Abstract
Background and Aims:
Laryngoscopic manipulation and endotracheal intubation are noxious stimuli capable of producing tachycardia, arrhythmias and hypertension. The aim of this study was to arrive at an optimal dose of dexmedetomidine by comparing two doses with placebo to attenuate stress response during laryngoscopy and endotracheal intubation.
Methods:
It was a randomised, prospective, double-blind placebo-controlled study. After Institutional Ethical Committee clearance, ninety patients of American Society of Anesthesiologists Physical Status 1 were enrolled in the study and divided into three equal groups. Group A received normal saline, Group B received injection dexmedetomidine 0.5 μg/kg and Group C received injection dexmedetomidine 0.75 μg/kg as infusion over 10 min. The general anaesthesia technique was standardised for all three groups. The primary outcome measures were haemodynamic response at 1, 3 and 5 min after intubation. The secondary outcome measures were to note down any adverse effects associated with drugs. The statistical package used was SPSS version 15.
Results:
Groups were well matched for their demographic data. There was a statistically significant difference (P < 0.05) between dexmedetomidine and normal saline in heart rate, systolic, diastolic and mean arterial pressures at all time points after tracheal intubation with dexmedetomidine 0.75 μg/kg being most effective. Sedation scores were more with dexmedetomidine. None of the patients had any adverse effects such as hypotension, bradycardia, respiratory depression and fall in oxygen saturation.
Conclusion:
Dexmedetomidine in a dose of 0.75 μg/kg intravenous is the optimal dose to attenuate stress response to laryngoscopy and endotracheal intubation.
Keywords: Anaesthesia, dexmedetomidine, general, intubation, laryngoscopy
INTRODUCTION
The augmented cardiovascular reflexes in the form of tachycardia and hypertension brought about by the noxious stimulus of laryngoscopy and intubation can prove to be detrimental for patients with cardiovascular and cerebrovascular diseases.[1] Several drugs and techniques have been tried by anaesthesiologists to attenuate the stress response to laryngoscopy and endotracheal intubation. α-2 agonists such as clonidine and dexmedetomidine have been used by some researchers for attenuation of the stress response to laryngoscopy. Few authors have used dexmedetomidine in a dose of 0.5 and 1 μg/kg and found them to be effective in attenuation of stress response to laryngoscopy and endotracheal intubation.[2,3,4] Although they found promising results, the higher dose of 1 μg/kg was associated with increased incidence of cardiovascular compromise in the form of hypotension and bradycardia.[3,4] It has also been found to be associated with increased sedation.[5] There are no studies until date with dexmedetomidine in a dose of 0.75 μg/kg. Hence, this study was undertaken with different doses of dexmedetomidine and comparing it with normal saline to arrive at an optimal dose of dexmedetomidine for attenuation of stress response to laryngoscopy and endotracheal intubation.
METHODS
After obtaining Institutional Ethical Committee clearance, the study was conducted at our Medical College Hospital. Ninety patients belonging to American Society of Anesthesiologists (ASA) Physical Status 1 in the age group of 18 –50 years of either sex, posted for elective surgeries under general anaesthesia, were enrolled for the study. Patients who were physically dependent on narcotics, those with a history of bronchial asthma, drug or alcohol abuse, known drug allergy to either clonidine or dexmedetomidine, cerebrovascular, neurologic, respiratory or ischemic heart disease (history of angina, previous myocardial infarction) and renal and hepatic dysfunction were excluded from the study. Patients with hypertension, diabetes mellitus, phaeochromocytoma, patients on β-blockers, antidepressants, anxiolytics, anticonvulsant or antipsychotics and any predicted difficult airway were also excluded from the study. Patients in whom laryngoscopy time exceeded 15 s were excluded from analysis.
All patients were provided with patient information sheet and written informed consent was obtained. All patients were evaluated a day before surgery. The patients were kept fasting overnight after 10:00 pm and received tablet ranitidine 150 mg orally and tablet alprazolam 0.5 mg orally as premedication at night before surgery. Patients were randomly divided into three groups of thirty each. Randomisation was done using computer-generated random number table. The double-blinding procedure was followed, in which the person administering the drug and the patients both were unaware as to which group the patient belonged to. One consultant anaesthesiologist prepared the intravenous (IV) infusions and coded them. The infusions were handed over to the resident anaesthetist to be administered to the patients. The resident anaesthetist was unaware of the contents of the syringe. The resident anaesthetist who administered the infusions recorded the parameters. The patients were unaware as to which group they belonged to. The results of the study were analysed at the end of the study and then the decoding procedure was done. Group A received 20 ml normal saline IV as infusion over 10 min. Group B received IV dexmedetomidine 0.5 μg/kg diluted to 20 ml with normal saline as infusion over 10 min. Group C received IV dexmedetomidine 0.75 μg/kg diluted to 20 ml with normal saline as infusion over 10 min.
