Abstract
Objectives. To investigate total and cause-specific cardiometabolic mortality among Supplemental Nutrition Assistance Program (SNAP) participants, SNAP-eligible nonparticipants, and SNAP-ineligible individuals overall and by age, gender, race/ethnicity, and other characteristics.
Methods. We performed a prospective study with nationally representative survey data from the National Health Interview Survey (2000–2009), merged with subsequent Public-Use Linked Mortality Files (2000–2011). We used survey-weighted Cox proportional hazards models adjusted for age and gender to estimate hazard ratios of total and cause-specific cardiometabolic mortality for 499 741 US adults aged 25 years or older.
Results. Over a mean of 6.8 years of follow-up (maximum 11.9 years), 39 293 deaths occurred, including 7408 heart disease, 2185 stroke, and 1376 diabetes deaths. Individuals participating in SNAP exhibited higher total and cardiovascular disease mortality, largely limited to non-Hispanic Whites and non-Hispanic Blacks, than both SNAP-eligible nonparticipants and SNAP-ineligible individuals, and higher diabetes mortality across races/ethnicities (P < .01).
Conclusions. Participants in SNAP require greater focus to understand and further address their poor health outcomes.
Public Health Implications. Low-income Americans require even greater efforts to improve their health than they currently receive, and such efforts should be a priority for public health policymakers.
The Supplemental Nutrition Assistance Program (SNAP), the largest US food-assistance program,1 covered 1 in 6 Americans during 20152 and represented more than half of the entire US Department of Agriculture’s annual budget of $155 billion.3 Eligibility for SNAP is determined by household income and resources—in particular, gross monthly household income at or below 130% of the poverty level.4,5 By many measures, SNAP targets a disadvantaged population, who are more likely to live under the poverty threshold and less likely to have health insurance or higher educational attainment, compared with nonparticipants.6 Consistent with this, SNAP participants cross-sectionally have higher rates of obesity,7–9 metabolic risk factors,9 and other health conditions6 compared with eligible as well as ineligible nonparticipants.
With recognition that low-income Americans are at higher risk of poor health outcomes because of multiple environmental, behavioral, and sociocultural risks, SNAP is designed to reduce food insecurity and improve the diet of participating individuals and families by providing financial assistance (average $125 per month per person) to purchase foods for at-home consumption.2,10 However, the extent to which SNAP is fully addressing the long-term health risks of low-income Americans is not well-established. According to data from 25 years ago,11 SNAP participants had higher all-cause mortality than income-eligible nonparticipants. Whether such disparities remain has not been evaluated. In addition, to our knowledge, no studies have examined cause-specific mortality for SNAP participants versus SNAP-eligible nonparticipants, which can help inform potential determinants of disparities in these populations. Among diet-related diseases, cardiometabolic diseases such as coronary heart disease (CHD), stroke, and diabetes are particularly relevant because of their health and economic burdens and links with diet.12,13
Understanding the relationship between SNAP participation status and total and cardiometabolic mortality is crucial for informing whether additional supportive interventions are needed to better serve this population. We therefore prospectively investigated the risk of total and cardiometabolic mortality comparing SNAP participants, SNAP income-eligible nonparticipants, and SNAP-ineligible individuals by linking together large, nationally representative data sets. As a second prespecified aim, we investigated potential differences in these relationships by age, gender, and race/ethnicity to help elucidate how SNAP status and potential interventions might relate to health disparities in these groups.
METHODS
We utilized nationally representative data from the 2000–2009 National Health Interview Survey (NHIS),14 which is based on multistage probability sampling (n = 80 000–100 000 respondents per year; overall response rate = 82%–88%) of the civilian, noninstitutionalized US population. In-home, interviewer-administered questionnaires assessed age, gender, race/ethnicity, family income, education, other participant characteristics, and SNAP participation. For the current investigation, we evaluated 499 741 adults aged 25 years or older who provided information on age, gender, race/ethnicity, and SNAP participation. We then linked NHIS data to mortality data from the Public-Use Linked Mortality Files,15 which provide follow-up for the NHIS sample through December 31, 2011 (additional details to follow).
Because both SNAP eligibility and participation are associated with diverse other characteristics that may influence health, our aim was not to draw inferences on the causal effect of SNAP on mortality, but to accurately describe the actual observed mortality differences among SNAP participants, SNAP-eligible nonparticipants, and SNAP-ineligible individuals to inform the need for further investigation and interventions in these populations.
Determining Program Participation and Eligibility
We categorized respondents as SNAP participants, SNAP-eligible nonparticipants, or SNAP-ineligible individuals. We identified SNAP participants as individuals who reported someone in their family (defined by NHIS as an individual or a group of 2 or more related persons who are living together in the same household) who participated in the program at any point during the previous year. We identified SNAP-eligible nonparticipants by monthly family gross income less than or equal to 130% of the poverty guideline (i.e., income-to-poverty ratio ≤ 1.305).
Although one primary federal eligibility criterion is household gross income,4 we used family gross income for consistency with how poverty-to-income ratio is measured, which is at the family level. We confirmed that household and family income are nearly identical in 96% of adults aged 25 years or older by using the 3-year Public-Use Microdata Sample from the American Community Survey (2007–2009).16 A second related criterion, monthly household net income less than or equal to 100% of the poverty guideline,4 was not assessed in NHIS and could not be used. Because of the categories of NHIS reporting of income-to-poverty ratio in 2000 to 2008 (i.e., 0–0.74, 0.75–1.24, 1.25–1.49, etc.), we utilized a poverty-to-income ratio of less than 1.25 to categorize SNAP eligibility in these years, and less than or equal to 1.30 in 2009 when more precise income data were reported. We utilized the established NHIS-imputed income data for 18% of the sample not reporting income to correct for observed biases that result from using data without imputation.17
Outcome Ascertainment
Our primary outcomes were all-cause mortality, cardiovascular mortality (including death from heart disease [International Classification of Disease 10th Revision codes I00–I09, I11, I13, I20–I51], and stroke [I60–I69]), and diabetes mortality (E10–E14), as identified by the Public-Use Linked Mortality Files.15 We also secondarily evaluated CHD and stroke mortality separately, as well as combined cardiometabolic mortality (the sum of deaths attributable to CHD, stroke, and diabetes).
