Abstract
Background and Aims:
Excessive requests for cross matching blood which is more than the blood required for transfusion are usually based on worst case assumptions leading to overestimation of blood usage. We investigated the blood ordering pattern and transfusion practices so as to incorporate a blood ordering schedule for streamlining the use of blood in various hospital departments.
Methods:
The study was conducted over a period of 19 months in a 350 bedded tertiary teaching hospital. Source of data was blood bank requisition forms and blood bank registers of patients who underwent elective or emergency procedures in the hospital, for which blood was ordered. Data were entered in MS Excel and analysed using SPSS version 20.
Results:
The blood bank was requested to prepare 10,594 units of blood for 2556 patients. The blood utilised was 16.04% of total cross matched blood, leaving 83.9% of units cross matched but not transfused to patient for whom it was prepared, i.e., wasted. The surgery department had the highest number of units cross matched and transfused. The least number of units cross matched and wasted due to non-transfusion were from the Department of Oncology.
Conclusion:
The current deficiency of explicit maximum blood order schedule in our hospital is the major factor responsible for high cross match: transfusion ratio. Therefore, a maximal surgical blood order schedule has been suggested to the hospital transfusion committee to implement maximum surgical blood order schedules for selected procedures.
Keywords: Cross match: transfusion ratio, transfusion practices, transfusion probability
INTRODUCTION
The transfusion of blood and blood products is an integral and essential part of hospital services. The blood requisition in elective and emergency procedures from Surgery, Trauma and Obstetrics and Gynaecology Departments are often associated with excessive demand for cross matching of blood which is often more than the required blood and blood products. This is usually based on worst case assumptions leading to overestimation of blood usage. The transfusion services, thus, are burdened in terms of unnecessary reagent usage, time and manpower. Over-ordering of blood leads to financial loss for the patient, increase in cost during the hospital stay and increase in demand for blood. This study aimed to investigate the blood ordering pattern for maximum utilisation of blood and pave the way for formulating maximum surgical blood ordering schedule (MSBOS) for procedures where a complete crossmatch appears mandatory. The MSBOS is a list of common elective surgical procedures for which the maximum numbers of units of blood are cross matched pre-operatively for each procedure.[1,2,3]
The elective surgeries utilise only 30% of cross matched blood and are viewed as one of the areas of hospital wastage of this vital resource.[4] Many studies have been conducted on blood ordering and transfusion practices in elective surgery and have demonstrated over-ordering and underutilisation of blood.[1,5]
A number of studies have shown meaningful reductions in crossmatch requests, number of units cross matched and units transfused after MSBOS was implemented and group and screen were introduced.[1] Units cross matched fell slightly more than the units transfused, resulting in the lower cross match: transfusion ratios (CTRs) and indicating more effective use of resources.
Therefore, the aim of the study was to investigate the blood ordering pattern and transfusion practices and subsequently incorporate a blood ordering schedule which streamlines the use of blood and blood products for elective and emergency surgical procedures and, therefore, decrease over-ordering of blood.
METHODS
An observational study was conducted over a period of 19 months from February 2014 to September 2015 in a 350-bedded tertiary care hospital.
Source of data was blood bank requisition forms and blood bank registers of patients who underwent elective or emergency procedures in the hospital, for which blood was ordered. Ethical approval was taken from the Institutional Ethical Committee. Patients’ age and sex, diagnosis, type of procedure performed, pre-procedure haemoglobin level and number of blood units required to be cross matched and transfused were obtained from blood bank requisition form.
The number of units prepared, cross matched and transfused as well as the number of patients for whom cross matching and transfusion were done was collected from blood bank registers. The blood which was cross matched but not transfused was considered as wasted. For the purpose of analysis, the department was categorised into Surgical, Obstetrics and Gynaecology, Medicine and Oncology.
Data were entered and analysed using SPSS version 20. Blood utilisation indices were computed with the following equation using MS Excel.
CTR = number of units cross matched/number of units transfusedA ratio of 2.5 and below is considered indicative of significant blood usage[1]
Transfusion probability (%T) = number of patients transfused/number of patients cross matched × 100. A value of 30% and above was considered indicative of efficient blood usage[6]
Transfusion index (TI) = number of units transfused/number of patients cross matched. A value of 0.5 or more was considered indicative of significant blood utilisation[6]
Mead's criteria:[6] MSBOS = 1.5 × TI
Code numbers were used instead of personal identification nomenclatures and the data were kept locked to maintain confidentiality of the information.