All patients were monitored with electrocardiography, pulse oximetry and non-invasive blood pressure. An IV line was secured, and the patients were administered IV fluid Ringer's lactate. IV glycopyrrolate 0.2 mg and IV ondansetron 50 μg/kg IV were given half an hour before induction. Baseline heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP) and oxygen saturation (SpO2) were measured after premedication. After 10 min, study drug infusion was given over 10 min. Any hypotension (SBP fall >20% from the baseline) was treated with increments of IV mephentermine 3 mg, and incidence of bradycardia (HR <50 beats) was treated with IV atropine 0.6 mg. After completion of drug infusion, sedation was assessed at 2, 5 and 10 min using Ramsay sedation score.[6] After noting the sedation scores and monitoring the haemodynamics for 10 min, the anaesthetic procedure was initiated. All the patients were pre-oxygenated for 3 min. General anaesthesia technique was standardised for all the three groups. Then, patients were induced with IV propofol 2 mg/kg bodyweight with IV lignocaine (preservative free) in concentration of 0.1% (1 mg of lignocaine to 1 ml of propofol), IV fentanyl 1 μg/kg and IV succinylcholine 2 mg/kg body weight. Following laryngoscopy and endotracheal intubation, the parameters recorded were HR, SBP, DBP and MAP at 1, 3 and 5 min after intubation. Anaesthesia was maintained with O2 and N2O in a ratio of 50% each and isoflurane 0.4%. Muscle relaxation was maintained with IV vecuronium 0.1 mg/kg with top ups of 0.04 mg/kg. After surgery, reversal was achieved with IV neostigmine 0.05 mg/kg and IV glycopyrrolate 0.01 mg/kg. After adequate recovery, patients were shifted to post-anaesthesia care unit and monitored for 12 h and later shifted to ward.
The primary objective of the study was to arrive at an optimal dose of IV dexmedetomidine by comparing different doses of the drug with normal saline in terms of attenuation of haemodynamic stress response to laryngoscopy and endotracheal intubation.
The statistician was involved before the start of the study. As per directions from statistician, a pilot study was conducted. The sample size was estimated using the mean HR at 5 min in three groups after pilot study. At 95% confidence limit and 90% power, a sample size of 26 was obtained in each group by taking largest mean difference at 7.91 and expected background standard deviation (SD) of 9.1. With 10% non-response sample size of 26 + 2.6, 30 participants were included in the study in each group.
Descriptive and inferential statistical analyses were carried out in the present study. software, statistical package for social sciences (SPSS) version 15 SPSS Inc, Chicago, USA. was used to analyse the data. Results on continuous measurements are presented as mean ± SD and results on categorical measurements are presented in number (%). Significance was assessed at 5 % level of significance.
Analysis of variance was used to find the significance of study parameters between three or more groups of patients. Post hoc Tukey test was used to find the pairwise significance (statistically significant P < 0.05).
