAP for all < 33 wk s gestation infants were introduced as a part of larger QI initiative (January-July 2011) |
| Training instructors in debriefing | Only two out of 6 instructors had formal training in simulation and debriefing. These two instructors in-turn trained other instructors |
| Technology | Fixed IP video cameras with audio and video capturing capability and mounted on the roof/walls of the delivery rooms were used. They were wired to a web server placed in a room adjacent to NICU. VR was supposed to be turned on by the resuscitation team members (primarily by RTs) and stopped at the end of resuscitation. This video was automatically stored on the webserver and could be accessed or retrieved by instructors till its erasure |
| Securing resources | Funding for installation of video camera, web server and storage were obtained from the hospital KT grant. All personnel in QI subcommittee contributed their non clinical time for the program |
| Consent from family and staff | Obtained waiver of consent as the project was introduced as a Quality assurance standard of care practice and not as a research study. Consent was required for use of video for non quality assurance activity such as teaching providers and learners beyond the NICU team members and for research |
| Information about NRQAA was to be provided for all care providers and parents | |
| Medical record vs quality assurance record Data ownership, management and disclosure of error | Video was considered, as quality of care documents as videos would offer any health benefit to patient would not be used for care and treatment of individual patient and those other records of resuscitation apart from video would be preserved in medical records |
| NRQAA committee was to oversee the NRQAA documents. No personal identifiers were collected. Any error was to be disclosed to the family as per the hospital policies | |
| Video storage and security | Videos were directly stored on hospital web servers. They were accessible from a single computer located in a room adjacent to NICU. All VD was supposed to happen in the same room. The room was locked at all times and had swipe access. Access to VR was limited to instructors. All instructors had to sign a confidentiality and security statement after receiving training in accessing and reviewing videos. Any use of videos by instructors apart from quality assurance activity as well as sharing of access information and delegation was prohibited |
| Following video review the videos were erased from the server manually | |
| Medico legal concerns | NRQAA was not organized through QCIPA, as viewing of video by all team members or occasionally by parent would not have been possible. Thus an opportunity for collaborative learning and reflecting on one’s own performance would have been lost |
| Care providers were to understand that a video was subpoenable and parents had to consult hospital legal counsel and NRQAA committee before the release of the video | |
| Risk of spoliation or intentional destruction of evidence allegation. Video erasure policy | Video destruction policy was defined with a caveat that any patients for whom there has been a report to hospital heath care liability insurance provider, a request for records, or involvement of a coroner, a professional college or any notice of any legal proceeding whatsoever involving the patient, that those videos be maintained as until any proceeding is finalized. We opted to delete the videos when videos are reviewed and debriefed or within 14 d of recording, whichever come first. We also informed care givers and parents that the videos will not be made available for any other reasons apart from those described above |
| Privacy of patient and staff | The video cameras were focused on the on the infant and not on caregivers. Caregivers’ hands were captured inadvertently during the process. All audio including caregivers’ conversation was captured during the VR. As per the Personal Heath Information protection Act, 2004 (PHIPA) NRQAA was to institute measures to ensure personal information is not inadvertently disclosed or accessed by inappropriate person through out the program course. |
| All learners while attending the VD activity were to sign a confidentiality agreement form. All NICU care providers were to abide with existing hospital confidential policy, which clearly prohibited the use of personal names or discussion performance issues outside the quality forums | |
| Privacy office recommendations | Management of access and transfer if any to be done by a person approved by NRQAA. The program lead is responsible for oversight of the process |
| Retention time to not exceed 14 d | |
| Transfer and destruction log along with the signature of individual conducting transaction should be noted | |
| Use encrypted USB key approved by hospital ICT team for any data transfer between NICU and hospital server | |
| Ensure erasure process meets security requirements | |
| Refusal from staff/family | Risk of refusal was proactively addressed by communicating the rationale for VR and attempting to minimize misconceptions among caregivers. An adequate lead-time and multiple forums to discuss concerns arising out of VR were provided. Similarly supervisors were encouraged to address concerns related to their respective professions and to support their colleagues during NRQAA |
| VR was supposed to be initiated by resuscitation team by turning on the switch as opposed to motion sensing/auto recording | |
| All video reviews and VDs were supposed to be done by physicians during the feasibility period | |
| Institutional support | All stakeholders were informed and their support was obtained before launching the project, e.g., Quality of care and patient safety team, Information technology, Privacy, Obstetrics, Engineering, Infection control, Executives, legal council, risk management, REB and senior executives of the hospital |
| Support from professional bodies | Support was obtained from Canadian Medical Protection Agency, Nursing association, heads of professional practice of nurses and respiratory therapy, nursing unions |
| Project management | Project timelines, committee members roles, training and evaluation were all defined by the program lead |
| Resource limitations | In order to minimize cost of installation, instructors time and workload the following limitations were accepted apriori before the launch of the program |
| Video cameras were installed in three out of possible 13 delivery rooms. These three rooms had contributed to 60%-70% of all high-risk deliveries in 2007-2009. Obstetric staffs were informed to preferentially triage all less than 33 wk gestation laboring mothers to above three rooms | |
| Video review was limited to first 10 min of life and scheduled VD to day deliveries on weekdays. | |
| Superimposition of heart rate, SpO2, pressure and flow from pulse oximter and ventilator onto VR s were not done | |
| Instructors did not have access to review the videos remotely | |
| Resources for all instructors to take certification courses in debriefing was limited |
NRQAA: Neonatal resuscitation as a quality assurance activity; VR: Video recording; NR: Neonatal resuscitation; VD: Video debriefing.