In the Public-Use Linked Mortality Files (2000–2011), NCHS staff matched NHIS respondents to the National Death Index (NDI),18 a database of all US deaths cataloged since 1979, by using standardized procedures.15 In brief, participants were screened for sufficient identifying information, such as social security number, name, date of birth, and state of residence. The NCHS used probabilistic matching methods to link these participants to records in the NDI. The NDI has been documented to capture nearly all deaths (∼97%) when social security numbers are available, as is the case for all eligible NHIS participants linked to the NDI.19,20
Statistical Analysis
We estimated the association between SNAP status and risk of mortality by using Cox proportional hazards, with time-at-risk from the date of survey response until death or censoring on December 31, 2011, the latest date of available linked mortality data. For cause-specific cardiometabolic mortality analyses, we censored participants for other causes of death. We tested the proportional hazards assumption by plotting and visually inspecting the survival functions against time and it was not rejected. All analyses accounted for the complex survey design, weighting, and multiply imputed data so that results are nationally representative over this 10-year time period.
Because our aim was to quantify the actual observed mortality differences among Americans by SNAP participation and eligibility, rather than to attempt to draw inference on the causal effects of SNAP per se, we adjusted our main findings only for age (25–34, 35–44, 45–54, 55–64, 65–74, ≥ 75 years) and gender. We also conducted stratified analyses by age (2 groups: 25–64 and ≥ 65 years), gender, and race/ethnicity (3 groups: non-Hispanic White, hereafter referred to as White; non-Hispanic Black, hereafter referred to as Black; and Hispanic); we did not evaluate “other” race/ethnicity because of small numbers and greater racial/ethnic heterogeneity within this category.
We also evaluated and included information from NHIS on other variables that might help explain any observed mortality differences, including education, region of residence, employment status, marital status, insurance coverage, family structure, and, available in randomly available subsets, self-reported smoking status, body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), alcohol use, physical activity, hypertension, and high cholesterol (Table 1). In secondary analyses, we adjusted for these additional variables to explore the extent to which such factors might partly explain the observed mortality differences by SNAP status. Information on dietary habits, of special interest in these populations, is unfortunately not available in NHIS.
TABLE 1—
Respondent Characteristics: US National Health Interview Survey 2000–2009
| Characteristic | No. | SNAP-Ineligible Individuals (n = 417 547) | SNAP Participants (n = 31 761) | SNAP-Eligible Nonparticipants (n = 50 433) |
| No. of deathsa | ||||
| All-cause | 39 293 | 29 868 | 2 884 | 6 541 |
| Coronary heart disease | 7 408 | 5 571 | 533 | 1 304 |
| Stroke | 2 185 | 1 668 | 145 | 373 |
| Diabetes | 1 376 | 989 | 143 | 244 |
| Cardiovascularb | 9 593 | 7 239 | 677 | 1 677 |
| Cardiometabolicc | 10 969 | 8 230 | 817 | 1 921 |
| Age, yd | 499 741 | 49.3 (49.2, 49.5) | 45.0 (44.8, 45.3) | 50.8 (50.5, 51.0) |
| Female | 499 741 | 51.0 (50.8, 51.1) | 61.9 (61.5, 62.4) | 55.9 (55.5, 56.3) |
| Race/ethnicity | 499 741 | |||
| Non-Hispanic White | 361 368 | 76.5 (76.1, 77.0) | 48.6 (47.3, 49.9) | 53.4 (52.3, 54.4) |
| Non-Hispanic Black | 55 258 | 9.1 (8.8, 9.4) | 26.4 (25.3, 27.6) | 16.4 (15.7, 17.2) |
| Hispanic | 58 394 | 9.4 (9.2, 9.7) | 20.7 (19.8, 21.6) | 24.4 (23.6, 25.3) |
| Non-Hispanic other | 24 721 | 4.9 (4.7, 5.0) | 4.3 (3.8, 4.8) | 5.8 (5.3, 6.2) |
| Education | 492 383 | |||
| <high school | 78 951 | 11.5 (11.3, 11.7) | 40.0 (39.2, 40.7) | 38.7 (37.9, 39.4) |
| High school or equivalent | 146 584 | 29.2 (28.9, 29.5) | 33.7 (33.1, 34.3) | 31.9 (31.3, 32.5) |
| Some college | 132 473 | 28.2 (28.0, 28.4) | 21.6 (21.0, 22.3) | 20.0 (19.1, 20.2) |
| College graduate | 134 374 | 31.1 (30.7, 31.6) | 4.7 (4.4, 5.0) | 9.7 (9.3, 10.2) |
| Region of residencee | 499 741 | |||
| Northeast | 94 490 | 19.4 (18.9, 19.9) | 17.5 (16.5, 18.5) | 16.0 (15.3, 16.7) |
| Midwest | 118 562 | 24.3 (23.6, 24.9) | 23.8 (22.6, 24.9) | 19.4 (18.6, 20.3) |
| South | 183 440 | 35.7 (35.0, 36.4) | 41.4 (40.0, 42.8) | 41.8 (40.8, 42.9) |
| West | 103 249 | 20.6 (20.1, 21.2) | 17.4 (16.3, 18.4) | 22.7 (21.8, 23.7) |
| Married | 498 330 | 68.4 (68.0, 68.7) | 35.7 (34.8, 36.5) | 46.8 (46.1, 47.5) |
| Employedf | 498 950 | 69.5 (69.2, 69.8) | 39.7 (39.0, 40.4) | 45.2 (44.5, 45.8) |
| Health insurance coverageg | 497 023 | 89.2 (89.0, 89.3) | 71.3 (70.7, 72.0) | 65.9 (65.2, 66.5) |
| Family structure | 255 754 | |||
| 1 adult, no children | 44 143 | 15.7 (15.5, 16.0) | 17.4 (16.7, 18.1) | 30.2 (29.5, 30.1) |
| Multiple adults, no children | 112 353 | 47.5 (47.3, 47.8) | 22.0 (21.2, 22.8) | 28.9 (28.3, 29.5) |
| 1 adult, at least 1 child | 8 798 | 2.2 (2.2, 2.3) | 14.2 (13.7, 14.7) | 6.2 (6.0, 6.5) |
| Multiple adults, at least 1 child | 90 486 | 34.5 (34.2, 34.9) | 46.4 (45.5, 47.3) | 34.7 (34.0, 34.9) |
| Poverty-to-income ratioh | 499 741 | |||
| 0–0.74 | 32 037 | 0.0 (0.0, 0.0) | 39.7 (38.8, 40.6) | 37.9 (37.2, 38.5) |