RESULTS
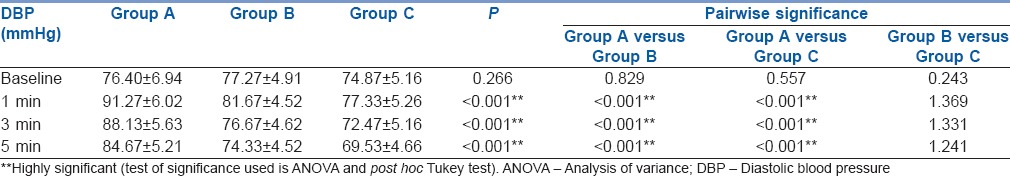
The groups were well matched for their demographic data [Table 1]. The surgeries routinely performed in our institute such as tympanoplasty, mastoidectomy, functional endoscopic sinus surgeries, breast surgeries such as fibroadenoma excision, laparoscopic surgeries such as appendicectomy and cholecystectomy and various orthopaedic surgeries such as upper limb fractures and microlumbar discectomies were included in our study. The basal readings of HR, SBP, DBP and MAP were similar in all the three groups. Maximum intubation response was seen at 1 min post-intubation in all the three groups. The haemodynamic variables never reached the baseline by 5 min in case of Group A. In Group B, they approached near the baseline by 3 min. In Group C, the variables fell below the baseline by 3 min. The group A had statistically higher values of HR, SBP, DBP and MAP at all time intervals post-intubation when compared to Group B and Group C. Hence, it can be inferred that the haemodynamic response was better obtunded in Group B and Group C, when compared with Group A. Although there was no statistically significant difference between Group B and Group C in any of the parameters at any point of time, in Group C patients, the intubation response was completely obtunded when compared to Group B. In Group C, the parameters fell below the baseline value at 3 min after intubation. This indicates that dexmedetomidine in a dose of 0.75 μg/kg was superior to dexmedetomidine in a dose of 0.5 μg/kg in completely attenuating the intubation response [Tables 2–5]. Neither bradycardia nor hypotension was observed in any of the patients. The sedation scores were more in Group B and Group C when compared to Group A [Table 6]. In none of the patients of any group did the SpO2 fall below 95%. None of the patients in any of the group needed oxygen supplementation.
Table 1.
Demographic details of patients
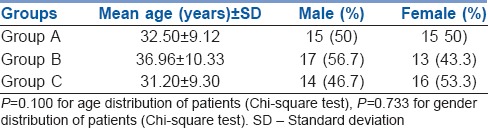
Table 2.
Comparison of heart rate between three groups

Table 5.
Comparison of mean arterial pressure between three groups
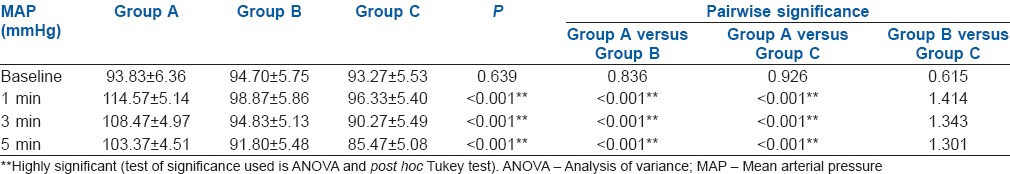
Table 6.
Sedation Scores between the three groups
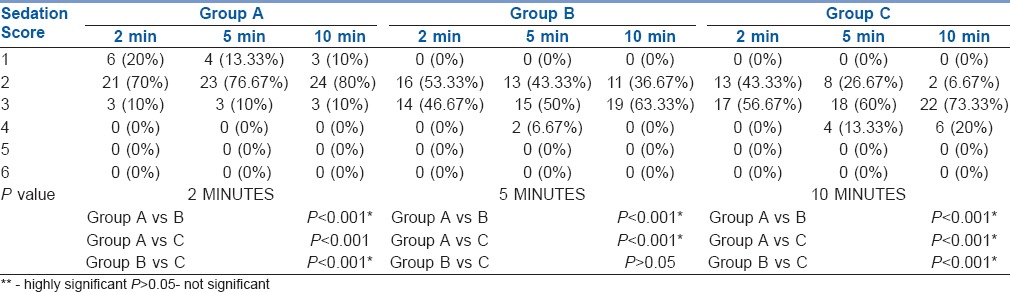
Table 3.
Comparison of systolic blood pressure between three groups
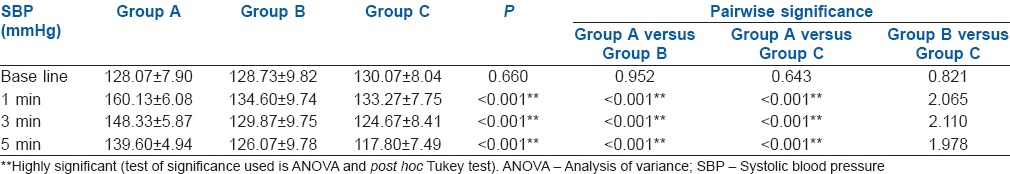
Table 4.
