Abstract
Objectives. To describe trends in suicides with opioid poisoning noted as a contributing cause of death.
Methods. Using National Vital Statistics data (1999–2014), we calculated age-adjusted rates of suicide with opioid poisoning (International Classification of Diseases, Tenth Revision codes T40.0–T40.4) per 100 000 population per year and annual percentage change (APC) in rates. We used Joinpoint regression to examine trends in suicide rates and proportion of suicides involving opioids.
Results. The annual age-adjusted death rate from suicide with opioid poisoning as a contributing cause of death increased from 0.3 per 100 000 in 1999 to 0.7 per 100 000 in 2009 (APC = 8.1%; P < .001), and remained at 0.6 to 0.7 per 100 000 through 2014. The percentage of all suicides with opioid poisoning listed as a contributing cause of death increased from 2.2% in 1999 to 4.4% in 2010 (P < .001). Rates were similar for men and women, higher among Whites than non-Whites, higher in the West, and highest for individuals aged 45 to 64 years.
Conclusions. Opioid involvement in suicides has doubled since 1999. These analyses underscore the need for health care providers to assess suicidal risk in patients receiving opioids.
Suicide is the most serious psychiatric adverse event. Age-adjusted suicide rates in the US population increased between 1999 and 2014 from 10.5 per 100 000 to 13.0 per 100 000 per year.1 Notably, suicide rates increased by 43% during this time period among men aged 45 to 64 years. This increase in suicide deaths occurred in parallel with a large increase in drug overdose deaths, especially those involving opioids. The age-adjusted rate of opioid analgesic poisoning deaths in the United States nearly quadrupled, from 1.4 per 100 000 in 1999 to 5.4 per 100 000 in 2011.2 These deaths are correlated with the increased use of prescription opioid therapy during this time, primarily to treat chronic nonmalignant pain.3
Studies have shown that individuals with chronic pain are at higher risk for mental health disorders4 and suicide,5 and nearly all psychiatric disorders have been shown to increase suicide risk.6 Individuals with mental health and substance use disorders are also more likely to receive opioids for chronic pain,7,8 with prior studies demonstrating increased rates of chronic prescription opioid therapy among those with depression,7 posttraumatic stress disorder (PTSD),9 substance use disorders,8 and borderline personality disorder.10 Whereas trends in unintentional opioid overdose deaths have been well described,11–13 the role of opioids in suicide has received less attention.
A few studies have investigated prescription opioid use and suicide. In an analysis of National Survey on Drug Use and Health (NSDUH) data, suicidal ideation was higher among respondents with past-year prescription opioid misuse14 than among those without such misuse. Using 2006–2013 data from US Poison Centers of the Researched Abuse, Diversion and Addiction-Related Surveillance (RADARS) System, West et al. found an increasing linear trend in death rates from all intentional exposures to prescription opioids among adults aged 60 years and older.15 In an analysis of data from Department of Veterans Affairs (VA) patients receiving opioids for chronic pain in 2004 to 2005, increased opioid dose was associated with increased risk for suicide death in 2004 to 2009.16
Using National Vital Statistics death certificate data, we report national trends in completed suicides in which opioid poisoning was listed as a contributing cause of death. Specifically, we sought to answer the following questions: (1) What percentage of suicides included opioid poisoning as a contributing cause of death? (2) Did rates of suicides involving opioids increase from 1999 through 2014?