| 0.75–1.24 | 40 402 | 0.0 (0.0, 0.0) | 29.1 (28.2, 29.9) | 61.5 (60.9, 62.2) |
| 1.25–1.99 | 66 054 | 14.4 (14.1, 14.7) | 17.5 (16.8, 18.2) | 0.6 (0.5, 0.7) |
| 2.00–3.99 | 155 798 | 36.5 (36.2, 36.9) | 11.1 (10.5, 11.8) | 0.0 (0.0, 0.0) |
| ≥ 4.00 | 205 449 | 49.1 (48.6, 49.5) | 2.5 (2.2, 2.9) | 0.0 (0.0, 0.0) |
| Body mass index,d,i,j kg/m2 | 218 540 | 27.2 (27.1, 27.2) | 29.4 (29.3, 29.5) | 27.4 (27.3, 27.5) |
| Smokingi | 255 754 | |||
| Never | 137 033 | 54.7 (54.3, 55.0) | 42.4 (41.5, 43.7) | 53.2 (52.4, 54.0) |
| Former | 62 813 | 25.9 (25.6, 26.1) | 16.7 (16.0, 17.3) | 20.5 (19.9, 21.1) |
| Current | 55 908 | 19.5 (19.2, 19.7) | 41.0 (40.0, 42.0) | 26.3 (25.6, 27.0) |
| Alcohol intakei,k | 181 872 | |||
| Never | 38 597 | 18.9 (18.6, 19.2) | 34.4 (33.4, 35.4) | 33.3 (32.5, 34.2) |
| Light | 97 925 | 55.1 (54.7, 55.4) | 48.3 (47.3, 49.3) | 46.4 (45.5, 47.3) |
| Moderate | 33 684 | 20.0 (19.4, 20.0) | 10.4 (9.8, 11.0) | 13.4 (12.8, 14.0) |
| Heavy | 11 665 | 6.3 (6.2, 6.5) | 6.8 (6.3, 7.4) | 6.8 (6.4, 7.3) |
| Physical activityi,l | 236 945 | |||
| Does not meet either guideline | 130 271 | 51.3 (50.8, 51.7) | 72.4 (71.5, 73.4) | 70.1 (70.0, 71.2) |
| Meets guideline for strength physical activity | 8 666 | 3.8 (3.7, 3.9) | 2.9 (2.7, 3.2) | 3.2 (2.9, 3.4) |
| Meets guideline for aerobic physical activity | 60 463 | 27.1 (26.8, 27.4) | 18.2 (17.5, 19.0) | 18.8 (18.2, 19.4) |
| Meets both guidelines | 37 545 | 17.9 (17.6, 18.2) | 6.4 (5.9, 6.8) | 7.2 (6.8, 7.6) |
Note. SNAP = Supplemental Nutrition Assistance Program. Some SNAP participants may have income-to-poverty ratios > 1.3 because income tests do not apply if all family members participate in Temporary Assistance for Needy Families or receive Supplemental Security Income. In addition, SNAP participation is on a monthly basis whereas data on income were collected on an annual basis. Values are proportions (95% confidence intervals) within each column unless otherwise noted, accounting for survey design sampling weights. Percentages might not add to 100 because of rounding. The sample size was n = 499 741.
International Classification of Disease, Tenth Revision, codes,15 as identified by National Center for Health Statistics Linked Mortality Public-Use Files: coronary heart disease (I00–I009, I11, I113, I20–I51), stroke (I60–I69), diabetes (E10–E14). Cardiovascular disease mortality includes deaths from coronary heart disease and stroke, and cardiometabolic disease mortality includes deaths from cardiovascular disease and diabetes.
Coronary heart disease and stroke.
Coronary heart disease, stroke, and diabetes.
Survey-weighted mean (95% confidence interval).
Census regions (https://www.census.gov/geo/reference/gtc/gtc_census_divreg.html).
Employed during week before interview. Includes working not for pay at a family business and part-time employment.
Includes coverage under private and public health insurance policy.
Computed as income divided by poverty threshold, accounting for family size and composition. Households with current gross incomes greater than 1.3 of the poverty threshold can have participated in SNAP because of meeting other criteria (e.g., household net income less than or equal to 1.0 of the poverty threshold) or because of increases in income since they participated in SNAP during the past year (https://www.census.gov/hhes/www/poverty/about/overview/measure.html).
Data available only for a random subsample of respondents in each year.
National Health Interview Survey staff computed body mass index based on self-reported height and weight.
Never = fewer than 12 drinks in lifetime; light = 3 or fewer drinks per week over the past year; moderate = 3 or more drinks per week up to 14 drinks per week over the past year (men), 3 or more drinks per week up to 7 drinks per week over the past year (women); heavy = greater than 14 drinks per week over the past year (men), greater than 7 drinks per week over the past year (women).
Leisure time physical activity guideline is from Healthy People 2020.
To consider the issue of reverse causation because of substantial prevalent disease, we conducted a sensitivity analysis in which we excluded all person-time and events in the first year of follow-up. We performed analyses with Stata version 14 (StataCorp LP, College Station, TX), with 2-tailed α < 0.01 to conservatively assess our 3 main mortality outcomes (all-cause, cardiovascular, diabetes).
RESULTS
When we compared the 499 471 US men and women in our analysis, the mean age of SNAP participants was about 4 to 6 years younger than either SNAP-ineligible individuals or SNAP-eligible nonparticipants (Table 1). Participants in SNAP were more likely to be female (61.9%) than SNAP-eligible nonparticipants (55.9%) or SNAP-ineligible individuals (51.0%). About half of both SNAP participants and SNAP-eligible nonparticipants were White; about three quarters of SNAP-ineligible individuals were White. About 1 in 4 (26.4%) and 1 in 6 (16.4%) of SNAP participants and SNAP-eligible nonparticipants were Black, respectively. SNAP-ineligible individuals were far more likely to have greater education, whereas SNAP participants and SNAP-eligible nonparticipants had much more similar distributions of educational attainment. Compared with SNAP-ineligible individuals, individuals eligible or participating in SNAP were slightly more likely to live in the southern United States, compared with other regions.