Phase II (August 2013-October 2013): Six out of 11 neonatal attending volunteered to participate in NRQAA as instructors and joined the QI sub-team (NRQAA committee). All of them were NRP trainers and two of them had training and certification in debriefing. They were requested to sign up for a one-week block of facilitation and evaluation of NRQAA activity. The NRQAA committee met on two occasions to finalize the NQAA interventions, facilitator roles, and instruments. All instructors received 2 h of training on: (1) facilitating pre-resuscitation briefing, reviewing VR and debriefing videos; (2) accessing and using video review software on the web server; (3) maintaining privacy and confidentiality; and (4) use of instruments by using a simulated VR of NR. All instructors received a manual comprising of terms of reference, instruments and tools to facilitate the interventions and perform evaluations.
Phase III (November 2013-January 2014): Physicians assisted and completed all VR and VD assessments and facilitations.
Phase IV (February 2014-July 214): We conducted a survey of all resuscitation team members and instructors. The instructors also participated in a focus group to discuss the preliminary results and to identify factors critical for sustainability of the program.
Planning the study of intervention
We used the accepted frameworks to assess the effectiveness of NRQAA program and standard criteria for reporting feasibility[16-18].
Interventions
We introduced three interventions as part of NRQAA program: (1) facilitated pre-resuscitation briefing; (2) VR and review; and (3) facilitated VD (Figure 1).
Figure 1.
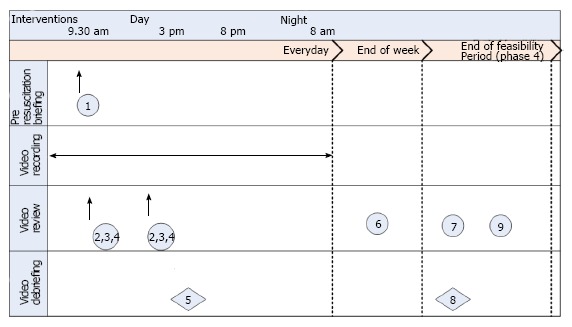
Interventions and tools for assessment. 1: Assessment of nontechnical skills (23); 2: Assessment of team behaviors (3); 3: Assessment of crisis resource management (19); 4: Debriefing template (20); 5: Caregiver feedback form; 6: Instructor weekly report; 7: Instructor survey (22); 8: Caregiver survey; 9: Focus group (21). Circle: Completed/attended by instructors; Diamond: Completed by caregivers.
Facilitated pre-resuscitation briefing: Optimal team performance during NR depends on gathering pertinent perinatal history, understanding team member roles and case specific preparation[10]. The list of potential high-risk deliveries and the scheduled resuscitation team members for a particular day were almost always known at the beginning of the day. Thus a structured daily pre-resuscitation briefing at 930 was introduced in our center in September 2011. It was mandatory for all resuscitation team members and was led by a neonatal fellow. The neonatal fellow gathered all relevant history and identified case specific preparation before the briefing. During the huddle, member roles were assigned, case specific care plans were discussed, and contingency planning for worst-case scenario was done.
During phase III, a neonatologist instructor observed the briefing process, facilitated case specific preparation and care planning, provided feedback to fellow and documented any system issues identified. The instructor also prompted members to turn on VR during resuscitation of an infant less than 33 wk of gestation.
VR and review: All resuscitation team members were requested to activate the VR when they attended a resuscitation of less than 33-wk gestation infant in OR-B, ISR-1 and room 8. The VR button was supposed to be turned on, just before receiving the baby on the resuscitaire and turned off after 10 min of resuscitation. All members received orientation on NRQAA activity in their respective monthly meetings in October 2013. All members were reminded to press the VR button during the pre-resuscitation briefing at the beginning of the day.
We reviewed every VR. The focus of evaluation was team behaviors[3], leader’s crisis resource management skills[19] and documentation of debriefing points[20] and system issues[5]. The instructor contacted the parents of infants whose resuscitation was recorded and provided an information sheet on NRQAA. Resuscitation team members were contacted when necessary to provide feedback on their performance. The most responsible physician in NICU was informed of any system issues identified during the review of videos.
Facilitated VD: Facilitated VD happened every afternoon at 3 pm in a room adjacent to NICU. All videos were accessed and projected during the discussion. The instructors were supposed to review the videos and identify the debrief points before the debriefing. The goal of VD was to create a collaborative learning environment that allows the caregivers to reflect their performance, share their thoughts and emotions without fear, learn how to recognize and improve their deficiencies. VD session was limited to resuscitation team members who participated in the NR, wherever was done. Other caregivers were allowed to attend the meeting if there was no objection from the participants. The VD session was structured. At the outset, the trainers clarified the purpose of the debriefing, participants and facilitator’s role, confidentiality measures and the need for filling the evaluation form. Then the video was presented without interruption for 5-10 min. We used the “observation, advocacy and inquiry” format to initiate debriefing[20]. Debriefing points were usually kept to a maximum of three to ensure in-depth discussions. Selected parts of a video could be replayed as necessary. Finally, the debriefing session was summarized to distil the lessons learned for future use. All VR done after 4 pm and during night shift or weekends were reviewed but without a VD. On days when there was no VR, a VD session was adjourned. The instructor facilitated VD and documented any system issues identified during resuscitation.