RESULTS
During the study, the hospital blood bank was requested to prepare 10,594 units of blood for 2556 patients who underwent major elective and emergency procedures. The majority of the patients were females, 1507 (59.2%), who underwent procedures in the elective schedule, and blood for transfusion was arranged by replacement donation [Table 1]. The blood units prepared per patient ranged from one to six units. From 10,594 units prepared, 1700 (16.04%) units were transfused and rest 8892 (83.9%) were prepared but not transfused. Thus, only 16.04% of total blood cross matched was utilised, leaving 83.9% of the units cross matched but not transfused to the patient for whom it was prepared, i.e., wasted. Surgery Department had the highest number of patients cross matched, 988 (38.7%), as well as with the highest no of units reserved, 5056 (47.72%), but not transfused, 4608 (43.5%). On the other hand, Obstetrics and Gynaecology were the departments with the second highest number of units cross matched and reserved for transfusion, 2162 (20.4%), but not transfused 1714 (16.17%).
Table 1.
Socio demographic and other characteristics of patients (N=10594)
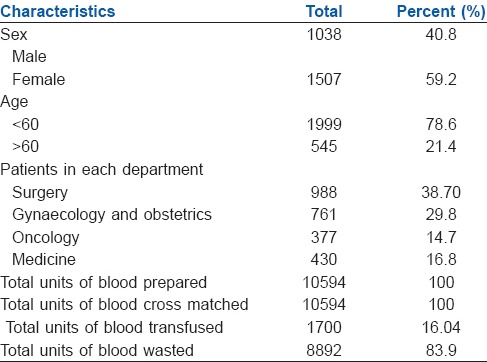
In the study that spanned over 19 months, a total of 10,594 blood requests were received. The Department of Surgery made 5056 (47.72%) requests for cross matched blood products followed by department of Obstetrics and Gynaecology which made 2162 (20.4%) requests. The blood crossmatch requests from the Department of Medicine were 1969 (18.58%), and the Oncology Department made 1407 (13.28%) requests for blood. A total of 10,594 units were cross matched, and of these, 1700 (16.04%) units were utilised, leading to 8892 (83.9%) of units not utilised due to non-transfusion [Figure 1].
Figure 1.
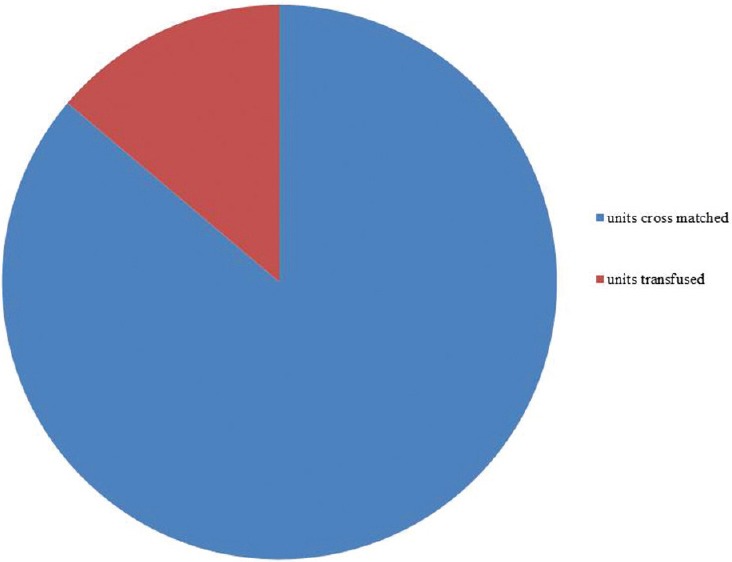
Number of units (cross matched versus transfused)
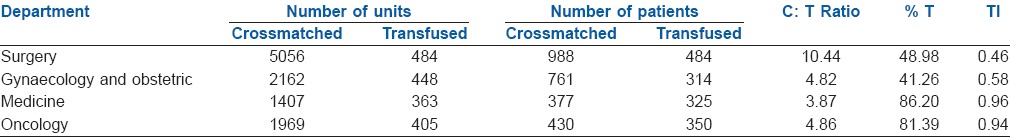
The comprehensive blood utilisation indices of the hospital were C/T ratio = 6.23. The %T = 57.62% and TI = 0.66, respectively. However, the blood utilisation indices of patients in different departments revealed different values [Table 2].