METHODS
We obtained data from the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics 1999–2014 multiple-cause-of-death mortality files, via multiple queries of the WONDER online database.17 Each record contains information on demographics, whether an autopsy report was used to complete the death certificate, place of death, 1 primary underlying cause of death, and up to 19 additional contributing causes of death (included in the multiple-cause-of-death field). We analyzed data limited to deaths among those aged 15 years and older and categorized as suicide on the basis of the following International Classification of Diseases, Tenth Revision (ICD-10)18 codes as the underlying cause of death: U03, X60 through X84, and Y87.0. We examined opioids as a contributing cause of death rather than focusing on underlying cause of death because multiple factors can contribute to suicide death, such as a multidrug overdose or hanging in the context of intoxication. To define suicide with opioid poisoning as a contributing cause of death, we further limited analyses to those cases with 1 or more of the following ICD-10 codes in the multiple-cause-of-death field: T40.0 (opium), T40.1 (heroin), T40.2 (other opioids), T40.3 (methadone), and T40.4 (other synthetic narcotics). We further limited certain analyses to specific age groups, gender, race, and census region. We also looked separately at rates of injuries with opioid poisoning of undetermined intent (ICD-10 diagnosis of Y10–Y33) listed as the underlying cause of death. We calculated age-adjusted rates by the direct method, using the 2000 census as the standard population.19 We also calculated the percentage of all suicides that included opioid poisoning as a contributing cause of death for each year. We evaluated trends in age-adjusted death rates and percentage of suicides including opioid poisoning using the Joinpoint Regression Program, version 4.3.1.0 (National Cancer Institute, Calverton, MD). Joinpoint fits the simplest Joinpoint model that the trend data allow using a Monte Carlo Permutation method.20 This allows for the calculation of an annual percentage change (APC) for each Joinpoint segment, thus denoting differing rates of change in disease trends over smaller subsets of a larger time period. The P value for a 2-sided test in which the true APC is zero is calculated on the basis of a t distribution. The Joinpoint Regression Program also calculates an average annual percentage change (AAPC) for the entire time period selected. We set the significance level at P < .05.
RESULTS
Between 1999 and 2014, there were 20 917 deaths identified as suicides with opioid poisoning listed on the death certificate as a contributing cause of death (Table 1). In most of these deaths, an autopsy report was known to have been used to complete the death certificate (65.6%), the underlying cause of death was poisoning (97.3%), and the place of death was the decedent’s home (67.1%). In a little more than half (54.7%) of the deaths, the underlying cause of death was an unspecified poisoning. Intentional self-poisoning by narcotics and hallucinogens (the category that includes opioids) was listed as the underlying cause of death in 41.3% of cases. Autopsy status was unknown for all deaths between 1999 and 2002. Between 2003 and 2014, the percentage of death certificates completed with autopsy information ranged from 67.7% (2004) to 82.2% (2006) per year, and did not change significantly by year (AAPC = 0.9%; 95% confidence interval [CI] = –0.6%, 2.5%).
TABLE 1—
Death Certificate Descriptives: Suicides With Opioid Poisoning as a Contributing Cause of Death, United States, 1999–2014
| Variable | Suicides With Opioid Poisoning as Contributor to Death, 1999–2014 (n = 20 917), No. (%) |
| Underlying cause of death | |
| Poisoning, total | 20 359 (97.3) |
| Narcotics and hallucinogens | 8 629 (41.3) |
| Other specified drugsa | 127 (0.6) |
| Other and unspecified drugs | 11 439 (54.7) |
| Chemicals and noxious substancesb | 165 (0.8) |
| Strangulation or suffocation | 257 (1.2) |
| Firearm | 116 (0.5) |
| Otherc | 159 (0.8) |
| Autopsy report present | |
| Yes | 13 719 (65.6) |
| No | 3 286 (15.7) |
| Unknownd | 3 912 (18.7) |
| Place of death | |
| Medical facility | 3 430 (16.4) |
| Decedent’s home | 14 027 (67.1) |
| Hospice,e nursing home, or long-term care facility | 90 (0.4) |
| Other or unknownf | 3 370 (16.1) |
Includes nonopioid analgesics, antipyretics, and antirheumatics (International Classification of Diseases, Tenth Revision code X60), antiepileptics, sedatives, hypnotics, and anti-Parkinson drugs (X61), and other drugs acting on the autonomic nervous system (X63).
Includes alcohol, solvents, gases, vapors, pesticides, and other unspecified chemicals.
Includes drowning or submersion, explosive material, smoke, fire and flames, self-harm with a sharp object, jumping from a high place, jumping or lying before a moving object, crashing a motor vehicle, and other means.
Autopsy report status was unknown for all deaths for the years 1999 through 2002.
Hospice was available as an option only for 2003 or later.
Unknown was available as an option only for 1999 through 2002.