Outcomes
The focus of feasibility analysis was to measure acceptability, demand, the usability of technology and instruments, adaptations, resource needs, unintended effects and limited efficacy[17,18] (Table 2). Limited efficacy was assessed using: (1) caregivers’ perception of VD on one’s learning and a likelihood of enhancing patient safety; and (2) ability of the program to create learning opportunities, identify latent safety threats and elicit solutions from caregivers during VD. Resource needs in initiation and maintenance of VD program were noted during the piloting. We surveyed instructors to determine the resource requirements for facilitating VD activity and its governance. Feasibility was defined apriori as less than 20% caregivers refusing to participate, the conduct VR and debriefing on more than 50% occasions, when resuscitated in delivery rooms with recording facilities, and perceived negative impact on team performance in fewer than 20% of caregivers. A decision on widespread adoption with confidence was based on likelihood of sustainability[21].
Table 2.
Detailed matrix of outcomes and data collection
| Video review | Video debrief feedback evaluation | End of pilot period caregiver survey | End of pilot period instructor survey | End of pilot period focus group | |
| Limited efficacy testing Caregivers’ perception on learning and enhancing patient safety Impact on desired organizational outcome Create learning environment Enhance patient safety | X | X | X | X | |
| Acceptability and demand1 Management2 Caregivers Parents Instructors | X | X | X | X | |
| Usability analysis to assess team behaviors, debrief and identify system issues VR and video review software technology2 Instruments | X | X | X | X | |
| Resource needs3 Initial Maintenance | X | ||||
| Unintended adverse or beneficial effects3 Sustainability Feasibility criteria Adaptations before widespread adoption | X | X | X | X | X |
| X | X |
Assessed by participation rates;
Assessed in phases II and III;
Assessed by observations from instructors logbook, team meeting minutes and comments in surveys. VR: Video recording.
Methods of evaluation
We used the mixed method to assess the effectiveness of implementation and outcomes. Necessary data was collected using participation rates, surveys, feedback forms, focus group, participant observation and by analyzing the comments on feedback forms and surveys.
Instruments to facilitate interventions
Four validated instruments were used to measure team behaviors and system issues[3,5,19,20,22,23]. These tools were chosen to standardize the facilitation process and evaluation of performance by multiple instructors. We used caregiver feedback forms to assess the effectiveness of VD and a survey of caregivers and instructors at the end of feasibility period to determine the overall effectiveness of implementation of the intervention and the impact of interventions. Ease and satisfaction of using the instruments were measured by incorporating the USE Questionnaire tool in the instructor survey. We used the weekly reports completed by the instructors to document the frequency of all NRQAA interventions, identify the system issues and individuals who need moderate to significant improvement in crisis management skills. A combination of the focus group, comments in the survey form and logbook notes of program lead were used to identify the challenges, necessary adaptations to enhance sustainability. Finally, NHS sustainability model and guide was used to determine the likelihood of sustainability[21].
Surveys were designed indigenously to gather caregivers’ experience, perceived impact, intentions to continue and their preferences for modifying the program. Instructors’ survey had categories on assessing the instruments and workload in addition to above categories. Readability and its appropriateness in measuring the desired outcomes were evaluated by piloting the survey on five caregivers and two instructors. Based on their suggestions, a final draft of the survey was created. Caregivers’ and instructors’ survey had 15 and 32 questions respectively, required grading the response on a Likert scale, and took 10 and 20 min to complete respectively. At the end of each category, a section for “comments and suggestion” was provided. No personal identifiers were collected.
A focus group discussion was planned to gather input from instructors, managers, and leaders to assess feasibility, the likelihood of sustainability and to identify necessary adaptations in intervention[21]. The focus group was of one-hour duration and was moderated by the program lead. The moderator took the field notes and summarized the impressions of the team at the end of the session to confirm participants’ agreement with the records.
Sample size: A 3-mo time frame was based on convenience and availability of instructors to participate in this study.
Statistical analysis
Data collected from multiple sources were tabulated and presented as a percentage. Responses to surveys on a five-point Likert scale were condensed into three categories for simplicity and expressed as percentages. The program lead performed a content analysis of field notes, survey responses and minutes of the focus group. The themes and patterns emerging from the triangulation of results were recorded by the program lead and independently confirmed by another instructor.
This project was approved by the hospital’s quality of care and patient safety committee as a standard of care quality assurance activity. Since we intended to publish the study and create information sheets for parents and caregivers, a research ethics board approval was also obtained. For any use of VR outside the NRQAA activity, consent forms were created and REB approval was obtained.
RESULTS
Out of 50 high-risk NRs, 30 were performed in delivery rooms with VR facilities. VR and VD occurred in 18 (60%) and 14 (47%) instances. Seventy-one caregivers (31% physicians, 23% nurses, 24% respiratory therapists, 11% nurse practitioners and 11% others) and six instructors participated in VD. The median (range) gestational age and birth weight of neonates were 31 (24-32) wk and 1195 (570-2070) grams respectively. Procedural interventions captured during VR included CPAP (17), Mask PPV (10), intubation and positive pressure ventilation (4) chest compression (2), umbilical venous catheterization (2), epinephrine (2) and normal saline bolus (2). Team behavior event rates observed per resuscitation, median (range) included information sharing 3 (2-8), inquiry 2 (0-4), assertion 3 (0-6), teaching 2 (0-4), evaluation of plans 2 (0-4) and an overall rate of 12 (3-21). The median (range) events of crisis resource management skills observed on leader included Leadership 5 (1-7), problem-solving 5 (1-6), situational awareness 5 (1-7), resource utilization 5 (1-7), communication 4 (1-6) and an overall rate of 4 (1-6). Thirty-nine out 60 caregivers’ (65%) responded to the end of study survey. Four instructors, nursing director, medical director, and nurse manager took part in the focus group.