Table 2.
Comparison between number of units cross matched and transfused
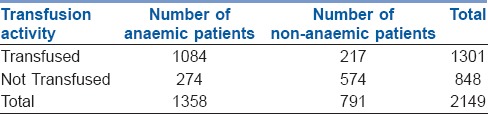
The most common reason for transfusion was anaemia, with haemoglobin of <10 g/dl. Overall number 1084 (63.2%) of patients who were anaemic pre-operatively were transfused and had more transfusions as compared to patients with normal pre-operative haemoglobin [Table 3].
Table 3.
Transfusion activity in relation to anaemia
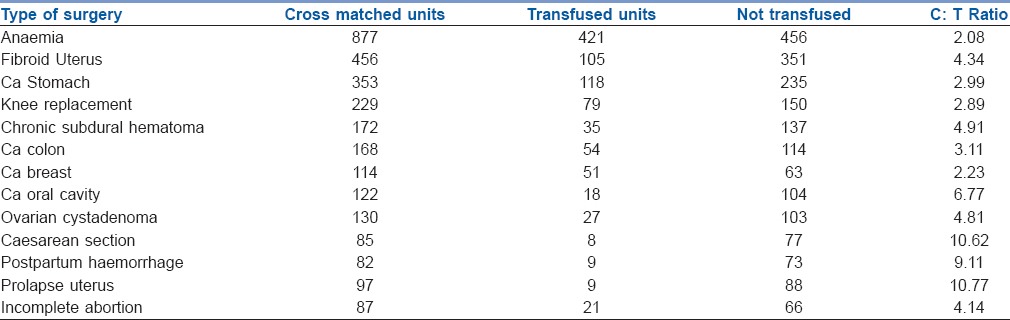
Eleven out of thirteen procedures had a CTR higher than 2.5. The majority of these procedures belonged to the Department of Obstetrics and Gynaecology and Surgery [Table 4].
Table 4.
Blood cross-match and transfusion patterns for different procedures with high C: T Ratio
DISCUSSION
The study aimed to investigate the blood ordering pattern and transfusion practices. The study revealed that the blood products which are cross matched for the purpose of transfusion are not transfused, and this impacts the transfusion services by underutilisation or over-ordering of blood products. The CTR in some procedures in our study varied from 2 to 10.6, and there is over-ordering of blood products in many procedures. The over-requisition of blood without subsequent utilisation has been reported by earlier workers.[5,7,8] The reason of over-ordering for blood is frequently based on the subjective anticipation of blood loss instead of audit-based estimates of the requirement in a particular procedure. The practice of making blood ready before scheduling a surgery may also be responsible for such a scenario combined with the fact that there is a great tendency to request more units of blood for elective procedures than what is actually required.
The current study revealed that 83.9% % of the cross matched blood was unutilised. Higher CTRs have also been reported by Collins et al. among the surgical categories, wherein the percentage of cases where none of the issued red blood cells were transfused ranged up to 93%, suggesting that gross over-ordering of crossmatches are seen in certain surgeries.[9] Similar findings were observed in our study where the surgical procedures of caesarean section, postpartum haemorrhage, prolapse uterus and carcinoma of oral cavity had higher CTRs. Further procedures such as ovarian cystadenomas, chronic subdural haematoma and incomplete abortions also had high CTRs.