Comparison of diastolic blood pressure between three groups
DISCUSSION
The introduction of general anaesthesia made it possible to induce a state of controlled unconsciousness so that the patient is insensitive to pain and unaware of the events occurring during the surgical procedure. The anaesthetised patients are unable to maintain an adequate airway on their own, and there arises the need to employ artificial airway maintenance devices such as endotracheal tube. Traditionally, laryngoscopy and endotracheal intubation has been the mainstay in safeguarding the airway in such patients. Although intubation has its own advantages such as a safe and secured airway and prevention of aspiration and delivery of anaesthetic gases, it is not without complications. Laryngoscopy and endotracheal intubation are noxious stimuli capable of producing a huge spectrum of stress responses such as tachycardia, hypertension, laryngospasm, bronchospasm, raised intracranial pressure and intraocular pressure.[1]
The haemodynamic changes brought about by laryngoscopy and intubation was first described by Reid and Brace.[7] The haemodynamic response is initiated within seconds of direct laryngoscopy and further increases with the passage of the endotracheal tube. The response is initiated within 5 s of laryngoscopy, peaks in 1–2 min and returns to normal levels by 5 min.[8] These changes are usually short lived and well tolerated by normal patients. In patients with cardiovascular disease, it can incite harmful effects such as myocardial ischaemia, ventricular dysrrhythmias, ventricular failure and pulmonary oedema. It can also lead to cerebrovascular accidents in cerebrovascular disease patients.[9]
Various drug regimens and techniques such as lignocaine, opioids, nitroglycerine, calcium channel blockers such as diltiazem and β-blockers such as esmolol have been tried for obtunding the stress response.[8,10,11,12,13] α-2 receptor agonists mediate their action through α-2A receptors located in locus caeruleus, the predominant noradrenergic nuclei of upper brainstem. The presynaptic activation of α-2A receptors in the locus caeruleus inhibits the noradrenaline release and brings about sedation and hypnosis. Post-synaptic activation of α-2 receptors in central nervous system brings about decreased sympathetic activity leading to bradycardia and hypotension.[14]
Dexmedetomidine is eight times more potent α-2 receptor agonist than clonidine. The action of dexmedetomidine is short lived with an elimination half-time of 2 h. Dexmedetomidine has a reversal drug for its sedative effect called as atipamezole. Atipamezole acts by increasing the central turnover of noradrenaline. These factors make dexmedetomidine superior to clonidine.[15,16]
Dexmedetomidine has been studied by few authors in a dose of 0.5 and 1 μg/kg.[2,3,4] No study has been done to see the efficacy of dexmedetomidine in a dose of 0.75 μg/kg for attenuation of laryngoscopy and intubation response. Hence, in this study, we chose to include injection dexmedetomidine in a dose of 0.5 and 0.75 μg/kg and compare it with normal saline for attenuation of laryngoscopy and intubation response. The control group was used to ascertain whether dexmedetomidine has a favourable action or not. The two doses of dexmedetomidine were used which were felt as appropriate.
To lessen stress response to laryngoscopy and endotracheal intubation, it is prudent to keep the laryngoscopy time as less as possible and limit the duration of noxious stimulus. Hence, the laryngoscopy time has been limited to 15 s in this study. Laryngoscopy time was monitored with a stopwatch, and cases in whom the time exceeded 15 s have been excluded from the study. Further one more factor that influences the stress response to laryngoscopy and endotracheal intubation is the intubating conditions. It has been shown by studies that use of anticholinergic drugs before intubation has provided good intubating conditions.[17] Anticholinergics by virtue of their antisialagogue action offer good intubating conditions by decreasing the secretions. Amongst anticholinergic glycopyrrolate has got good antisialagogue action with less chance of causing increase in HR.[18] Hence, injection glycopyrrolate was chosen as good premedicant, to decrease the secretions and offer ideal intubating conditions on one side and not to interfere in haemodynamic parameters much with its moderate effect on the HR on the other side. The baseline values were recorded after glycopyrrolate administration to account for any small changes in readings. Further, it has been administered to all groups to eliminate any bias in readings. With this, any change in haemodynamic parameters recorded can be attributed to administration of study drug.
Smitha et al. compared the effect of 0.5 and 1 μg/kg of dexmedetomidine with normal saline in attenuating stress response. They found out that dexmedetomidine 1 μg/kg was more effective than dexmedetomidine 0.5 μg/kg in controlling haemodynamic responses to tracheal intubation. The intergroup comparison revealed a statistically significant reduction in HR by dexmedetomidine than normal saline.[19] These findings correlated with findings in our study.