Limited efficacy
Ninty-one percent of caregivers reported increased ability to reflect individual’s performance and learning team behaviors. Similarly, 91% of caregivers perceived VD activity to enhance patient safety. Despite VR happening on 18 occasions, 48 issues related to resuscitation policy and procedures, team member roles and latent safety threats were identified during the study (Table 3, Table 4, Table 5, Table 6). Solutions to above issues were elicited or provided by caregivers or instructors in 21 (43%) issues. Instructors identified ten caregivers as requiring moderate to significant improvement in CRM skills and suggested further training. On eight occasions, caregivers’ recognized a deficiency in communication and sought instructors’ suggestions on learning those skills. Also, structured opportunities for creating team situational awareness, role clarification and infant specific contingency planning occurred during the pre-resuscitation huddle.
Table 3.
Policy, caregiver roles and latent safety threat issues noted during: Pre-resuscitation briefing
| Issues | Solution |
| When do I call an attending for help during resuscitation? | Whenever chest compression is initiated |
| Can I transfer the first twin from resuscitaire to a basinet and then receive the next twin on the same resuscitaire? | No! Two separate resuscitaire should be kept ready |
| Why should I know the indication for a laboring mother receiving meropenam and opioids? | To decide on appropriateness of using Naloxone, neonatal isolation and performing a septic work up |
| Where is the main surgical OR where a C-section is happening on a mother with placenta increta? | To ensure resuscitation team members reach the OR in time |
| What special preparation is necessary? | Higher room temperature, familiarization with the new environment and all necessary equipment should be ensured |
| What are the indications for admitting a newborn with fetal arrhythmia to NICU? | Arrhythmia noted on connecting to a multi-channel monitor in stabilization room |
| How do I create beds for four less than 28 wk, anticipated high-risk deliveries? | Efficient problem solving and triaging |
| What worst case scenario should I anticipate while attending a delivery in a mother with Spinal Muscular Atrophy, unexplained IUGR and non-reassuring fetal heat rate | Hypoplastic lung with difficulty in resuscitation |
| What is the role of learners (clerks, residents, others) during resuscitation? | Team leader should assign roles on a case by case basis during the team huddle |
| Who is responsible for gathering all information on an anticipated high-risk delivery and case specific preparation? | The expectation is that the neonatal fellow covering the Labor and Delivery unit is responsible for gathering information and case specific care planning. The dedicated resuscitation nurse is responsible for calling a team huddle before attending a high risk delivery |
| How should the family’s preference for resuscitating a 23 or 24-wk infant be documented in antenatal consults and handed over? | Family’s preference for resuscitation should be documented in written and handed over at every shift. If family’s preferences change, the revised plans should be documented in written |
Table 4.
Policy, caregiver roles and latent safety threat issues noted during: Issues noted during video reviewing
| Potential problems/negative impact | |
| Communication | |
| Not-verbalizing the reasons for initiating an intervention. e.g., intubation, chest compression, etc. | Lack of understanding the reasons behind an intervention, limits team members' ability to provide suggestions |
| Chest compression and PPV rhythm not verbalized “one and two and three and breathe” | Lack of synchronization delays neonate’s response to resuscitation |
| Heart rate is not verbalized after auscultating | Delay in making a decision on initiation/non initiation of chest compression |
| Excessive reliance on non-verbal communication, e.g., asking for a suction catheter by “stretching hands” after inserting the laryngoscope orally, as opposed to a “verbal request” | Delay in receiving suction catheter causes frustration in the intubator and delays the resuscitation efforts |
| Silencing alarms and not communicating the alarm to the team leader | Lack of awareness impedes accurate decision making and timely initiation of interventions |
| Team members not communicating assertively, e.g., Considering a higher peak inspiratory pressure in a non-responding infant | Delay in trouble shooting leading to ineffective resuscitation |
| Not sharing of relevant obstetric information with NR team during resuscitation of a depressed infant, e.g., MSL, abruption, Morphine | Delay in considering appropriate interventions, e.g., ET suction, fluid bolus and Naloxone respectively |
| Leadership | |
| Leader was totally passive | Leads to momentary assumption of role by another member. Often results in delayed decision making, team losing focus, excessive indulgence in unnecessary interventions, e.g., suctioning, and lack of assessment of response to interventions |
| Fixation error, e.g., Making decisions of intubation and chest compression in a nonresponsive infant without ensuring good seal during mask ventilation | Unnecessary invasive interventions with a potential for adverse events |
| Lack of evaluation of plans during resuscitation | Prevents team members ability to provide suggestions |
| Team members positioning/configuration | |
| Hands free team leader standing at the head end and RRTs who are on one side of the infant | Leader impedes effective delivery of mask ventilation |
| Initiating chest compression with the side walls up | Impedes effective performance of chest compression |
| Technical | |
| Ineffective seal around the mask during mask ventilation | Delay in responding to resuscitation |
| Attempting nasal intubation while resuscitating an unresponsive infant with severe bradycardia | Potential delay in intubation |
| Not venting stomach after a prolonged mask PPV | Secondary deterioration in SpO2 and heart rate |
| Not vigilant about FiO2 during resuscitation. Started 100% FiO2 only after 90 s of chest compression | Delay in response to resuscitation |
| Extubation while securing the ET tube as ET tube is not held firmly against the hard palate during taping | Potential for secondary deterioration or delay in resuscitation |
NR: Neonatal resuscitation.