As would be expected, SNAP-ineligible individuals were more likely to be employed and had higher household incomes. SNAP-ineligible individuals were also more likely to be married and to be in families with multiple adults and no children. Differences in health insurance were more modest and, interestingly, a greater proportion of SNAP participants had health insurance compared with SNAP-eligible nonparticipants. Mean BMI for all groups was overweight (25.0 to <30.0 kg/m2), yet BMI was higher among SNAP participants compared with the other groups. Participants in SNAP were more likely to be current smokers; prevalence of heavy alcohol intake was similar among groups. SNAP-ineligible individuals were more likely to meet guidelines for physical activity. The prevalence of hypertension was similar between SNAP participants and SNAP-eligible nonparticipants, but lower for SNAP-ineligible individuals. The prevalence of high cholesterol was similar across all groups.
Mortality by SNAP Status
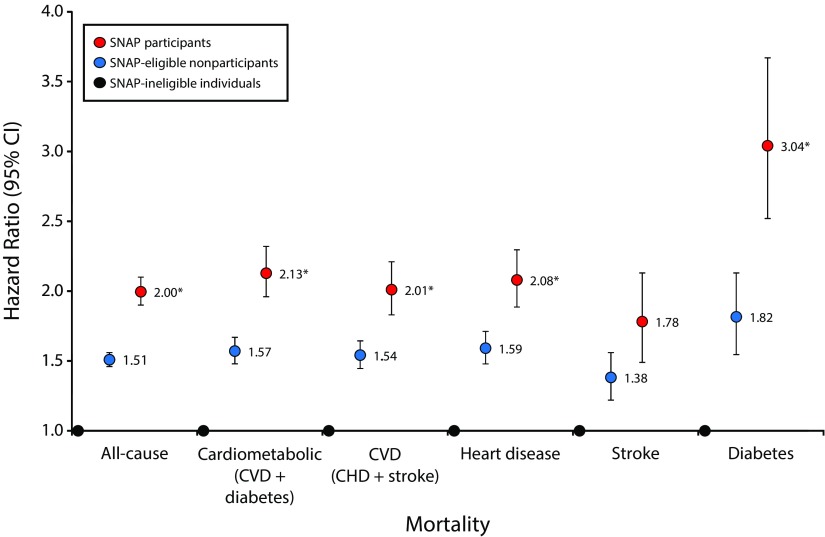
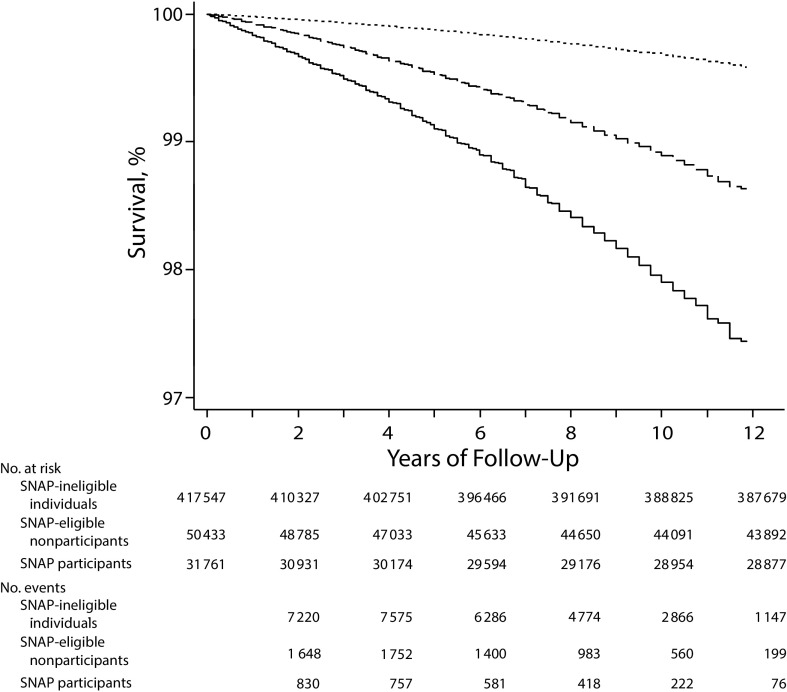
During a mean 6.8 years of follow-up (maximum 11.9 years), 39 293 deaths occurred, including 9593 from cardiovascular disease (7408 CHD; 2185 stroke) and 1376 from diabetes (Table 1). When we adjusted for age and gender, SNAP participants exhibited the highest risk of all-cause and cardiometabolic mortality, followed by SNAP-eligible nonparticipants and then SNAP-ineligible individuals (Figure 1). Total mortality was 51% higher among SNAP-eligible nonparticipants (hazard ratio [HR] = 1.51; 95% confidence interval [CI] = 1.46, 1.56), and 100% higher among SNAP participants (HR = 2.00; 95% CI = 1.90, 2.10). Mortality differences were largest for deaths attributable to diabetes, with 82% higher risk (HR = 1.82; 95% CI = 1.55, 2.13) among SNAP-eligible nonparticipants and 3-fold higher risk (HR = 3.04; 95% CI = 2.52, 3.67) among SNAP participants, compared with SNAP-ineligible individuals. Notably, mortality was significantly higher (P < .01) among SNAP participants compared with SNAP-eligible nonparticipants for all outcomes (except for stroke mortality; P = .016). Mortality differences were consistent over time, with increasing divergence of survival throughout follow-up (Figure 2). Findings were very similar in sensitivity analyses excluding all person-time and events occurring in the first year of follow-up (data not shown).
FIGURE 1—
Risk of All-Cause and Cause-Specific Cardiometabolic Mortality Comparing Supplemental Nutrition Assistance Program (SNAP) Participants, SNAP-Eligible Nonparticipants, and SNAP-Ineligible Individuals; United States, 2000–2011
Note. CHD = coronary heart disease; CI = confidence interval; CVD = cardiovascular disease; SNAP = Supplemental Nutrition Assistance Program. Circles represent hazard ratios, and error bars represent 95% CIs. Values are adjusted for age and gender and weighted to represent the US population. International Classification of Disease, Tenth Revision, codes15: coronary heart disease (I00–I009, I11, I13, I20–I51), stroke (I60–I69), diabetes (E10–E14). Cox proportional hazards model, adjusted for age (25–34, 35–44, 45–54, 55–64, 65–74, ≥ 75 years) and gender. The sample size was n = 499 471.