Among suicides with opioids listed as a contributing cause of death, the majority (97.7%; n = 20 434) were poisoning with prescription opioids (ICD-10 codes T40.2, T40.3, T40.4). Deaths with heroin poisoning (ICD-10 code 40.1) listed as a contributing cause of death were few: 634 (0.30%) for the 16-year period, ranging from 22 in 2007 to 98 in 2014. Methadone poisoning (T40.3) was listed as a contributing cause of death in 2681 suicides (12.8%) over the 16-year time period; the number increased from 56 in 1999 to 254 in 2006 and then decreased to 142 in 2014.
Age-Adjusted Suicide Death Rates and Proportion Involving Opioids
The annual age-adjusted death rate for suicides with opioid poisoning listed as a contributing cause of death increased from 0.3 per 100 000 population in 1999 to 0.7 per 100 000 in 2009 (APC = 8.1%; P < .001), and remained at 0.6 to 0.7 per 100 000 through 2014 (Table 2). Similarly, the percentage of all suicides that had opioid poisoning listed as a contributing cause of death increased from 2.2% in 1999 to 4.4% in 2010 (for 1999–2002, APC = 13.6%; for 2002–2008, APC = 5.3%; P < .001) and remained relatively stable after that. The AAPC in suicide rates by sociodemographic category ranged from 4.3% (South) to 7.1% (Midwest) per year between 1999 and 2014. Age-adjusted death rates were similar for men and women, higher among Whites than non-Whites, and higher in the Western census region (Table 3).
TABLE 2—
Suicides With Opioid Poisoning as a Contributing Cause of Death Among Individuals Aged 15 Years and Older: United States, 1999–2014
| Suicides With Opioid Poisoning as a Contributing Cause of Death |
||||
| Year | All Suicides | No. of Deaths | % of All Suicide Deaths | Age-Adjusted Rate per 100 000 |
| 1999 | 28 939 | 640 | 2.2 | 0.3 |
| 2000 | 29 036 | 695 | 2.4 | 0.3 |
| 2001 | 30 328 | 882 | 2.9 | 0.4 |
| 2002 | 31 381 | 1 032 | 3.3 | 0.4 |
| 2003 | 31 227 | 988 | 3.2 | 0.4 |
| 2004 | 32 143 | 1 157 | 3.6 | 0.5 |
| 2005 | 32 357 | 1 218 | 3.8 | 0.5 |
| 2006 | 33 073 | 1 300 | 3.9 | 0.5 |
| 2007 | 34 408 | 1 434 | 4.2 | 0.6 |
| 2008 | 35 808 | 1 532 | 4.3 | 0.6 |
| 2009 | 36 632 | 1 634 | 4.5 | 0.7 |
| 2010 | 38 083 | 1 687 | 4.4 | 0.6 |
| 2011 | 39 221 | 1 577 | 4.0 | 0.6 |
| 2012 | 40 285 | 1 666 | 4.1 | 0.6 |
| 2013 | 40 748 | 1 650 | 4.1 | 0.6 |
| 2014 | 42 341 | 1 825 | 4.3 | 0.7 |
| Total | 556 010 | 20 917 | 3.8 | 0.5 |
Note. The annual percentage change was 8.1% (95% confidence interval [CI] = 5.4%, 10.9%) for 1999–2008 and 0.3% (95% CI = −3.4%, 4.1%) for 2009–2014.
TABLE 3—
Suicides With Opioid Poisoning as a Contributing Cause of Death, by Sociodemographic Characteristic: United States, 1999 and 2014
| Age-Adjusted Rate per 100 000 per Year |
|||
| Characteristic | 1999 | 2014 | Average Annual Percentage Change (95% CI) |
| Gender | |||
| Female | 0.3 | 0.7 | 5.3 (3.2, 7.5) |
| Male | 0.3 | 0.7 | 4.8 (2.9, 6.9) |
| Race | |||
| White | 0.3 | 0.8 | 6.9 (2.7, 11.4) |
| Non-White | 0.1 | 0.2 | 5.3 (2.0, 8.7) |
| Census region | |||
| West | 0.5 | 0.8 | 5.1 (2.5, 7.8) |
| Midwest | 0.2 | 0.6 | 7.1 (3.1, 11.3) |
| South | 0.3 | 0.6 | 4.3 (0.6, 8.1) |
| Northeast | 0.2 | 0.5 | 6.3 (0.1, 12.9) |
Note. CI = confidence interval.