Table 5.
Policy, caregiver roles and latent safety threat issues noted during: System issues noted during video debriefing
| Suggestions/solutions | |
| No response from NICU front desk when called for additional help by resuscitation team in infant stabilization room | Avoid unmanned NICU front desk all the time |
| Preterm infant on CPAP transferred directly to NICU as opposed to stabilization in infant stabilization room and then to NICU | Transfer through stabilization room ensures that a ventilator and incubator is always ready for stabilization |
| Person attending resuscitation is different from the one who participated in team huddle | Case specific preparation and management plans discussed during team huddle becomes redundant |
| Difficulty in paging the resuscitation team members as the composition of resuscitation team changed during a shift | Dedicated resuscitation pagers to be carried by resuscitation team members as opposed to individual personal pagers |
| Infant stabilization room stocking was exhausted when 3 deliveries happened during a shift. Health care aides were replenishing stocks once a shift | Health care aides will be called to replenish stocks when necessary |
| Delay in sending the blood samples from infant stabilization room to lab | Tube system restored |
| Needle stick injury to a resuscitation team member while setting up the resuscitaire | Educate all caregivers to remove sharps after the procedures |
| Fall and injury to foot while running to attend a pink code in labor and delivery unit | Educate caregivers on taking precautions to avoid injury |
| Undue delay in starting a PIV in infant stabilization room due to non-availability of personnel | Educate RN team members about creating a backup support to establish PIV in time |
| Who is the first responder (MD/NP) to attend labor and delivery calls during handover? (8-9 am and 5-6 pm) | The day resuscitation team (MD/NP) members |
| Pending high-risk deliveries and family’s preference for resuscitation was not passed on to day team. Thus the day team was unclear about their roles when called to attend delivery | Should be an essential part of handover |
Table 6.
Policy, caregiver roles and latent safety threat issues noted during: Skills related questions posed by care givers during video debriefing
| How do I communicate assertively? |
| How do I develop leadership skills? |
| What do I do when a RRT/TT member/Resident asks for intubation when the fellow is almost about to intubate? |
| How do I provide constructive feedback to team members during resuscitation? |
| When should I be “hands-on” and “hands-off” during resuscitation? |
| How can I ensure that I get others input during a difficult resuscitation? |
| It is very difficult to maintain a global perspective during resuscitation. How do I maintain it? |
| How do I deal with a member passing sarcastic comments/gestures during resuscitation? “Wish you all the best” |
Acceptability and demand
None of the caregivers refused to participate in a video-recording activity. Instructors did not report any untoward instances during their interaction with family, after VD event. Unit leaders and managers supported visible support in promoting caregiver participation and reviewing caregivers’ suggestions. Most caregivers (90%) and instructors (100%) expressed their willingness to participate in VD activity and supported the idea of integrating it into a resuscitation team routine. Apart from 78% of caregivers’ liking the debriefing experience, they appreciated the opportunity to discuss and provide suggestions on concerns (78%). Only 10% reported that VR made them over conscious, and it may have had a “negative impact” on their performance. Fifty-nine percent of caregivers said that VD on selected NRs, once every two weeks, as opposed to all NRs, was acceptable. Similarly, 53% felt that making the VD activity open to all NICU caregivers, as opposed to those who were involved in a particular resuscitation was acceptable.
Usability
The instructors expressed satisfaction with video-recording and video review software technology (83%). Apart from being easy to learn and use, they reported that the technology helped them to be more effective in supporting analysis and conduct of VD. However, only 50% of instructors expressed satisfaction with the quality of audio VR, as significant challenges in understanding the scenario, assessing team behaviors and quality of procedures and interpretation of response to resuscitation based on audible pulse tone and alarm sounds. All instructors expressed satisfaction with orientation, maintenance of confidentiality and templates used for a pre-resuscitation huddle, VR review, and VD.
Resource needs
Resource needs for facilitation; documentation and support of VD activity are provided in Table 7. The focus group identified that the following elements are crucial for the sustainability of the program. These include: (1) instructors’ team should be interdisciplinary with a representative from MD, RN, and RRT group; (2) Instructors should be enthusiastic, non-judgmental and possess background training in simulation, debriefing and QI; and (3) one of the instructors should take on additional role of governance.
Table 7.