*Significantly different than SNAP-eligible nonparticipants for same event and gender at P < .01.
FIGURE 2—
All-Cause Survival According to Supplemental Nutrition Assistance Program Status at Baseline Among US Adults: 2000–2011
Note. SNAP = Supplemental Nutrition Assistance Program. Dotted line = SNAP-ineligible individuals; dashed line = SNAP-eligible nonparticipants; solid line = SNAP participants. Similar findings were observed for cause-specific cardiometabolic mortality (data not shown). The sample size was n = 499 471.
By age and gender.
Findings were consistent when stratified by age, although, as would be expected, proportional mortality differences by SNAP status were larger among individuals aged 25 to 64 years, whereas absolute mortality difference by SNAP status were larger among individuals aged 65 years or older (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Results were also consistent with the overall findings when stratified by gender (Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
By race/ethnicity.
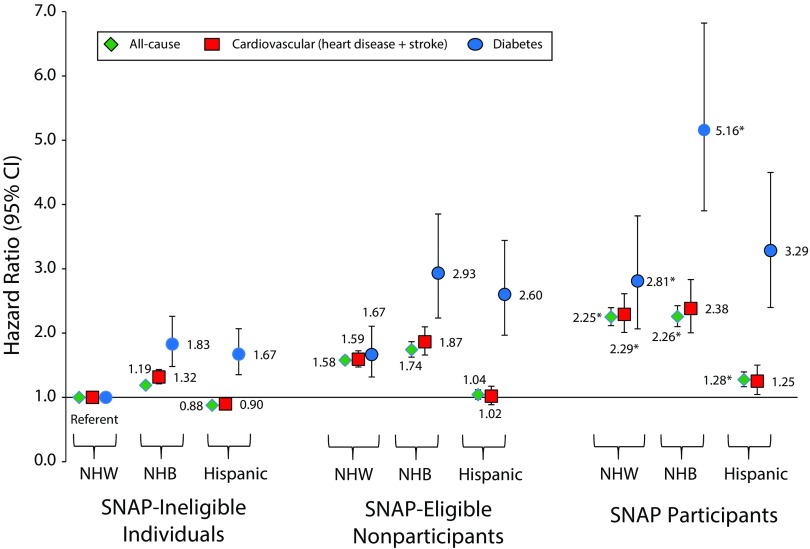
Higher all-cause and cardiovascular mortality among SNAP participants was largely restricted to Whites (HR = 2.25; 95% CI = 2.12, 2.40; and HR = 2.29; 95% CI = 2.01, 2.61) and Blacks (HR = 2.26; 95% CI = 2.10, 2.43; and HR = 2.38; 95% CI = 2.01, 2.83), with a smaller risk difference among Hispanics (HR = 1.28; 95% CI = 1.17, 1.40; and HR = 1.25; 95% CI = 1.04, 1.50; Figure 3). By contrast, higher diabetes mortality among SNAP participants was evident in Whites (HR = 2.81; 95% CI = 2.07, 3.82), Hispanics (HR = 3.29; 95% CI = 2.40, 4.50), and especially Blacks (HR = 5.16; 95% CI = 3.90, 6.82). When we compared SNAP-eligible nonparticipants to SNAP-ineligible individuals, we saw similar racial/ethnic disparities, but these differences were of smaller magnitude. Key exceptions were among Hispanics: Hispanic SNAP-eligible nonparticipants did not have higher total or cardiovascular mortality compared with SNAP-ineligible Whites; SNAP-ineligible Hispanics actually had lower total and cardiovascular mortality compared with SNAP-ineligible Whites.
FIGURE 3—
Risk of All-Cause and Cause-Specific Cardiometabolic Mortality Comparing SNAP Participants, SNAP-Eligible Nonparticipants, and SNAP-Ineligible Individuals by Race/Ethnicity: United States, 2000–2011
Note. CHD = coronary heart disease; CI = confidence interval; NHB = non-Hispanic Black; NHW = non-Hispanic White; SNAP = Supplemental Nutrition Assistance Program. Circles represent hazard ratios, and error bars represent 95% CIs. Values are adjusted for age and gender and weighted to represent the US population. International Classification of Disease, Tenth Revision, codes15: coronary heart disease (I00–I009, I11, I13, I20–I51), stroke (I60–I69), diabetes (E10–E14). Cox proportional hazards model, adjusted for age (25–34, 35–44, 45–54, 55–64, 65–74, ≥ 75 years) and gender. The sample size was n = 499 471.
*Significantly different than SNAP-eligible nonparticipants for same event and race/ethnicity at P < .01.
Adjustment for Potential Explanatory Variables
Disparities in mortality by SNAP status were smaller following additional adjustment for race/ethnicity, education, region of residence, employment status, marital status, insurance coverage, family structure, and, in a subset, BMI, smoking, alcohol intake, physical activity, hypertension, and high cholesterol (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Among these, differences in race/ethnicity, region, insurance coverage, family structure, BMI, smoking status, alcohol intake, physical activity, and hypertension each had little appreciable influence, whereas differences in education, employment status, and marital status (and, for stroke, physical activity) each partly attenuated the disparities in mortality, suggesting that these factors at least partly explain the differences in risk of death. Yet, even with these additional adjustments, significant (P < .01) differences in mortality remained among SNAP-ineligible individuals, SNAP-eligible nonparticipants, and SNAP participants. Additional adjustment for high cholesterol in a small subset removed remaining mortality differences between SNAP-eligible nonparticipants and SNAP participants, although significant (P < .01) differences in all-cause mortality between these groups and SNAP-ineligible individuals remained.
DISCUSSION
In this nationally representative investigation of nearly half a million Americans enrolled and followed from 2000 through 2011, individuals in families participating in SNAP during the previous year exhibited higher risk of subsequent all-cause, cardiovascular, and especially diabetes mortality, compared with either SNAP-eligible nonparticipants or SNAP-ineligible individuals. Risk among SNAP-eligible nonparticipants was only about half as large as that of SNAP participants, even though many sociodemographic characteristics were similar in these groups (other than age and gender, which were adjusted in all analyses). These observed mortality differences by SNAP status were similar in subgroups stratified by age and gender. When stratified by race/ethnicity, mortality differences according to SNAP status were more heterogeneous, with several interesting findings. To our knowledge, this is the first investigation to evaluate all-cause and cause-specific cardiometabolic mortality differences according to SNAP status in the contemporary era.