The CTR is used[5] for evaluating blood transfusion practices. The overall CTR of 6.31 observed in the current study is considered to be indicative of inefficient blood usage. Still, the CTR widely varied and was very high in many surgeries of the Department of Surgery and Gynaecology and Obstetrics. Similar findings regarding certain surgeries are observed in another study by Subramanian et al., which revealed that certain surgeries such as cholecystectomy (open/laparoscopic), thyroidectomy, ureterolithotomy, gastro/cysto-jejunostomy, vagotomy/pyloroplasty, incisional hernia repair, varicose vein surgery and omentopexy had none of the three indices showing optimum blood utilisation.[10]
The probability of transfusion for a given procedure (%T), which signifies the probability of transfusion, and a value of 30% and above have been suggestive of significant blood usage.[11] The results of the present study revealed an overall transfusion probability of 57.62% as % T is dependent on the number of patients transfused and indicates appropriate transfusion as compared to number of units crossmatched per patient which were in excess of those transfused. This finding is similar to the study by Subramanian et al., in which %T for laprotomy, vascular surgery, amputation, few neck procedures and orthopaedic procedures was >50%.[10]
Regarding TI, a value of 0.5 or more is indicative of significant blood utilisation.[4] The TI reported in the current study was 0.65. Reports of TI in the range of 0.1 to 0.4 has also been reported in various surgical procedures.[12] This finding of higher blood ordering pattern, especially in the Department of Surgery and Obstetrics and Gynaecology, needs to be revised and over-ordering of blood should be minimised.
The Obstetrics and Gynaecology and Surgery Unit had the highest consumption of requested blood with a CTR of 4.82 and 10.96, respectively, and %T of 41.26% and 48.98%, respectively. Although the overall CTR is raised, still the %TI reflects appropriate blood usage for the respective departments as this finding may reflect the anticipated transfusion requirement of patients with caesarean section, postpartum haemorrhage, prolapsed uterus and debulking surgery for carcinomas which lead to more number of blood units being cross matched per patient and less number of units transfused per patient. Furthermore, low incidence of prophylactic patient blood management in the aforementioned conditions may have contributed to high CTR.
Ineffectual transfusion practice with a high CTR and %T as observed in the present study has led to unnecessary wastage of blood and unavailability of blood for patients in need as cross matched blood is usually held in reserve. A similar pattern of over-ordering of blood leading to holding up of blood bank reserve as cross matched blood is considered reserved blood has been observed by Bashawri et al.[11] Patients requiring blood immediately or with legitimate blood requirements are deprived of it. This results in aging of blood units and wastage of blood bank resources.[13] This also leads to increase in the workload of blood bank personnel as well as wastage of reagents, workforce and time with financial implications to both the patient and blood bank.[14]
The factors predictive of pre- and peri-operative blood transfusion are anaemia as RBC transfusion is the only way to rapidly treat severe anaemia.[15]
In the absence of an explicit MSBOS, ordering for blood transfusion is frequently based on the subjective anticipation of blood loss instead of audit-based estimates of the requirement in a particular procedure. The current deficiency of explicit MSBOS in our hospital is the major factor responsible for this. Based on the findings in our study, a Maximal Surgical Blood Order Schedule calculation by the formula 1.5 × TI[6] has been suggested to the hospital transfusion committee. The formulation of data-driven MSBOS and adhering to transfusion guidelines and prospective audit allied to educational programmes may be effective in modifying clinician's behaviour in ordering transfusions and, therefore, reduce the number of unused units and generate considerable cost savings.[14] However, transfusion requirements are subjective, and there is no fool proof way which can estimate blood loss or intraoperative modifications. The universal implementation of MSBOS within the institute is another hurdle.[16]
Other measures with proven improvement in CTR and %T are type and screen (T and S), save and abbreviated crossmatch.[14] The MSBOS specifies the number of blood units to be routinely cross matched for elective surgical procedures based on retrospective analysis of actual blood usage for these procedures.[14] The T and S is determination of the patient's ABO group and Rh type and screening for unexpected, clinically significant allo-antibodies. If the screen is negative, ABO-compatible blood from the local inventory can be used with a quick spin crossmatch. By contrast, if the antibody screen is positive, then workup is necessary to determine the target antigen and identifying antigen-negative units for transfusion. The limitation of our study is that data was collected and catogorized into four broad specialities, however data on use of blood in OT/Critical Care, surgical speciality may have provided more useful insights.