Resource needs for facilitating video-debriefing activity and ongoing maintenance of the program
| Time | |
| Facilitation of team activities1 | |
| Facilitating a pre-resuscitation briefing | 15 min |
| Reviewing a resuscitation video | 30-60 min |
| Facilitating a VD | 60-90 min |
| Documentation of team activities-good practice1 | |
| Completing pre-resuscitation briefing template | 5 min |
| Completing a video review template | 5 min |
| Completing a video debrief template | 5 min |
| Completing a weekly reporting template | 5 min |
| Informing parents about VD activity | 15 min |
| Ongoing maintenance | |
| Training instructors-once | 2 h |
| Training instructors to ensure reliable review and debriefing-once | 2 h |
| Scheduling instructors and booking rooms | 1-2 h/mo |
| Trouble shooting equipment, deleting videos and ensuring confidentiality of patients and caregivers | 1-2 h/mo |
| Reporting system issues to quality councils and ensuring appropriate training for candidates lacking skills | 1-2 h/mo |
| Addressing system issues and implementing solutions | Variable |
Usual time taken for facilitating a single video-debriefing activity, unless otherwise stated. VD: Video debriefing.
Feasibility
The study results showed, no caregiver refusal to participate in VR; VR performed on 60% of occasions and less than 10% caregivers’ perceiving a negative impact on team performance. Thus criteria for the feasibility of VR and VD of NR in the delivery room intervention were met.
Sustainability
On completing the NHS sustainability and model guide during the focus group, a score of 32 was obtained for implementing the intervention in the current form. A score of less than 45 indicates the need for adaptations. Further discussions about changes in the intervention to ensure sustainability and continued accrual of benefits generated a list of adaptations (Table 8).
Table 8.
Issues affecting sustainability and suggested adaptations
| Themes | Issue affecting sustainability | Suggested adaptations |
| Resources | Same day video-debriefing is resource intensive Transfer of ownership from project lead to unit leadership helps in buy-in | Conduct video-debriefing once every 2 wk on selected resuscitation recordings. Make the debriefing sessions open to all caregivers |
| Provide resources for scheduling instructors, maintaining technology, and compensate for instructors time and effort Consider VR all deliveries and team members to seek video-debriefing on selected cases by attending on service/call | ||
| Low rate of VR | Hesitation to voluntarily record and participate in VR | Change from caregiver activated recording to motion sensor activated VR Link to certification/competence assessment (caregivers/learners) |
| System to remedy identified latent safety threats in real time | Identified but unaddressed issues result in caregiver disengagement | Set timelines for action |
| Support caregivers to take ownership on addressing issues | ||
| Communicate actions arising out of identified issues | ||
| Establish connections with Quality and Education committees for systematic training on frequently identified issues | ||
| Inability to assess impact of team actions during resuscitation | Lack of vitals (heart rate, SpO2) data on VR | Consider superimposing vitals data on video-recording |
| Inconsistency in demonstrating team behaviors by caregivers | Lack of focused training in team behaviors and error prevention | Sustain video-debriefing activity for creating learning and self evaluation |
| Team behavior evaluation not mandatory for maintenance of professional accreditation or trainee certification | Integrate demonstration of team behaviors during resuscitation into professional accreditation and certification requirements |
VR: Video recording.
Unintended adverse and beneficial effects
VR and review was helpful in assessing adoption of gentle resuscitation practices, adequacy of team preparation and documentation of facts on charts. Self-reflection of behaviors allowed caregivers to focus on improving their deficiencies and reinforcing their good practices. Thirty percent of caregivers reported that VR had a positive impact on their performance. No issues about maintenance of infant or caregivers’ confidentiality and erasure of videos were found. We did not receive any request for VR by parents and we did not take consent from parents for using VR for purposes other than NRQAA. Challenges observed during piloting are provided in Table 9.
Table 9.
Challenges identified during video recording and debriefing program
| Challenges |
| Reminding care providers about team huddle, debriefing or turn-on the VR |
| Conflict with my other work (e.g., NICU service, etc.) |
| Reviewing videos in time |
| Engaging care providers during debriefing |
| Reviewing videos recorded in night |
| Providing feedback to caregivers who could not attend debriefing |
| Completing team huddle, video review and debrief templates in time |
| Completing the weekly report template |
| Interpreting the audio to assess team communication |
| Identifying debrief issues arising from videos for debriefing |
| Time for VD (60 min) |
| Informing parents about VD in a timely manner, once the VR has happened |
| Delay in implementing project on time |
| Reinforcing expectations, providing opportunities for learning especially with rapid turnover of caregivers and trainees in a tertiary centre |
VR: Video recording; VD: Video debriefing.
DISCUSSION
Our study has shown that it is feasible to adopt VR and VD of NR in DR as a standard of care quality assurance activity to enhance caregivers’ learning and create opportunities that improve patient safety. Despite its complexity and implementation challenges, the intervention was acceptable, implementable, and potentially sustainable with adaptations in a real world setting. To date, no such feasibility study has been reported.
Strengths of this study include methodology and potential for generalizability. Feasibility objectives and criteria, setting and constraints, intervention and implementation strategy were well defined. Validated instruments for evaluation and frameworks for design and implementation were used. Detailed results including lessons learned and mitigation strategies for challenges were found. We believe that such a comprehensive and rigorous approach may allow other centers in making informed decisions on the type of technology, scale of implementation that achieves objectives with limited resources, and adopting strategies that facilitate the application of intervention. Jo Rycroft-Malone has described that “sustained implementation of evidence into practice is a planned facilitated process involving interplay between individuals, evidence, and context to promote evidence-informed practice”[24]. A careful consideration of all above elements was considered in designing and implementing the intervention in our centre. Finally, clarity on the role of organization (enabling and empowering) and project leads (facilitate caregivers’ performing discrete practical tasks during NR) in facilitating implementation played a major role in successful implementation[17].