Participation in SNAP is linked to many sociocultural, environmental, and behavioral characteristics.6,21 For example, people who perceive themselves to be at higher health risk, which can have consequences for employment, food security, and poverty, may be more likely to elect to participate in SNAP.6,22 Compared with nonparticipants, SNAP participants are more likely to have children or other family members with developmental delays or functional limitations, and are more likely to report forgoing medical care because of financial hardship.6 Such conditions, whether acute or chronic, likely influence individuals’ choice to participate in SNAP, yet the effects of these specific influences on the choice to participate in SNAP are challenging to assess in large nationally representative data sets. Thus, it is crucial to emphasize that our findings should not be interpreted as a causal effect of participating in SNAP. For instance, it is plausible that these individuals, if they did not participate in SNAP, might have even worse health outcomes.
Among potential explanatory variables, differences in education, employment status, and marital status each appeared to partly, but not fully, account for the observed disparities in mortality. Adjustment for high cholesterol in a small subset removed remaining mortality differences between SNAP-eligible nonparticipants and SNAP participants, yet differences in all-cause mortality remained between these groups and SNAP-ineligible individuals. Although our investigation does not specify the cause of these disparities, we can conclude that these disparities exist and that low-income Americans require even greater efforts to improve their health than they currently receive.
Lifestyle habits are principal determinants of cardiometabolic diseases, major contributors to the identified health disparities in our analysis. More than 40% of SNAP participants were current smokers, compared with 26% of SNAP-eligible nonparticipants and 20% of SNAP-ineligible Americans, and only 18% met guidelines for aerobic physical activity (although this was similarly poor among SNAP-eligible nonparticipants). Suboptimal diet is a leading cause of poor health,23 and SNAP participants tend to have lower diet quality than nonparticipants.24
Modifications to SNAP provide a natural opportunity to improve the health of its participants: SNAP is an existing point of contact, diet is a major determinant of cardiometabolic diseases,12 and this is an area of active policy discussion and innovation at state and national levels. For example, recent experience in Massachusetts demonstrated that providing a financial incentive to SNAP participants of $0.30 for every $1.00 spent on fruits and vegetables increased consumption of these foods by 26%.25 On the basis of this success, the US Department of Agriculture has funded similar projects in 26 states, totaling $31 million.26 Although this is promising, this subsidy represents less than 0.1% of the $82 billion SNAP budget,3 suggesting a need for larger and broader economic incentives on more healthy food items.
In addition, SNAP could omit or provide financial disincentives for unhealthful options.27,28 For example, the recent bipartisan report on hunger and food security concluded that sugar-sweetened beverages should be removed from program eligibility,29 which has precedent in other currently omitted items such as alcohol, prepared hot foods, and dietary supplements. Although questions remain about political feasibility and implementation,10,30,31 broad public support exists for these proposals, even among SNAP participants.32,33 Another major US Department of Agriculture feeding program, the Special Supplemental Nutrition Program for Women, Infants, and Children, already contains potential exemplar health criteria.34
Several modeling studies have estimated that altering financial incentives for different foods purchased by SNAP participants would improve diets and reduce CVD and diabetes.35–37 For SNAP, a voluntary, combined incentive–restriction program (which we would term “SNAP-plus”) might be effective and well-received. If participants elected to participate in SNAP-plus, the Electronic Benefits Transfer system would provide a 30% subsidy for selected healthful foods (e.g., for each $1 spent on fruits or vegetables, 70% would come from the usual SNAP benefit and 30% from additional government subsidies) and restrictions on the use of SNAP benefits for selected unhealthful foods. Pilot studies are needed to adequately evaluate the effectiveness of restricting such purchases, and to minimize administrative challenges and burden to participants and retailers.31
More broadly, state or national pricing frameworks and incentives for industry (agriculture, manufacturers, retailers, restaurants) could increase prices of less-healthful foods and subsidize prices of more-healthful foods for all Americans, normalizing prices closer to true societal costs and thereby altering incentives across the food system to improve health and reduce disparities.38,39 Additional effective approaches for improving dietary habits can include focused mass media campaigns, food and menu labeling, changes to the built food environment, and food procurement policies and quality standards in schools, worksites, and government offices.40
The health system represents another key platform to help reduce health disparities. We found that SNAP participants were more likely than SNAP-eligible nonparticipants to have health insurance, yet still had worse outcomes, indicating a need for health systems strengthening to address their risk. For instance, several organizations are testing novel health systems strategies to better evaluate and address social determinants of health.41 Promising community approaches include standardized training of community-based health workers42 and improved reimbursement for community-based health education.43,44 Our findings highlight the need for careful investigation of the major determinants of the identified mortality differences by SNAP participation status, including the notable heterogeneity by race/ethnicity, and corresponding evidence-informed interventions and evaluation.
Strengths and Limitations
Our analysis has several strengths. This is the first study, to the best of our knowledge, to compare all-cause and cause-specific cardiometabolic mortality among SNAP participants, SNAP-eligible nonparticipants, and SNAP-ineligible individuals overall and stratified by age, gender, and race/ethnicity. The large sample size and numbers of events allowed us to detect meaningful health disparities among groups. These data are nationally representative for age, gender, and race/ethnicity, making our findings generalizable to the US population.
Potential limitations should be considered. Cause-of-death coding is subject to error, with possible overestimation of CHD mortality45,46 and underestimation of diabetes mortality.47 Thus, our findings should be considered the best available national estimates, rather than perfect clinical determination, of mortality differences. The overall NHIS response rate was 82% to 88%; although this is relatively high, SNAP participants were 6% of the sample, compared with 8% to 9% of all US adults during the same time period.48–50 This indicates either underparticipation or underreporting by SNAP participants in NHIS, as observed by others,6 and may result from sicker individuals, who may be more likely to participate in SNAP, being less likely to participate in national surveys. Thus, our findings may underestimate the true mortality differences according to SNAP participation.
The NHIS survey does not assess the duration of time individuals have been in SNAP, and SNAP participation is also dynamic over time, with changes in monthly participation status as household income and other conditions vary.51 As a consequence, some participants may have been misclassified because of movement in and out of SNAP over time. Yet, the mortality differences we observed were stable over time, indicating that, even with some inevitable misclassification, SNAP participation status over the previous year usefully discriminates future health risk. Our analysis aimed to determine and describe mortality differences according to SNAP status, not draw inference on causal effects of participating in SNAP. Other household and individual characteristics and conditions may be related to both SNAP participation and risk of mortality; our findings heighten the need to identify and address the determinants of these poor health outcomes.