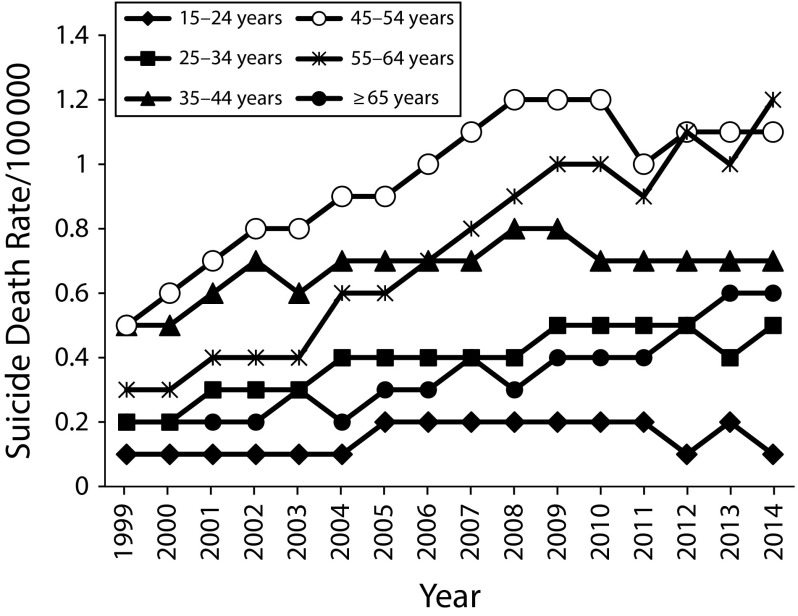
Suicide Death Rates by Age Group
Crude rates for suicide deaths with opioid poisoning listed as a contributing cause of death are depicted by 10-year age group in Figure 1. Rates were highest for individuals aged 45 to 54 years. The trend was significant for increasing suicide rates between 1999 and 2008 for all age groups (Table A, available as a supplement to the online version of this article at http://www.ajph.org). The largest absolute increase in suicide rates was observed for those aged 55 to 64 years; rates in this age group increased from 0.3 per 100 000 in 1999 to 0.9 per 100 000 in 2008, then to 1.2 per 100 000 in 2014 (for 1999–2008, APC = 13.9%; 95% CI = 10.6%, 17.3%; for 2008–2014, APC = 3.7%; 95% CI = 0%, 7.5%).
FIGURE 1—
Suicides With Opioid Poisoning as a Contributing Cause of Death, by Age Group and Year: United States, 1999–2014
Sensitivity and Other Analyses
Limiting analyses to only suicides with poisoning as the underlying cause of death, and opioid poisoning as a contributing cause of death, slightly reduced the absolute number of suicides (n = 20 410) and the age-adjusted rate (from 0.3 per 100 000 in 1999 to a peak of 0.5 per 100 000 in 2006). Limiting analyses to suicides with only prescription opioid poisoning as a contributing cause of death decreased the absolute number of deaths by 473 but did not change the age-adjusted rates. To evaluate possible sources of misclassification of suicides with opioid involvement, we examined suicides with unspecified drug poisoning listed as a cause of death, and deaths of undetermined intent in which opioid poisoning was listed as a contributing cause of death. A total of 49 456 suicides had unspecified drug poisoning listed as a contributing cause of death (ICD-10 code T50.9); in 34 203 suicides—6.15% of all suicides for the 1999–2014 time period—unspecified drug poisoning was listed as the only cause of death (ICD-10 codes X64 [underlying cause] and T50.9). Similar to suicides with opioid poisoning as a contributing cause of death, age-adjusted rates of injuries of undetermined intent with opioid poisoning listed as a contributing cause of death increased from 0.3 per 100 000 in 1999 to a peak of 0.7 per 100 000 per year in 2006 through 2009 before decreasing to 0.5 to 0.6 per 100 000 per year for 2010 through 2014.