Based on apriori agreed upon criteria for feasibility, VR of NR in DR is feasible in a tertiary perinatal centre. Caregivers’ perceived enhanced learning and organization’s ability to create opportunities for learning and identify latent safety threats, observed in this study is consistent with other reports. We speculate that VR and VD of NR in DR creates opportunities that facilitate caregiver learning, promotes the interprofessional collaborative practice and creates a mechanism to address latent safety threats affecting patient safety. Integration of this intervention as a resuscitation team routine is likely to enhance caregivers’ delivery of effective, safe and high-quality NR.
Key factors that helped in operationalization of the project in our centre included management support, implementation as a standard of care QA activity as opposed to the research study and ensuring caregivers’ readiness through multiple educational sessions, team behavior workshops and acquaintance with VR.
Our study had limitations. Assessment of impact of VR and VD of NR in DR intervention on patient outcomes, cost effectiveness, and actual team performance were beyond the scope of the study. The results may not be generalizable where centers are planning on adopting a technology or implementation strategy different from ours. Sample size was low and duration of study was short to determine any impact on clinical outcomes. A multivariate regression model to identify major barriers and enablers of adoption of VR in NR could not be performed due to small sample size[25].
A pragmatic cluster randomized trial evaluating the impact of VR of NR on patient and organizational outcomes is warranted. In future, feedback to initiate immediate corrective actions during a NR is desirable[2,26]. Similarly, a provision for printing an objective performance report directly from the monitor that shows response to various actions during NR may eliminate the need for a debriefing instructor[2,26].
It is feasible to adopt VR and VD of NR in delivery room as a standard of care quality assurance activity to enhance caregivers’ learning and create opportunities that improve patient safety. Despite its complexity with inherent challenges in implementation, the intervention was acceptable, implementable, and potentially sustainable. The comprehensive approach and detailed results from our study may allow other centers in making informed decisions on the type of technology, scale of implementation that achieves objectives with limited resources, and adopting strategies that facilitate the application of VR of NR.
ACKNOWLEDGMENTS
We thank the NICU staff for participating and taking ownership during the implementation of the initiative and changing their practices during resuscitation and stabilization. We thank all the neonatologists for supporting this project. We are grateful to Drs. Fusch C and Thomas S for their suggestions on implementing the project. Finally we thank Dr. Thabane for his valuable suggestions on study design and reporting.
COMMENTS
Background
Despite proven benefits video recording (VR) of neonatal resuscitation (NR) is not adopted by all perinatal centres. Major reasons include challenges in operationalization and sustainability. Understanding the enablers and mitigation strategies is crucial on making a decision on widespread adoption of VR of NR by hospitals. The authors conducted a feasibility analysis of introducing VR of NR in the delivery room.
Research frontiers
VR of NR and debriefing has been shown to be an effective tool in enhancing resuscitation team learning and addressing latent safety threats that compromise the quality of resuscitation. In this study, there is a suggestion that a systematic approach to operationalization of this technology helps in widespread adoption in a perinatal centre.
Innovations and breakthroughs
There is evidence of benefits of VR of NR in improving the quality and safety of resuscitation. However there is a gap in literature in understanding and addressing challenges associated with operationalization. Despite its complexity with inherent challenges in implementation, VR of NR was acceptable, implementable, and potentially sustainable with adaptations in real world setting.
Applications
The current study provides a framework for implementation and sustainability for centres considering adopting VR of NR.
Peer-review
This is a well-written article investigating an interesting issue in the neonatal care.
Footnotes
Supported by the Centre for Healthcare Optimization Research and Delivery (CHORD) at Hamilton Health Sciences with an aim of facilitating knowledge transfer initiatives from health care and supportive teams.
Institutional review board statement: The study was reviewed and approved by the institutional review boards of McMaster University and Faculty of Health Sciences Hamilton and Hamilton Health Sciences Quality and patient safety committee.
Clinical trial registration statement: This study was planned to assess feasibility (pilot or proof of concept) of wide scale adoption and study of video recording of neonatal resuscitation. We didn’t register this feasibility study in clinical trial registry.
Informed consent statement: A waiver of consent was obtained from ethics review board for this study.
Conflict-of-interest statement: The authors of this manuscript having no conflicts of interest to disclose.
Data sharing statement: All data supporting the study are provided in full in the results section of the manuscript, whereas video recording clips were deleted after review to ensure subject’s privacy and confidentiality. There is no additional data available.