Public Health Implications
Individuals participating in SNAP exhibited higher risk of subsequent all-cause and cause-specific cardiometabolic mortality compared with SNAP-eligible nonparticipants and SNAP-ineligible individuals, particularly for diabetes mortality. These mortality differences were consistent by age and gender, whereas racial/ethnic differences and disparities were more varied. These results show that low-income Americans require even greater efforts to improve their health than they currently receive, and such efforts should be a priority for public health policymakers.
ACKNOWLEDGMENTS
This study was supported by the National Heart, Lung, and Blood Institute, R01 HL115189.
Note. The funding agency did not contribute to study design and conduct; data collection, management, analysis, or interpretation; preparation, review, or approval of the article; or decision to submit the article for publication.
HUMAN PARTICIPANT PROTECTION
Institutional review was not needed because human participants were not involved in this study.
Footnotes
See also Galea and Vaughan, p. 363.
REFERENCES
- 1.US Department of Agriculture, Food and Nutrition Service. Supplemental Nutrition Assistance Program (SNAP) 2015. Available at: http://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program-snap. Accessed November 11, 2016.
- 2.US Department of Agriculture, Food and Nutrition Service. Supplemental Nutrition Assistance Program (SNAP) national level annual summary. 2016. Available at: http://www.fns.usda.gov/pd/supplemental-nutrition-assistance-program-snap. Accessed November 11, 2016.
- 3.US Department of Agriculture. FY 2016 Budget Summary and Performance Plan. 2015. Available at: http://www.usda.gov/wps/portal/usda/usdahome?navid=BUDGET. Accessed November 11, 2016.
- 4.US Department of Agriculture, Food and Nutrition Service. Supplemental Nutrition Assistance Program (SNAP) eligibility. 2016. Available at: http://www.fns.usda.gov/snap/eligibility. Accessed November 11, 2016.
- 5.US Census Bureau. How the Census Bureau measures poverty. 2016. Available at: http://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html. Accessed November 11, 2016.
- 6.Bitler M. The health and nutrition effects of SNAP: selection into the program and a review of the literature on its effects. 2014. University of Kentucky Center for Poverty Research Discussion Paper Series, DP2014-02. Available at: http://uknowledge.uky.edu/ukcpr_papers/8. Accessed November 15, 2016.
- 7.Nguyen BT, Shuval K, Bertmann F, Yaroch AL. The Supplemental Nutrition Assistance Program, food insecurity, dietary quality, and obesity among US adults. Am J Public Health. 2015;105(7):1453–1459. doi: 10.2105/AJPH.2015.302580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeBono NL, Ross NA, Berrang-Ford L. Does the food stamp program cause obesity? A realist review and a call for place-based research. Health Place. 2012;18(4):747–756. doi: 10.1016/j.healthplace.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Leung CW, Willett WC, Ding EL. Low-income Supplemental Nutrition Assistance Program participation is related to adiposity and metabolic risk factors. Am J Clin Nutr. 2012;95(1):17–24. doi: 10.3945/ajcn.111.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pomeranz JL, Chriqui JF. The Supplemental Nutrition Assistance Program: analysis of program administration and food law definitions. Am J Prev Med. 2015;49(3):428–436. doi: 10.1016/j.amepre.2015.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krueger PM, Rogers RG, Ridao-Cano C, Hummer RA. To help or to harm? Food stamp receipt and mortality risk prior to the 1996 Welfare Reform Act. Soc Forces. 2004;82(4):1573–1599. [Google Scholar]
- 12.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187–225. doi: 10.1161/CIRCULATIONAHA.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mozaffarian D, Benjamin EJ, Go AS et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services, Centers for Disease Control and Prevention. National Health Interview Survey, 2000–2009. Available at: http://www.cdc.gov/nchs/nhis/index.htm. Accessed November 15, 2016.
- 15.US Department of Health and Human Services, Centers for Disease Control and Prevention. Linkage methods/analytical support. Available at: http://www.cdc.gov/nchs/data_access/data_linkage/mortality/linkage_methods_analytical_support.htm. Accessed November 15, 2016.
- 16.US Census Bureau. American Community Survey, Public-Use Microdata Sample. 2016. Available at: http://www.census.gov/programs-surveys/acs/technical-documentation/pums/about.html. Accessed November 8, 2016.
- 17.Schenker N, Raghunathan TE, Chiu PL, Makuc DM, Zhang GY, Cohen AJ. Multiple imputation of missing income data in the National Health Interview Survey. J Am Stat Assoc. 2006;101(475):924–933. [Google Scholar]
- 18.US Department of Health and Human Services, Centers for Disease Control and Prevention. National Death Index. Available at: http://www.cdc.gov/nchs/ndi.htm. Accessed November 15, 2016.
- 19.Hermansen SW, Leitzmann MF, Schatzkin A. The impact on National Death Index ascertainment of limiting submissions to Social Security Administration Death Master File matches in epidemiologic studies of mortality. Am J Epidemiol. 2009;169(7):901–908. doi: 10.1093/aje/kwn404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12(7):462–468. doi: 10.1016/s1047-2797(01)00285-x. [DOI] [PubMed] [Google Scholar]
- 21.Gray KF, Kochhar S. Characteristics of Supplemental Nutrition Assistance Program households: fiscal year 2014. US Department of Agriculture, Food and Nutrition Service. 2015. Available at: http://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program-snap/reports-all. Accessed November 15, 2016.
- 22.Gundersen C, Jolliffe D, Tiehen L. The challenge of program evaluation: when increasing program participation decreases the relative well-being of participants. Food Policy. 2009;34(4):367–376. [Google Scholar]
- 23.Murray CJ, Atkinson C, Bhalla K et al. US Burden of Disease Collaborators. The state of U.S. health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: a systematic review. Am J Prev Med. 2015;49(4):594–604. doi: 10.1016/j.amepre.2015.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bartlett S, Klerman J, Olsho L . Evaluation of the Healthy Incentives Pilot (HIP): Final Report. US Department of Agriculture, Food and Nutrition Service; 2014. Available at: http://www.fns.usda.gov/hip/healthy-incentives-pilot. Accessed November 15, 2016. [Google Scholar]
- 26.US Department of Agriculture, National Institute of Food and Agriculture. Food Insecurity Nutrition Incentive (FINI) grant program. 2016. Available at: https://nifa.usda.gov/program/food-insecurity-nutrition-incentive-fini-grant-program. Accessed November 15, 2016.