DISCUSSION
To our knowledge, this is the first report investigating national trends in rates of suicides involving opioids. Our analysis of National Vital Statistics data demonstrates a small but significantly increasing presence of opioids as a contributing cause of death in suicides. This is especially apparent for middle-aged Americans, among whom opioid-related suicides appear to have quadrupled. Age-adjusted suicide rates increased, as did the percentage of all suicides in which opioids were a contributing cause of death, and this increase was greatest between 1999 and 2009. Previous research has documented a dose-dependent increased risk of unintentional overdose and death among patients treated with long-term opioid therapy for chronic pain.21 Our analyses suggest increased involvement of opioids in intentional overdose and suicide as well.
We were unable to determine the source of the opioids from this data; however, this increase in suicide death rates parallels increases in opioid prescribing. The number of opioid prescriptions dispensed by retail pharmacies increased from 116 million in 1999 to 219 million in 2011,22 and the percentage of adults reporting prescription opioid use in the prior 30 days increased from 5.0% in 1999 through 2002 to 6.9% in 2003 through 2006.23 In parallel with a recent report on the increase of suicide death rates overall,1 we found that rates of suicides with opioids increased most significantly among individuals aged 45 to 64. The increase in suicides with opioids as a contributing cause of death observed in our study also parallels increases in drug poisoning deaths overall and those that specifically involve opioids.2,11
Demographic differences observed in rates of suicide involving opioids are likely influenced by multiple factors, including state-to-state variability in death certificate completion,24 demographic trends in suicides overall,6 and the availability of opioids. We found that rates of suicide with opioid poisoning as a contributing cause of death increased over the time period examined regardless of age, gender, race, or geographic region, but they were higher overall among Whites than non-Whites and in the West than in other census regions. In general, suicide rates tend to be higher for non-Hispanic Whites relative to Blacks and Asians or Pacific Islanders.6 Several studies have found lower opioid prescribing rates among Blacks than Whites.25 Drug poisoning rates in general have been reported to be higher in the West and Northeast,11 and drug poisoning deaths involving opioid analgesics, specifically, have been higher among non-Hispanic Whites relative to non-Hispanic Blacks.2,13
The rates of suicide with opioid involvement reported in our study are likely to be an underestimate of self-injury with opioids. Suicides are believed to be undercounted on death certificates, in part because of constraints on medical examiners and coroners in the determination of a death as suicide.24 Impulsivity6 and impaired decision-making26 have been associated with suicidal behavior, and suicide attempters have been shown to have increased mortality from accidental and undetermined causes, in addition to subsequent completed suicide.27,28 Some researchers have proposed a new class of death—drug self-intoxication—that encompasses suicides as well as a proportion of such deaths deemed unintentional or of undetermined intent.24 Of note, we found that deaths with undetermined intent in which opioids were a contributing cause of death increased at a rate similar to that of suicides.
Opioids could potentially be a risk for suicide, as well as a means of suicide. Prior research has shown that more than 90% of those who die by suicide had a diagnosable mental disorder at the time of death.6 Individuals with a history of depression7 and PTSD9 are more likely to receive prescription opiates for chronic pain, in higher doses, and for longer periods of time. Hence, our results may reflect increasing access to opioids among a population at higher risk for suicide. Similarly, individuals with past or current substance use disorders8 and those with borderline personality disorder10 are more likely to receive prescription opioids for pain conditions. These individuals are at higher risk for suicide behaviors6,29 and, in particular, impulsive acts. Regardless of intention, opioids have high potential lethality in overdose.21 Lastly, opioids may lift mood in the short term but are likely to depress mood in the long term.30 Recent studies suggest that chronic opioid therapy might increase risk for incident, recurrent, and treatment-resistant depression.31,32
Strengths and Limitations
Strengths of the study include the presentation of national population-based data trending over an extended 16-year time frame and a focus on 2 issues of public health importance: suicide and adverse outcomes related to opioids. To our knowledge, national trends in rates of suicides involving opioids have not been reported previously.