Manuscript source: Invited manuscript
Specialty type: Pediatrics
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: June 28, 2016
First decision: September 5, 2016
Article in press: November 17, 2016
P- Reviewer: Sergi CM, Zhang ZH S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Kattwinkel J, Short J, Shavell L editors. Elk Grove Village: American Academy of Pediatrics; 2006. Text book of neonatal resuscitation. 5th editors. [Google Scholar]
- 2.Evaluating Resuscitation Quality. [accessed 2016 Jun 24] Available from: http://www.resuscitationcentral.com/documentation/resuscitation-quality-cpr-ecc-guidelines/
- 3.Thomas EJ, Sexton JB, Helmreich RL. Translating teamwork behaviours from aviation to healthcare: development of behavioural markers for neonatal resuscitation. Qual Saf Health Care. 2004;13 Suppl 1:i57–i64. doi: 10.1136/qshc.2004.009811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas EJ, Williams AL, Reichman EF, Lasky RE, Crandell S, Taggart WR. Team training in the neonatal resuscitation program for interns: teamwork and quality of resuscitations. Pediatrics. 2010;125:539–546. doi: 10.1542/peds.2009-1635. [DOI] [PubMed] [Google Scholar]
- 5.Wetzel EA, Lang TR, Pendergrass TL, Taylor RG, Geis GL. Identification of latent safety threats using high-fidelity simulation-based training with multidisciplinary neonatology teams. Jt Comm J Qual Patient Saf. 2013;39:268–273. doi: 10.1016/s1553-7250(13)39037-0. [DOI] [PubMed] [Google Scholar]
- 6.Cordero L, Hart BJ, Hardin R, Mahan JD, Nankervis CA. Deliberate practice improves pediatric residents’ skills and team behaviors during simulated neonatal resuscitation. Clin Pediatr (Phila) 2013;52:747–752. doi: 10.1177/0009922813488646. [DOI] [PubMed] [Google Scholar]
- 7.Weinstock P, Halamek LP. Teamwork during resuscitation. Pediatr Clin North Am. 2008;55:1011–1024. doi: 10.1016/j.pcl.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Gelbart B, Hiscock R, Barfield C. Assessment of neonatal resuscitation performance using video recording in a perinatal centre. J Paediatr Child Health. 2010;46:378–383. doi: 10.1111/j.1440-1754.2010.01747.x. [DOI] [PubMed] [Google Scholar]
- 9.Gelbart B, Barfield C, Watkins A. Ethical and legal considerations in video recording neonatal resuscitations. J Med Ethics. 2009;35:120–124. doi: 10.1136/jme.2008.024612. [DOI] [PubMed] [Google Scholar]
- 10.Finer N, Rich W. Neonatal resuscitation for the preterm infant: evidence versus practice. J Perinatol. 2010;30 Suppl:S57–66. doi: 10.1038/jp.2010.115. [DOI] [PubMed] [Google Scholar]
- 11.Carbine DN, Finer NN, Knodel E, Rich W. Video recording as a means of evaluating neonatal resuscitation performance. Pediatrics. 2000;106:654–658. doi: 10.1542/peds.106.4.654. [DOI] [PubMed] [Google Scholar]
- 12.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Donnell CP, Kamlin CO, Davis PG, Morley CJ. Ethical and legal aspects of video recording neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2008;93:F82–F84. doi: 10.1136/adc.2007.118505. [DOI] [PubMed] [Google Scholar]
- 14.Nadler I, Sanderson PM, Van Dyken CR, Davis PG, Liley HG. Presenting video recordings of newborn resuscitations in debriefings for teamwork training. BMJ Qual Saf. 2011;20:163–169. doi: 10.1136/bmjqs.2010.043547. [DOI] [PubMed] [Google Scholar]
- 15.Roberts KD, Leone TA, Edwards WH, Rich WD, Finer NN. Premedication for nonemergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics. 2006;118:1583–1591. doi: 10.1542/peds.2006-0590. [DOI] [PubMed] [Google Scholar]
- 16.Kirkpatrick DL. VA: ASTD: Alexandria; 1975. Techniques for Evaluating Training Programs. [Google Scholar]
- 17.Stetler CB, Damschroder LJ, Helfrich CD, Hagedorn HJ. A Guide for applying a revised version of the PARIHS framework for implementation. Implement Sci. 2011;6:99. doi: 10.1186/1748-5908-6-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, Thabane M, Giangregorio L, Goldsmith CH. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J, Neilipovitz D, Cardinal P, Chiu M. A comparison of global rating scale and checklist scores in the validation of an evaluation tool to assess performance in the resuscitation of critically ill patients during simulated emergencies (abbreviated as “CRM simulator study IB”) Simul Healthc. 2009;4:6–16. doi: 10.1097/SIH.0b013e3181880472. [DOI] [PubMed] [Google Scholar]
- 20.Debriefing tool. Harvard: Centre for Medical Simulation; 2012. Institute for Medical Simulation, Comprehensive instructor workshop manual handouts; pp. 131–132. [Google Scholar]
- 21.Maher L, Gustafson D, Evans A. NHS Sustainability Model and Guide: NHS Institute for Innovation and Improvement. [accessed 2016 Jun 24] Available from: http://www.stcsig.org/usability/newsletter/index.html.
- 22.Lund AM. Measuring usability with the USE questionnaire. Usability Interface. 2001;82:2016. [Google Scholar]
- 23.Fletcher G, Flin R, McGeorge P. Rating non-technical skills: developing a behavioural marker system for us in anaesthesia. Cogn Technol Work. 2004;6:165–171. [Google Scholar]
- 24.Rycroft-Malone J, Seers K, Chandler J, Hawkes CA, Crichton N, Allen C, Bullock I, Strunin L. The role of evidence, context, and facilitation in an implementation trial: implications for the development of the PARIHS framework. Implement Sci. 2013;8:28. doi: 10.1186/1748-5908-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Z. Model building strategy for logistic regression: purposeful selection. Ann Transl Med. 2016;4:111. doi: 10.21037/atm.2016.02.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edelson DP, Litzinger B, Arora V, Walsh D, Kim S, Lauderdale DS, Vanden Hoek TL, Becker LB, Abella BS. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–1069. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]