Menda et al. conducted a study on ischaemic heart disease patients undergoing fast-track coronary artery bypass graft comparing dexmedetomidine 1 μg/kg and placebo. They inferred that in the placebo group, the systolic arterial pressure increased significantly after the intubation when compared to pre-intubation period, whereas it did not change significantly in the dexmedetomidine group.[4]
Two different doses of dexmedetomidine 1 and 0.5 μg/kg were compared with lignocaine 1.5 mg/kg to maintain haemodynamic stability associated with intubation by Gulabani et al. Dexmedetomidine 1 μg/kg was found to be more effective than dexmedetomidine 0.5 μg/kg and lignocaine.[20] Hence, it is of clinical use in cardiac patients in whom the stress response to laryngoscopy and intubation is highly unacceptable. The variations in DBP were in accordance with the recordings of our clinical trial. The variation in MAPs was parallel to the magnitude of change in SBP and DBP. In our study, though there was no statistical difference between dexmedetomidine 0.5 μg/kg and 0.75 μg/kg, the latter more effectively attenuated the intubation response. In fact, the values of the parameters fell below the baseline by 3 and 5 min following intubation with dexmedetomidine 0.75 μg/kg.
The sedation scores obtained were higher for dexmedetomidine group than normal saline in our study. A study by Manne et al. noting the effects of low-dose dexmedetomidine infusion on haemodynamic stress response, sedation and post-operative analgesia requirement in patients undergoing laparoscopic cholecystectomy also observed increasing sedation levels with dexmedetomidine.[21] Dexmedetomidine in a dose of 1 μg/kg has been shown to cause increased sedation levels and need for oxygen supplementation by few authors.[22,23] Dexmedetomidine when administered in different doses has been shown to cause irregular breathing with episodes of apnoea, especially with doses of 1.0 and 2.0 μg/kg.[23] Hence, in our study, dexmedetomidine has been administered slowly as an infusion over 10 min, followed by observation of its effect on respiration and SpO2. Further dexmedetomidine in a dose of 1 μg/kg has been found to be associated with increased incidence of adverse effects such as bradycardia and hypotension.[3,4] In our study, though six patients (20%) in Group C had sedation score of 4, none of them had fall in SpO2 below 95% or needed oxygen supplementation. No other adverse effects such as bradycardia or hypotension were noted in any of the group, and none of them required any medical intervention of any sort. Hence, in our study, dexmedetomidine 0.75 μg/kg effectively attenuated the stress response to laryngoscopy and intubation without any adverse effects on the haemodynamics or on the respiratory system. All patients were monitored in the post-operative period as a single dose of dexmedetomidine has a duration of action of 4 h.[23]
There were few limitations of our study. Invasive blood pressure monitoring was not used which would have provided us a better comprehension giving us beat-to-beat recording of the parameters. This was not performed due to cost constraints. Plasma catecholamine level monitoring was not performed due to the limited facilities available at our set-up. This could have comprehensively concluded the usefulness of dexmedetomidine.
CONCLUSION
Dexmedetomidine in doses of 0.5 and 0.75 μg/kg was more effective compared to normal saline in attenuating the haemodynamic stress response to laryngoscopy and endotracheal intubation. Dexmedetomidine 0.75 μg/kg attenuated the haemodynamic stress response to laryngoscopy and endotracheal intubation completely compared to 0.5 μg/kg. Both the doses of dexmedetomidine were devoid of any significant adverse effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 2.Sulaiman S, Karthekeyan RB, Vakamudi M, Sundar AS, Ravullapalli H, Gandham R. The effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass grafting. Ann Card Anaesth. 2012;15:39–43. doi: 10.4103/0971-9784.91480. [DOI] [PubMed] [Google Scholar]
- 3.Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55:352–7. doi: 10.4103/0019-5049.84846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menda F, Köner O, Sayin M, Türe H, Imer P, Aykaç B. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth. 2010;13:16–21. doi: 10.4103/0971-9784.58829. [DOI] [PubMed] [Google Scholar]