Limitations of our study include those inherent to the use of death certificate data and their indirect determination of suicidal intent. Limitations also include individual and state-to-state variability in completion of death certificates, including variability in substances tested for and circumstances under which tests are performed. There are several potential sources of misclassification. Some accidental or unintentional deaths involving opioids might actually have been intentional. In addition, it is possible that opioids contributed to some suicides but were not tested for or noted on the death certificate. Using probit regression models to account for poisonings in which no specific drug was identified on death certificates, Ruhm estimated the proportion of intentional deaths with opioid analgesic involvement to be 52% higher in 1999 and 40% higher in 2012 than reported.33 In our analyses, approximately 6% of suicide deaths between 1999 and 2014 included only unspecified drug poisoning as a cause of death; some of these may have included opioids.
Heroin deaths have the potential to be misclassified because morphine is a metabolite of heroin.34 Heroin deaths therefore might be underestimated, although this should be constant from year to year. Reporting bias is unlikely to account for our findings. It is doubtful that knowledge about the current prescription opioid epidemic significantly increased the inclusion of opioids on suicide death certificates, because the greatest increases were observed prior to 2009, before the extent of the opioid epidemic was fully appreciated. We were unable to determine the source of opioids (prescribed or illicit) used in suicide, or how long (if at all) individuals were taking opioids regularly prior to death. We were also unable to account for relevant clinical variables (e.g., chronic pain, psychiatric disorders) that may increase risk for suicide and risk for death by overdose. However, because restriction of access to lethal means reduces suicide rates,6 the accessibility of opioids should be considered an additional risk factor for those already at high risk for suicide.
Conclusions
In conclusion, this study demonstrates increasing rates of opioid involvement in suicides. Given the high prevalence of chronic pain and mental disorders among individuals receiving prescription opioid therapy for pain, these data underscore the need for health care providers to assess for new and recurrent suicidal thinking in patients receiving opioids. Future studies should examine clinical variables associated with the use of opioids in suicide and mediators and modifiers of suicide risk among individuals receiving opioids.
ACKNOWLEDGMENTS
M. D. Sullivan was supported by the following grants: R34 DA033384-01 (National Institute on Drug Abuse [NIDA]), Pfizer Independent Grants for Learning & Change no. 19561405, and IH-1304-6379 (Patient-Centered Outcomes Research Institute). M. J. Edlund was supported by RO1 5R01DA034627-03 (NIDA).
HUMAN PARTICIPANT PROTECTION
This study used publicly available, de-identified National Vital Statistics data and was exempt from the need for protocol approval.
REFERENCES
- 1.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. 2016;(241):1–8. [PubMed] [Google Scholar]
- 2.Chen LH, Hedegaard H, Warner M. Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011. NCHS Data Brief. 2014;(166):1–8. [PubMed] [Google Scholar]
- 3.Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden JB, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440–449. doi: 10.1016/j.pain.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 5.Calati R, Laglaoui Bakhiyi C, Artero S, Ilgen M, Courtet P. The impact of physical pain on suicidal thoughts and behaviors: meta-analyses. J Psychiatr Res. 2015;71:16–32. doi: 10.1016/j.jpsychires.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs DG, Baldessarini RJ, Conwell Y . Practice Guideline for the Assessment and Treatment of Suicidal Behaviors. Arlington, VA: American Psychiatric Association; 2003. [Google Scholar]
- 7.Braden JB, Sullivan MD, Ray GT et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31(6):564–570. doi: 10.1016/j.genhosppsych.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weisner CM, Campbell CI, Ray GT et al. Trends in prescribed opioid therapy for non-cancer pain for individuals with prior substance use disorders. Pain. 2009;145(3):287–293. doi: 10.1016/j.pain.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seal KH, Shi Y, Cohen G et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–947. doi: 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 10.Frankenburg FR, Fitzmaurice GM, Zanarini MC. The use of prescription opioid medication by patients with borderline personality disorder and axis II comparison subjects: a 10-year follow-up study. J Clin Psychiatry. 2014;75(4):357–361. doi: 10.4088/JCP.13m08557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;(81):1–8. [PubMed] [Google Scholar]
- 12.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 13.King NB, Fraser V, Boikos C, Richardson R, Harper S. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: a systematic review. Am J Public Health. 2014;104(8):e32–e42. doi: 10.2105/AJPH.2014.301966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford JA, Perna D. Prescription drug misuse and suicidal ideation: findings from the National Survey on Drug Use and Health. Drug Alcohol Depend. 2015;157:192–196. doi: 10.1016/j.drugalcdep.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 15.West NA, Severtson SG, Green JL, Dart RC. Trends in abuse and misuse of prescription opioids among older adults. Drug Alcohol Depend. 2015;149:117–121. doi: 10.1016/j.drugalcdep.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 16.Ilgen MA, Bohnert AS, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157(5):1079–1084. doi: 10.1097/j.pain.0000000000000484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. National Center for Health Statistics. CDC WONDER online database. Multiple cause of death, 1999–2014. Available at: http://wonder.cdc.gov/mcd-icd10.html. Accessed October 19, 2016.