- 27.Leung CW, Hoffnagle EE, Lindsay AC et al. A qualitative study of diverse experts’ views about barriers and strategies to improve the diets and health of Supplemental Nutrition Assistance Program (SNAP) beneficiaries. J Acad Nutr Diet. 2013;113(1):70–76. doi: 10.1016/j.jand.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blumenthal SJ, Hoffnagle EE, Leung CW et al. Strategies to improve the dietary quality of Supplemental Nutrition Assistance Program (SNAP) beneficiaries: an assessment of stakeholder opinions. Public Health Nutr. 2014;17(12):2824–2833. doi: 10.1017/S1368980013002942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Commission on Hunger. Freedom From Hunger: An Achievable Goal for the United States of America. 2015. Available at: http://cybercemetery.unt.edu/archive/hungercommission/20151217000051/https://hungercommission.rti.org. Accessed November 15, 2016.
- 30.Pomeranz JL. Implications of the Supplemental Nutrition Assistance Program tax exemption on sugar-sweetened beverage taxes. Am J Public Health. 2015;105(11):2191–2193. doi: 10.2105/AJPH.2015.302850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Department of Agriculture, Food and Nutrition Service. Implications of restricting the use of food stamp benefits. 2007. Available at: http://www.fns.usda.gov/sites/default/files/arra/FSPFoodRestrictions.pdf. Accessed November 15, 2016. [Google Scholar]
- 32.Long MW, Leung CW, Cheung L, Blumenthal SJ, Willett WC. Public support for policies to improve the nutritional impact of the Supplemental Nutrition Assistance Program (SNAP) Public Health Nutr. 2014;17(1):219–224. doi: 10.1017/S136898001200506X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leung CW, Ryan-Ibarra S, Linares A et al. Support for policies to improve the nutritional impact of the Supplemental Nutrition Assistance Program in California. Am J Public Health. 2015;105(8):1576–1580. doi: 10.2105/AJPH.2015.302672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Agriculture, Food and Nutrition Service. Women, Infants, and Children (WIC): WIC food packages—regulatory requirements for WIC-eligible foods. 2016. Available at: http://www.fns.usda.gov/wic/wic-food-packages-regulatory-requirements-wic-eligible-foods. Accessed November 15, 2016.
- 35.Basu S, Seligman H, Bhattacharya J. Nutritional policy changes in the Supplemental Nutrition Assistance Program: a microsimulation and cost-effectiveness analysis. Med Decis Making. 2013;33(7):937–948. doi: 10.1177/0272989X13493971. [DOI] [PubMed] [Google Scholar]
- 36.Basu S, Seligman HK, Gardner C, Bhattacharya J. Ending SNAP subsidies for sugar-sweetened beverages could reduce obesity and type 2 diabetes. Health Aff (Millwood) 2014;33(6):1032–1039. doi: 10.1377/hlthaff.2013.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Long MW, Gortmaker SL, Ward ZJ et al. Cost effectiveness of a sugar-sweetened beverage excise tax in the US. Am J Prev Med. 2015;49(1):112–123. doi: 10.1016/j.amepre.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mozaffarian D, Rogoff KS, Ludwig DS. The real cost of food: can taxes and subsidies improve public health? JAMA. 2014;312(9):889–890. doi: 10.1001/jama.2014.8232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colchero MA, Popkin BM, Rivera JA, Ng SW. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016;352:h6704. doi: 10.1136/bmj.h6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Afshin A, Penalvo J, Del Gobbo L et al. CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet. Curr Cardiol Rep. 2015;17(11):98. doi: 10.1007/s11886-015-0658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48(2):215–218. doi: 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 42.Kim K, Choi JS, Choi E et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106(4):e3–e28. doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peek ME, Ferguson M, Bergeron N, Maltby D, Chin MH. Integrated community-healthcare diabetes interventions to reduce disparities. Curr Diab Rep. 2014;14(3):467. doi: 10.1007/s11892-013-0467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clark NM, Quinn M, Dodge JA, Nelson BW. Alliance system and policy change: necessary ingredients for improvement in diabetes care and reduction of disparities. Health Promot Pract. 2014;15(2 suppl):11S–22S. doi: 10.1177/1524839914543829. [DOI] [PubMed] [Google Scholar]
- 45.Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: time for a reassessment? J Am Coll Cardiol. 1999;34(3):618–620. doi: 10.1016/s0735-1097(99)00250-8. [DOI] [PubMed] [Google Scholar]
- 46.Messite J, Stellman SD. Accuracy of death certificate completion: the need for formalized physician training. JAMA. 1996;275(10):794–796. [PubMed] [Google Scholar]
- 47.Andresen EM, Lee JA, Pecoraro RE, Koepsell TD, Hallstrom AP, Siscovick DS. Underreporting of diabetes on death certificates, King County, Washington. Am J Public Health. 1993;83(7):1021–1024. doi: 10.2105/ajph.83.7.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cunnyngham K. Characteristics of Supplemental Nutrition Assistance Program households: fiscal year 2000. US Department of Agriculture, Food and Nutrition Service. 2001. Available at: http://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program-snap/reports-all. Accessed November 15, 2016.
- 49.Leftin J, Gothro A, Eslami E. Characteristics of Supplemental Nutrition Assistance Program households: fiscal year 2009. US Department of Agriculture, Food and Nutrition Service. 2010. Available at: http://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program-snap/reports-all. Accessed November 15, 2016.
- 50.US Census Bureau, Bureau of Labor Statistics. Current Population Survey 2000–2009, data on age and sex. Available at: https://www.census.gov/population/age/data/cps.html. Accessed November 15, 2016.
- 51.Leftin J, Wemmerus N, Mabli J, Godfrey T, Tordella S. Dynamics of Supplemental Nutrition Assistance Program participation from 2008–2012. 2014. Available at: http://www.fns.usda.gov/dynamics-and-determinants-supplemental-nutrition-assistance-program-participation-2008-2012. Accessed November 15, 2016.