- 5.Laha A, Ghosh S, Sarkar S. Attenuation of sympathoadrenal responses and anesthetic requirement by dexmedetomidine. Anesth Essays Res. 2013;7:65–70. doi: 10.4103/0259-1162.113996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reid LC, Brace DE. Irritation of respiratory tract and its reflex effect on heart surgery. Surg Gynaecol Obstet. 1940;70:157–62. [Google Scholar]
- 8.Henderson J. In: Airway management in the adult. Miller's Anaesthesia. 7th ed. Miller RD, editor. Philadelphia: Churchill Livingstone; 2010. pp. 1573–610. [Google Scholar]
- 9.Prys-Roberts C, Greene LT, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971;43:531–47. doi: 10.1093/bja/43.6.531. [DOI] [PubMed] [Google Scholar]
- 10.Adachi YU, Satomoto M, Higuchi H, Watanabe K. Fentanyl attenuates the hemodynamic response to endotracheal intubation more than the response to laryngoscopy. Anesth Analg. 2002;95:233–7. doi: 10.1097/00000539-200207000-00043. [DOI] [PubMed] [Google Scholar]
- 11.Mikawa K, Hasegawa M, Suzuki T, Maekawa N, Kaetsu H, Goto R, et al. Attenuation of hypertensive response to tracheal intubation with nitroglycerin. J Clin Anesth. 1992;4:367–71. doi: 10.1016/0952-8180(92)90157-v. [DOI] [PubMed] [Google Scholar]
- 12.Kumar S, Mishra MN, Mishra LS, Bathla S. Comparative study of the efficacy of I.V. esmolol, diltiazem and magnesium sulphate in attenuating haemodynamic response to laryngoscopy and tracheal intubation. Indian J Anaesth. 2003;47:41–4. [Google Scholar]
- 13.Rathore A, Gupta GK, Tanwar GL, Rehman H. Attenuation of the pressure response to laryngoscopy and endotracheal intubation with different doses of esmolol. Indian J Anaesth. 2002;46:449–52. [Google Scholar]
- 14.Paranjpe JS. Dexmedetomidine: Expanding role in anesthesia. Med J DY Patil Univ. 2013;6:5–13. [Google Scholar]
- 15.Yazbek-Karam VG, Aouad MM. Perioperative uses of dexmedetomidine. Middle East J Anaesthesiol. 2006;18:1043–58. [PubMed] [Google Scholar]
- 16.Karhuvaara S, Kallio A, Salonen M, Tuominen J, Scheinin M. Rapid reversal of alpha 2-adrenoceptor agonist effects by atipamezole in human volunteers. Br J Clin Pharmacol. 1991;31:160–5. doi: 10.1111/j.1365-2125.1991.tb05505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falick YS, Smiler BG. Is anticholinergic premedication necessary? Anesthesiology. 1975;43:472–3. doi: 10.1097/00000542-197510000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Hata TM, Hata JS. In: Preoperative patient assessment and management. Clinical Anesthesia. 7th ed. Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R, editors. New Delhi: Wolters Kluwer Health, Lippincott Williams and Wilkins; 2013. pp. 583–611. [Google Scholar]
- 19.Smitha KS, Shukla D, Sathesha M, Rao R, Nethra S, Sudhhesh K, et al. Comparison of two different doses of dexmedetomidine in attenuating hemodynamic changes during laryngoscopy. J Evol Med Dent Sci. 2014;3:13501–8. [Google Scholar]
- 20.Gulabani M, Gurha P, Dass P, Kulshreshtha N. Comparative analysis of efficacy of lignocaine 1.5 mg/kg and two different doses of dexmedetomidine (0.5 μg/kg and 1 μg/kg) in attenuating the hemodynamic pressure response to laryngoscopy and intubation. Anesth Essays Res. 2015;9:5–14. doi: 10.4103/0259-1162.150167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manne GR, Upadhyay MR, Swadia V. Effects of low dose dexmedetomidine infusion on haemodynamic stress response, sedation and post-operative analgesia requirement in patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2014;58:726–31. doi: 10.4103/0019-5049.147164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sulhyan SR, Vagarali AT, Patil SS, Dixit MD. A comparative clinical study of dexmedetomidine versus placebo to attenuate hemodynamic response to endotracheal intubation in patients undergoing off pump coronary arterial bypass grafting. J Sci Soc. 2014;41:151–5. [Google Scholar]
- 23.Belleville JP, Ward DS, Bloor BC, Maze M. Effects of intravenous dexmedetomidine in humans. I. Sedation, ventilation, and metabolic rate. Anesthesiology. 1992;77:1125–33. doi: 10.1097/00000542-199212000-00013. [DOI] [PubMed] [Google Scholar]