- 18.The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 19.Anderson RN, Rosenberg HM. Age Standardization of Death Rates: Implementation of the Year 2000 Standard. Hyattsville, MD: Centers for Disease Control and Prevention; 1998. [PubMed] [Google Scholar]
- 20.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for Joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 21.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315(15):1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Prescription Opioid Abuse and Heroin: Hearings Before the House Committee on Energy and Commerce Subcommittee on Oversight and Investigations, 113th Cong, 2nd Sess (statement of N. Volkov, April 29, 2014)
- 23.Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: United States, 1999–2012. NCHS Data Brief. 2015;(189):1–8. [PubMed] [Google Scholar]
- 24.Rockett IR, Caine ED. Self-injury is the eighth leading cause of death in the United States: it is time to pay attention. JAMA Psychiatry. 2015;72(11):1069–1070. doi: 10.1001/jamapsychiatry.2015.1418. [DOI] [PubMed] [Google Scholar]
- 25.Burgess DJ, Nelson DB, Gravely AA et al. Racial differences in prescription of opioid analgesics for chronic noncancer pain in a national sample of veterans. J Pain. 2014;15(4):447–455. doi: 10.1016/j.jpain.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Jollant F, Bellivier F, Leboyer M et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162(2):304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 27.Ostamo A, Lonnqvist J. Excess mortality of suicide attempters. Soc Psychiatry Psychiatr Epidemiol. 2001;36(1):29–35. doi: 10.1007/s001270050287. [DOI] [PubMed] [Google Scholar]
- 28.Nordentoft M, Breum L, Munck LK, Nordestgaard AG, Hunding A, Laursen Bjaeldager PA. High mortality by natural and unnatural causes: a 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. BMJ. 1993;306(6893):1637–1641. doi: 10.1136/bmj.306.6893.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goodman M, Roiff T, Oakes AH, Paris J. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79–85. doi: 10.1007/s11920-011-0249-4. [DOI] [PubMed] [Google Scholar]
- 30.Lutz PE, Kieffer BL. Opioid receptors: distinct roles in mood disorders. Trends Neurosci. 2013;36(3):195–206. doi: 10.1016/j.tins.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scherrer JF, Svrakic DM, Freedland KE et al. Prescription opioid analgesics increase the risk of depression. J Gen Intern Med. 2014;29(3):491–499. doi: 10.1007/s11606-013-2648-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scherrer JF, Salas J, Copeland LA et al. Prescription opioid duration, dose, and increased risk of depression in 3 large patient populations. Ann Fam Med. 2016;14(1):54–62. doi: 10.1370/afm.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruhm CJ. Drug poisoning deaths in the United States, 1999–2012: a statistical adjustment analysis. Popul Health Metr. 2016;14:2. doi: 10.1186/s12963-016-0071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Milone MC. Laboratory testing for prescription opioids. J Med Toxicol. 2012;8(4):408–416. doi: 10.1007/s13181-012-0274-7. [DOI] [PMC free article] [PubMed] [Google Scholar]