CONCLUSION
Developing a blood ordering policy, which is a guide to expect normal blood usage for surgical procedures, can decrease over-ordering of blood, thereby reducing unnecessary compatibility testing, returning of unused blood and wastage due to outdating. It also allows for a more efficient management of blood inventory. In this respect, the hospital blood transfusion committee has to implement MSBOSs for selected surgical procedures, conduct regular auditing about the effectiveness of the blood requesting policy using the CTR and offer periodic feedbacks to improve blood ordering, handling, distribution and utilisation practices of this scarce resource.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Friedman BA, Oberman HA, Chadwick AR, Kingdon KI. The maximum surgical blood order schedule and surgical blood use in the United States. Transfusion. 1976;16:380–7. doi: 10.1046/j.1537-2995.1976.16476247063.x. [DOI] [PubMed] [Google Scholar]
- 2.Friedman BA. An analysis of surgical blood use in United States hospitals with application to the maximum surgical blood order schedule. Transfusion. 1979;19:268–78. doi: 10.1046/j.1537-2995.1979.19379204208.x. [DOI] [PubMed] [Google Scholar]
- 3.Carter L, Kim SJ, Schneidman-Duhovny D, Stöhr J, Poncet-Montange G, Weiss TM, et al. Prion protein-antibody complexes characterized by chromatography-coupled small-angle X-ray scattering. Biophys J. 2015;109:793–805. doi: 10.1016/j.bpj.2015.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sowayan SA. Use of blood in elective surgery: An area of wasted hospital resource. Ann Saudi Med. 1994;14:326–8. doi: 10.5144/0256-4947.1994.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olawunmi HO, Bolaji BO. Blood utilization in elective surgical procedures in Ilorin. Trop J Health Sci. 2006;13:15–7. [Google Scholar]
- 6.Mead JH, Anthony CD, Sattler M. Hemotherapy in elective surgery: An incidence report, review of the literature, and alternatives for guideline appraisal. Am J Clin Pathol. 1980;74:223–7. doi: 10.1093/ajcp/74.2.223. [DOI] [PubMed] [Google Scholar]
- 7.Musa AU, Ndakotsu MA, Hassan A, Kilishi A, Kwaifa IK. Pattern of blood transfusion request and utilization at a Nigerian University Teaching Hospital. Sahel Med J. 2014;17:19–22. [Google Scholar]
- 8.Collins RA, Wisniewski MK, Waters JH, Triulzi DJ, Alarcon LH, Yazer MH. Excessive quantities of red blood cells are issued to the operating room. Transfus Med. 2015;25:374–9. doi: 10.1111/tme.12263. [DOI] [PubMed] [Google Scholar]
- 9.Vibhute M, Kamath SK, Shetty A. Blood utilisation in elective general surgery cases: Requirements, ordering and transfusion practices. J Postgrad Med. 2000;46:13–7. [PubMed] [Google Scholar]
- 10.Subramanian A, Sagar S, Kumar S, Agrawal D, Albert V, Misra MC. Maximum surgical blood ordering schedule in a tertiary trauma center in Northern India: A proposal. J Emerg Trauma Shock. 2012;5:321–7. doi: 10.4103/0974-2700.102391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bashawri LA. Pattern of blood procurement, ordering and utilization in a University Hospital in Eastern Saudi Arabia. Saudi Med J. 2002;23:555–61. [PubMed] [Google Scholar]
- 12.Ebose EM, Osalumese IC. Blood shortage situation: An audit of red blood cell order and pattern of utilization. Afr J Biotechnol. 2009;8:5922–5. [Google Scholar]
- 13.Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, et al. Guidelines for the clinical use of red cell transfusions. Br J Haematol. 2001;113:24–31. doi: 10.1046/j.1365-2141.2001.02701.x. [DOI] [PubMed] [Google Scholar]
- 14.Pei Z, Szallasi A. Prevention of surgical delays by pre-admission type and screen in patients with scheduled surgical procedures: Improved efficiency. Blood Transfus. 2015;13:310–2. doi: 10.2450/2014.0172-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du Pont-Thibodeau G, Harrington K, Lacroix J. Anemia and red blood cell transfusion in critically ill cardiac patients. Ann Intensive Care. 2014;4:16. doi: 10.1186/2110-5820-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iyer SS, Shah J. Red blood cell transfusion strategies and maximum surgical blood ordering schedule. Indian J Anaesth. 2014;58:581–9. doi: 10.4103/0019-5049.144660. [DOI] [PMC free article] [PubMed] [Google Scholar]


